Abstract
Bacterial lipopolysaccharide (LPS) is a known ligand of Toll-like receptor 4 (TLR4) which is expressed in cardiac fibroblasts (CF). Differentiation of CF to cardiac myofibroblasts (CMF) is induced by transforming growth factor-β1 (TGF-β1), increasing alpha-smooth muscle actin (α-SMA) expression. In endothelial cells, an antagonist effect between LPS-induced signaling and canonical TGF-β1 signaling was described; however, it has not been studied whether in CF and CMF the expression of α-SMA induced by TGF-β1 is antagonized by LPS and the mechanism involved. In adult rat CF and CMF, α-SMA, ERK1/2, Akt, NF-κβ, Smad3, and Smad7 protein levels were determined by western blot, TGF-β isoforms by ELISA, and α-SMA stress fibers by immunocytochemistry. CF and CMF secrete the three TGF-β isoforms, and the secretion levels of TGF-β2 was affected by LPS treatment. In CF, LPS treatment decreased the protein levels of α-SMA, and this effect was prevented by TAK-242 (TLR4 inhibitor) and LY294002 (Akt inhibitor), but not by BAY 11-7082 (NF-κβ inhibitor) and PD98059 (ERK1/2 inhibitor). TGF-β1 increased α-SMA protein levels in CF, and LPS prevented partially this effect. In addition, in CMF α-SMA protein levels were decreased by LPS treatment, which was abolished by TAK-242. Finally, in CF LPS decreased the p-Smad3 phosphorylation and increased the Smad7 protein levels. LPS treatment prevents the CF-to-CMF differentiation and reverses the CMF phenotype induced by TGF-β1, through decreasing p-Smad3 and increasing Smad7 protein levels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bacterial lipopolysaccharide (LPS) is an essential component of the cell wall in pathogenic gram-negative bacteria. LPS is an important mediator in septic shock secondary to infection as well as in cardiac disease [30]. LPS is also a well-known agonist of Toll-like receptor 4 (TLR4), a receptor expressed by innate immune system cells as well as non-immune system cells [41]. This ligand’s interaction with TLR4 activates the NF-κβ, ERK1/2, Akt, and other intracellular signaling pathways that promote early inflammatory responses, inducing the expression of cytokines and other pro-inflammatory mediators [29, 30] and triggering an immediate response to restore homeostasis [17]. In addition, TLR4 recognizes damage-associated molecular patterns (DAMPs) [26], including heat shock proteins such as HSP60 and HSP70 [6]; surfactant protein A; high-mobility group box 1 protein (HMGB1); fibrinogen; fibronectin-EDA [28]; and polysaccharides, such as heparan sulfate (HS) [18]. It has recently been shown that TLR4-KO mice are protected against isoproterenol-induced cardiac fibrosis, which is associated with cardiac fibroblast autophagy [14]. In addition, TLR4 promotes left ventricular fibrosis and maladaptive remodeling [37], lung fibroblast proliferation [21], and cytokine release [49].
Cardiac fibroblasts (CF) are cells of mesenchymal origin that play an important role in cardiac remodeling, a process that typically occurs after a damaging stimulus to cardiac tissue. CF are considered “sentinel cells,” as they are key cellular elements in repairing damaged tissue [11]. The purpose of remodeling is to replace damaged areas and restore heart function [16]. If the repair process is prolonged due to the persistent presence of a harmful stimulus, it becomes chronic and pathological, resulting in increased risk of heart dysfunction [45]. All of these changes trigger local inflammatory responses, which mediate resolution of the fibrotic process with the help of the immune system, synthesizing cytokines and growth factors such as transforming growth factor beta 1 (TGF-β1). In response to TGF-β1, CF differentiates into cardiac myofibroblasts (CMF). CMF are characterized by high levels of alpha-smooth muscle actin (α-SMA), a contractile protein marker for this phenotype that provides sufficient mechanical tension to contract and close the wound, forming scar tissue [5]. Thus, CMF have an active role in the pathogenesis of fibrosis, given their ability to secrete high levels of extracellular matrix proteins and fibrogenic cytokines.
Currently, there is evidence for a role of TLR involvement with fibroblasts in diseases like asthma, where TLR3 stimulation by a synthetic analog of double-stranded RNA significantly increases the amount of active TGF-β1 and thus induces differentiation into myofibroblasts [35]. A model of lung fibroblasts and myofibroblasts demonstrated that autocrine effects of TGF-β1 induce secretion of hyaluronic acid, an extracellular matrix component that is an endogenous ligand of TLR4 and is essential for myofibroblast phenotype maintenance [44]. In contrast, NF-κβ activation is known to have an antagonistic effect on α-SMA in vascular smooth muscle cells [32]. Finally, evidence suggests an ambiguous role of TLR4 in the myofibroblast differentiation process and phenotype maintenance. Despite extensive literature on the pro-inflammatory and pro-fibrotic cytokines released by CF and CMF after cardiac tissue damage, it is not known exactly how the TLR4 receptor contributes to the secretion of these proteins, or how activation regulates the transition from an inflammatory to a fibrotic phase. The effects of TLR4 on cardiac fibroblast α-SMA expression and modulation of myofibroblast differentiation are also yet to be described.
In this work, we demonstrate the effect of LPS-induced TLR4 activation on α-SMA protein expression in CF, as well as the signaling pathways involved in reversing CMF differentiation. Additionally, we determine the cellular signaling pathways used by TLR4 to inhibit TGF-β1-induced fibrosis. Our hypothesis is that TLR4 activation prevents TGF-β1-induced differentiation of CF into CMF.
Methods and Materials
Reagents
The following reagents were obtained from Sigma Chemical Co (St. Louis, MO, USA): trypan blue, selective inhibitor of MAP kinase kinases, PD98059 (PD), PI3k inhibitor, LY294002 (LY), NF-κβ inhibitor, BAY 11-7082 (BAY), ketamine, collagenase, Triton X-100, the primary antibodies for α-SMA, and GAPDH. Trypsin/EDTA, pre-stained molecular weight standards, fetal bovine serum (FBS), and fetal calf serum (FCS) were obtained from Gibco BRL (Carlsbad, CA, USA). 488 Alexa Fluor®-conjugated secondary antibodies was obtained from Sigma-Aldrich. Anti-Smad7 was obtained from Santa Cruz Biotechnology (Dallas, USA). LPS and TAK-242 (TLR4 inhibitor) were obtained from InvivoGen (San Diego, USA). All organic and inorganic compounds were from Merck (Darmstadt, Germany). The primary antibodies for ERK1/2 (#9102), p-ERK1/2 (#9101), Akt (#9272), p-Akt (#9271), Smad3 (#9515), and p-Smad3 (#9520) were purchased from Cell Signaling Technology (Boston, MA, USA). The enhanced chemo-luminescence reagent was from PerkinElmer Life Sciences, Inc. (Boston, MA, USA). TGF-β1 was from Millipore (Billerica, MA, USA). Secondary antibodies conjugated with horseradish peroxidase were obtained from Calbiochem. The sterile plastic material used for CF cultures was purchased from Falcon®.
Animals
Male adult Sprague Dawley rats were obtained from the animal breeding facility of the Faculty of Chemical and Pharmaceutical Sciences at the University of Chile. The animals were housed in cages (12-h light/dark cycles) with access to rat chow and water ad libitum. All studies were performed in compliance with the NIH Guide for the Care and Use of Laboratory Animals, updated in 2011 (http://grants.nih.gov/grants/olaw/Guide-for-the-Care-and-Use-of-Laboratory-Animals), and experimental protocols were approved by our Institutional Ethics Review Committee.
Cell Culture and Treatments
CF were isolated from the left ventricle (LV) of adult Sprague Dawley rats. Briefly, LV were harvested, cut into small pieces (~1–2 mm), and placed in a petri dish. A total of 10 mL Dulbecco’s modified Eagle’s medium containing 10% fetal bovine serum (FBS) and antibiotics was added to petri dishes. Petri dishes were maintained at 37 °C under 5% CO2 in a humidified incubator until reaching 70% confluence. Adherent cells were cultivated. Cells from passage 1 were used for all experiments. Cells were maintained in M199 medium for 18 h until experiments were performed. Immunocytochemical staining was used to evaluate the extent of cell purity achieved in our cell culture preparations. Monoclonal antibodies directed against sarcomeric (striated muscle) actin and desmin (Sigma Chemical Co, St Louis, Mo) were used to positively identify cardiac myocytes and smooth muscle cells, whereas a polyclonal antibody directed against human factor VIII was used for endothelial cells (Dako Corp., Carpinteria, Calif). Positive staining with a polyclonal anti-vimentin antibody (Santa Cruz Biotech, CA) and negative for the above-mentioned factors characterized cardiac fibroblasts.
Differentiation from Cardiac Fibroblasts to Cardiac Myofibroblasts
Primary CF cultures were stimulated with TGF-β1 (5 ng/mL) for 96 h and characterized as CMF (α-SMA positive), as described by Copaja et al., 2011 [8].
Western Blot Analysis
After respective treatments, cells were lysed in 50 mM Tris, 300 mM NaCl, 1 mM MgCl2, 0.5 mM EDTA, 0.1 mM EGTA, 20% glycerol, 1% NP40, 0.5 mM DTT, and inhibitor cocktail. Lysates were vigorously vortexed for 10 s and centrifuged at 15,000 rpm for 10 min, and total protein content was determined using Bradford assay. Equivalent amounts of protein were subjected to SDS–PAGE. Western blotting was performed by transferring proteins to nitrocellulose membranes and blocking with 10% fat-free milk (w/v) in TBS-Tween for 1 h at room temperature. Membranes were probed with the appropriate primary antibody overnight at 4 °C and then with peroxidase-conjugated secondary antibody for 2 h at room temperature. Finally, the ECL Advance Western Blotting Detection kit was used for immunodetection. Protein levels were determined by densitometric analysis using ImageJ (NIH, Bethesda, MD, USA) and normalized to the corresponding GAPDH level.
Immunofluorescence Assay
The images by immunocytochemistry were obtained with confocal microscopy. FCs were grown on coverslips. After completion of the corresponding stimuli, the cells were washed with 10% PBS and fixed for 20 min with 4% paraformaldehyde. They were then washed and permeabilized with 0.1% Triton X-100 for 10 min. After the time was over, they were washed with 10% PBS and blocked with 3% BSA for 1 h. They were then washed again and incubated with primary antibody to α-SMA (1:50) in BSA overnight. The next day, the cells were washed and the Alexa Fluor® 566-conjugated secondary antibody (red staining), in addition to Hoechst (1:100) for nuclear labeling, was placed for 2 h. Quantification of the total relative fluorescence of the images obtained by confocal microscopy was performed using the ImageJ program, 10× magnification images, scale bar of 50 μm. Identical exposure-time were used to capture images.
TGF-β Luminex Immunobead Assay
Total TGF-β1, TGF-β2, and TGF-β3 levels in CF and CMF were measured using Luminex bead assay (Upstate-Millipore) with HCl activation. Cell samples were activated by adding 1 N HCl to each tube. Tubes were then incubated for 1 h at room temperature, and samples were neutralized by adding 1 N NaOH. Cell samples were pipetted into a 96-well plate and incubated overnight with 25 μL of 1 × beads coupled to TGF-β1, TGF-β2, and TGF-β3, protected from light. Controls included assay buffer and recombinant human TGF-β1 and TGF-β2. Serial dilutions of TGF-β1 and TGF-β2 were added to wells in the same plate to generate a standard curve. After overnight incubation, 25 μL of biotinylated secondary cytokine antibody mixture was applied for 1.5 h in the dark at room temperature. The reactions were detected with streptavidin–phycoerythrin conjugate with a Luminex 100 IS 2.3 system (Merck).
Statistical Analysis
Data are presented as mean ± SEM from at least n independent experiments. Statistical analysis was performed using one-way ANOVA and Tukey’s test for multiple comparisons with GraphPad Prism 5.0 software. p < 0.05 was considered statistically significant.
Results
Cardiac Fibroblasts and Myofibroblasts Secrete TGF-β (1, 2, and 3) Isoforms
First, as shown in Fig. 1a–c both CF and CMF secreted TGF-β1, TGF-β2, and TGF-β3, respectively, into the culture medium. However, CMF secreted significantly higher levels of the three TGF-β isoforms than CF (15 vs. 45 pg/mL for TGF-β1; 131 vs. 762 pg/mL for TGF-β2; and 11 vs. 26 pg/mL for TGF-β3, CF vs. CMF, respectively). It is noteworthy that both CF and CMF released significantly higher levels of TGF-β2 than TGF-β1 or 3 in all study groups. Furthermore, to determine the ability of LPS to modulate of TGF-β1, 2, and 3 expressions through TLR4, CF and CMF were stimulated with LPS for 48 h in the presence or absence of TAK-242 (a TLR4 signaling pathway inhibitor). The results show that LPS significantly reduced TGF-β2 and TGF-β3 levels to 48 h in CMF, but not in CF, as compared to baseline (762 vs. 466 pg/mL for TGF-β2; 26 vs. 15 pg/mL for TGF-β3) but had no significant effect on TGF-β1. On the other hand, TAK-242 completely inhibited the effect triggered by LPS (762 vs. 656 pg/mL and 26 vs. 27 pg/mL for TGF-β2 and 3, respectively).
Effect of LPS on TGF-β (1, 2 and 3) expression in cardiac fibroblasts and myofibroblasts. CF and MCF were stimulated for 48 h with LPS (1 μg/mL) in the presence or absence of TAK-242 (4 μM/mL). Quantification of the total levels of TGF-β1 (a), TGF-β2 (b), and TGF-β3 (c) normalized by the number of cells. +++p < 0.001 myofibroblasts vs fibroblasts; #p < 0.05 versus control CF; *p < 0.05 versus control CMF. The results are means (±SEM) of 5 independent experiments
LPS Decreases α-SMA Expression in CF
We determined the effect of LPS on α-SMA protein levels in CF. Cells were stimulated with LPS (1 μg/mL) for 24, 48, 72, and 96 h. Figure 2a shows that from 24 h, LPS decreased α-SMA protein levels relative to the control, and that this difference reached significance by 48 h. For immunofluorescence assay, cells were stimulated with LPS (1 μg/mL) for 24 and 72 h. Figure 2b shows that treated cells had lower α-SMA expression and stress fiber assembly rates. This result was similar, after quantifying the relative fluorescence of anti α-SMA. In addition, these cells were smaller and showed reduced stress fiber assembly as compared to control CF.
LPS inhibits the expression of α-SMA in CF. a CF were stimulated with LPS (1 μg/mL) for 24, 48, 72, and 96 h. α-SMA protein levels were quantified by western blotting. GAPDH was used as a load control. *p < 0.05 versus control 48 h; **p < 0.01 versus control 72 and 96 h. The results are means (±SEM) of 5 independent experiments. b CF were stimulated with LPS (1 μg/ml) for 24 and 72 h. α-SMA was detected by immunofluorescence using anti-α-SMA antibody, Alexa Fluor® 566-conjugated secondary antibody (red staining), and Hoechst for the nuclei (blue). c Quantification of the total relative fluorescence of the images obtained by confocal microscopy, 10x magnification images, scale bar of 50 μm. Identical exposure-time were used to capture images. The intensity of staining obtained with anti-α-SMA antibody was measured in each unaltered cell. **p < 0.01 versus control 24 h; ++< 0.01 versus control 72 h. The results are means (± SEM) of 5 independent experiments
TLR4 Participates in the Decreased α-SMA Expression Induced by LPS
To determine the role of TLR4 in the LPS-induced decrease in α-SMA expression, cells were pre-treated for 30 min with TAK-242 (4 μM/mL), a TLR4 signaling pathway inhibitor, and then stimulated with LPS (1 μg/mL). Figure 3a shows that after 48 h, TAK-242 had reverted the decreased α-SMA expression induced by LPS to control levels, whereas TAK-242 alone did not alter α-SMA levels. For immunofluorescence assay, the cells were pre-treated for 30 min with TAK-242, stimulated with LPS for 48 h, and fixed in coverslips. Figure 3b shows that LPS reduced both α-SMA expression and assembly into stress fibers; however, TAK-242 inhibited these LPS-induced effects. This result was similar, after quantifying the relative fluorescence of anti α-SMA.
Participation of TLR4 α-SMA protein levels in CF. A) CF were stimulated with LPS (1 μg/ml) for 72 h in the presence or absence of TAK-242 (4 μM/mL). α-SMA protein levels were quantified by western blotting. GAPDH was used as a load control. ***p < 0.001 versus control. The results are means (± SEM) of 5 independent experiments. b CF were stimulated with LPS (1 μg/ml) for 72 h in the presence or absence of TAK-242 (4 μM/mL). α-SMA was detected by immunofluorescence using anti-α-SMA antibody, Alexa Fluor® 566-conjugated secondary antibody (red staining), and Hoechst for the nuclei (blue). c Quantification of the total relative fluorescence of the images obtained by confocal microscopy, 10x magnification images, scale bar of 50 μm. Identical exposure-time were used to capture images. The intensity of staining obtained with anti-α-SMA antibody was measured in each unaltered cell. **p < 0.01 versus control; +++p < 0001 versus LPS. The results are means (± SEM) of 5 independent experiments
LPS Activates NF-κβ, ERK1/2, and Akt Through TLR4 to Decrease α-SMA Levels
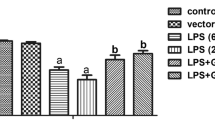
After characterizing the involvement of TLR4 in α-SMA expression in CF, we determined whether the NF-κβ, ERK1/2, and Akt signaling pathways were involved in these effects. Figure 4a shows that LPS (1 μg/mL) significantly increased p65-NF-κβ phosphorylation from 5 to 30 min. ERK1/2 was phosphorylated significantly from 30 min, peaking at 60 min (Fig. 4b), whereas Akt was phosphorylated significantly from 60 min, with levels holding steady to 120 min (Fig. 4c). However, despite these findings, it remained unclear whether these proteins were involved in the LPS-induced decreases in α-SMA protein expression. To this end, CF were stimulated for 48 h with LPS in the presence or absence of the respective inhibitors. BAY 11-7082 (10 μM, an NF-κβ inhibitor) alone reduced α-SMA protein levels as compared to control. However, NF-κβ inhibition did not prevent the LPS-induced effect on α-SMA expression (Fig. 4d). PD98059 (10 μM, an ERK1/2 inhibitor) alone did not affect α-SMA expression levels nor prevent the LPS-induced effect on α-SMA expression (Fig. 4e). Finally, LY294002 (10 μM, an Akt inhibitor) alone did not reduce α-SMA expression compared to control, whereas the effect of LPS (1 μg/mL) was blocked by LY294002 (Fig. 4f).
LPS through Akt decrease α-SMA protein levels in adult cardiac fibroblast. CF were stimulated with LPS (1 μg/ml) for 5, 15, 30, 60, or 120 min, and a representative image of p-NF-κβ (a), p-ERK 1/2 (b) y p-Akt (c), and quantification of the p-NF-κβ/NF-κβ total, p-Akt/Akt total, p-ERK/ERK total, ratio normalized as fold over control were shown. The results are means (± SEM) of 6 independent experiments. CF were stimulated with LPS (1 μg/ml) for 72 h in the presence or absence of: d BAY 11-7082 (0,5 μM); e PD98059 (10 μM) or f LY294002 (1 μM). α-SMA protein levels were quantified by western blotting. GAPDH was used as a load control. *p < 0.05 vs control, **p < 0.01 versus control, and ***p < 0001 versus control. The results are means (± SEM) of 5 independent experiments
LPS Inhibits the Signaling Pathway Triggered by TGF-β1 Through TLR4
According to our initial results, CF are able to secrete TGF-β isoforms, which induce α-SMA expression through an autocrine mechanism. Thus, we next tested whether LPS could prevent the increased α-SMA expression induced by the exogenous addition of TGF-β1. CF were pre-treated with LPS 1 (μg/mL), and 30 min later the cells were stimulated with TGF-β1 (5 ng/mL). Figure 5a shows that TGF-β1 (48 h) significantly increased α-SMA expression levels relative to the controls. However, LPS treatment inhibited partially this TGF-β1-induced increase in α-SMA expression. Similarly, Fig. 5b shows the immunocytochemical evidence of TGF-β1-induced α-SMA expression and assembly into stress fibers. However, pre-treatment with LPS reduced α-SMA expression and assembly, in both TGF-β1-treated CF and untreated CF. This result was confirmed, after quantifying the relative fluorescence of anti α-SMA.
Inhibition of effects and signaling TGF-β by LPS. a and b CF were pre-stimulated with LPS (1 μg/mL) for 30 min and then were stimulated with TGF-β1 (5 ng/mL) for 72 h. α-SMA protein levels were quantified by western blotting. GAPDH was used as a load control. ***p < 0.001 versus control; +p < 0.05 versus TGF-β1. The results are means (± SEM) of 4 independent experiments. α-SMA was detected by immunofluorescence using anti-α-SMA antibody, Alexa Fluor® 566-conjugated secondary antibody (red staining) and Hoechst for the nuclei (blue). Quantification of the total relative fluorescence of the images obtained by confocal microscopy, 10x magnification images, scale bar of 50 μm. Identical exposure-time were used to capture images. The intensity of staining obtained with anti-α-SMA antibody was measured in each unaltered cell. **p < 0.01 versus control; +p < 0.05 versus TGF-β1. The results are means (± SEM) of 5 independent experiments. c CF were pre-stimulated with LPS (1 μg/mL) for 1 h and then were stimulated with TGF-β1 (5 ng/mL) for 2 h. p-Smad3 protein levels were quantified by western blotting. Total Smad3 was used as a load control. ***p < 0.01 versus control; +p < 0.05 versus TGF-β1. The results are means (± SEM) of 4 independent experiments. D) CF were pre-stimulated with LPS (1 μg/mL) for 1 h and then were stimulated with TGF-β1 (5 ng/mL) for 2 h. Smad7 protein levels were quantified by western blotting. GAPDH was used as a load control. ***p < 0.001 versus control; +p < 0.05 versus LPS. The results are means (± SEM) of 4 independent experiments
In CF, TGF-β1 activates several signaling pathways, including its canonical pathway (Smad3), to induce α-SMA expression and assembly. Thus, we tested whether an LPS-induced decrease in α-SMA expression would modify Smad3 protein phosphorylation and Smad7 levels. As shown in Fig. 5c, treating CF for 2 h with TGF-β1 (5 ng/mL) significantly increased Smad3 phosphorylation relative to controls. LPS blocked this effect of TGF-β1 in CF. We also studied the key negative regulator of TGF-β1 signaling, Smad7, which may be associated with the anti-fibrotic effects of TLR4 activation. As shown in Fig. 5d, CF treated with TGF-β1 did not show significantly altered Smad7 protein levels. However, LPS treatment increased Smad7 protein levels relative to the control. In addition, in CF pre-treated with LPS for 1 h and then treated with TGF-β1, Smad7 protein levels were partially reduced, although they remained higher than control levels.
LPS Decreases α-SMA Expression Levels in CMF
It is well established that CF differentiation into CMF is triggered by TGF-β1 and that this process is characterized by a significant increase in α-SMA expression and assembly, which is used as a marker for the myofibroblast phenotype. Due to the high levels of α-SMA production in CMF, we wanted to assess whether LPS was able to reverse the myofibroblast phenotype and if so, whether this reversal occurred via TLR4. To this end, CF were treated with TGF-β1 for 96 h (to induce CF-to-CMF differentiation) and then washed and maintained in DMEM for 24 h until the experiments. The cells were pre-treated with TAK-242 (4 μM) for 1 h and then stimulated with LPS (1 μg/mL) for 48 h. Figure 6a shows that the CMF expressed significantly higher levels of α-SMA levels and that treatment with TAK-242 did not modify these levels. Pre-treatment with TAK-242 inhibited the LPS-induced decrease in α-SMA expression. CMF were prepared as described above for immunofluorescence assays. Figure 6b shows that LPS reduced both α-SMA expression and assembly in CMF. TAK-242 alone did not affect α-SMA assembly, but the inhibitor completely blocked the effect of LPS on α-SMA assembly into stress fibers. This result was confirmed, after quantifying the relative fluorescence of anti α-SMA in CMF.
TLR4 activation regulates α-SMA expression on cardiac myofibroblasts. a CMF were stimulated with LPS (1 μg/mL) for 24 h in the presence or absence of TAK-242 (4 μM/mL). α-SMA protein levels were quantified by western blotting. GAPDH was used as a load control. ***p < 0.001 versus control; ###p < 0.001 versus LPS. The results are means (± SEM) of 4 independent experiments. c) CMF were stimulated with LPS (1 μg/mL) for 24 h in the presence or absence of TAK-242 (4 μM/mL) and SB431542 (10 μM/mL). α-SMA protein levels were quantified by western blotting. GAPDH was used as a load control. ***p < 0.001 versus control. The results are means (± SEM) of 4 independent experiments. In B) and d α-SMA was detected by immunofluorescence using anti-α-SMA antibody, Alexa Fluor® 566-conjugated secondary antibody (red staining), and Hoechst for the nuclei (blue). The respective quantification of the total relative fluorescence of the images obtained by confocal microscopy is shown, 10x magnification images, scale bar of 50 μm. Identical exposure-time were used to capture images. The intensity of staining obtained with anti-α-SMA antibody was measured in each unaltered cell. *p < 0.05 versus control; ++p < 0.01 versus LPS (for (B). The results are means (± SEM) of 5 independent experiments. ++p < 0.01 vs control (d). The results are means (± SEM) of 5 independent experiments
To corroborate this effect, we treated CMF with SB431542 (a TGF-β1R antagonist). This blocker decreased α-SMA expression levels (Fig. 6c). According to previous results, by quantifying the relative fluorescence of anti-SMA, it was confirmed that SB431542 reduced the expression of α-SMA and the assembly in tension fibers. The size of the cell was also reduced (Fig. 6d). TAK-242 did not significantly affect the assembly of α-SMA.
Finally, Fig. 7 summarizes schematically that in CF the treatment with LPS regulates expression of Smad7 and p-Smad3, which triggers the decreases in α-SMA expression levels, whereas in CMF LPS triggers the regression of this differentiated phenotype induced by TGF-β1.
Schematic representation of LPS effects in CF and CMF on α-SMA expression levels. (Left) Cardiac fibroblast. Mechanical stress stimulates the secretion of TGF-βs (black lines), which in autocrine manner (red arrow) stimulates the TGF-β1 receptor and activates Smad3-dependent signaling pathway, increasing α-SMA expression levels (red lines). LPS through TLR4/Akt/Smad7 signal transduction pathway (blue lines) reduces the effects of TGF-β1 on α-SMA expression levels. (Right) Cardiac myofibroblast. Exogenous TGF-β1 addition or TGF-βs secreted by mechanical stress stimulates (black lines) the TGF-β1 receptor (red arrow), increasing α-SMA expression levels (red lines) and their assembly into stress fibers. LPS via TLR4 (blue lines) reduces both expression levels, as well as α-SMA assembly on stress fibers. Inhibition of TGF-β1 receptor signaling by SB431542 reverses the effects of TGF-β1
Discussion
LPS is a well-known endotoxin with numerous effects on cardiac function. In a murine model, chronic exposure to subclinical LPS levels results in cardiac fibrosis and severe cardiac dysfunction, increasing mortality after 2–3 months [24]. In a human cardiac fibroblast model, LPS enhanced mRNA expression of inflammatory cytokines such as tumor necrosis factor-a (TNF-α) and IL-1β and caused overproduction of nitric oxide [39]. In the heart, CF play a central role in maintaining extracellular matrix homeostasis and differentiation into CMF but also mediate inflammatory and fibrotic myocardial remodeling in the diseased heart [5]. Here, we show that in CF and CMF, LPS decreases levels of α-SMA protein, which may be critical in the wound healing process after cardiac injury.
TLR4 Differentially Modulates the TGF-β Isoforms Released by Cardiac Fibroblasts and Myofibroblasts
Our results show that both CF and CMF secrete all three TGF-β isoforms, and moreover, that CMF secrete higher levels of each TGF-β isoform than CF. These results are consistent with the increased α-SMA levels in both cells and suggest that TGF-β secreted by CF and CMF can increase α-SMA expression through an autocrine mechanism, which are consistent with those described by Tiede et al. [36]. The TGF-β family consists of 3 isoforms, TGF-β1, TGF-β2, and TGF-β3, encoded by different genes; of the three, TGF-β1 has been studied most extensively [27]. All three protein isoforms share similar affinities for the cognate receptors. TGF-β1 is released primarily by platelets in tissue repair events and is the main promoter fibroblast-to-myofibroblast differentiation [40]. Myofibroblasts are also able to secrete TGF-β1 into the extracellular medium, which can activate the respective receptors and self-perpetuate the phenotype via an autocrine mechanism [9]. To our knowledge, this is the first evidence that TGF-β2 is the main isoform secreted by CF and CMF. In light of our finding that these cells secrete high levels of TGF-β2, we suggest that this isoform may be key in maintaining the cardiac myofibroblast phenotype, possibly serving as a target for inducing balanced α-SMA mRNA and protein expression. Indeed, TGF-β1 and TGF-β2 induce CF-to-CMF differentiation in vivo and in vitro, whereas TGF-β3 acts as a negative regulator of myofibroblastic phenotype in vivo but not in vitro. Thus, while the behavior of the three different TGF-β isoforms is similar in vitro, TGF-β isoforms may play different, but complementary, roles in vivo in myofibroblast modulation during wound repair [33]. Further evidence from the literature is consistent with these findings on TGF-β isoform secretion. In the rat heart, adrenergic stimulation [4] and coronary artery ligation [10] alter cardiac TGF-β isoform expression patterns, with increased secretion of TGF-β2 over TGF-β1. On the other hand, LPS reduces secretion of TGF-β2 and 3, but not TGF-β1, in CMF, whereas this effect was not significant in CF. There is parallel data available on the effects of LPS on TGF-β secretion. In human articular chondrocytes, LPS selectively decreases expression of TGF-β2 and 3, but not TGF-β1 [2]. In this sense, some authors argue that LPS sensitizes TGF-β-mediated actions [3], whereas another report indicates that LPS desensitizes cytokine-mediated actions [32]. This effect appears to be dependent on cell type. This finding suggests that in CMF, LPS reduces the release of TGF-β isoforms, possibly inducing a negative effect on healing process, where CMF play a fundamental role. Thus, in our model we cannot discard that probably the sum of three different isoforms (total secreted TGF-βs) can be responsible of observed effects.
TLR4 Activation by LPS Inhibit α-SMA Expression
The cultured CF showed time-dependent increases in α-SMA expression levels. The literature suggests that TGF-β isoforms secreted into the culture medium act via an autocrine mechanism to induce α-SMA expression. Our results confirm this idea, as CMF incubated with SB431542 (a TGF-β1R antagonist) showed decreased α-SMA levels, whereas TAK-242 did not affect α-SMA levels. The LPS-induced decrease in α-SMA expression suggests that TLR4 activation can inhibit fibroblasts differentiation into myofibroblasts. These data are consistent with the literature, which provides evidence that in vascular smooth muscle cells derived from human aorta, human coronary artery, or rat aorta, LPS stimulation inhibits production of α-SMA triggered by endothelin-1 (ET1) and TGF-β1. This inhibition occurs at a transcriptional level, since LPS inhibits α-SMA mRNA and promoter activity [32, 38]. The model mentioned above postulates that the α-SMA promoter is controlled largely by regulatory elements (such as CArG boxes), activated serum response factors (SRF), and TGF-β control elements (TCE). The authors showed that LPS is unable to alter SRF activity but potently inhibits inducible TCE activity. In contrast, in a sepsis model using human CF, LPS significantly increased α-SMA levels [39], indicating that the effect of LPS on cardiac tissue may be dependent on the animal model and cell type used.
TLR4 Activation Through PI3K/Akt Decreases α-SMA Expression in CF
In this study, LPS acted via TLR4 to trigger the ERK1/2, PI3K/Akt, and NF-κβ signaling pathways in the CF, with activation kinetics comparable to data in the literature [34, 43]. We also found that the ERK1/2 intracellular signaling pathway did not participate in decreasing α-SMA expression. However, our results demonstrate that LY294002 is capable of reversing the effect of LPS-induced TLR4 activation, suggesting that PI3K/Akt intracellular signaling cascade activation is related to decreased α-SMA expression levels. Abdalla et al. demonstrated that in rat embryo fibroblasts, TGF-β1 actives Akt1 and induce α-SMA synthesis through transcription factors such as SRF and myocardin, suggesting that Akt1 is an important modulator of CF-to-CMF differentiation [1]; however, we showed here that LPS operates via the TLR4/Akt signaling pathway to decrease α-SMA protein levels. In addition, the NF-κβ inhibitor alone reduced α-SMA levels, and there was no synergic effect between NF-κβ inhibitor (BAY 11-7082) and LPS. Therefore, although LPS activates NF-κβ, our results cannot allow us to determine whether this signaling pathway is involved in the decreased α-SMA expression triggered by LPS. Future studies to elucidate the participation of NF-κβ in LPS-induced α-SMA decreases would be worthwhile.
LPS Interrupts the TGF-β1 Signaling Pathway
When TGF-β1 binds to its receptor, the canonical (Smad proteins) and non-canonical (MAPK) intracellular pathways are activated [12, 13, 42]. In CF, Smad proteins, particularly Smad3, regulate pro-fibrogenic responses and CMF differentiation [25], whereas Smad7 is associated with a negative feedback loop that halts or reduces the intensity of a signal [46]. Pre-treating the CF with LPS resulted in lower p-Smad3 but higher Smad7 protein levels as compared to CF treated only with TGF-β1. Taken together, these results suggest that LPS-induced TLR4 activation inhibits the TGF-β1 signaling pathways mediated by Smad proteins, leading to decreased expression of α-SMA and secondly, that increased Smad7 levels pose an obstacle to TGF-β1R activation. Data from our laboratory have shown that TGF-β1-induced activation of Smad2/3 in CF regulates collagen secretion and cardiac myofibroblast differentiation (as evidenced by increased α-SMA). Furthermore, the increased Smad7 levels in CF treated with LPS may be related to decrease TGF-β1 signaling, via receptor internalization and promotion of degradation. Ebisawa et al. showed that Smad7 interacts with Smurf1, an E3 ubiquitin ligase, which induces Smad7 ubiquitination and translocation to the cytoplasm [15]. This recruitment of Smad7 to Smurf1 facilitates binding and rapid degradation of the TGF-β1R. These results demonstrate a new role for Smad7 in inducing TGF-βR degradation, through recruitment of an E3 ligase receptor [22]. Moreover, Hayashi et al. [20] showed that Smad7 in the cytosol can bind to TGF-βR directly or in a ternary complex with BAMBI (BMP and activin membrane-bound inhibitor) to inhibit TGF-β1 signaling [46]. Other studies have shown that Smad7 inhibits TGF-β through multiple mechanisms [47]. At the core, Smad7 can undergo epigenetic changes after binding to histone deacetylases (HDAC) such as HDAC1, SIRT1, and P300 acetyltransferase [19, 23]. It can also block target gene induction by interfering with the binding of Smads to activating promoters [48]. Likewise, Conery et al. and Remy et al. showed that activated Akt interacts directly with non-phosphorylated Smad3, sequestering it outside the core and preventing its phosphorylation and nuclear translocation [7, 31]. This results in the inhibition triggered by TGF-β- and Smad3-mediated effects.
In CMF, LPS Reduces α-SMA Expression
Similar to the results in CF, LPS reduced α-SMA expression in CMF, and this effect was blocked by TAK-242, indicating the involvement of TLR4. We hypothesize that this process is carried out through the same mechanisms described above, suggesting that in CF, LPS-induced TLR4 activation may modulate TCE activity, leading to altered TGF-β1 stimulation and diminished α-SMA expression.
In conclusion LPS-induced TLR4 activation inhibits cardiac fibroblast-to-myofibroblast differentiation. We also propose that in CF, LPS-induced TLR4 activation inhibits TGF-β1 signaling, characterized by decreased p-Smad3 but increased Smad7 protein levels. The foregoing suggests that TLR activation by LPS in CF has a double-edged consequence; its anti-fibrotic effect may be beneficial, if used to slow cardiac fibrosis through pharmacological manipulation, or detrimental, impeding normal healing after cardiac injury.
Clinical Significance
The development of TLR4 receptor agonists could represent a promising pharmaceutical drug, which when used in defined time windows could ensure correct scar formation without leading to the development of cardiac fibrosis. CF-to-CMF differentiation is a key process necessary for proper cardiac repair after tissue damage. The early use of TLR4 agonists to avoid or prevent CF differentiation in the healing process, since it leads to an improper wound healing and consequently decreased heart function. In this regard, the use of TLR4 agonists in later stages of cardiac repair could avoid cardiac fibrosis development due to a decrease in the excessive extracellular matrix deposition by CMF.
Limitations
This study was performed under in vitro conditions, which only studies the effect of LPS in a single cell type. However, it should be noted that cardiac tissue is comprised of several cell types: cardiomyocytes, vascular, and endothelial cells, which may also respond to a stimulus like LPS as a TLR4 agonist. Moreover, the presence of this receptor in immune cells that extravasate to cardiac tissue after injury makes it even more complex to study whether these effects on CF-to-CMF equilibrium take place under in vivo conditions.
References
Abdalla, M., Goc, A., Segar, L., & Somanath, P. (2013). Response factor differentiation via myocardin and serum expression and myofibroblast Akt1 mediates alpha-smooth muscle actin. Journal of Biological Chemistry, 288(46), 33483–33493. PubMed PMID: 24106278. PubMed Central PMCID: PMC3829193.
Ayache, N., Boumediene, K., Mathy-Hartert, M., Reginster, J. Y., Henrotin, Y., & Pujol, J. P. (2002). Expression of TGF-betas and their receptors is differentially modulated by reactive oxygen species and nitric oxide in human articular chondrocytes. Osteoarthritis Cartilage, 10, 344–352. PubMed PMID: 12027535.
Bhattacharyya, S., Kelley, K., Melichian, D. S., Tamaki, Z., Fang, F., Su, Y., et al. (2013). Toll-like receptor 4 signaling augments transforming growth factor-β responses: a novel mechanism for maintaining and amplifying fibrosis in scleroderma. American Journal of Pathology, 182, 192–205.
Briest, W., Homagk, L., Rassler, B., Ziegelhöffer-Mihalovicová, B., Meier, H., Tannapfel, A., et al. (2004). Norepinephrine-induced changes in cardiac transforming growth factor-beta isoform expression pattern of female and male rats. Hypertension, 44(4), 410–418. PubMed PMID: 15326086.
Brown, R. D., Ambler, S. K., Mitchell, M. D., & Long, C. S. (2005). The cardiac fibroblast: therapeutic target in myocardial remodeling and failure. Annual Review of Pharmacology and Toxicology, 45, 657–687. PubMed PMID: 15822192.
Chen, T., Guo, J., Han, C., Yang, M., & Cao, X. (2009). Heat shock protein 70, released from heat-stressed tumor cells, initiates antitumor immunity by inducing tumor cell chemokine production and activating dendritic cells via TLR4 pathway. Journal of Immunology, 182(3), 1449–1459. PubMed PMID: 19155492.
Conery, A. R., Cao, Y., Thompson, E. A., Townsend, C. M., Jr., Ko, T. C., & Luo, K. (2004). Akt interacts directly with Smad3 to regulate the sensitivity to TGF-beta induced apoptosis. Nature Cell Biology, 6(4), 366–372. PubMed PMID: 15104092.
Copaja, M., Venegas, D., Aránguiz, P., Canales, J., Vivar, R., Catalán, M., et al. (2011). Simvastatin induces apoptosis by a Rho-dependent mechanism in cultured cardiac fibroblasts and myofibroblasts. Toxicology and Applied Pharmacology, 255(1), 57–64. PubMed PMID: 21651924.
Dabiri, G., Campaner, A., Morgan, J. R., & Van De Water, L. (2006). A TGF-beta1-dependent autocrine loop regulates the structure of focal adhesions in hypertrophic scar fibroblasts. Journal of Investigative Dermatology, 126(5), 963–970. PubMed PMID: 16498397.
Deten, A., Hölzl, A., Leicht, M., Barth, W., & Zimmer, H. G. (2001). Changes in extracellular matrix and in transforming growth factor beta isoforms after coronary artery ligation in rats. Journal of Molecular and Cellular Cardiology, 33, 1191–1207. PubMed PMID: 11444923.
Díaz-Araya, G., Vivar, R., Humeres, C., Boza, P., Bolívar, S., & Muñoz, C. (2015). Cardiac fibroblasts as sentinel cells in cardiac tissue: Receptors, signaling pathways and cellular functions. Pharmacological Research, 101, 30–40. PubMed PMID: 26151416.
Dobaczewski, M., Bujak, M., Li, N., Gonzalez-Quesada, C., Mendoza, L. H., Wang, X. F., et al. (2010). Smad3 signaling critically regulates fibroblast phenotype and function in healing myocardial infarction. Circulation Research, 107, 418–428. PubMed PMID: 20522804. PubMed Central PMCID: PMC2917472.
Dobaczewski, M., Gonzalez-Quesada, C., & Frangogiannis, N. G. (2010). The extracellular matrix as a modulator of the inflammatory and reparative response following myocardial infarction. Journal of Molecular and Cellular Cardiology, 48, 504–511. PubMed PMID: 19631653. PubMed Central PMCID: PMC2824059.
Dong, R. Q., Wang, Z. F., Zhao, C., Gu, H. R., Hu, Z. W., Xie, J., et al. (2015). Toll-like receptor 4 knockout protects against isoproterenol-induced cardiac fibrosis: The role of autophagy. Journal of Cardiovascular Pharmacology and Therapeutics, 20(1), 84–92. PubMed PMID: 24950765.
Ebisawa, T., Fukuchi, M., Murakami, G., Chiba, T., Tanaka, K., Imamura, T., et al. (2001). Smurf1 interacts with transforming growth factor-β type I receptor through Smad7 and induces receptor degradation. Journal of Biological Chemistry, 276, 12477–12480. PubMed PMID: 11278251.
Fan, D., Takawale, A., Lee, J., & Kassiri, Z. (2012). Cardiac fibroblasts, fibrosis and extracellular matrix remodeling in heart disease. Fibrogenesis Tissue Repair, 5(1), 15. PubMed PMID: 22943504. PubMed Central PMCID: PMC3464725.
Fang, H., Ang, B., Xu, X., Huang, X., Wu, Y., Sun, Y., et al. (2014). TLR4 is essential for dendritic cell activation and anti-tumor T-cell response enhancement by DAMPs released from chemically stressed cancer cells. Cellular and Molecular Immunology, 11(2), 150–159. PubMed PMID: 24362470. PubMed Central PMCID: PMC4003380.
Goodall, K. J., Poon, I. K., Phipps, S., & Hulett, M. D. (2014). Soluble heparan sulfate fragments generated by heparanase trigger the release of pro-inflammatory cytokines through TLR-4. PLoS One, 9(10), e109596.
Gronroos, E., Hellman, U., Heldin, C. H., & Ericsson, J. (2002). Control of Smad7 stability by competition between acetylation and ubiquitination. Molecular Cell, 10, 483–493. PubMed PMID: 12408818.
Hayashi, H., Abdollah, S., Qiu, Y., Cai, J., Xu, Y. Y., Grinnell, B. W., et al. (1997). The MAD-related protein Smad7 associates with the TGF-β receptor and functions as an antagonist of TGF-β signaling. Cell, 89, 1165–1173. PubMed PMID: 9215638.
He, Z., Gao, Y., Deng, Y., Li, W., Chen, Y., Xing, S., et al. (2012). Lipopolysaccharide induces lung fibroblast proliferation through Toll-like receptor 4 signaling and the phosphoinositide3-kinase-Akt pathway. PLoS ONE, 7(4), e35926. PubMed PMID: 22563417. PubMed Central PMCID: PMC3338545..
Kavsak, P., Rasmussen, R. K., Causing, C. G., Bonni, S., Zhu, H., Thomsen, G. H., et al. (2000). Smad7 binds to Smurf2 to form an E3 ubiquitin ligase that targets the TGF-β receptor for degradation. Molecular Cell, 6, 1365–1375. PubMed PMID: 11163210.
Kume, S., Haneda, M., Kanasaki, K., Sugimoto, T., Araki, S., Isshiki, K., et al. (2007). SIRT1 inhibits transforming growth factor β-induced apoptosis in glomerular mesangial cells via Smad7 deacetylation. Journal of Biological Chemistry, 282, 151–158. PubMed PMID: 17098745.
Lew, W. Y., Bayna, E., Dalle Molle, E., Contu, R., Condorelli, G., & Tang, T. (2014). Myocardial fibrosis induced by exposure to subclinical lipopolysaccharide is associated with decreased miR-29c and enhanced NOX2 expression in mice. PLoS ONE, 9(9), e107556R.D.
Li, P., Wang, D., Lucas, J., Oparil, S., Xing, D., Cao, X., et al. (2008). Atrial natriuretic peptide inhibits transforming growth factor beta-induced Smad signaling and myofibroblast transformation in mouse cardiac fibroblasts. Circulation Research, 102, 185–192. PubMed PMID: 17991884.
Yu, L., Wang, L., & Chen, S. (2010). Endogenous toll-like receptor ligands and their biological significance. Journal of Cellular Molecular Medicine, 14(11), 2592–2603. PMCID: PMC4373479.
Massagué, J. (1990). The transforming growth factor-beta family. Annual Review of Cell Biology, 6, 597–641. PubMed PMID: 2177343.
Okamura, Y., Watari, M., Jerud, E. S., Young, D. W., Ishizaka, S. T., Rose, J., et al. (2001). The extra domain A of fibronectin activates Toll-like receptor 4. Journal of Biological Chemistry, 276(13), 10229–10233. PubMed PMID: 11150311.
Peri, F., & Calabrese, V. (2014). Toll-like receptor 4 (TLR4) modulation by synthetic and natural compounds: an update. Journal of Medicinal Chemistry, 57(9), 3612–3622. PubMed PMID: 24188011. PubMed Central PMCID: PMC4040398.
Tavener, S. A., & Kubes, P. (2005). Is there a role for cardiomyocyte toll-like receptor 4 in endotoxemia? Trends in Cardiovascular Medicine, 15(5), 153–157. PubMed PMID: 16165010.
Remy, I., Montmarquette, A., & Michnick, S. W. (2004). PKB/Akt modulates TGF-beta signaling through a direct interaction with Smad3. Nature Cell Biology, 6(4), 358–365. PubMed PMID: 15048128.
Sandbo, N., Taurin, S., Yau, D. M., Kregel, S., Mitchell, R., & Dulin, N. O. (2007). Downregulation of smooth muscle alpha-actin expression by bacterial lipopolysaccharide. Cardiovascular Research, 74(2), 262–269. PubMed PMID: 17303098.
Serini, G., & Gabbiani, G. (1996). Modulation of alpha-smooth muscle actin expression in fibroblasts by transforming growth factor-beta isoforms: An in vivo and in vitro study. Wound Repair Regen, 4, 278–287. PubMed PMID: 17177825.
Stawowy, P., Goetze, S., Margeta, C., Fleck, E., & Graf, K. (2003). LPS regulate ERK1/2-dependent signaling in cardiac fibroblasts via PKC-mediated MKP-1 induction. Biochemical and Biophysical Research Communications, 303, 74–80. PubMed PMID: 12646169.
Sugiura, H., Ichikawa, T., Koarai, A., Yanagisawa, S., Minakata, Y., Matsunaga, K., et al. (2009). Activation of Toll-like receptor 3 augments myofibroblast differentiation. American Journal of Respiratory Cell and Molecular Biology, 40(6), 654–662. PubMed PMID: 18988918.
Tiede, K., Stöter, K., Petrik, C., Chen, W. B., Ungefroren, H., Kruse, M. L., et al. (2003). Angiotensin II AT (1)-receptor induces biglycan in neonatal cardiac fibroblasts via autocrine release of TGF-β in vitro. Cardiovascular Research, 60(3), 538–546.
Timmers, L., Sluijter, J. P., van Keulen, J. K., Hoefer, I. E., Nederhoff, M. G., Goumans, M. J., et al. (2008). Toll-like receptor 4 mediates maladaptive left ventricular remodeling and impairs cardiac function after myocardial infarction. Circulation Research, 102(2), 257–264. PubMed PMID: 18007026.
Tomasek, J., McRae, J., Owens, G., & Haaksma, C. (2005). Regulation of α-Smooth Muscle Actin Expression in Granulation Tissue Myofibroblasts Is Dependent on the Intronic CArG Element and the Transforming Growth Factor-β1 Control Element. American Journal of Pathology, 166(5), 1343–1351. PubMed PMID: 15855636. PubMed Central PMCID: PMC1606390.
Tomita, K., Takashina, M., Mizuno, N., Sakata, K., Hattori, K., Imura, J., et al. (2015). Cardiac fibroblasts: Contributory role in septic cardiac dysfunction. Journal of Surgical Research, 193(2), 874–887.
Turner, N. A., & Porter, K. E. (2013). Function and fate of myofibroblasts after myocardial infarction. Fibrogenesis Tissue Repair, 6(1), 5. PubMed PMID: 23448358. PubMed Central PMCID: PMC3599637.
Uematsu, S., & Akira, S. (2008). Toll-like receptors and innate inmunity. Handbook of Experimental Pharmacology, 183, 1–21. PubMed PMID: 18071652.
Vivar, R., Humeres, C., Varela, M., Ayala, P., Guzmán, N., Olmedo, I., et al. (2011). Cardiac fibroblast death by ischemia/reperfusion is partially inhibited by IGF-1 through both PI3 K/Akt and MEK-ERK pathways. Experimental and Molecular Pathology, 93(1), 1–7. PubMed PMID: 22537549.
Verstrepen, L., Bekaert, T., Chau, T. L., Tavernier, J., Chariot, A., & Beyaert, R. (2008). TLR-4, IL-1R and TNF-R signaling to NF-kappaβ: Variations on a common theme. Cellular and Molecular Life Sciences, 65, 2964–2978. PubMed PMID: 18535784.
Webber, J., Meran, S., Steadman, R., & Phillips, A. (2009). Hyaluronan orchestrates transforming growth factor-beta1-dependent maintenance of myofibroblast phenotype. Journal of Biological Chemistry, 284(14), 9083–9092. PubMed PMID: 19193641. PubMed Central PMCID: PMC2666557.
Weber, K. T. (2004). Fibrosis in hypertensive heart disease: Focus on cardiac fibroblasts. Journal of Hypertension, 22(1), 47–50. PubMed PMID: 15106793.
Yan, X., Lin, Z., Chen, F., Zhao, X., Chen, H., Ning, Y., et al. (2009). Human BAMBI cooperates with Smad7 to inhibit transforming growth factor-β signaling. Journal of Biological Chemistry, 284, 30097–30104. PubMed PMID: 19758997; PubMed Central PMCID: PMC2781564.
Yoshida, K., & Matsuzaki, K. (2012). Differential regulation of TGF-β/Smad signaling in hepatic stellate cells between acute and chronic liver injuries. Front Physiol, 3, 53. PubMed PMID: 22457652. PubMed Central PMCID: PMC3307138.
Zhang, S., Fei, T., Zhang, L., Zhang, R., Chen, F., Ning, Y., et al. (2007). Smad7 antagonizes transforming growth factor-β signaling in the nucleus by interfering with functional Smad-DNA complex formation. Molecular and Cellular Biology, 27, 4488–4499.
Zeuke, S., Ulmer, A. J., Kusumoto, S., Katus, H. A., & Heine, H. (2002). TLR4-mediated inflammatory activation of human coronary artery endothelial cells by LPS. Cardiovascular Research, 56(1), 126–134. PubMed PMID: 12237173.
Acknowledgements
This work was supported by FONDECYT (Grant 1130300 to G. Díaz-Araya) and CONICYT (Grant 63130233 to S Bolivar).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bolívar, S., Santana, R., Ayala, P. et al. Lipopolysaccharide Activates Toll-Like Receptor 4 and Prevents Cardiac Fibroblast-to-Myofibroblast Differentiation. Cardiovasc Toxicol 17, 458–470 (2017). https://doi.org/10.1007/s12012-017-9404-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12012-017-9404-4