Abstract
Global efforts to control iodine deficiency through the highly successful strategy of salt iodization have been in effect for over two decades. In 2016, urinary iodine concentration (UIC) data in school-age children are available for 127 countries: 15 countries are classified as iodine deficient, 102 have optimal iodine nutrition, and 10 have excess iodine intakes. This reflects tremendous global progress against iodine deficiency. Increasingly, countries are recognizing the importance of monitoring the iodine status in populations that are particularly vulnerable to the negative consequences of iodine deficiency, such as pregnant women. For the first time, global UIC data in pregnant women have been compiled and presented, based on surveys from 65 countries. The iodine intake in pregnant women is insufficient in 37 countries, and the main challenge is to further strengthen the delivery of salt iodization programs to ensure that iodized salt meets the iodine requirements of pregnant women.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Iodine deficiency
- Monitoring
- Iodine status
- Urinary iodine
- Epidemiology
- Pregnant women
- School-age children
- Iodized salt
Introduction
Iodine deficiency is the result of insufficient dietary iodine intake, which can lead to inadequate production of thyroid hormones and many adverse effects at all life stages, collectively known as iodine deficiency disorders (IDD) [1–3]. Thyroid hormones are particularly critical for fetal neurodevelopment, and severe iodine deficiency during pregnancy may result in maternal and fetal hypothyroidism and cognitive impairment in children, but the effects of mild-to-moderate iodine deficiency are less clear [4, 5]. Iodine deficiency during pregnancy remains a common cause of preventable cognitive impairment worldwide [6, 7]. The universality of iodine deficiency and its devastating impact on health and development have been at the root of global control efforts through salt iodization since the 1920s [8]. Yet, in spite of tremendous progress realized and achievement of high levels of program coverage in many countries, iodine deficiency remains a threat to global public health, with its greatest impact on infants and pregnant women [9].
Global Distribution of Iodine Deficiency
Iodine deficiency is an ecological phenomenon in many parts of the world [2]. Iodine distribution in the environment is wide but uneven, with the highest concentrations found in the oceans (45–60 μg/L) [10]. From the ocean surface, iodine volatilizes into the atmosphere and is returned to land with rain and snowfall [11]. In areas affected by past glaciation and denudation this cycle is slow, and iodine is only partially replenished [12]. In many regions, the loss of iodine from the topsoil is exacerbated by high rainfall, flooding, deforestation, and overgrazing by livestock. Crops grown in iodine-depleted soils typically do not contain enough iodine to cover the dietary needs of people and livestock. As a result, populations consuming them will become iodine deficient unless iodine is reintroduced into the food chain through deliberate efforts or public health programs, e.g., salt iodization [13].
A recognized clinical indicator of thyroid dysfunction, goiter was traditionally relied on to identify regions of low iodine intake [14]. High goiter rates were reported among populations living in mountain ranges and on alluvial plains, which led to the misperception that iodine deficiency was geographically confined to these areas [2]. With the increasing use of urinary iodine concentration (UIC), which reflects a broad range of iodine intakes, the global distribution of iodine deficiency has been better understood. It is now recognized that iodine deficiency may be present (albeit in milder forms) in regions without endemic goiter, in coastal areas, large cities, and industrialized countries, where it previously had been considered to be non-existent [2, 15]. Many of the worst affected regions are also the most heavily populated (Table 3.1) [16].
Global Monitoring of Iodine Nutrition
Collecting and reporting of national, regional, and global data on iodine status has been essential for estimating the current magnitude of iodine deficiency, tracking national progress and effectiveness of prevention strategies, and identifying population groups or pocket areas that may be at risk of insufficient or excessive iodine intakes [2]. Since 2005, the World Health Organization (WHO) has reported on the global iodine status to the World Health Assembly every 3 years, most recently in 2016 [17, 18]. All countries are advised to assess their population iodine status every 5 years, even if they have already achieved optimal iodine nutrition, to reinforce the importance of program sustainability, as well as to safeguard against program backsliding and re-emergence of iodine deficiency as a public health problem [2, 17, 19].
Biomarkers of Iodine Status
Since 2001, UIC in school-age children (SAC, aged 6–12 years) has been the main indicator of iodine status and has been considered a proxy for the general population. Criteria have been established based on the median UIC level to determine the iodine status of populations (Table 3.2) [2]. The shift from reliance on goiter to an objective biomarker of exposure has improved the availability and quality of nationally representative data. Unlike goiter, UIC reacts immediately to changes in iodine intake and is, thus, ideal for monitoring the impact of salt iodization programs [2, 20].
Global Databases on Iodine Nutrition
The WHO online Global Database on Iodine Deficiency is a repository of national and sub-national data from population-based surveys of iodine status conducted between 1960 and 2007 [21]. Although the mandate to track and report the global progress against iodine deficiency lies with WHO, since 2011 the collection of population data has been supported by the Iodine Global Network (IGN, previously known as the International Council for the Control of Iodine Deficiency Disorders, ICCIDD), a technical advisory group to the WHO on iodine nutrition [22]. The available studies and estimates can be accessed on the IGN’s website, where they are regularly updated [23].
Methods to Estimate the Global Burden of Iodine Deficiency
To estimate the global status of iodine nutrition, national or sub-national UIC surveys with a population-based sampling frame and using accredited UIC analysis techniques are considered for inclusion. Nationally-representative UIC surveys are given priority over sub-national studies. Between 2003 and 2012, global estimates reported UIC data collected over the preceding 10 year period, while the 2016 estimates extend this time-frame to 15 years. In an effort to harmonize data reporting, the 2016 global estimate is the first to rely exclusively on data in school-age children (6–12 years) to estimate the iodine status in the general population (see Sect. 5 and Table 3.3). Previous global estimates included national UIC data from pre-school children, women of reproductive age, and adults when data in SAC were not available. But because the epidemiological criteria for assessing population iodine nutrition (in Table 3.2) were developed based on urine volumes and iodine concentration data in school-age children, their application in other population groups has been challenged [19, 24, 25]. Population UIC is typically not normally distributed, and the median of the UIC distribution is used instead of the mean to classify the countries’ iodine status into different degrees of public health significance (Table 3.2). For the current analysis, the acceptable range of median UICs in school-age children (100–299 μg/L) has been presented as a single category of optimal iodine intake [26].
Between 2003 and 2011, efforts were made to estimate the number of iodine deficient individuals using the UIC distribution and the reported proportion of the population with UICs below 100 μg/L [27, 28]. The national prevalence of iodine deficiency was estimated by multiplying this proportion by the country’s total population (of SAC and the general population), and the data were pooled for regional and global estimates [19, 22]. In recent years this approach has come under much criticism [19] because it assumes, incorrectly, that the UIC values reported in national surveys reflect habitual iodine intake and are, therefore, good markers of individual iodine status. In practice, this is not the case as UIC levels are highly variable from day to day, and iodine concentration in a single spot urine sample reflects only recent intake [29]. This method is likely to overestimate the real prevalence of iodine deficiency and has contributed to the erroneous perception that the global progress against iodine deficiency is slowing. In 2011, this approach led to an apparent paradox, where 74% of the children globally who were classified as iodine deficient were living in countries with an adequate median UIC, and only 26% were in countries classified as iodine deficient [19, 22]. Given this limitation, the WHO UIC median of 100 μg/L is the only meaningful metric of population iodine status, as even in countries with effective USI programs and adequate iodine intakes (i.e., median UIC ≥100 μg/L), there will be a proportion of individuals with a UIC below the 100 μg/L cut-off [19]. An alternative approach to estimating the prevalence of inadequate iodine intakes based on the estimated average requirement (EAR), and using repeat spot UIC samples to better characterize variations in iodine consumption, is currently being developed [19, 30]. In the meantime, global iodine status should continue to be reported as the number of countries with overall insufficient, adequate, and excessive iodine intake based on the recommended median UIC cut-off points.
Global Trends in Iodine Nutrition
The first comprehensive review of endemic goiter, undertaken in 1960 by WHO, estimated that iodine deficiency affected approximately 20–60% of the world’s population, mostly in low- and middle-income countries [31, 32]. Before the 1990s, only a few countries in the world with previously documented goiter prevalence were considered iodine sufficient, mainly due to iodized salt programs and iodine in dairy products, including Switzerland, some Scandinavian countries, the USA, Canada, and Australia [1]. The first global estimate of the number of individuals at risk of iodine deficiency followed in 1993 [14]. Based on the total prevalence of goiter in more than 120 countries, around 1.57 billion people were estimated to be living in areas at risk of iodine deficiency, 12% of the population had palpable goiter, and 2% suffered from endemic cretinism [14, 31]. Based on a total goiter prevalence (TGR) >5%, 113 out of 121 countries with data were classified as iodine deficient. In subsequent years, many countries introduced and scaled up salt iodization programs, and estimates on the coverage of iodized salt at the household level and on population iodine status became more readily available [15]. Global estimates of iodine deficiency based on UIC were published in 2003, 2007, 2011, 2015, and 2016 [22, 27, 28, 33, 34]. The number of countries classified as iodine deficient has declined consistently over the past two decades, roughly halving every 10 years, and countries classified with severe deficiency (mUIC <20 μg/L) have not been recorded for more than a decade (Fig. 3.1 and Table 3.3). Salt iodization programs, strong political commitment, and engagement with the salt industry at the global, regional, and national level have all played a pivotal role in this achievement.
Current Global Iodine Status
School-Age Children
The 2016 global estimate of iodine nutrition, based on surveys of school-age children conducted between 2002 and 2016, shows that the iodine intake is insufficient in 15 countries, sufficient in 102, and excessive in 10 countries (Table 3.3 and Fig. 3.2) [34]. Among the 15 countries with insufficient intake, only two are classified as moderately deficient and 13 as mildly deficient. The dwindling number of countries with insufficient iodine intake, from 32 in 2011 and 25 countries in 2015 to 15 countries in 2016 [22, 33, 34] is mainly a reflection of continuing progress to improve the coverage of iodized salt at the national level. However, the stricter data inclusion criteria applied in 2016 (see Sects. 3.3 and 3.4) have meant that eligible UIC surveys are available for fewer countries: 126 countries in 2016 compared with 154 countries in 2015, and 148 countries in 2011. This represents a drop in global population data coverage from 98.2% of 6–12 year-olds in 2015 to 93.3% in 2016, and it may confound trend analysis (Fig. 3.1). At the same time, many countries continue to sustain or strengthen their iodine monitoring efforts. Since 2015, 18 new nationally-representative surveys in SAC have been reportedFootnote 1. In 2016, there is considerable regional variation in population data coverage, ranging from more than 99% in the Americas, where salt iodization and national iodine nutrition monitoring programs have been very well-implemented and effective, to approximately 80% in Europe, where iodine nutrition surveillance and prophylaxis are heterogeneous, with many countries lacking regulatory support.
Iodine nutrition based on the median urinary iodine concentration (mUIC) in school-age children, by country in 2016 [34]
Although the proportion of sub-national surveys is steadily decreasing, in 2016 they cover around 27% of the world’s SAC population in 20 countries (Table 3.3). Sub-national UIC surveys are commonly carried out to provide a rapid assessment of iodine status in the population in pre-selected areas, but due to a lack of sampling rigor and adherence to basic principles of randomization, they may over- or underestimate the burden of iodine deficiency at the national level and should be interpreted with caution [1, 22].
Re-emergence of Iodine Deficiency
When iodine deficiency control programs lapse in areas that were previously considered iodine sufficient, the risk of IDD reappears, and such countries require remedial action to revitalize and strengthen the sustainability of their USI programs [35]. Like many countries which pledged to eliminate iodine deficiency at the 1990 World Summit for Children, Vietnam mandated salt iodization in the 1990s. By 2005, adequately iodized salt was reaching more than 90% of households in Vietnam, and the country was declared as iodine sufficient (with a median UIC in SAC of 139 μg/L in 2003) [22]. However, Vietnam downgraded the USI program to voluntary in 2005. The household coverage of iodized salt and the iodine status in SAC declined as a result, but the ongoing monitoring detected these declines and led to renewed efforts to reinstate the program in 2016 [36]. Vietnam’s experience highlights the fact that prevention of iodine deficiency is an ongoing process, which necessitates long-term political commitment and sustainable implementation.
Australia and New Zealand are frequently cited as examples of industrialized countries where a change in dairy farming practices led to a re-appearance of iodine deficiency, when iodine-containing sterilizers were replaced with other chemicals, and the consumption of milk, the primary source of iodine in the diet, declined at the same time [37, 38]. To address these decreases in iodine intake, both countries mandated the use of iodized salt in commercially baked bread in 2009, and more recent surveys in SAC have confirmed that the iodine status has improved.
Excess Iodine Intake
Iodine excess occurs when the iodine intake is too high, generally as a result of over-iodization of salt (addition of too much iodine to salt at the point of production due to poor quality control or high iodization standards) or high intake of iodine from other sources, including iodine in local water supplies [39]. A high population intake of iodine, manifesting as a median UIC ≥300 μg/L, was reported in five countries in 2003, seven countries in 2007, and 10 countries in 2016 [27, 28, 34]. This gradual upward trend demonstrates the importance of regular monitoring of iodine status to detect not only inadequate but also excessive iodine intakes, and to better understand the sources of iodine in the diet [22]. It is important to note, however, that the benefits of correcting iodine deficiency far outweigh the health risks associated with excess.
Iodine Status and Trends in Pregnant Women
During pregnancy, the daily requirement for iodine increases from 150 μg in non-pregnant women to 250 μg to account for increased renal clearance of iodine and to cover the needs of the developing fetus [40]. In a population of pregnant women, a median UIC <150 μg/L indicates that iodine intake is insufficient, and a median UIC of 500 μg/L or higher indicates that iodine intakes are excessive (Table 3.4) [2, 41]. The increased requirement puts pregnant women and their offspring at higher risk of iodine deficiency than the general population, particularly if the availability of iodine in the diet is poor [42]. Recent studies indicate that pregnant women may be at risk of iodine deficiency even when school-age children in the same area are maintaining adequate iodine intakes [43–48]. As such, there is growing awareness of the need to monitor the iodine status of pregnant women through national surveys and to make programmatic adjustments to ensure that their needs are met.
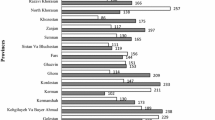
In 2016, recent surveys (conducted between 2002 and 2016) in pregnant women cover a third of the world’s countries (65 out of 194 WHO member states) [34]. By comparison, only 42 countries had data on the iodine status of pregnant women in 2006 according to the WHO Global Database on Iodine Deficiency [20, 21]. Figure 3.3 shows the global status of iodine nutrition in 2016 based on surveys in pregnant women. Although the 65 surveys are distributed across all six WHO regions, 28 (43%) cover more than a half of the European region (Table 3.5). Data coverage is also reasonably high (6 out of 11 of countries) in South-East Asia. The lowest coverage is in Sub-Saharan Africa, where only 17%, or 7 out of 39 countries have data. It should be noted that fewer than a half of the country estimates are based on nationally representative surveys, which adds uncertainty to the data and highlights the need to systematically expand national iodine monitoring to include pregnant women.
Iodine nutrition based on the median urinary iodine concentration (mUIC) in pregnant women, by country in 2016 [34]
The iodine status of pregnant women is sufficient in 23 countries, which in a majority of cases can be attributed to long-standing salt iodization programs. In these countries, the median UIC is generally lower in pregnant women compared to SAC, as seen in China (198 μg/L in SAC vs. 155 μg/L in PW in 2014), Thailand (237 μg/L in SAC vs. 156 μg/L in PW in 2014), Mongolia (171 μg/L in SAC vs. 152 μg/L in PW in 2010), and Indonesia (223 μg/L in SAC vs. 172 μg/L in PW in 2013). However, this is expected given physiological adaptations associated with pregnancy, including increased renal clearance of iodine and greater urine volume.
At the same time, the iodine intake is classified as low in 37 out of the 65 countries with available data. Globally, a number of countries are reporting adequate iodine intakes among SAC coupled with inadequate intakes in pregnant women, such as in the Philippines (mUIC of 168 μg/L in SAC vs. 105 μg/L in PW in 2013), Sri Lanka (164 μg/L in SAC vs. 113 μg/L in PW in 2010), and Belgium (113 μg/L in SAC vs. 124 μg/L in PW) [34]. A previous US NHANES reported a median UIC among 6–11 year-old children to be above 200 μg/L, but only 125 μg/L in pregnant women [49]. In Europe, three-quarters of countries report inadequate iodine intakes among pregnant women, and only 11% of countries among school-age children [34]. This emerging trend clearly highlights the need to make adjustments in the USI strategy to ensure that the dietary needs of pregnant women are met, but also to better understand how to interpret UIC data in this population group.
WHO/UNICEF recommend iodine supplementation of all pregnant women in countries where salt iodization is not feasible or incomplete [40]. Iodine supplementation of pregnant and lactating women has been recommended by scientific societies and regulatory bodies in Australia [15], USA and Canada [50], and Europe [51, 52], but it has not been widely adopted. Randomized controlled trials investigating the effects of iodine supplementation on pregnant women exposed to mild-to-moderate iodine deficiency are lacking, and its long-term benefits and safety in this group are unclear [5].
Remaining Challenges
Although USI programs have been implemented in more than 140 countries, and around 75% of households globally have access to adequately iodized salt [53, 54], some countries and sub-groups within countries continue to be at risk of sub-optimal iodine intakes. Despite ongoing efforts to improve access to iodized salt for all populations, disparities in household coverage have been reported at the sub-national level, where coverage could vary between rural and urban areas, or between the poorest and the richest socio-economic strata. In an analysis of iodized salt coverage amongst 11 low- and lower-middle-income countries in 2010, the coverage of iodized salt in urban areas was 8.7% higher than in rural areas, and 19.3% higher in the richest than in the poorest quintile in low-income countries [9]. A recent national survey in the Philippines suggests that such inequity may translate into a significantly lower iodine status among the rural poor [55]. Advocating the importance of iodine to national governments, encouraging the salt industry to iodize all salt for human consumption, and the food industry to use iodized salt in the manufacture of processed foods and condiments are all critical actions needed to ensure progress towards the global elimination of iodine deficiency. While overall program performance may be satisfactory, it is imperative to focus on reaching disadvantaged groups, particularly pregnant women and those of lower SES, in order to ensure that the entire population is protected from IDD.
Notes
- 1.
These include Bangladesh, Burkina Faso, China, Ecuador, Egypt, Ethiopia, Indonesia, Japan, Panama, Paraguay, Peru, Spain, Sri Lanka, Switzerland, Uruguay, Venezuela, Vietnam, and Yemen.
Abbreviations
- EAR:
-
Estimated average requirement
- IDD:
-
Iodine deficiency disorders
- ICCIDD:
-
International Council for the Control of Iodine Deficiency Disorders
- IGN:
-
Iodine Global Network
- PW:
-
Pregnant women
- SAC:
-
School-age children
- TGR:
-
Total goiter rate
- UIC:
-
Urinary iodine concentration
- WHO:
-
World Health Organization
- WRA:
-
Women of reproductive age
References
Zimmermann MB, Jooste PL, Pandav CS. Iodine-deficiency disorders. Lancet. 2008;372(9645):1251–62.
World Health Organization, United Nations Children’s Fund, International Council for Control of Iodine Deficiency Disorders. Assessment of iodine deficiency disorders and monitoring their elimination. A guide for programme managers. Geneva: WHO; 2007.
Eastman CJ, Zimmermann MB. The iodine deficiency disorders. In: LJ DG, Beck-Peccoz P, Chrousos G, Dungan K, Grossman A, JM H, et al., editors. Endotext [Internet]. South Dartmouth: MDText.com, Inc.; 2000.
Zimmermann MB. Iodine deficiency. Endocr Rev. 2009;30(4):376–408.
Pearce EN, Lazarus JH, Moreno-Reyes R, Zimmermann MB. Consequences of iodine deficiency and excess in pregnant women: an overview of current knowns and unknowns. Am J Clin Nutr. 2016;104(Suppl 3):918S–23S.
Zimmermann MB. The importance of adequate iodine during pregnancy and infancy. World Rev Nutr Diet. 2016;115:118–24.
Bougma K, Aboud FE, Harding KB, Marquis GS. Iodine and mental development of children 5 years old and under: a systematic review and meta-analysis. Nutrients. 2013;5(4):1384–416.
UNICEF-WHO Joint Committee on Health Policy. World summit for children-mid-decade goal: iodine deficiency disorders (IDD). UNICEF–WHO Joint Committee on Health Policy special session; 27–28 January 1994. Geneva: WHO; 1994.
Thach Duc T, Hetzel B, Fisher J. Access to iodized salt in 11 low- and lower-middle-income countries: 2000 and 2010. Bull World Health Organ. 2016;94(2):122–9.
Fuge R, Johnson CC. The geochemistry of iodine—a review. Environ Geochem Health. 1986;8(2):31–54.
Goldschmidt VW. Geochemistry. Oxford: Oxford University Press; 1954.
Zimmermann MB. Iodine deficiency in industrialised countries. Proc Nutr Soc. 2010;69(1):133–43.
Hetzel BS. The story of iodine deficiency. Oxford: Oxford University Press; 1989.
World Health Organization, United Nations Children’s Fund, International Council for Control of Iodine Deficiency Disorders. Global prevalence of iodine deficiency disorders, Micronutrient Deficiency Information System (MDIS) working paper no. 1. Geneva: Micronutrient Deficiency Information System/WHO; 1993.
Li M, Eastman CJ. The changing epidemiology of iodine deficiency. Nat Rev Endocrinol. 2012;8(7):434–40.
Rohner F, Zimmermann M, Jooste P, Pandav C, Caldwell K, Raghavan R, et al. Biomarkers of nutrition for development-iodine review. J Nutr. 2014;144(8):1322S–42S.
World Health Organization. Resolution WHA58.24. Sustaining the elimination of iodine deficiency disorders. Fifty-eighth World Health Assembly, Geneva, 25 May 2005. Geneva: WHO; 2005.
World Health Organization. Sustaining the elimination of iodine deficiency disorders (resolution WHA60.21). Progress report: Report by the Secretariat. Sixty-ninth World Health Assembly, Geneva, 1 April 2016. Geneva: WHO; 2016.
Zimmermann MB, Andersson M. Assessment of iodine nutrition in populations: past, present, and future. Nutr Rev. 2012;70(10):553–70.
Andersson M, de Benoist B, Rogers L. Epidemiology of iodine deficiency: salt iodisation and iodine status. Best Pract Res Clin Endocrinol Metab. 2010;24(1):1–11.
World Health Organization [Internet]. The WHO global database on iodine deficiency 2007 [cited 1 July 2016]. Available from: http://www.who.int/vmnis/iodine/data/en/index.html
Andersson M, Karumbunathan V, Zimmermann MB. Global iodine status in 2011 and trends over the past decade. J Nutr. 2012;142(4):744–50.
The Iodine Global Network. Global iodine scorecard and map [Internet]. Zurich: The Iodine Global Network; 2016 [cited 28 September 2016]. Available from: http://www.ign.org/scorecard.htm
Dold S, Zimmermann MB, Baumgartner J, Davaz T, Galetti V, Braegger C, Andersson M. A dose-response crossover iodine balance study to determine iodine requirements in early infancy. Am J Clin Nutr. 2016;104(3):620–8.
Brough L, Thomson BM, Skeaff SA. Revisiting the iodine global network’s definition of iodine status by country. Br J Nutr. 2016;115(2):374–6.
Zimmermann MB, Aeberli I, Andersson M, Assey V, Yorg JA, Jooste P, Jukić T, Kartono D, Kusić Z, Pretell E, TO Jr SL, Untoro J, Timmer A. Thyroglobulin is a sensitive measure of both deficient and excess iodine intakes in children and indicates no adverse effects on thyroid function in the UIC range of 100–299 μg/L: a UNICEF/ICCIDD study group report. J Clin Endocrinol Metab. 2013;98(3):1271–80.
Andersson M, Takkouche B, Egli I, Allen HE, de Benoist B. Current global iodine status and progress over the last decade towards the elimination of iodine deficiency. Bull World Health Organ. 2005;83(7):518–25.
de Benoist B, McLean E, Andersson M, Rogers L. Iodine deficiency in 2007: global progress since 2003. Food Nutr Bull. 2008;29(3):195–202.
König F, Andersson M, Hotz K, Aeberli I, Zimmermann MB. Ten repeat collections for urinary iodine from spot samples or 24-hour samples are needed to reliably estimate individual iodine status in women. J Nutr. 2011 Nov;141(11):2049–54.
Zimmermann MB, Hussein I, Al Ghannami S, El Badawi S, Al Hamad NM, Abbas Hajj B, et al. Estimation of the prevalence of inadequate and excessive iodine intakes in school-age children from the adjusted distribution of urinary iodine concentrations from population surveys. J Nutr. 2016 Jun;146(6):1204–11.
Hetzel BS. The nature and magnitude of the Iodine Deficiency Disorders (IDD). In: Hetzel BS, editor. Towards the global elimination of brain damage due to iodine deficiency. Delhi: Oxford University Press; 2004.
Clements FW, de Moerloose J, de Smet MP, Holman JCM, Kelly FC, Langer P, et al. Endemic goitre, WHO monograph series no. 44. Geneva: WHO; 1960.
The Iodine Global Network. Global iodine nutrition scorecard 2015 [Internet]. Zurich: The Iodine Global Network; 2015 [cited 1 June 2016]. Available from: http://www.ign.org/cm_data/Scorecard_2015_August_26_new.pdf
The Iodine Global Network. Global Iodine Nutrition Scorecard 2016 [Internet]. Zurich: The Iodine Global Network; 2016 [cited 1 August 2016]. Available from: http://www.ign.org/cm_data/Scorecard_2016_SAC_PW.pdf
Pearce EN, Andersson M, Zimmermann MB. Global iodine nutrition: where do we stand in 2013? Thyroid. 2013;23(5):523–8.
UNICEF East Asia and Pacific Regional Office (EAPRO). Meeting report: the East Asia Pacific regional workshop on achievement of universal salt iodization for optimal iodine nutrition, 12–14 October 2015, Bangkok[Internet]. Bangkok: UNICEF, IGN, GAIN, MI; 2016 [cited 2 October 2016]. Available from: http://www.unicef.org/eapro/East_Asia_Pacific_Regional_Workshop_on_Achievement_of_Universal_Salt_Iodization_for_Optimal_Iodine_Nutrition.pdf
Li M, Eastman CJ, Waite KV, Ma G, Zacharin MR, Topliss DJ, et al. Are Australian children iodine deficient? Results of the Australian National Iodine Nutrition Study. Med J Aust. 2006;184(4):165–9.
Li M, Waite KV, Ma G, Eastman CJ. Declining iodine content of milk and re-emergence of iodine deficiency in Australia. Med J Aust. 2006;184(6):307.
Delange F, de Benoist B, Pretell E, Dunn JT. Iodine deficiency in the world: where do we stand at the turn of the century? Thyroid. 2001;11(5):437–47.
World Health Organization, United Nations Children’s Fund. Reaching optimal iodine nutrition in pregnant and lactating women and young children. Joint statement by the World Health Organization and the United Nations Children’s Fund. Geneva: WHO; 2007.
Andersson M, de Benoist B, Delange F, Zupan J. Prevention and control of iodine deficiency in pregnant and lactating women and in children less than 2-years-old: conclusions and recommendations of the Technical Consultation. Public Health Nutr. 2007;10(12A):1606–11.
Glinoer D. Iodine nutrition requirements during pregnancy. Thyroid. 2006;16(10):947–8.
Wong EM, Sullivan KM, Perrine CG, Rogers LM, Pena-Rosas JP. Comparison of median urinary iodine concentration as an indicator of iodine status among pregnant women, school-age children, and nonpregnant women. Food Nutr Bull. 2011;32(3):206–12.
Vandevijvere S, Amsalkhir S, Bensouda Mourri A, Van Oyen H, Moreno-Reyes R. Iodine status of pregnant women in Belgium. Br J Nutr. 2013;109:2276–84.
Granfors M, Andersson M, Stinca S, Åkerud H, Skalkidou A, Sundström Poromaa I, Wikström AK, Filipsson NH. Iodine deficiency in a study population of pregnant women in Sweden. Acta Obstet Gynecol Scand. 2015;94(11):1168–74.
Marchioni E, Fumarola A, Calvanese A, Piccirilli F, Tommasi V, Cugini P, et al. Iodine deficiency in pregnant women residing in an area with adequate iodine intake. Nutrition. 2008;24(5):458–61.
Gowachirapant S, Winichagoon P, Wyss L, Tong B, Baumgartner J, Melse-Boonstra A, et al. Urinary iodine concentrations indicate iodine deficiency in pregnant Thai women but iodine sufficiency in their school-aged children. J Nutr. 2009;139(6):1169–72.
Lindorfer H, Krebs M, Kautzky-Willer A, Bancher-Todesca D, Sager M, Gessl A. Iodine deficiency in pregnant women in Austria. Eur J Clin Nutr. 2015;69(3):349–54.
Caldwell KL, Miller GA, Wang RY, Jain RB, Jones RL. Iodine status of the US population, National Health and Nutrition Examination Survey 2003–2004. Thyroid. 2008;18(11):1207–14.
Stagnaro-Green A, Abalovich M, Alexander E, Azizi F, Mestman J, Negro R, et al. Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and postpartum. Thyroid. 2011 Oct;21(10):1081–125.
Lazarus J, Brown RS, Daumerie C, Hubalewska-Dydejczyk A, Negro R, Vaidya B. 2014 European thyroid association guidelines for the management of subclinical hypothyroidism in pregnancy and in children. Eur Thyroid J. 2014;3(2):76–94.
Zimmermann M, Delange F. Iodine supplementation of pregnant women in Europe: a review and recommendations. Eur J Clin Nutr. 2004;58(7):979–84.
The #FutureFortified Global Summit on Food Fortification: event proceedings and recommendations for food fortification programs [Internet]. Basel: Sight and Life on behalf of Global Alliance for Improved Nutrition (GAIN), July 2016 [cited 30 September 2016]. Available from: http://www.gainhealth.org/wp-content/uploads/2016/07/FutureFortifiedSupplement-6-July-2016.pdf
UNICEF. Household consumption of adequately iodized salt [Internet]. October 2014 [cited 2 October 2016]. Available from: http://data.unicef.org/wp-content/uploads/2015/12/Iodized-salt-consumption-SOWC-6-November-2014_67.xlsx
Perlas LA, Serafico ME, Ulanday JRC, Marcos JM, Alibayan MV, Desnacido JA. 8th national nutrition survey, Philippines 2013. Manila: Food and Nutrition Research Institute, Department of Science and Technology; 2014.
Acknowledgments
We thank Vincent Assey, Karen Codling, Nita Dalmiya, Gregory Gerasimov, Izzeldin Hussein, Pieter Jooste, John Lazarus, Gary Ma, Qian Ming, Chandrakant S. Pandav, Elizabeth Pearce, Eduardo A. Pretell, Ekaterina Troshina, and Michael B Zimmermann for providing recent country data on iodine status. We also thank Karen Abbott for help in compiling data on the iodine status in pregnant women.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Gizak, M., Gorstein, J., Andersson, M. (2017). Epidemiology of Iodine Deficiency. In: Pearce, E. (eds) Iodine Deficiency Disorders and Their Elimination. Springer, Cham. https://doi.org/10.1007/978-3-319-49505-7_3
Download citation
DOI: https://doi.org/10.1007/978-3-319-49505-7_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-49504-0
Online ISBN: 978-3-319-49505-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)