Abstract
Leukemia is a major type of cancer affecting a significant segment of the population, and especially children. In fact, leukemia is the most frequent childhood cancer, with 26 % of all cases, and 20 % mortality. The multidrug resistance phenotype (MDR) is considered one of the major causes of failure in cancer chemotherapy. The present study aimed to investigate the relationship between the expression of MDR1 and CYP450 genes in human chronic myelogenous leukemia cells (K-562) treated with cisplatin (cisPt) and two ruthenium-based coordinated complexes [cisCRu(III) and cisDRu(III)]. The tested compounds induced apoptosis in K-562 tumor cells as evidenced by caspase 3 activation. Results also revealed that the amplification of P-gp gene is greater in K-562 cells exposed to cisPt and cisCRu(III) than cisDRu(III). Taken together, all these results strongly demonstrate that MDR-1 overexpression in K-562 cells could be associated to a MDR phenotype, and moreover, it is also contributing to the platinum and structurally related compound, resistance in these cells.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Leukemia is a major type of cancer affecting a significant segment of the population, and especially children. In fact, leukemia is the most frequent childhood cancer, with 26 % of all cases, and 20 % mortality [1]. The annual incidence of leukemia is 1.3 to 1.5/105, with a slight male preponderance, but no significant differences across ethnicities. During the initial chronic phase (CP), cellular differentiation and function are largely maintained, therapy is effective, and mortality is low. Without effective treatment, the disease invariably progresses to blastic phase (BP), a rapidly fatal acute myeloid leukemia. The central problem is that chronic myelogenous leukemia (CML) is usually diagnosed in BP, an indolent stage characterized by expansions of differentiating cells that can last for several, sometimes many years, and the acquisition of additional mutations promotes progression to advanced therapy-refractory disease. Unfortunately, when CML becomes BP therapy-refractory, they are almost incurable with the currently available drug therapy [2].
Chronic myelogenous leukemia (CML) cells are characterized by the presence of a BCR-ABL fusion gene, which produce a chimeric protein known as BCR-ABL with constitutive tyrosine kinase activity [3]. Imatinib mesylate emerged as a very useful compound for clinical development, since it potently inhibits all of the ABL tyrosine kinases and it has proven to be highly effective in the treatment of the CML [4]. However, some leukemia relapse can occur and several mechanisms of resistance were well described [5].
The multidrug resistance phenotype (MDR) is considered one of the major causes of failure in cancer chemotherapy, and it is associated with the overexpression of P-glycoprotein (P-gp or MDR1) in tumor cell membranes. While cytochrome P450 proteins are responsible for phase I metabolism of xenobiotics, P-gp, the product of the MDR1 gene, is an ATP-dependent pump that transports a wide variety of structurally diverse compounds out of the cell, resulting in a decrease of its intracellular accumulation [6, 7] and it is among the strongest prognostic factors in acute myeloid leukemia [8].
Heavy metal coordination complexes such as platinum, gallium, and ruthenium have been investigated for their possible antitumor activity [8, 9]. Among the most studied metal complexes, cisplatin and related platinum-based drugs have drawn much attention. Since cisplatin [cis-diamminedichloroplatinum (II)] was approved by the American Food and Drugs Administration (FDA) for cancer therapy in 1978, it has become the most widely used anticancer drug, with an estimated 70 % of patients receiving the compound as part of their treatment [10, 11].
While the chemotherapeutic success of platinum is undeniable, it is by no means the perfect drug. It is not effective against many common types of cancer, toxicity and drug resistance are common, and it has a deplorable range of side effects, which can include nerve damage, hair loss, and nausea [12].
To overcome these limitations, some compounds based on ruthenium have been developed and tested against cancer cell lines. Several studies have been shown that ruthenium compounds present relevant antineoplastic activities towards several tumor lineages in vitro and in vivo, as well as antimetastatic properties with lower systemic cytotoxicity, when compared to platinum-based compounds; additionally, these ruthenium compounds were shown to have a greater effect on tumor cells than on normal cells [13, 14].
Although significant progress has been made towards understanding leukemia transformation and disease progression, the molecular mechanism of multidrug resistance to chemotherapy remained largely unknown in K-562 tumor cells. Since previous studies show that the resistance to chemotherapy exhibited in multidrug-resistant human leukemic K-562 cells was mediated by P-gp and others CYP450 proteins, the present study aimed to investigate the relationship between the expression of MDR1 and CYP450 genes in human chronic myelogenous leukemia cells (K-562) treated with cisplatin and two ruthenium(III) compounds.
Material and Methods
Ruthenium(III) Compound Synthesis, Cisplatin, and Chemicals
The ruthenium(III) complexes cis-(dichloro)tetrammineruthenium(III) chloride {cis-[RuCl2(NH3)4]Cl} and cis-tetraammine(oxalato)ruthenium(III) dithionate {cis-[Ru(C2O4)(NH3)4]2(S2O6)} were synthesized at the Chemistry Institute of Universidade Federal de Mato Grosso by the methods described in detail previously [15–17]. Cisplatin [cis-diamminedichloroplatinum (II)] was obtained from Sigma-Aldrich (Sigma-Aldrich Corp, St. Louis, MO, USA).
The stock solutions of Ru(III) complexes and cisplatin were freshly prepared before use in DMSO (Sigma-Aldrich Corp, St. Louis, MO, USA). The final concentration of DMSO in cell culture medium did not exceed 0.25 % (v/v).
Cell Culture
The human chronic myelogenous leukemia cells (K-562 ATCC®# CCL-243TM) were purchased from the American Type Culture Collection (ATCC, Rockville, MD, USA). Tumor cells were cultured in RPMI 1640 medium (pH 7.2–7.4) at 37 °C, under a 5 % CO2 humidified atmosphere. Media were supplemented with 100 U mL−1 penicillin G, 100 μg mL−1 streptomycin, 2 mM l-glutamine, 1.5 g L−1 sodium bicarbonate, 4.5 g L−1 glucose, 10 mM HEPES, 1.0 mM sodium pyruvate, and 10 % fetal calf serum (FCS) (w/v) (all reagents were obtained from Gibco®, Invitrogen, Carlsbad, CA, USA) and subcultured two to three times a week at an appropriate plating density.
Cell Viability Determination by MTT Assay
The cytotoxic activity of ruthenium(III) compound was measured by 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide (MTT) assay as previously described [18]. Cisplatin and Ru(III) metallodrugs were added to final concentrations from 0 to 500 μM. The logarithmically growing K-562 cells were washed twice with supplemented RPMI medium and centrifuged at (1000 rpm) 300×g/15 min/10 °C. Cells were plated at a density of 5 × 104 cells/well into flat-bottomed 96-well microplates (Nalge-Nunc, Rochester, NY, USA) and cultured for 24 h.
Cell death was evaluated after 72-h treatment, or the cells were exposed to the complexes for 24 h; then, after removal of the complexes, a fresh medium was added, and the cells were incubated for 48 h of recovery time. Then, 10 μL MTT (5 mg mL−1) (Sigma-Aldrich, St. Louis, MO, USA) was added to each well and incubated for additional 6 h. The microplates were then centrifuged (300×g/15 min/10 °C) and the culture media were discarded. Then, 200 μL of PBS/20 % of SDS was added to each well and plates were kept in the dark overnight.
Absorbance was measured at 545 nm (OD545nm) using an automated microplate reader (Stat Fax 2100, Awareness Technology Inc, Palm City, FL, USA). The viability rate was calculated as follows:
The IC50 values (compound concentrations that produce 50 % of cell growth inhibition) were calculated from curves constructed by plotting cell survival (%) versus drug concentration (μM) using GraphPad Prism 4.02 for Windows (GraphPad Software, San Diego, CA, USA). All experiments were made in triplicate.
Cell Toxicity Measurement with LDH Assay
LDH is a cytoplasmic enzyme, and LDH reduction is often associated with cell membrane damage and cell death [19]. The activity of LDH was measured spectrophotometrically by assaying reduced nicotinamide adenine dinucleotide (NAD) oxidation at 510 nm during LDH-catalyzed reduction of pyruvate to lactate. Briefly, cells were cultured at a density of 5 × 104 cells/well into flat-bottomed 96-well microplates (Nalge-Nunc, Rochester, NY, USA) and incubated for 24 h with cisplatin and ruthenium(III) complexes at IC50 concentrations. After 24 h of incubation, the cell culture supernatant was removed and centrifuged to eliminate non-adherent particles and cell debris. Samples of supernatant for each drug tested were then analyzed for DHL activity using a DHL colorimetric kit (Doles LTDA, Goiânia, GO, Brazil). All experiments were made in triplicate.
Reverse Transcription and Real-Time Quantitative PCR
The human chronic myelogenous leukemia cells K-562 were treated with different concentrations of Ru(III) complexes and cisplatin for different periods. Total RNA was extracted with Tri Reagent® (Sigma-Aldrich Co., St. Louis, MO, USA) following the manufacturer’s protocol. Total RNA (2.0 μg) was used to produce complementary DNA (cDNA) with ABgene one-step Verso™ RT-PCR Kit (Thermo Fisher Scientific Inc., Waltham, MA, USA) in a total of 25 μL reaction mixture according to the manufacturer’s protocol. Real-time PCR reactions were then carried out by a LineGene K fluorescence quantitative PCR detection system (Hangzhou BIOER Tech Co., Tokyo, Japan). Homo sapiens apoptosis-related cysteine peptidases (caspases) 3, 8, and 9 messenger RNA (mRNA) expression were quantified for apoptosis cell profiling using specific primers (Table 1).
Furthermore, MDR-1 mRNA [H. sapiens ATP-binding cassette, subfamily B (MDR/TAP), member 1 (ABCB1)]; CYP3A4 mRNA (H. sapiens cytochrome P450, family 3, subfamily A, polypeptide 4); CYP2C9 mRNA (H. sapiens cytochrome P450, family 2, subfamily C, polypeptide 9); and CYP2C19 mRNA (H. sapiens cytochrome P450, family 2, subfamily C, polypeptide 19) were detected in order to evaluate the expression profile of these genes in cells exposed to the cisplatin and ruthenium(III) complexes (Table 1).
A total of 25 μL reaction mixture: 2 μL of cDNA, 10 μL of SYBR Green PCR Master Mix (LGC Biotechnology, Middlesex, UK), and 2.5 μL of each forward and reverse primer (100 nM μL−1). The PCR program was initiated at 15 min at 95 °C before 40 thermal cycles, each of 30 s at 95 °C, 30 s at 55 °C, and 30 s at 72 °C. Data were analyzed according to relative quantification method. Each sample was normalized by the expression of following endogenous genes: GAPDH (H. sapiens glyceraldehyde-3-phosphate dehydrogenase) and B2M (H. sapiens beta-2-microglobulin) (Table 1). Checking of the products was performed by melting curve analysis and agarose gel electroforesis of qPCR products.
Statistical Analysis
Statistical analysis of the results was performed using one-way ANOVA and Tukey’s post test for multiple comparisons with controls. All statistical analyses were performed using the statistical software GraphPad Prism 4 (GraphPad Software Inc., La Jolla, CA, USA). A probability of 0.05 or less was deemed statistically significant. The following notation was used throughout: *p < 0.05, **p < 0.01, relative to control.
Results
The Dose-Dependent Cytotoxicity of cisPt, cisCRu(III), and cisDRu(III) on K-562 Tumor Cells
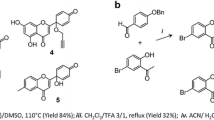
The anticancer drug cis-diamminedichloroplatinum(II) [cisPt] and two ruthenium(III) complexes, cis-(dichloro)tetrammineruthenium(III) chloride [cisCRu(III)], and cis-tetraammine(oxalato)ruthenium(III) dithionate [cisDRu(III)] (Fig. 1) were evaluated in a comparative in vitro MTT cell viability assay with human chronic myelogenous leukemia cell line K-562.
Cell viability was detected after the cells were treated with cisPt, cisCRu(III), and cisDRu(III) at concentrations from 0.2 to 500 μM for 48 h.
Measurement of the number of living cells using MTT or similar assays in drug-treated and control cultures is the most commonly used method in cell-based screening experiments. The results can be interpreted as an indicator for the cytotoxic selectivity of the applied drug towards tumorigenic tissue. The IC50 values for compounds tested are depicted in Table 2. The data indicate that cisDRu(III) is the most cytotoxic compound of three on tested cell line, followed by cisPt and cisCRu(III) (Fig. 2).
Although the cytotoxicity of cisDRu(III) on K-562 presented be higher than others two metallocomplexes, the results show that K-562 tumor cells treated with different concentration of cisPt and ruthenium complexes cisCRu(III) and cisDRu(III), ruthenium-based coordinated complexes, presented moderate cytotoxic and antiproliferative activities.
Cytomembrane Damage of K-562 Cells Induced by cisPt and Ruthenium(III) Complexes
The lactate dehydrogenase (LDH) release experiments (Fig. 3) using K-562 IC50 concentrations of cisPt, cisCRu(III), and cisDRu(III) showed loss of cell vitality, which corroborates results observed on MTT assays. The compound cisDRu(III) caused K562 cytomembrane damage on a scale higher than cisPt and cisCRu(III).
Caspase Activity and Apoptosis on K-562 Tumor Cell Line
The effects of cisPt, cisCRu(III), and cisDRu(III) on mRNA expression of caspase 3, caspase 8, and caspase 9 were analyzed by real-time quantitative PCR after 6 h of treatment. As it is possible to see from these results, the activities of caspase 8 and caspase 9 changed modestly in treated cells when compared to untreated control cells. Moreover the mRNA expression of caspase 3 was slightly increased (from 1.8- to 2.6-fold) after 6 h exposure to cisPt, cisCRu(III), and cisDRu(III) (Fig. 4). Caspase 3 was reported to be an important key executioner of apoptosis. As shown in Fig. 4, the induction of caspase 3 by cisDRu(III) is increased when related to cisPt and cisCRu(III) levels, what could probably explain the relative low IC50 of cisDRu(III).
Alterations of caspases expression after treatment with cisPt, cisCRu(III), and cisDRu(III), for 6 h. Samples are in relation to the untreated control cell line with a transcription rate set up to a value of one. The data are expressed as mean ± SEM of n = 3. Means among bars without a common letter are statistically different (Tukey’s test, p < 0.05)
Determination of Multidrug Resistance Phenotype in K-562 Tumor Cell Line
The expression of MDR and CYPs genes in K-562 tumor cells were evaluated by real-time reverse-transcription PCR using specifics primers. Although K-562 tumor cells have never been exposed to cisPt, cisCRu(III), and cisDRu(III) before these experiments, qPCR analysis revealed that the amplification of MDR1 and CYPs genes are greater on K-562 cells treated with metallocomplexes compared to untreated cells. As shown in Fig. 5, treatment of K-562 with cisPt, cisCRu(III), and cisDRu(III) resulted in significantly induced MDR-1 expression levels.
Alterations of MDR1-mRNA expression using RT-qPCR after treatment with cisPt, cisCRu(III) and cisDRu(III), respectively, for 24 and 48 h. Samples are in relation to the untreated control cell line with a transcription rate set up to a value of one. The data are expressed as mean ± SD of n = 3. Means among bars without a common letter are statistically different (Tukey’s test, p < 0.05)
Results also revealed that the amplification of P-gp gene is greater in K-562 cells exposed to cisPt and cisCRu(III) than cisDRu(III). Is important to note that cisPt and cisCRu(III) are structurally similar. Taken together, all these results strongly demonstrate that P-gp overexpression in K-562 cells could be associated to a MDR phenotype, and moreover, it is also contributing to the platinum and structurally related compound, resistance in these cells.
To evaluate the clinical relevance of the observations that certain anticancer drugs are able to induce cytochrome P450 (CYPs) genes activity, and mRNA and protein expression levels, expression levels of CYPs was quantified by real-time PCR after treatment with metallodrugs (Fig. 6).
Alterations of CYPs mRNAs expression using RT-qPCR after treatment with cisPt, cisCRu(III), and cisDRu(III), respectively, for 24 and 48 h. Samples are in relation to the untreated control cell line with a transcription rate set up to a value of one. The data are expressed as mean ± SD of n = 3. Means among bars without a common letter are statistically different (Tukey’s test, p < 0.05)
CYP2C9 is an important cytochrome P450 enzyme with a major role in the oxidation of both xenobiotic and endogenous compounds. The metallocomplexes did not exert a significant effect on induction of CYP3A4 expression on K-562 cells. On the other hand, as expected, cisPt, cisCRu(III), and cisDRu(III) enhanced CYP2C9 and CYP2C19 mRNA expression levels; cisDRu(III) caused a fivefold CYP2C9 increase, while cisPt and cisCRu(III) were shown to increase the expression of CYP2C9 by three- and fourfold, respectively, after 48 h or treatment. CYP2C19 also showed an increasing on mRNA levels, although they were more modest than those presented by CYP2C9.
Discussion
Metal-based chemotherapy for cancer treatment has been broadly used for many decades, and cisplatin, an inorganic platinum complex, is one of the most widely used metal-based anticancer drugs [20]. Cisplatin is known to exert its anticancer effects by interacting with DNA and inducing programmed cell death and has proven to be a highly effective chemotherapeutic agent for treating a variety of cancers, especially testicular cancer, for which it has a >90 % cure rate [21]. Unfortunately, similar to most chemotherapeutic agents, cisplatin is nonselective and attacks other types of rapidly dividing cells in the body, such that nearly all people treated with cisplatin experience gastrointestinal problems, including intense nausea and vomiting [20].
The issue of drug resistance should also be considered. The cellular mechanisms leading to MDR are still not fully understood, and several factors seem to be of importance [22]. Most frequently discussed are (a) lowering of the intracellular concentration of the drug either by blocking uptake or increasing efflux, (b) increased rates of repair of the drug damage, and (c) accelerated rates of drug inactivation by protein binding (e.g., metallothionein and glutathione S-transferase) and conjugation to small molecules such as glutathione [7].
It has been shown that MDR cells overexpress certain efflux proteins, which leads to a significantly lower intracellular level of chemotherapeutical agents. The most prominent example of this superfamily of proteins, for which a similar mechanism of action is assumed, is P-glycoprotein (P-gp) or MDR protein (MRP1). MRP1 mainly transports neutral and charged molecules in unmodified form, but it can also accept metabolized substrates such as GSH, glucuronide, or sulfate conjugates [23, 24].
In this study, we have investigated the effects of platinum and ruthenium-based compounds on transmembrane transport proteins involved in drug efflux (MDR-1). Furthermore, the cytochrome P450 genes expression was also analyzed. The study presented here demonstrates that human chronic myelogenous leukemia cells K-562 expressed relatively high levels of P-gp, as detected by RT-PCR analyses (Fig. 5). This is in line with previous reports, in which MDR-1 expression was detected in K-562 tumor cells treated with cisPt. Our results suggest, that structurally related compounds might act relatively equally, inducing the expression of these proteins. K-562 tumor cells treated with the metal complexes cisPt and cisCRu(III), pretty similar compounds, have much higher levels of MDR-1 expression than cells treated with cisDRu(III), a broader and more complex compound.
All metal compounds used in this study induced specific members of cytochrome P450 families. The compounds cisPt, cisCRu(III), and cisDRu(III) enhanced CYP2C9 and CYP2C19 mRNAs expression levels, but they did not affect CYP3A4 mRNA expression levels (Fig. 6). CYPs isoforms are involved in the metabolism of a number of therapeutic drugs [25]. Pharmacogenetic variations in CYP2C family leads to inappropriate concentration of drugs and their metabolites, which may result in toxicity and risk of adverse drug reactions, or lack of therapeutic benefits [26]. Poor metabolizer (PM) and extensive metabolizer (EM) phenotypes has been demonstrated based on the ability to metabolize CYP2C substrates [27].
Our results suggest that cisDRu(III) induces CYP2C9 and CYP2C19 activity, in a manner much more intense than cisPt and cisCRu(III), and this activity could be involved in cisDRu(III) mechanism of action, since CYP2C family is known to be involved in the bioactivation of some environmental procarcinogen(s) and therapeutic agents to reactive DNA-binding metabolites [28–30]. Ruthenium complexes have been shown to have DNA-binding activities that can inhibit tumor cells growth. It has been demonstrated that ruthenium(III) complexes treatment causes DNA damage and oxidative stress in a number cancer cells [8, 17, 31].
Cell death under physiological conditions usually occurs via apoptosis. Morphologically, the most obvious characteristics of this form of cell death are cytoplasmatic and nuclear condensation, followed by internucleosomal DNA cleavage, membrane blebbing, and finally cell fragmentation [32]. Cell death due to apoptosis has received much attention, since it has been found that many chemotherapeutic drugs induce apoptosis in a variety of tumor cell [33].
The mechanisms of apoptosis mainly involve two signaling pathways identified according to the initiator caspase: the death receptor pathway involving caspase 8 (extrinsic), and the mitochondrial pathway (intrinsic), in which various signals can trigger the release of harmful proteins by mitochondria into the cytoplasm, leading to activation of caspase 9. Both pathways result in the downstream activation of caspase 3. Caspase 3 is able to cleave a variety of substrates, thereby contributing to the typical morphological and biochemical features observed in apoptosis inducing DNA fragmentation [34–37].
In the present study, our results showed clearly that cisPt, cisCRu(III), and cisDRu(III), induced apoptosis in K-562 tumor cells as evidenced by caspase 3 activation. cisDRu(III) elevated caspase 3 activity significantly in K-562 cells relative to the untreated control. However, only a slight increase in caspase 8 and caspase 9 activations was observed in treated K-562 cells. This result could be related to the fact that caspase 8 and caspase 9 are considered to be an important initiating event in apoptosis, whereas caspase 3 is involved in the effector phase of the apoptotic process [38]. Based on this evaluation, it is possible that caspases play an important role in the activation and executioner phase of platinum and ruthenium compound-induced apoptosis. Several studies have shown that ruthenium complexes, such as Nami-A, KP1019, and RAPTA-C, induce apoptosis through caspase activation, particularly caspase 3 [39, 40].
In summary, the data presented here clearly show that cisPt, cisCRu(III), and cisDRu(III) induces apoptosis in human K562 cells, as verified by caspase 3 activation. Although some genes that confer multidrug resistance are known, it is clear that many other genes remain to be identified. Based on this investigation, we propose that cytochrome P450 genes represent a useful chemosensitivity marker in K-562 cells. We plan to investigate other cell lines and other P450 proteins that may be associated with in its role in drug resistance, since the mechanisms by which ruthenium complexes induce cytotoxicity and apoptosis on tumor cell lines may not only be by the consequence of direct DNA binding and damage, but also by the interactions with a myriad of proteins like cytochrome P450, P-gp, and caspases; via oxidative stress promotion, reduction of MDR-1 phenotype and apoptosis induction via extrinsic activation pathway [41]. It is anticipated that the continued identification and characterization of novel mechanisms of drug resistance will enable the development of a new generation of anticancer drugs that increase cancer sensitivity and/or represent more effective chemotherapeutic agents.
References
Pereira FC, Lima AP, Vilanova-Costa CAST, Pires WCP, Ribeiro ASBB, Pereira LCG, Pavanin LA, dos Santos WB, Silveira-Lacerda EP (2014) Cytotoxic effects of the compound cis-tetraammine(oxalato)ruthenium(III) dithionate on K-562 human chronic myelogenous leukemia cells. Springer Plus 3:301
Deininger MW (2008) Chronic myeloid leukemia: a historical perspective. American Society of Hematology Education Program Book, 50th Anniversary Review 418
Srabanti R, Jayashree B, Labanya M, Kausik P, Dipyaman G, Sandip B, Monidipa G, Nabendu B, Utpal C, Santu B (2009) N-acetyl cysteine enhances imatinib-induced apoptosis of Bcr-Abl+ cells by endothelial nitric oxide synthase-mediated production of nitric oxide. Apoptosis 14:298–308
Deininger MWN, Goldman JM, Melo JV (2000) The molecular biology of chronic myeloid leukemia. Blood 96:3343–3356
Mahon FX, Belloc F, Lagarde V, Chollet C, Moreau-Gaudry F, Reiffers J, Goldman JM, Melo JV (2003) MDR1 gene overexpression confers resistance to imatinib mesylate in leukemia cell line models. Blood 101(6):2368–2373
Runge D, Kohler C, Kostrubsky VE, Jager D, Lehmann T, Runge DM, May U, Stolz DB, Strom SC, Fleig WE, Michalopoulos GK (2000) Induction of cytochrome P450 (CYP)1A1, CYP1A2, and CYP3A4 but not of CYP2C9, CYP2C19, multidrug resistance (MDR-1) and multidrug resistance associated protein (MRP-1) by prototypical inducers in human hepatocytes. Biochem Biophys Res Commun 273:333–341
Coburger C, Lage H, Molnár J, Hilgeroth A (2009) Impact of novel MDR modulators on human cancer cells: reversal activities and induction studies. Pharm Res 26(1)
Assef Y, Rubio F, Coló G, del Mónaco S, Costas MA, Kotsias BA (2009) Imatinib resistance in multidrug-resistant K562 human leukemic cells. Leuk Res 33(5):710–716
Alama A, Tasso B, Novelli F, Sparatore F (2009) Organometallic compound in oncology: implications of novel organotins as antitumor agents. Drug Discov Today 14:500–508
Dorcier A, Ang WH, Bolaño S, Gonsalvi L, Juillerat-Jeannerat L, Laurenczy G, Peruzzini M, Phillips AD, Zanobini F, Dyson PJ (2006) In vitro evaluation of rhodium and osmium RAPTA analogues: the case for organometallic anticancer drugs not based on ruthenium. Organometallics 25:4090–4096
Stordal B, Pavlakis N, Davey R (2007) A systematic review of platinum and taxane resistance from bench to clinic: an inverse relationship. Cancer Treat Rev 33(8):688–703
Jirsova K, Mandys V, Gispen WH, Bar PR (2006) Cisplatin-induced apoptosis in cultures of human Schwann cell. Neurosci Lett 392:22–26
Sava G, Bergamo A (2000) Ruthenium-based compounds and tumour growth control (review). Int J Oncol 17:353–365
Vock CA, Ang WH, Scolaro C, Phillips AD, Lagopoulos L, Juillerat-Jeanneret L, Sava G, Scopelliti R, Dyson PJ (2007) Development of ruthenium antitumor drugs that overcome multidrug resistance mechanisms. J Med Chem 50(9):2166–2175
Pavanin LA, Giesbrecht E, Tfouni E (1985) Synthesis and properties of the ruthenium(II) complexes cis-Ru(NH3)4(isn)L2+ spectra and reduction potentials. Inorg Chem 24:4444–4446
Pereira FC, Vilanova-Costa CAST, Lima AP, Ribeiro ASBB, da Silva HD, Pavanin LA, Silveira-Lacerda EP (2009) Cytotoxic and genotoxic effects of cis-tetraammine(oxalato)ruthenium(III) dithionate on the root meristem cells of Allium cepa. Biol Trace Elem Res 128(3):258–268
Silveira-Lacerda EP, Vilanova-Costa CAST, Pereira FC, Hamaguchi A, Pavanin LA, Goulart LR, Homsi-Brandenburgo MI, Santos WB, Soares AM, Nomizo A (2010) The ruthenium complex cis-(dichloro)tetraammineruthenium(III) chloride presents immune stimulatory activity on human peripheral blood mononuclear cells. Biol Trace Elem Res 133:270–283
Mosman T (1983) Rapid colorimetric assay for cellular growth and survival: application to proliferation and cytotoxicity assays. J Immunol Methods 16:55–63
Lobner D (2000) Comparison of the LDH and MTT assays for quantifying cell death: validity for neuronal apoptosis. J Neurosci Methods 96:147–152
Alderden RA, Mellor HR, Modok S, Hambley TW, Callaghan R (2006) Cytotoxic efficacy of an anthraquinone linked platinum anticancer drug. Biochem Pharmacol 71:1136–1145
Zhang CX, Lippard SJ (2003) New metal complexes as potential therapeutics. Curr Opin Chem Biol 7(4):481–489
Ang WH, Khalaila I, Allardyce CS, Juillerat-Jeanneret L, Dyson PJ (2005) Rational design of platinum(IV) compounds to overcome glutathione-S-transferase mediated drug resistance. J Am Chem Soc 127:1382–1383
Marzolini C, Paus E, Buclin T, Kim RB (2004) Polymorphisms in human MDR1 (P-glycoprotein): recent advances and clinical relevance. Clin Pharmacol Ther 75:13–33
Fischer V, Einolf HJ, Cohen D (2005) Efflux transporters and their clinical relevance. Min Rev Med Chem 5:183–195
Goldstein JA (2001) Clinical relevance of genetic polymorphisms in the human CYP2C subfamily. Br J Clin Pharmacol 52:349–355
Rodriguez-Antona C, Ingelman-Sundberg M (2006) Cytochrome P450 pharmacogenetics and cancer. Oncogene 25:1679–1691
Tanaka E (1999) Update: genetic polymorphism of drug metabolizing enzymes in humans. J Clin Pharm Ther 24:323–329
Tsuneoka Y, Fukushima K, Matsuo Y, Ichikawa Y, Watanabe Y (1996) Genotype analysis of the CYP2C19 gene in the Japanese population. Life Sci 59:1711–1715
Xing SW, Qing CS (2004) Frequencies of poor metabolizers of cytochrome P450 2C19 in esophagus cancer, stomach cancer, lung cancer and bladder cancer in Chinese population. World J Gastroenterol 10:1961–1963
Yoshiyuki Y, Ken-ichi F, Nakayama K, Suzuki A, Nakamura K, Yamazaki H, Kamataki T (2004) Establishment of ten strains of genetically engineered Salmonella typhimurium TA1538 each co-expressing a form of human cytochrome P450 with NADPH-cytochrome P450 reductase sensitive to various promutagens. Mutat Res 562:151–162
Menezes CSR, Gebrim LC, Ávila VMR, Ferreira MJ, Vieira CU, Pavanin LA, Homsi-brandeburgo MI, Hamaguchi A, Silveira-Lacerda EP (2007) Analysis in vivo of antitumor activity, cytotoxicity and interaction between plasmid DNA and the cis-dichlorotetramineruthenium(III) chloride. Chem Biol Interact 167:116–124
Wyllie AH, Kerr JFR, Currie AR (1980) Cell death: the significance of apoptosis. Int Rev Cytol 68:251–306
Silveira-Lacerda EP, Vilanova-Costa C, Hamaguchi A, Pavanin LA, Goulart LR, Homsi-brandeburgo MI, Santos WB, Soares AM, Nomizo A (2010) The ruthenium complex cis-(dichloro)tetraammineruthenium(III) chloride presents selective cytotoxicity against murine B cell lymphoma (A-20), murine ascitic sarcoma 180 (S-180), human breast adenocarcinoma (SK-BR-3), and human T cell leukemia (Jurkat) tumor cell lines. Biol Trace Elem Res 135:98–111
Cohen GM (1997) Caspases: the executioners of apoptosis. Biochem J 326:1–16
Kaufmann SH, Earnshaw WC (2000) Induction of apoptosis by cancer chemotherapy. Exp Cell Res 256(1):42–49
Kaufmann SH, Hengartner MO (2001) Programmed cell death: alive and well in the new millennium. Trends Cell Biol 11(12):526–534
Fesik SW (2005) Promoting apoptosis as a strategy for cancer drug discovery. Nature 5:876–885
Shi Y (2002) Mechanisms of caspase activation and inhibition during poptosis. Mol Cell 9:459–470
Kapitza S, Jakupec MA, Uhl M, Keppler BK, Marian B (2005) The heterocyclic ruthenium(III) complex KP1019 (FFC14A) causes DNA damage and oxidative stress in colorectal tumor cells. Cancer Lett 226:115–121
Chatterjee S, Kundu S, Bhattacharya A, Christian G, Hartinger CG, Dyson PJ (2008) The ruthenium(II)–arene compound RAPTA-C induces apoptosis in EAC cells through mitochondrial and p53–JNK pathways. JBIC J Biol Inorg Chem 13:1149–1155
Vilanova-Costa CAST, Porto HKP, Pereira FC, Lima AP, dos Santos WB, Silveira-Lacerda EP (2014) The ruthenium complexes cis-(dichloro)tetramineruthenium(III) chloride and cis-tetraammine(oxalato)ruthenium(III) dithionate overcome resistance inducing apoptosis on human lung carcinoma cells (A549). Biometals 27:459–469
Acknowledgments
The authors gratefully acknowledge the financial support of Research and Projects Financing (FINEP) (Grant No. 01.06.0941.00/CT-Saúde to Elisângela de Paula Silveira-Lacerda) and Foundation for the Support of Research in the State of Goias (FAPEG). Coordination for the Advancement of Higher Education Staff (CAPES) through fellowship to Cesar Augusto Sam Tiago Vilanova-Costa, Hellen Karine Paes Porto and Lucas Carlos Gomes Pereira.
Funding Sources
There are no financial or personal interests that might be viewed as inappropriate influences on the work presented herein. This manuscript was completely financed by governmental and nonprofit institutions, the Brazilian National Counsel of Technological and Scientific Development (CNPq), Research and Projects Financing (FINEP), Coordination for the Advancement of Higher Education Staff (CAPES), and Foundation for the Support of Research in the State of Goias (FAPEG).
Ethical Approval
No studies involving humans or experimental animals were conducted in this work. The human chronic myelogenous leukemia K-562 cells were purchased from the American Type Culture Collection (ATCC, Rockville, MD, USA) and cultured in vitro.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vilanova-Costa, C.A.S.T., Porto, H.K.P., Pereira, L.C.G. et al. MDR1 and Cytochrome P450 Gene-Expression Profiles as Markers of Chemosensitivity in Human Chronic Myelogenous Leukemia Cells Treated with Cisplatin and Ru(III) Metallocomplexes. Biol Trace Elem Res 163, 39–47 (2015). https://doi.org/10.1007/s12011-014-0133-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-014-0133-2