Abstract
The standard of salt iodine content in China has been adjusted several times since implementation of the universal salt iodization (USI) in 1995. The new standard of iodized salt content was adjusted from 35 ± 15 to 30 ± 9 mg/kg in Henan province in 2012. We aimed to determine whether the vulnerable populations were iodine sufficient after the adjustment of salt iodine content and to provide a guideline for the adjustment of USI policy in China. Two cross-sectional surveys of iodine status in vulnerable populations, including reproductive-age, pregnant and lactating women, infants <2 years, and children aged 8–10 years, were conducted in Henan province in 2013 and 2014. In 2013, the median urinary iodine concentration (mUIC) of reproductive-age women was 200.1 μg/L and that of school children aged 8–10 years was 221.0 μg/L. These mUICs were considered as “more than adequate.” The mUICs of reproductive-age women and school children in 2014 showed a significant decline compared to the mUICs in 2013 (P = 0.012 and P = 0.001, respectively). The mUICs of the pregnant women were 204.2 μg/L in 2013 and 202.5 μg/L in 2014, which both met the requirement level recommended by WHO. In 2013, the mUIC of lactating women was 169.1 μg/L and that of infants <2 years was 203.2 μg/L, which were significantly lower than that of 2014 (P < 0.001 and P < 0.001, respectively). The lactating women and infants in 2013 and 2014 were both regarded as “iodine adequate.” Iodine status of the vulnerable populations is still adequate as a whole in Henan province after decreasing the salt iodine content. However, the mUIC of school children aged 8–10 years is slightly above the adequate level. To reduce the risk of iodine excess in the general population and prevent the possibility of iodine deficiency of the vulnerable population, it is necessary to explore the appropriate level of iodized salt content.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Iodine deficiency disorders (IDDs) refer to a spectrum of adverse effects of iodine deficiency on growth and development in humans and animals [1, 2], including endemic goiter, cretinism, spontaneous abortion, stillbirth, birth defects, and brain damage. To eliminate IDDs, salt iodization is regarded as a safe and cost-effective method because salt is consumed by most people at constant levels and the cost of salt iodization is low [3]. Universal salt iodization (USI) was recommended by the World Health Organization (WHO) in 1994, providing that all food for humans and animals should be iodized by iodized salt. By 2006, almost 120 countries have adopted salt iodization programs [4]. From 1990 to 2007, global household coverage rates with iodized salt increased from 20 to 70 % [4]. The number of iodine-deficient countries decreased from 110 in 1993 to 32 in 2011 [5].
The correlation between the level of iodine intake and the incidence of thyroid disease is a U-shaped curve [6]. Insufficient or excess iodine intakes may increase the occurrence of thyroid disease. The introduction of USI may increase the risk of iodine-induced hyperthyroidism, hypothyroidism, autoimmune thyroiditis, etc. [7]. Therefore, an optimal level of salt iodine is crucial both to prevent IDD and to avoid side effects caused by iodine excess. The iodized salt level is 20–40 mg/kg recommended by WHO, 15–25 mg/kg in Germany, 20 mg/kg in Australia, and 25 mg/kg in Switzerland [8].
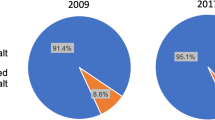
To prevent and control IDD, China adopted the USI policy in 1995. The USI policy has been successful and effective. In 2000, the stage goal of IDD elimination was achieved in most provinces of China. According to the national IDD surveillance data, household coverage rates with iodized salt increased from 39.9 to 95.3 %, and goiter rates of children aged 8–10 years decreased from 20.4 to 2.5 % between 1995 and 2011, respectively [9]. However, iodine concentration of table salt was excessive, and median urinary iodine content of children exceeded the adequate range recommended by WHO (100–200 μg/L) [10]. In fact, the standard iodine content in table salt was adjusted several times from 1995 to 2012. Initially, the standard salt iodine content only included a lower limit (≥20 mg/kg). In 1997, an upper limit (≤60 mg/kg) was included in the standard. The national IDD survey in 1999 showed that median urinary iodine concentrations (mUICs) in 14 provinces exceeded 300 μg/L and median salt iodine concentrations of 24 provinces were above 40 mg/kg. Based on these data, the iodine content in table salt was adjusted from 20–60 mg/kg to 20–50 mg/kg in 2000. The recent national survey in 2011 showed that iodine status in the general population in China was still above the sufficient level. Therefore, a new standard of salt iodine content (20, 25, or 30 ± 30 % mg/kg) has been implemented since 2012, and each province has selected its own level of salt iodine content.
Henan province had significant numbers of individuals with iodine deficiency. In the early 1950s, prevalence rates of endemic goiter and cretinism had reached 50.0 and 11.0 % in some mountainous areas, respectively. Potassium iodide pills, 0.66 % iodine tincture, kelp injections, and other iodine-fortified supplements were used to prevent and control IDD. It was not until 1970s that iodized salt was adopted as the prophylaxis of IDD but only in some pilot counties. Before introducing the USI policy, goiter rate was 17.8 % and mUIC was 76.0 μg/L in children aged 7–14 years in Henan province, based on provincial survey in 1994. In the latest national survey of 2011, the goiter rate decreased to 4.5 % and the mUIC increased to 201 μg/L [11]. Therefore, we selected 30 ± 9 mg/kg as the new iodized salt standard in Henan province in 2012. Routine iodine nutritional surveys are usually conducted in school children. Few studies have been done on high-risk populations, for example, reproductive-age, pregnant and lactating women, and infants [5]. To reflect the changes of iodine status before and after the adjustment of salt iodine content, a continuous surveillance of iodine status of five groups of vulnerable populations, including reproductive-age, pregnant and lactating women, infants <2 years, and children aged 8–10 years, was conducted in Henan province of China from 2011 to 2014. Based on surveys conducted in 2013 and 2014 in Henan province, this paper mainly describes iodine status of vulnerable populations after the implementation of a new standard of salt iodine content.
Methods
Participants
Two cross-sectional surveys of iodine status in vulnerable populations were conducted in Henan province in 2013 and 2014. The vulnerable populations included reproductive-age, pregnant and lactating women, infants <2 years, and children aged 8–10 years using a multistage sampling design for each survey. The sampling method was detailed in our previous study [12]. For women and infants, a county was first selected from each city; secondly, a maternal and children’s hospital or obstetric clinic was selected from each chosen county; finally, no less than 200 women or infants were selected from each chosen hospital or clinic. For children aged 8–10, a county was also chosen in the first stage; two or three primary schools (according to the school size) were then selected from each chosen county, no less than 200 children were finally enrolled from each chosen school (Fig. 1).
All subjects were required to live in investigated regions for more than 1 year. Those who had no health problems or thyroid diseases were enrolled. The water iodine content in each of the investigated regions was less than 100 μg/L. All participants, including women, infants, and children, were asked to provide urine samples and socioeconomic information. In addition, mothers of infants provided feeding practices.
Measurement of Urinary Iodine
The same measurement methods and equipments were used for the two surveys. A 10-ml midstream urine sample was collected from each participant in the morning according to the instruction of a health care professional. The participants were required to avoid consuming iodine-enriched foods before sampling. These samples were sealed in plastic bottle and delivered to local CDC laboratories. Urinary iodine was measured by the acid digestion method (As3+-Ce4+ catalytic spectrophotometry) [13]. The external and internal quality control of urinary iodine was provided by China National CDC. The coefficient of variation for UIC was 2.0 % at 68.2 ± 1.3 μg/L and 0.9 % at 193.0 ± 10.0 μg/L.
Evaluation Criteria for Iodine Status in Vulnerable Populations
The evaluation criteria of iodine status, as determined by UIC, recommended by WHO is as follows: for reproductive-age women and children, <100 μg/L is deficient, 100–199 μg/L is adequate, 200–299 μg/L is more than adequate, and ≥300 μg/L is excessive; for pregnant women, <150 μg/L is deficient, 150–249 μg/L is adequate, 250–499 μg/L is more than adequate, and ≥500 μg/L is excessive; for lactating women and infant <2 years, <100 μg/L is deficient and ≥100 μg/L is adequate [14].
Statistical Analysis
Data management and analyses were performed with EXCEL and SPSS 17.0. Normally distributed data was expressed as mean ± SD. Group differences of normally distributed data were tested by t test and ANOVA. As UIC distribution was non-normally distributed; it was expressed as median and interquartile ranges. Median values of UIC were presented by year and by type of vulnerable populations. Non-parametric tests, including Mann-Whitney U test or Kruskal-Wallis H test, were performed to compare group differences of UIC. The level of significance was set at p < 0.05.
Ethics
The medical ethics committee of Henan provincial CDC approved the survey. Written informed consent was obtained from all participants or parents of infants and children.
Results
Table 1 presents the characteristics and iodine status of five groups of vulnerable populations in 2013 and 2014 survey. 66,446 and 74,015 subjects were enrolled in 2013 and 2014 surveys, respectively. Ages of reproductive-age, pregnant and lactating women, and school children aged 8–10 years were not significantly different between 2013 and 2014 surveys. Mean age of infants in 2014 was slightly less than infants in 2013 (p < 0.01).
In 2013, the mUIC of reproductive-age women was 200.1 μg/L and that of school children aged 8–10 years was 221.0 μg/L. According to the WHO criterion for the general population, they were considered as “more than adequate.” The mUICs of the two groups in 2014 showed a significant decline compared to the mUICs in 2013 (p = 0.012 and p = 0.001, respectively). But the mUIC of school children aged 8–10 years in 2014 was still greater than iodine sufficient level recommended by WHO (100–199 μg/L). The mUICs of pregnant women were 204.2 μg/L in 2013 and 202.5 μg/L in 2014, both of which met the requirement level recommended by WHO (150–249 μg/L). The mUICs of lactating women and infants <2 years in 2013 were 169.1 and 203.2 μg/L, respectively, which were significantly less than those observed in 2014 (174.8 and 217.9 μg/L; p < 0.001 and p < 0.001, respectively). The lactating women and infants were regarded as “adequate” in both 2013 and 2014.
The mUICs in the most vulnerable populations declined from 2013 to 2014, after stratifying by urban and rural areas (Fig. 2). Nevertheless, the mUICs of lactating women in 2013 were increased compared with lactating women in 2014, both living in urban (p = 0.004) and rural areas (p < 0.001); infants <2 years of age living in rural areas in 2013 had an increased mUIC compared with 2014.
Change in mUIC of the vulnerable populations from 2013 to 2014 stratified by urban and rural areas. In the urban area, the mUICs of pregnant women, infant <2 years, and school children aged 8–10 in 2013 were significantly greater than that in 2014; however, the mUICs of lactating women in 2013 were significantly less than that in 2014. In the rural area, the mUICs of reproductive-age and pregnant women in 2013 were significantly greater than that in 2014; however, the lactating women and infants <2 years of age in 2013 had a decreased mUIC comparing to year 2014. mUIC median urinary iodine concentration. *Significant differences between groups: p < 0.05
Reproductive-age women living in urban areas had decreased mUICs than reproductive-age women living in rural areas in both 2013 (p = 0.004) and 2014 (p = 0.329). There were significant differences in mUICs of pregnant women between urban and rural areas in both 2013 (p < 0.001) and 2014 (p < 0.001). However, the mUICs between urban and rural lactating women were not significantly different in both 2013 (p = 0.891) and 2014 (p = 0.638). The mUICs of school children aged 8–10 years living in urban areas were 217.0 μg/L in 2013 and 187.0 μg/L in 2014, significantly less than rural school children only in 2014 (p < 0.001). In addition, the difference of mUIC between urban and rural infants was opposite direction between 2013 and 2014 survey.
As shown in Table 2, the mUICs of pregnant women in the second and third trimesters were stable between 2013 and 2014 (p > 0.05). The mUICs of pregnant women in the first trimester decreased significantly from 203.1 μg/L in 2013 to 191.4 μg/L in 2014 (p < 0.001). The mUICs of pregnant women in the third trimester were significantly greater than in the first and second trimesters, both in 2013 and 2014 survey (p < 0.001).
As shown in Table 3, the mUICs of school children aged 8 and 9 years decreased significantly from 2013 to 2014 (p < 0.01), while the mUIC of children aged 10 years did not change over the same period (p > 0.05). The mUIC of school children failed to reach statistical significance in 2013 survey, whereas they were significantly different among the three age groups in 2014 survey.
2020 parents of infants <1 year provided information about their feeding patterns. Figure 3 shows the differences in mUIC of infants <1 year between different feeding patterns. About 67 % of infants <1 year were being breast-fed, and their mUIC (246.8 μg/L) was greater than formula-fed infants (194.3 μg/L) (P < 0.001) and mixed-fed infants (234.7 μg/L) (P < 0.001). The formula-feeding patterns included domestic formula milk, imported formula milk, and home-prepared foods. There was no significant difference in mUIC between the three groups.
Differences in mUIC of infants <1 years between different feeding patterns. The numbers of infants <1 year receiving breast feeding, formula feeding, and mixed-feeding were 1364, 200, and 456, respectively. Among them, the artificial-feeding patterns included domestic formula milk, imported formula milk, and home-prepared foods. mUIC median urinary iodine concentration. **Significant differences between groups: p < 0.001
Discussion
In 2012, the salt iodine content was adjusted from 35 ± 15 to 30 ± 9 mg/kg in Henan province. Our data indicated that the iodine status of pregnant women, lactating women, and infants reached the recommended value in both 2013 and 2014 after the implementation of a new standard of salt iodine content. The mUICs of school children aged 8–10 years were above the adequate level in both 2013 and 2014. The mUIC of reproductive-age women in 2014 fell to the normal level (100–199 μg/L). Compared with data before adjustment of salt iodine content [12, 15], the mUICs in pregnant women, lactating women, infants, and school children increased slightly from 2011 to 2014. Nevertheless, the mUIC in reproductive-age women decreased from 204.5 μg/L in 2011 to 195.0 μg/L in 2014. These results suggest that iodine status of vulnerable populations did not noticeably decline as expected after decreasing salt iodine content. The main reason for these values is that the salt iodine content in Henan province decreased slowly after implementation of new salt iodine content (the median salt iodine contents were 28.6 mg/kg in 2011 and 26.8 mg/kg in 2014). Another reason is that iodized salt is not the only source of dietary iodine. A similar study in Zhejiang province of China found that the mUIC of school children aged 8–10 years significantly decreased from 237.1 μg/L in 2011 to 174.3 μg/L in 2013, which was inconsistent with our results [16]. After adjustment of salt iodine content in 2012, three levels were recommended to each province to choose, 20, 25, or 30 ± 30 % mg/kg, respectively. Our province selected 30 ± 30 % mg/kg as our new salt iodine criterion, which was higher than that of Zhejiang province (25 ± 30 % mg/kg). The choice may account for the difference.
Our findings showed that vulnerable populations, both in urban and rural areas, were “iodine sufficient.” The UICs were different among the five groups of vulnerable populations, however. The mUICs of reproductive-age women and school children aged 8–10 years in urban areas were decreased compared with rural populations, whereas the mUICs of urban pregnant women were greater than rural pregnant women. Some urban residents are afraid of excess iodine intake and prefer to purchase non-iodized salt [17]. During pregnancy, urban women have greater opportunity to access high-protein food and other nutritional supplements, and have more knowledge about IDD than rural women, which may explain the difference of mUIC between urban and rural pregnant women.
There are a few studies on gestational change of UIC, but their results are conflicting [18–21]. Some studies reported that the mUIC showed a decrease with increasing gestation, while others showed an increase or steady change. The observed differences are governed by the local level of water iodine, sample size, overall iodine status, and thyroid physiology [21, 22]. In the present study, we found that the mUICs of pregnant women increased during gestation and was greatest in the third trimester, both in the 2013 and 2014 surveys. The gestational pattern of UIC is in accordance with previous reports from the USA [23], Hong Kong [24], and Iran [22]. During early gestation, increased concentrations of serum thyroxine-binding globulin (TBG) and the stimulation of thyrotropin (TSH) receptors by human chorionic gonadotropin (HCG) result in increasing thyroid hormone production [25]. Deiodinase in the placenta enhances degradation of thyroid hormone. Furthermore, increased renal iodine clearance and iodine shifting from mother to fetus tend to decrease the circulating plasma iodine concentration. To compensate for increased iodine demand and depletion of total iodine stores during pregnancy, increased thyroidal iodine extraction may explain increased UIC in late gestation [26].
Infant iodine status is dependent on many factors, including feeding pattern, iodine level of formula and food, breast-milk iodine content, and renal function for iodine clearance. In our infants <1 year, the proportion being breast-fed was 67 %, and their mUIC was significantly greater than those formula-fed or mixed-fed. Infants receiving formula had greater UIC than breast-fed infants [27]. These results are contrary to ours, partially due to the greater mUIC in lactating women in this study. On the other hand, we found that mUIC of infants receiving imported formula was greater than infants receiving domestic formula and home-prepared foods, although there was no significant difference. Chinese people are more likely to purchase imported formula because they believe it is beneficial to their babies. Foreign countries, in general, pay particular attention to iodine supplementation of infant formula. For example, infant formula must be fortified with iodine in the USA [28] and Europe [29].
Overall, iodine status of vulnerable populations is still adequate in Henan province after decreasing salt iodine content. However, the mUIC of school children aged 8–10 years is slightly above the adequate level. To reduce the risk of iodine excess in the general population and prevent the possibility of iodine deficiency of the vulnerable population, it is necessary to explore the appropriate level of iodized salt content.
References
Hetzel BS (1983) Iodine deficiency disorders (IDD) and their eradication. Lancet 2:1126–1129
Editorial L (1983) From endemic goiter to iodine deficiency disorders. Lancet 2:1121–1122
Campbell N, Dary O, Cappuccio FP, Neufeld LM, Harding KB, Zimmermann MB (2012) Collaboration to optimize dietary intakes of salt and iodine: a critical but overlooked public health issue. Bull World Health Organ 1:73–74. doi:10.2471/BLT.11.092080
World Health Organization (2007) Assessment of iodine deficiency disorders and monitoring their elimination, 2nd edn. WHO, Geneva
Anderson M, Karumbunathan V, Zimmermann MB (2012) Global iodine status in 2011 and trends over the past decade. J Nutr 4:744–750. doi:10.3945/jn.111.149393
Laurberg P, Bülow Pedersen I, Knudsen N, Ovesen L, Andersen S (2001) Environmental iodine intake affects the type of nonmalignant thyroid disease. Thyroid 5:457–469
Zimmermann MB (2008) Iodine requirements and the risks and benefits of correcting iodine deficiency in populations. J Trace Elem Med Biol 22:81–92
WHO/UNICEF/ICCIDD (1996) Recommended iodine levels in salt and guidelines for monitoring their adequacy and effectiveness WHO/NUT96.13. WHO, Geneva
Shen H (2013) The problems and challenges for China after achieving the national elimination IDD standard. Chin J Prev Med 47:5–7(in Chinese)
Li S, Zheng Q, Xu J, Gorstein J, Wang H, Dong H (2011) Iodine excess or not: analysis on the necessity of reducing the iodine content in edible salt based on the national monitoring results. Asia Pac J Clin Nutr 20:501–506
Zheng H, Li X, Yang J (2013) Investigation on iodine deficiency disoroders status in Henan province. Chin J Endemiol 5:35–37(in Chinese)
Yang J, Zheng H, Li X, Zhu L, Hao Z, Chen G, Wang Y (2014) Assessment of iodine status and associated factors in vulnerable populations in Henan Province, China, in 2012. Asia Pac J Clin Nutr 23:626–633
China’s Ministry of health (2011) GB26878-2011 national food safety standards: iodine content in edible salt. Standards Press of China, Beijing(in Chinese)
UNICEF (2011) The state of the world’s children 2011: adolescence: an age of opportunity. United Nations Children’s fund, New York
Yang J, Zheng H, Chen G (2013) Iodine nutritional status of the vulnerable population in Henan province in 2011. Chin J Prev Med 1:14–17(in Chinese)
Zou Y, Lou X, Ding G, Z M, W Z, G M (2014) Iodine nutritional status after the implementation of the new iodized salt concentration standard in Zhejiang Province, China. BMC Public Health 14:836
Yu J, Liu P, Liu Y, Liu SJ, Sun DJ (2014) Should both iodised and non-iodised salt be made available in Chinese cities? A cross-sectional survey. BMJ Open 4:e005397. doi:10.1136/bmjopen-2014-005397
Stilwell G, Reynolds PJ, Parameswaran V, Blizzard L, Greenaway TM, Burgess JR (2008) The influence of gestational stage on urinary iodine excretion in pregnancy. J Clin Endocrinol Metab 5:1737–1742
Brander L, Als C, Buess H, Haldimann F, Harder M, Hanggi W, Herrmann U, Lauber K, Niederer U (2003) Urinary iodine concentration during pregnancy in an area of unstable dietary iodine intake in Switzerland. J Endocrinol Investig 5:389–396
Elnagar B, Eltom A, Wide L, Gebre-Medhin M, Karlsson FA (1998) Iodine status, thyroid function and pregnancy: study of Swedish and Sudanese women. Eur J Clin Nutr 52:351–355
Fuse Y, Ohashi T, Yamaguchi S, Yamaguchi M, Shishiba Y, Irie M (2011) Iodine status of pregnant and postpartum Japanese women: effect of iodine intake on maternal and neonatal thyroid function in an iodine-sufficient area. J Clin Endocrinol Metab 12:3846–3854. doi:10.1210/jc.2011-2180
Rostami R, Beiranvand A, Khakhali H, Salary S, Aghasi M, Nourooz-Zadeh J (2012) Evaluation of accessibility of iodinated salt and nutritional iodine status during pregnancy. Iran J Public Health 8:56–60
Alvarez-Pedrerol M, Guxens M, Mendez M, Canet Y, Martorell R, Espada M, Plana E, Rebagliato M, Sunyer J (2009) Iodine levels and thyroid hormones in healthy pregnant women and birth weight of their offspring. Eur J Endocrinol 160:423–429
Kung AW, Lao TT, Chau MT, Tam SC, Low LCK (2000) Goitrogenesis during pregnancy and neonatal hypothyroxinaemia in a borderline iodine sufficient area. Clin Endocrinol 53:725–731
Leung AM, Pearce EN, Braverman LE (2011) Iodine nutrition in pregnancy and lactation. Endocrinol Metab Clin N Am 40:765–777. doi:10.1016/j.ecl.2011.08.001
Stilwell G, Reynolds PJ, Parameswaran V, Blizzard L, Greenaway TM, Burgess JR (2008) The influence of gestational stage on urinary iodine excretion in pregnancy. J Clin Endocrinol Metab 93:1737–1742
Andersson M, Aeberli I, Wüst N, Piacenza AM, Bucher T, Henschen I (2010) The Swiss iodized salt program provides adequate iodine for school children and pregnant women, but weaning infants not receiving iodine-containing complementary foods as well as their mothers are iodine deficient. J Clin Endocrinol Metab 95:5217–5224
U.S. Food and Drug Administration (1980) The Federal Food, Drug, and Cosmetic Act (FFDCA), 21U.S.C. §350a, Section 412. (i). Requirements for infant formula. Code of Federal Regulations
Commission of the European Communities (2006) Commission Directive 2006/125/EC of December 5 2006 on processed cereal-based foods and baby foods for infants and young children. Official Journal of the European Union L 339:16–35
Acknowledgments
The authors thank the participating women and infants. We are grateful to the support of all the cooperating municipal- and county-level Centers for Disease Control and Prevention, including Zhengzhou, Kaifeng, Luoyang, Pingdingshan, Jiyuan, Anyang, Hebi, Xinxiang, Jiaozuo, Puyang, Xuchang, Luohe, Shangqiu, Zhoukou, Zhumadian, Nanyang, Xinyang, and Sanmenxia. We also thank all participating colleagues from the above organizations for their hard work. And we are very grateful to Dr. Chun-yu Liu (National Heart, Lung, and Blood Institute’s Framingham Heart Study) for the assistance in revising the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Financial Support
This work was supported by grants from the Public Health transfer trust and the key scientific and technological project of Henan province (142102310390).
Conflicts of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Yang, J., Zhu, L., Li, X. et al. Iodine Status of Vulnerable Populations in Henan Province of China 2013–2014 After the Implementation of the New Iodized Salt Standard. Biol Trace Elem Res 173, 7–13 (2016). https://doi.org/10.1007/s12011-016-0619-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-016-0619-1