Abstract
The aim of this study was to explore the effect of butylphthalide on the brain edema, blood–brain barrier of rats of rats after focal cerebral infarction and the expression of Rho A. A total of 195 sprague–dawley male rats were randomly divided into control group, model group, and butylphthalide group (40 mg/kg, once a day, by gavage). The model was made by photochemical method. After surgery 3, 12, 24, 72, and 144 h, brain water content was done to see the effect of butylphthalide for the cerebral edema. Evans blue extravasation method was done to see the changes in blood–brain barrier immunohistochemistry, and Western blot was done to see the expression of Rho A around the infarction. Compared with the control group, the brain water content of model group and butylphthalide group rats was increased, the permeability of blood–brain barrier of model group and butylphthalide group rats was increased, and the Rho A protein of model group and butylphthalide group rats was increased. Compared with the model group, the brain water content of butylphthalide group rats was induced (73.67 ± 0.67 vs 74.14 ± 0.46; 74.89 ± 0.57 vs 75.61 ± 0.52; 77.49 ± 0.34 vs 79.33 ± 0.49; 76.31 ± 0.56 vs 78.01 ± 0.48; 72.36 ± 0.44 vs 73.12 ± 0.73; P < 0.05), the permeability of blood–brain barrier of butylphthalide group rats was induced (319.20 ± 8.11 vs 394.60 ± 6.19; 210.40 ± 9.56 vs 266.40 ± 7.99; 188.00 ± 9.22 vs 232.40 ± 7.89; 288.40 ± 7.86 vs 336.00 ± 6.71; 166.60 ± 6.23 vs 213.60 ± 13.79; P < 0.05), and the Rho A protein of butylphthalide group rats was decreased (western blot result: 1.2230 ± 0.0254 vs 1.3970 ± 0.0276; 1.5985 ± 0.0206 vs 2.0368 ± 0.0179; 1.4229 ± 0.0167 vs 1.7930 ± 0.0158;1.3126 ± 0.0236 vs 1.5471 ± 0.0158; P < 0.05). The butylphthalide could reduce the brain edema, protect the blood–brain barrier, and decrease the expression of Rho A around the infarction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cerebral edema is the secondary pathological process following cerebral infarction, and it may aggravate cerebral ischemia and hypoxia, increase infarct size, and induce high mortality and morbidity. Increased blood–brain barrier permeability after cerebral infarction may explain the occurrence of cerebral edema. Rho A protein is a major protein of Rho family, and it can bind with the GTP to participate in intercellular signal transduction. The activated Rho A combines with GTP to activate Rho-associated protein kinase II kinase, and accordingly, the activated myosin light chain phosphatation results in myosin light chain phosphorylation, increases blood–brain barrier (BBB) permeability, and aggravates cerebral edema [1]. DL-3-n-butylphthalide (NBP) is a class of drugs for acute ischemic cerebrovascular disease and has obvious therapeutic effect against on acute cerebral infarction. However, there is no study addressing the NBP on cerebral edema and Rho A protein expression in cerebral infarction rats. In this study, we aim to observe the influence of NBP on cerebral edema, BBB permeability, and cortical expression of Rho A in focal cerebral infarction rats, established using photochemical methods, in a broader attempt to provide evidence for clinical NBP applications.
Materials and Methods
Experimental Animals
A total of 220 cleaning healthy male Sprague–Dawley rats, weighing 280–320 g, were purchased from Beijing Vital River Laboratory Animal Technology Co., Ltd., (Beijing, China; certificate number SCXL (Beijing) 2002-003). All experimental procedures on animals were in accordance with the Guidelines for the Care and Use of Animals, issued by International Guidance Center of Life. Rats were housed in Animal Breeding Center of Dalian Medical University, China, under a natural-light, quiet, moderate-temperature room, allowing water ad libitum. All animals were randomly divided into a control group (n = 20), a model group (n = 100), and a NBP group (n = 100). Rats in NBP group were treated with NBP soft capsules the CSPC NBP Pharmaceutical Co., Ltd., China (40 mg/kg, once per day, orally), while rats in the control and model groups were given the same amount of vegetable oil by gavage.
Establishing Models
After rats were anesthetized using 10 % of chloral hydrate 3–5 mL/kg intraperitoneally, the rats in the model and NBP groups were injected with photosensitizer red tetrazolium (tetraiodotetrachloro-fluorescein B) 150 mg/kg into the tail vein. The head was fixed in a stereotaxic apparatus (NARISHIGE Company, Japan) and routinely disinfected, and then, a midline scalp incision was cut, exposing the right skull. The 6-mm-diameter skull was drilled at 3 mm right and 2 mm posterior to the bregma, and radiated using green cold light for 30 min, followed by skin suture. The awake rats after anesthesia were evaluated using Longa behavioral score scale, and those with 1–3 points were included. In the control group, rats were only injected with saline into the tail vein, the skull was exposed and grinded, and the irradiation exposure time was the same as above.
Criteria for successful models in Longa behavior score scale: 0 point, no defects; 1 point, rats cannot extend contralateral forelimb; 2 points, rats can extend contralateral forelimb; 3 points, rats circled mildly to the contralateral side; 4 points, rats circled severely to the contralateral side; and 5 points, rats failed to the contralateral side.
Determination of Brain Water Content
Five rats in each group were randomly selected at each time point and decapitated under 5–10 % chloral hydrate anesthesia. Brain tissues (200 mg) around the infarct area were collected; wet weight was measured using MA110 electronic analytical balance (Shanghai Second Balance Instrument Factory, Shanghai, China) and recorded, and then, brain tissues were placed in the oven at 105 °C and dried for 48 h to constant weight. Brain water content was calculated by Elliot formula:
Determination of BBB Permeability
Rats in each group were injected with 20 g/L of EB 3 mL/kg via the tail vein 1 h prior to the sacrifice and anesthetized with 10 % chloral hydrate. Subsequent to the thoracotomy, rats were injected with 37 °C saline through the left ventricle puncture to the aorta until clear liquid outflow from the right atrial appendage was visible. Cortical tissues (200 mg) were removed around the infarct size, weighed and immersed in 3 mL of dimethylformamide, followed by water bath at 37 °C for 48 h and 1,500×g centrifugation for 10 min. After the supernatant was discarded, the absorbance at 630 nm was measured using a microplate reader, and EB content was obtained from the standard curve. EB exudation in each group at each time point was analyzed and compared.
Immunohistochemical Detection for the Number of Rho A Positive Cells Around the Infarct Cortex
Five rats were randomly selected in each group at each time point for deep anesthesia, 4 % paraformaldehyde perfusion and decapitation. Then, the brains were harvested and fixed in 4 % paraformaldehyde overnight at 4 °C, and 2-mm-thick coronal slices containing the infarct area were rinsed using tap water for 48 h, graded with ethanol dehydration, xylene transparent, embedded in paraffin, and sectioned into slices at 5 μm thickness.
Three slices in each rat were dewaxed using xylene for 5 min, dehydrated using gradient alcohol, and digested with 3 % hydrogen peroxide at room temperature for 10 min, to eliminate endogenous peroxidase. Then, the slices were repaired in high-pressure heat and incubated with anti-Rho A (1:100; Wuhan Boster Biological Engineering Co., Ltd., Wuhan, Hubei Province, China) at 4 °C overnight. On the next morning, slices were tanked out and rinsed with PBS, then incubated with secondary antibody at 37 °C for 1 h, colorated with 3,3′-diaminobenzidine, rinsed and counter-stained with hematoxylin, dehydrated, transparent, and mounted with neutral gum. Under the light microscopy, cell nuclei were stained blue, and the positive cell swelling and yellow dye were observed. Under 400× magnification, five visual fields were randomly selected around the infarct area, and the number of positive cells in each visual field was calculated with the Image-Pro-Plus image analysis system (Media Cybernetics, USA).
Western Blot Analysis for Rho A Protein Expression in Peri-Infarct Cortex
Total protein in peri-infarct brain tissue was extracted using a cell lysate, and the protein content in each slice was determined using Coomassie brilliant blue staining. A total of 100 μg protein in each slice was subject to 15 % sodium dodecyl sulfate polyacrylamide gel electrophoresis, transferred to nitrocellulose film, and blocked using 5 % skim milk. The slices were incubated with goat anti-Rho A (rI’11r18/serl9) polyclonal primary antibody (1:500) and goat anti-actin polyclonal antibody (1:1,000) at 4 °C overnight and then hybridized with horseradish peroxidase-labeled goat anti-rabbit secondary antibody (1:1,000). Slices were developed using EcL luminescence agent for 3 min, exposed, and fixed. The mean absorbance value in Western blot analysis was analyzed using digital imaging analysis system, and the target absorbance served as the reference.
Statistical Analysis
Data among groups were compared using SPSS 17.0 software with analysis of variance, and all results were expressed as mean ± SD. A P < 0.05 level indicates a significant difference (Table 1).
Results
Determination of Brain Water Content
Brain water content in the control group was 71.78 ± 0.72 % and was significantly higher than the model and NBP groups (P < 0.05). In addition, the brain water content in NBP group was significantly decreased compared with model group (P < 0.05; Table 2).
Determination of BBB Permeability
The amount of Evans blue exudation in the control group was 11.20 ± 3.49, which was significantly lower than the model group (P < 0.05). Compared with the model group, Evans blue exudation in NBP group was reduced (P < 0.05; Table 2).
Immunohistochemistry Staining
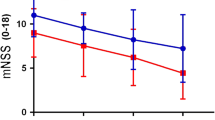
There is a small amount of brown-yellowish positive cells in the control group, accounting for 17.40 ± 2.07. The number of positive cells surrounding the infarct area was significantly increased in the model group compared with control group (P < 0.05), and the number of positive cells in NBP group was significantly reduced compared with model group (P < 0.05; Table 3; Fig. 1a–c).
Western Blot Analysis
The band gray value of the control group was 1.0716 ± 0.0069. The Rho A content in brain tissue surrounding the infarction was significantly increased in model group compared with the control group (P < 0.05). The myosin light chain content in peri-infarct cortex was decreased in NBP group compared with the model group (P < 0.05; Table 4; Fig. 2).
Discussion
Cerebral infarction is a common clinical ischemic cerebrovascular disease; cerebral edema is a major secondary pathological process after acute cerebral infarction and results in functional and structural damage in brain tissue; accordingly, diffuse brain edema can trigger the increase of intracranial pressure, even herniation, causing irreversible secondary pathological changes and brain death. Brain edema formation following acute cerebral infarction may apparently aggravate cerebral infarction symptoms and central nervous system injury. In this study, we established focal cerebral infarction models with photochemical method and detected the changes in brain tissue wet and dry weights. The results showed brain tissue water content increased significantly after acute cerebral infarction, and the most significant increase was observed at 24 h. This finding indicates that cerebral edema occurs immediately after acute cerebral infarction, especially at 24 h. The mechanisms underlying brain edema formation includes microcirculation disorder, ischemia and hypoxia, inflammatory injury, BBB damage, calcium overload, free radical damage, oxidative stress, and aquaporin-4 overexpression [2].
Rho A is the main member of Rho protein family, and the biological characteristics of Rho proteins contribute to reconstruct actin cytoskeleton are involved in the maintenance of the structural contractility of the cytoskeleton and the intact cell junction. Previous studies showed that some extracellular agonists (such as α-receptor agonist norepinephrine) could activate G-protein-coupled receptors, which trigger Rho A activation into Rho GTP, and Rho GTP further activates Rho-associated kinase, thus directly leading to myosin light chain phosphorylation [3]. The myosin light chain phosphorylation can also be activated by myosin light chain phosphatase, causing enhanced cytoskeleton contractility, increased endothelial permeability, and promoting brain edema formation [3]. In this study, immunohistochemistry and Western blot analysis showed that Rho A protein content around the infarct area increased significantly after acute cerebral infarction. Growing evidence showed that both oxyhemoglobin [4] and endothelin [5] can activate cell surface receptors and Rho A. Thrombin also functions to activate Rho A, thereby activating Rho-associated kinase and myosin light chain phosphorylation, which are characteristics of increased vascular endothelial permeability, BBB damage, and cerebral edema [6]. Moreover, extracellular angiotensin II and interleukin-1β may also increase Rho A expression and functions [7]. Tumor necrosis factor-α can activate Rho A through its receptors, thereby activating Rho GTP enzyme and promoting myosin light chain phosphorylation, and accordingly, smooth muscle is more sensitive to Ga2+, actomyosin contractility increased, vascular smooth muscle contracted, thereby aggravating cerebral ischemia/hypoxia and brain edema [8]. The stress response and inflammation after cerebral ischemia are closely related to the Rho signaling pathway. We speculate that after cerebral infarction caused increased endothelin and inflammatory reactions can activate Rho A, thereby activating Rho-associated kinase, inducing myosin light chain phosphorylation, increasing BBB permeability, and aggravating cerebral edema.
NBP is a class of newly emerged drugs for acute ischemic cerebrovascular disease. The results of this study showed that NBP reduced brain edema formation, hindered the increased BBB permeability, and decreased Rho A protein expression in the peri-infacrt cortex after cerebral infarction occurs. Previous studies showed that NBP reduced the number of neutrophils and the expression of interleukin-1β, tumor necrosis factor-α and other inflammatory cytokines at the infarct area [9], inhibited superoxide anion radical formation, and scavenged free radicals [10]. Accordingly, NBP could protect the mitochondria [11], increase energy metabolism at the ischemic area, and reduce BBB damage [12]. We speculate that NBP contributes to inhibit inflammatory response through decreasing the expression of interleukin-1β, tumor necrosis factor-α, and other inflammatory cytokines, thereby reducing the inflammatory response-caused activation of Rho A, suppressing myosin light chain phosphorylation, reducing BBB permeability damage and cerebral edema formation. In addition, acute cerebral infarction triggers systemic stress response, which accordingly increased the release of endothelin. NBP also plays an important role on reducing oxidative stress [13]. We speculate that NBP can reduce Rho A activation, hinder myosin light chain phosphorylation, suppress the increased BBB permeability, and reduce cerebral edema formation through lowing oxidative stress and endothelin.
In summary, NBP inhibits Rho A protein expression in cerebral cortex around focal cerebral infarction, thereby reducing myosin light chain phosphorylation, BBB damage and cerebral edema, further providing evidence for treating cerebral infarction and clinical application of NBP.
References
Kawasaki, K., et al. (2009). Correspondence between neurological deficit, cerebral infarct size, and Rho-kinase activity in a rat cerebral thrombosis model. Journal of Molecular Neuroscience, 39(1–2), 59–68.
Yongliang, L., Peng, W., & Jianming, L. (2013). Advance on the mechanism of brain edema after head injury. Guide of Chinese Medicine, 11(8), 3.
Duan, W. G., et al. (2007). Advances in the study of Rho kinase and its inhibitors. Yao Xue Xue Bao, 42(10), 1013–1022.
Alexander, J. S. (2000). Rho, tyrosine kinase, Ca(2+), and junctions in endothelial hyperpermeability. Circulation Research, 87(4), 268–271.
Wickman, G., Lan, C., & Vollrath, B. (2003). Functional roles of the rho/rho kinase pathway and protein kinase C in the regulation of cerebrovascular constriction mediated by hemoglobin: Relevance to subarachnoid hemorrhage and vasospasm. Circulation Research, 92(7), 809–816.
Lan, C., et al. (2004). Endothelin-1 modulates hemoglobin-mediated signaling in cerebrovascular smooth muscle via RhoA/Rho kinase and protein kinase C. American Journal of Physiology-Heart and Circulatory Physiology, 286(1), H165–H173.
Hiroki, J., et al. (2004). Inflammatory stimuli upregulate Rho-kinase in human coronary vascular smooth muscle cells. Journal of Molecular and Cellular Cardiology, 37(2), 537–546.
Doe, C., et al. (2007). Novel Rho kinase inhibitors with anti-inflammatory and vasodilatory activities. Journal of Pharmacology and Experimental Therapeutics, 320(1), 89–98.
Xu, H. L., & Feng, Y. P. (2000). Inhibitory effects of chiral 3-n-butylphthalide on inflammation following focal ischemic brain injury in rats. Acta Pharmacologica Sinica, 21(5), 433–438.
Bo, S., et al. (2011). The protective mechanism of dl-3-n butylphthalide on oxidative stress injury in rat bone marrow mesenchymal stem cells. International Journal of Cerebrovascular Diseases, 11(2), 5.
Xiong, J., & Feng, Y. P. (2000). The protective effect of butylphthalide against mitochondrial injury during cerebral ischemia. Acta Pharmaceutica Sinica, 35, 5.
Zhang, Y., et al. (2006). 2-(1-Hydroxypentyl)-benzoate increases cerebral blood flow and reduces infarct volume in rats model of transient focal cerebral ischemia. Journal of Pharmacology and Experimental Therapeutics, 317(3), 973–979.
Zhaozhong, C., & Yipu, F. (1999). Effect of 3-n-butylphthalide on reperfusion induced lipid peroxidation following cerebral ischemia in rats and superoxide radical formation in vitro. Journal of Chinese Pharmaceutical Sciences, 8, 5.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hu, J., Wen, Q., Wu, Y. et al. The Effect of Butylphthalide on the Brain Edema, Blood–Brain Barrier of Rats After Focal Cerebral Infarction and the Expression of Rho A. Cell Biochem Biophys 69, 363–368 (2014). https://doi.org/10.1007/s12013-013-9808-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12013-013-9808-0