Abstract
Introduction
Imatinib, a small-molecule inhibitor of the Bcr-Abl kinase, is a successful drug for treating chronic myeloid leukemia (CML). Bcr-Abl kinase stimulates the production of H2O2, which in turn activates Abl kinase. We therefore evaluated whether N-acetyl cysteine (NAC), a ROS scavenger improves imatinib efficacy.
Materials and methods
Effects of imatinib and NAC either alone or in combination were assessed on Bcr-Abl+ cells to measure apoptosis. Role of nitric oxide (NO) in NAC-induced enhanced cytotoxicity was assessed using pharmacological inhibitors and siRNAs of nitric oxide synthase isoforms. We report that imatinib-induced apoptosis of imatinib-resistant and imatinib-sensitive Bcr-Abl+ CML cell lines and primary cells from CML patients is significantly enhanced by co-treatment with NAC compared to imatinib treatment alone. In contrast, another ROS scavenger glutathione reversed imatinib-mediated killing. NAC-mediated enhanced killing correlated with cleavage of caspases, PARP and up-regulation and down regulation of pro- and anti-apoptotic family of proteins, respectively. Co-treatment with NAC leads to enhanced production of nitric oxide (NO) by endothelial nitric oxide synthase (eNOS). Involvement of eNOS dependent NO in NAC-mediated enhancement of imatinib-induced cell death was confirmed by nitric oxide synthase (NOS) specific pharmacological inhibitors and siRNAs. Indeed, NO donor sodium nitroprusside (SNP) also enhanced imatinib-mediated apoptosis of Bcr-Abl+ cells.
Conclusion
NAC enhances imatinib-induced apoptosis of Bcr-Abl+ cells by endothelial nitric oxide synthase-mediated production of nitric oxide.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Imatinib also known as STI571 or Gleevec is the most widely studied p210Bcr-Abl kinase inhibitor and a successful drug for treating CML [1, 2]. Bcr-Abl kinase stimulates the production of reactive oxygen species (ROS) [3, 4]. ROS, in turn, induces activation of Abl kinase [5, 6]. Since ROS activates Abl kinase, we hypothesized that Bcr-Abl-induced endogenous ROS may counteract the activity of Bcr-Abl kinase inhibitor imatinib. A ROS scavenger may therefore enhance imatinib-induced cell death. Thus, experiments were designed to see the effect of NAC, a ROS scavenger [7], on imatinib-induced cell death.
Our data indicate that NAC, as hypothesized, enhanced imatinib-induced cell death. However, experiments to understand the mechanism of NAC-induced enhanced cytotoxicity did not support our hypothesis. Although NAC was able to decrease intracellular ROS, the precise mechanism of observed enhancement of cell death was mainly due to NAC-induced increased expression of endothelial nitric oxide synthase and consequent production of nitric oxide.
Materials and methods
Cell culture and reagents
Bcr-Abl+ CML cell line K562 [8] was purchased from the American Type Culture Collection (Manassas, USA). Additional Bcr-Abl+ CML cell lines KU812 [9] and KCL-22 [10] were generously provided by Dr. Carlo Gambacorti-Passerini, Instituto Nazionale Tumori, Milan, Italy. Unless otherwise stated, all cells were cultured in RPMI-1640 medium containing 10% fetal bovine serum and 100 U/ml penicillin–streptomycin (Life Technologies, USA). Antibodies were purchased from the following suppliers: Antibodies to c-Abl (rabbit polyclonal IgG), Bax (rabbit polyclonal IgG), c-IAP1 (rabbit polyclonal IgG), Bcl-XL (mouse monoclonal, IgG1) and Bcl-2 (mouse monoclonal, IgG1) were purchased from Santa Cruz Biotechnology, USA. Antibodies to cleaved poly ADP-ribose polymerase (PARP; mouse monoclonal, IgG1), endothelial nitric oxide synthase (eNOS; mouse monoclonal, IgG1), inducible nitric oxide synthase (iNOS; mouse monoclonal, IgG1) and neuronal nitric oxide synthase (nNOS, mouse monoclonal, IgG2a) were from BD Biosciences, USA. Antibodies to cleaved caspase 3 (rabbit polyclonal IgG), cleaved caspase 8 (mouse monoclonal IgG1), cleaved caspase 9 (rabbit polyclonal IgG), phospho-c-Abl (Tyr 245, rabbit polyclonal IgG) were from Cell Signaling Technologies, USA. N-acetyl-l-cysteine (NAC), mitochondrial membrane potential-sensitive fluorescent dye 5,5′,6,6′-Tetrachloro-1,1′,3,3′-tetraethylbenzimidazolylcarbocyanine Iodide (JC-1), hydrogen peroxide sensitive dye 2′–7′-dichlorodihydrofluorescein (DCF), cell-permeable photo-stable nitric oxide fluorescent indicator 3-amino, 4-amino methyl-2′,7′-difluoro fluorescein diacetate (DAF-FM), sodium nitroprusside (SNP, a nitric oxide inducer), S-methyl-l-thiocitrulline (SMTC, pharmacological inhibitors of nNOS), Aminoguanidine (AG, pharmacological inhibitor of iNOS), L-n 5-(1-Iminoethyl) ornithine dihydrochloride (l-nio, pharmacological inhibitor of eNOS) and glutathione monoethyl ester were from Calbiochem, USA. Imatinib Mesylate in its generic form was obtained from Natco Pharma Ltd. Hyderabad, India.
Clinical samples
Fresh peripheral blood samples were donated by three chronic myeloid leukemia patients with stable phase of the disease admitted to the Institute of Hematology and Transfusion Medicine, Medical College, Kolkata before receiving any treatment. All three patients were Philadelphia Chromosome positive as determined by bone marrow cytogenetic analysis. Peripheral blood samples were collected with due approval from the Human Ethics Committee of the respective institutes and all experiments with human blood were conducted under an approved institutional Human Ethics Committee protocol (Informed consent was provided according to the Declaration of Helsinki). Mononuclear cells were separated by Ficoll/Hypaque density gradient centrifugation.
In vitro generation of imatinib-resistant CML cell line, K562R
Imatinib resistant CML cell line K562R was generated from imatinib-sensitive CML cell line K562 following a published method [11]. Briefly K562 cells were incubated with increasing concentrations of imatinib, and surviving cells were collected by centrifugation and treated with two-fold higher concentrations of imatinib.
Cell viability assays
K562, K562R, KU812, KCL22 (1 × 104 cells/well) in triplicate were incubated in 0.2 ml RPMI 1640-10% fetal calf serum containing varying concentrations of imatinib and NAC. After 72 h of culture, cells were collected by centrifugation (at 1000 g for 5 min). Cell viability was determined by the trypan blue exclusion assay [12]. At least 200 cells were examined in each sample. Viability of primary CML cells was determined in the same way except that recombinant human granulocyte macrophage colony-stimulating factor (rhGM-CSF, 100 ng/ml; R & D Systems, USA) was included [12].
Annexin V–PI binding assays
Cells were seeded at 1.5 × 105 cells/ml in the presence or absence of NAC and imatinib either alone or in combination for 72 h. Evaluation of apoptosis by the annexin V–propidium iodide (PI) binding assay was performed using the annexin V–fluorescein isothiocyanate (FITC) Apoptosis Detection Kit (BD Biosciences, USA) according to the supplier’s instructions. Analysis was performed in a flow cytometer (BD LSR, Becton Dickinson, USA). Apoptotic cells stained by annexin V are in the lower-right quadrant. Late-stage apoptotic cells stained with both annexin V and PI are in the upper-right quadrant.
Immunoblotting
Cells (1.0 × 105 cells/ml) after receiving treatment as indicated in the figure legends were collected by centrifugation, and boiled for 5 min in sodium dodecyl sulfate (SDS) buffer. Aliquots containing 80 μg total cellular protein were separated by SDS–polyacrylamide gel electrophoresis (PAGE) containing 10% polyacrylamide, transferred to nitrocellulose, and probed with primary antibodies indicated in the figure legends followed by horseradish peroxidase-coupled secondary antibody [12].
Flow cytometry
Treated and untreated cells (as indicated in the figure legends) were immediately fixed with 4% paraformaldehyde, permeabilized by fluorescence-activated cell-sorter permeabilizing solution (BD Biosciences, USA). Before staining, permeabilized cells were treated with heat inactivated 2% normal goat serum to block nonspecific staining. After blocking, cells were stained with indicated antibodies for 30 min. Isotype-matched control mouse antibodies and normal rabbit sera were used as controls for specific mouse and rabbit antibodies, respectively. After washing, cells were incubated with multiple adsorbed FITC-conjugated secondary antibodies, washed, and analyzed in a flow cytometer.
Measurement of intracellular nitric oxide
To measure changes in intracellular nitric oxide levels, treated and untreated cells were incubated with the cell permeable dye DAF-FM DA (3 μM) for 60 min at 37°C [13]. Cells were then washed with phosphate buffer saline (PBS) and analyzed in a flow cytometer.
Measurement of intracellular ROS
Intracellular H2O2 generation was measured by flow cytometry following staining with DCF [14]. Treated and untreated cells were incubated with DCF (10 μM) for 20 min, washed with PBS and analyzed in a flow cytometer.
Measurement of mitochondrial membrane potential
Mitochondrial membrane potential was measured using mitochondrial membrane potential sensitive fluorescent dye JC-1 [15]. Treated and untreated cells were incubated with JC-1 (10 μM) for 30 min, washed with PBS and analyzed in a flow cytometer.
siRNA knockdown
K562 cells were transfected with control siRNA and siRNAs for nNOS, iNOS or eNOS (purchased from Santa Cruz Biotechnology, USA). Transfections were carried out following the manufacturer’s (Santa Cruz Biotechnology, USA) instructions. The transfection reagent used for siRNA transfection was purchased from Santa Cruz Biotechnology (siRNA Transfection Reagent: sc-29528). 48 h post transfection, the cells were treated with NAC and imatinib as indicated.
Semiquantitative RT-PCR
Total RNA was isolated with RNA extraction reagent TRIzol (Life technologies). The superscript one-step RT-PCR kit (Life technologies) was used for reverse transcription of mRNA into DNA and for PCR with 500 ng total RNA as described elsewhere [16]. The sequences of the oligonucleotide primers used were as follows: actin, Sense: 5′-Atg gAT gAT gAT ATC gCC gCg-3′, Antisense: 5′-CTA gAA gCA TTT gCg gTg gAC-3′ and eNOS, Sense: 5′-ACC TgC AAA gCA gCA AgT CCA Cg-3′, Antisense: 5′-CCg AAC ACC AAA gTC ATg ggA gT-3′ [17].
Statistical analysis
Paired Student’s t-test for statistical analysis was performed using the web-based service http://www.physics.csbsju.edubin/stats/paired_t-test.
Results
NAC potentiates imatinib-induced cell death in Bcr-Abl+ CML cell lines and primary cells from CML patients
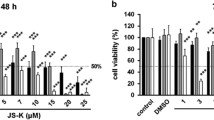
We evaluated the effects of the H2O2 scavenger NAC on imatinib-induced cell death in a panel of imatinib-sensitive Bcr-Abl+ CML cell lines, in vitro-generated imatinib-resistant CML cell line K562R and primary cells from three CML patients by cell viability and annexin V–PI binding assays. As expected, NAC reduced the level of intracellular H2O2 in a dose dependant manner both in the presence and absence of 0.25 μM imatinib (Fig. 1a). Imatinib alone at this concentration reduced intracellular H2O2 concentration only marginally (Fig. 1a). Addition of NAC alone (upto a concentration of 5.0 mM) has no effects on the cell survival (Fig. 1b). However, combined treatment of NAC and imatinib significantly enhanced imatinib-mediated killing of K562 cells (Fig. 1b). The combined effect became significant when imatinib was used at the concentrations of 0.25 μM or higher and NAC was used at the concentrations of 2.5 mM and higher (Fig. 1b). However, another ROS scavenger glutathione did not enhance imatinib-mediated killing rather partially reversed the effect of imatinib (Fig. 1c). Addition of exogenous H2O2 in the coculture did not have any effect on the NAC-mediated enhancement of imatinib-induced killing (Fig. 1d). Combined treatment of NAC and imatinib also significantly enhanced imatinib-mediated killing of in vitro generated imatinib-resistant CML cell line, K562R (Fig. 1e), two additional imatinib-sensitive CML cell lines KU812, KCL-22 (Fig. 1f) and primary cells from three CML patients (Fig. 1g). Development of K562R as imatinib-resistant cell line is shown in the inset of Fig. 1e. NAC induced enhancement of imatinib mediated cell death was attributed to apoptosis and necrosis (Fig. 2a, b). NAC-mediated enhancement of imatinib-induced killing was further confirmed by cleavage of caspases 8, 3, 9 and PARP in K562 cells both by flow cytometry (Fig. 3a) and by western blot of cleaved caspase 3 and cleaved PARP (Fig. 3b). NAC-mediated enhancement of imatinib-induced killing also correlated with enhanced up-regulation of pro-apoptotic protein Bax, and down-regulation of anti-apoptotic proteins like c-IAP1, Bcl-XL, and Bcl-2 (Fig. 4). Co treatment of NAC and imatinib also resulted in enhanced decrease in mitochondrial membrane potential in K562 cells compared to treatment with NAC or imatinib alone (Fig. 5).
N-acetyl cysteine enhances imatinib-mediated cell death of imatinib-sensitive/resistant Bcr-Abl+ CML cell lines and primary cells from CML patients. a N-acetyl cysteine reduces intracellular level of H2O2. K562 cells were incubated with graded concentrations of NAC in the presence and absence of imatinib (0.25 μM) for 24 h. Intracellular H2O2 was measured by DCF fluorescence. Data represent the mean ± SD of three experiments. *P < 0.01 compared to media treatment alone. b K562 cells were cultured in medium or with graded concentrations of NAC and imatinib either alone or in combination for 72 h and viability was determined by trypan blue dye exclusion assay. Data represent the mean ± SD of six experiments. *P < 0.05 compared to imatinib alone; **P < 0.01 compared to imatinib alone. c NAC but not glutathione enhances imatinib-mediated death of K562 cells. K562 cells were cultured with imatinib (0.25 μM) in the presence or absence of NAC (5.0 mM) or glutathione (5.0 mM) for 72 h and viability was determined by trypan blue dye exclusion assay. Data represent mean ± SD of six experiments. d Exogenous H2O2 does not reverse NAC-mediated enhancement of imatinib-induced cell death. K562 cells were cultured for 72 h with imatinib (0.25 μM) and NAC (5.0 mM) either alone or in combination in the presence and absence of graded concentrations (10 μM; 25 μM) of exogenous H2O2. Cell viability was determined by trypan blue dye exclusion. Data represent mean ± SD of six experiments. e Viability of imatinib resistant K562 cells (K562R) after indicated treatment for 72 h. Comparison of imatinib sensitivity of K562 and K562R cells is shown in the inset on the right. Data represent mean ± SD of six experiments. *P < 0.01 compared to treatment with imatinib alone. f Indicated Bcr-Abl+ CML cell lines were treated with imatinib in the presence and absence of NAC for 72 h. and cell viability was determined. Data represent the mean ± SD of six experiments. *P < 0.05 compared to imatinib alone. g Mononuclear cells from three Bcr-Abl+ CML patients were cultured in medium containing rhGM-CSF (100 ng/ml for 72 h) in the presence and absence of imatinib and NAC as indicated before determination of cell viability. Data represent the mean ± SD of three experiments. *P < 0.05 compared to imatinib treatment alone
NAC-induced enhancement of imatinib-mediated cell death is attributed to apoptosis and necrosis. a Bcr-Abl+ CML cell lines (K562, KU812, KCL-22) and K562R were treated with imatinib (0.25 μM for imatinib-sensitive cell lines and 2.0 μM for K562R) in the presence and absence of NAC (5.0 mM) for 72 h. Annexin V–PI binding assay was then performed using Annexin V-FITC apoptosis detection kit followed by analysis in a flow cytometer. Results are representative of three similar experiments. b Annexin V–PI binding assays on Bcr-Abl+ primary CML cells were performed in the same way except that rhGM-CSF (100 ng/ml) was included. Values in the quadrants represent percent positive cells
The effect of treatment with imatinib in the presence and absence of NAC on the cleavage of PARP, caspase 8, caspase 3 and caspase 9 in Bcr-Abl+ CML cell line. a Flow cytometric analysis. K562 cells were treated as indicated for 72 h, fixed, permeabilized, and stained with control antibodies (filled histograms) or antibodies to cleaved PARP, cleaved caspase–8, –3, –9 (solid lines). Values within the histograms represent the specific mean fluorescence intensity (MFI) after subtracting the respective control values. Data are representative of three similar experiments. b Immunoblots of cleaved caspase 3 and cleaved PARP in whole cell lysates of K562 cells following indicated treatments for 72 h. Data are representative of three similar experiments
Flow cytometric analysis showing the effect of treatment with imatinib in the presence and absence of NAC on the expression of pro- and anti-apoptotic proteins in K562 cells. Cells were treated as indicated for 72 h, fixed, permeabilized and stained with control antibodies (filled histograms) or antibodies to Bax, c-IAP1, Bcl-XL or Bcl-2 (solid lines). Values within histograms represent the specific MFI (after subtracting the respective control values). Results are representative of three similar experiments
NAC enhances imatinib-mediated depolarization of mitochondrial membrane potential. K562 cells were treated with imatinib (0.25 μM) in the presence and absence of NAC (5.0 mM) as indicated for 72 h and stained with the mitochondrial membrane potential-sensitive dye JC-1 and analyzed in a flow cytometer. The percentage of cells expressing green and red fluorescence is indicated per each condition tested. Results are representative of three similar experiments
NAC-induced enhancement of imatinib-mediated cell death correlates with NAC-mediated NO production
To understand the mechanism of NAC-mediated potentiation of imatinib-induced killing of Bcr-Abl+ cells, status of Bcr-Abl phosphorylation was evaluated in K562 cells in the presence and absence of NAC and imatinib. As evident from the Fig. 6a, combination of NAC with imatinib resulted in no further inhibition of phosphorylation of Bcr-Abl and unfused Abl proteins compared to imatinib alone. None of the reagents affected the expression of these proteins. The concentration of NAC (5.0 mM) that significantly potentiated imatinib-mediated cell death had no effect on Bcr-Abl phosphorylation when used alone. Thus, NAC does not potentiate imatinib-induced inhibition of Bcr-Abl phosphorylation.
Co-treatment with NAC does not affect imatinib-mediated inhibition of Bcr-Abl phosphorylation but enhances intracellular NO production. a Immunoblot analysis of Bcr-Abl phosphorylation in K562 cells treated with indicated concentrations of imatinib in the presence and absence of NAC (5.0 mM) for 24 h. Results are representative of three similar experiments. b Detection of intracellular NO in K562 cells after treatment with imatinib in the presence and absence of varying concentrations of NAC. K562 cells were treated as indicated for 24 h, stained with DAF-FM and analyzed in a flow cytometer. Data represent the mean ± SD of three experiments. c Detection of intracellular NO in K562R cells after treatment for 24 h. with imatinib in the presence and absence of NAC. Data represent the mean ± SD of six experiments. d NAC but not glutathione enhances NO production. K562 cells were cultured with imatinib in the presence and absence of NAC or glutathione for 24 h, stained with DAF FM and analyzed in flow cytometer. Data represent the mean ± SD of six experiments
N-acetyl cysteine has been reported to induce NO in vascular endothelial cells [18]. This reactive nitrogen species is capable of inducing apoptosis and necrosis [19]. We therefore evaluated the possible role of NO in NAC-mediated potentiation of imatinib-induced killing of imatinib-sensitive and imatinib-resistant BCR-Abl+ CML cells. NAC, in a dose-dependent manner, in the presence and absence of imatinib resulted in enhanced production of NO in imatinib-sensitive Bcr-Abl+ cells (Fig. 6b). Enhanced production of NO was also detectable by NAC in imatinib-resistant K562R cells both in the presence or absence of imatinib (Fig. 6c). However, glutathione neither potentiated imatinib-mediated killing of K562 cells (Fig. 1c) nor induced enhanced production of NO in this cell line irrespective of the presence of imatinib (Fig. 6d). Thus, NAC-mediated potentiation of imatinib-induced killing correlates with NAC-induced NO production.
NAC-induced upregulation of eNOS is responsible for NAC-mediated NO production
Next we investigated the source of NO that was detectable in the presence of NAC using two approaches (1) employing pharmacological inhibitors of nitric oxide synthase (NOS) isoforms and (2) knocking down NOS isoforms using siRNAs.
Pharmacological inhibitors, which preferentially inhibit different isoforms of NOS, were pre-incubated with K562 cells for 1 h before treatment with imatinib and NAC. Evaluation of apoptosis indicates that l-nio, a preferential inhibitor of endothelial nitric oxide synthase (eNOS) [20] but not SMTC or AG, preferential inhibitors of neuronal nitric oxide synthase (nNOS) [21] or inducible nitric oxide synthase (iNOS) [22] respectively reversed, virtually completely, NAC-mediated potentiation of imatinib-induced apoptosis (Fig. 7). Of note, none of these inhibitors has any effect on cell death induced by imatinib alone (results not shown).
NAC-mediated enhancement of imatinib-induced apoptosis is reversed in the presence of the pharmacological inhibitor of eNOS, not nNOS or iNOS. K562 cells were treated with imatinib (0.25 μM) and NAC (5.0 mM) either alone or in combination in the presence and absence of the pharmacological inhibitors of nNOS (SMTC, 100 μM), iNOS (AG, 200 μM) or eNOS (l-nio, 200 μM) for 72 h. Annexin V–PI binding assay was then performed followed by analysis in a flow cytometer. Results are representative of three similar experiments
To confirm this finding, K562 cells were transfected with control siRNA, eNOS siRNA, nNOS siRNA or iNOS siRNA and then treated with imatinib in the absence and presence of NAC. Transfection with control siRNA, eNOS siRNA, nNOS siRNA or iNOS siRNA did not affect cell viability in the presence or absence of imatinib alone (Fig. 8a). However, NAC-mediated potentiation of imatinib-induced cell death was reversed nearly completely in K562 cells transfected with eNOS siRNA but not with nNOS siRNA or iNOS siRNA (Fig. 8a). Transfection of K562 cells with NOS siRNAs brought down the respective proteins markedly (Fig. 8b). Of note, NAC treatment resulted in upregulation of only eNOS protein which continued to be detectable in the presence of imatinib and transfection with eNOS siRNA attenuated this upregulation (Fig. 8b). Expression of eNOS mRNA was also upregulated by NAC in the presence or absence of imatinib in K562 cells (Fig. 8c). Transfection with eNOS siRNA also attenuated NAC-mediated upregulation of intracellular NO (Fig. 8d). We also found that addition of a NO donor, sodium nitroprusside (SNP) [23], upregulated intracellular NO and potentiate imatinib-mediated apoptosis (Fig. 9).
Depletion of endogenous eNOS, not nNOS or iNOS by siRNA attenuates NAC-induced enhancement of imatinib-mediated apoptosis. a Effect of transfection with nNOS siRNA, iNOS siRNA or eNOS siRNA on NAC-induced potentiation of imatinib-mediated cell death. K562 cells were transfected with control siRNA, nNOS siRNA, iNOS siRNA or eNOS siRNA for 48 h. Cells were then treated with imatinib (0.25 μM) in the presence and absence of NAC (5.0 mM) for 72 h and viability was determined by trypan blue dye exclusion test. Results shown represent the mean ± SD of three experiments; *P < 0.05 compared to media or NAC treatment alone; **P < 0.01 compared to imatinib treatment alone. b NAC-induced enhanced expression of eNOS was attenuated by transfection with eNOS siRNA. K562 cells were transfected with control siRNA, nNOS siRNA, iNOS siRNA or eNOS siRNA for 48 h. Cells were then treated with imatinib (0.25 μM) in the presence and absence of NAC (5.0 mM) for 24 h and analyzed for nNOS, iNOS and eNOS proteins by immunoblot. Results are representative of three similar experiments. c eNOS mRNA expression in K562 cells as determined by RT-PCR after indicated treatment for 8 h. Results are representative of three similar experiments. d Effect of transfection with eNOS siRNA on enhancement of NO production by treatment with NAC in the presence and absence of imatinib. K562 cells were transfected with control siRNA or eNOS siRNA for 48 h. Cells were then treated with imatinib in the presence and absence of NAC for 24 h, stained with DAF-FM and analyzed in flow cytometer. The results are representative of three similar experiments
Co-treatment with nitric oxide donor sodium nitroprusside (SNP) enhances imatinib-mediated apoptosis of K562 cells. Left panel, Κ562 cells were treated with medium or with SNP (800 μM) in the presence and absence of imatinib (0.25 μM) for 72 h. Annexin V–PI binding assays were then performed. The results are representative of three similar experiments. Right panel, SNP treatment enhances intracellular NO production. K562 cells were treated with imatinib (0.25 μM) in the presence and absence SNP (800 μM) for 24 h, stained with DAF-FM and analyzed in a flow cytometer. The results are representative of three similar experiments
Discussion
In the current study we show that imatinib-induced cell death may be significantly increased by co-treatment with NAC in imatinib-sensitive Bcr-Abl+ CML cell lines, primary cells from CML patients and in an in vitro generated imatinib-resistant CML cell line.
Although imatinib is the frontline therapy for CML, resistance is increasingly encountered. In this context, our finding is significant since co-treatment with NAC significantly enhances imatinib-induced cell death not only of imatinib-sensitive Bcr-Abl+ cell lines and primary cells from CML patients but also of a imatinib-resistant Bcr-Abl+ CML cell line.
Conflicting literature exists on the effect of NAC on Bcr-Abl+ cells. Some studies suggested growth-enhancing effect of NAC on Bcr-Abl+ cells [15] while others suggested otherwise [18, 19]. In our experiment, NAC alone upto a concentration of 5.0 mM has no effect on the viability of Bcr-Abl+ CML cell lines or primary cells.
N-acetyl cysteine-mediated enhancement of sensitivity of Bcr-Abl+ cells to imatinib was attributed to both apoptosis and necrosis which was supported by a number of biochemical assays i.e., decrease in mitochondria membrane potential, cleavage of PARP, caspases and up-regulation and down-regulation of pro and anti-apoptotic proteins respectively. Bcr-Abl induces ROS [3], which in turn activates Abl [5]. We therefore evaluated the possibility that in the condition of co-treatment, NAC may further inhibit Bcr-Abl phosphorylation compared to imatinib alone leading to enhanced cell death. This possibility was ruled out by comparing phosphorylation status of Bcr-Abl in co-treatment cultures compared to treatment with NAC or imatinib alone. To evaluate whether scavenging of intracellular ROS was responsible for NAC-mediated potentiation of imatinib-mediated cell death, H2O2 was added exogenously in one experiment and another ROS scavenger glutathione was included in an additional experiment. Exogenous H2O2 did not reverse NAC-mediated potentiation of imatinib-mediated cell death. Unlike NAC, glutathione did not enhance imatinib-mediated cell death. Taken together, our data suggest that scavenging of intracellular ROS is not responsible for NAC-mediated potentiation of imatinib-mediated cell death.
Nitric oxide is capable of inducing both apoptosis and necrosis in a variety of cells [9]. We therefore investigated the role of NO in the enhanced cell death under co treatment (NAC plus imatinib) condition. Varying concentrations of imatinib alone did not appreciably alter the level of intracellular NO in Bcr-Abl+ CML cell lines. However, treatment with NAC significantly increased the level of intracellular NO in these cells in a dose dependent manner, which continued to be detectable in the presence of imatinib.
Use of pharmacological inhibitors and siRNAs of different isoforms of NOS indicate that eNOS-induced NO plays a key role in NAC-mediated enhancement of imatinib-induced cell death.
In summary, our study showed that co-treatment with NAC significantly enhanced imatinib-mediated killing of Bcr-Abl+ cells. NAC-induced upregulation of eNOS leading to enhancement of intracellular NO production rather than downregulation of intracellular ROS appears to be responsible for this effect. We conclude that treatment of CML patients with NAC plus imatinib merits clinical evaluation.
Abbreviations
- NAC:
-
N-acetyl cysteine
- CML:
-
Chronic myeloid leukemia
- NO:
-
Nitric oxide
- NOS:
-
Nitric oxide synthase
- ROS:
-
Reactive oxygen species
- SNP:
-
Sodium nitroprusside
References
Druker BJ, Talpaz M, Resta DJ, Peng B, Buchdunger E, Ford JM et al (2001) Efficacy and safety of a specific inhibitor of the BCR-ABL tyrosine kinase in chronic myeloid leukemia. N Engl J Med 344:1031–1037. doi:10.1056/NEJM200104053441401
O’Brien SG, Guilhot F, Larson RA, Gathmann I, Baccarani M, Cervantes F et al (2003) Imatinib compared with interferon and low-dose cytarabine for newly diagnosed chronic-phase chronic myeloid leukemia. N Engl J Med 348:994–1004. doi:10.1056/NEJMoa022457
Sattler M, Verma S, Shrikhande G, Byrne CH, Pride YB, Winkler T et al (2000) The BCR/ABL tyrosine kinase induces production of reactive oxygen species in hematopoietic cells. J Biol Chem 275:24273–24278. doi:10.1074/jbc.M002094200
Koptyra M, Falinski R, Nowicki MO, Stoklosa T, Majsterek I, Nieborowska-Skorska M et al (2006) BCR/ABL kinase induces self-mutagenesis via reactive oxygen species to encode imatinib resistance. Blood 108:319–327. doi:10.1182/blood-2005-07-2815
Sun X, Majumder P, Shioya H, Wu F, Kumar S, Weichselbaum R et al (2000) Activation of the cytoplasmic c-Abl tyrosine kinase by reactive oxygen species. J Biol Chem 275:17237–17240. doi:10.1074/jbc.C000099200
Kumar S, Mishra N, Raina D, Saxena S, Kufe D (2003) Abrogation of the cell death response to oxidative stress by the c-Abl tyrosine kinase inhibitor STI571. Mol Pharmacol 63:276–282. doi:10.1124/mol.63.2.276
Storozhevykh TP, Senilova YE, Persiyantseva NA, Pinelis VG, Pomytkin IA (2007) Mitochondrial respiratory chain is involved in insulin-stimulated hydrogen peroxide production and plays an integral role in insulin receptor autophosphorylation in neurons. BMC Neurosci 8:84–90. doi:10.1186/1471-2202-8-84
Lozzio CB, Lozzio BB (1975) Human chronic myelogenous leukemia cell-line with positive Philadelphia chromosome. Blood 45:321–334
Kishi K (1985) A new leukemia cell line with Philadelphia chromosome characterized as basophil precursors. Leuk Res 9:381–390. doi:10.1016/0145-2126(85)90060-8
Kubonishi I, Miyoshi I (1983) Establishment of a Ph1 chromosome-positive cell line from chronic myelogenous leukemia in blast crisis. Int J Cell Cloning 1:105–117
Donato NJ, Wu JY, Stapley J, Gallick G, Lin H, Arlinghaus R et al (2003) BCR-ABL independence and LYN kinase overexpression in chronic myelogenous leukemia cells selected for resistance to STI571. Blood 101:690–698. doi:10.1182/blood.V101.2.690
Bandyopadhyay G, Biswas T, Roy KC, Mandal S, Mandal C, Pal BC et al (2004) Chlorogenic acid inhibits Bcr-Abl tyrosine kinase and triggers p38 mitogen-activated protein kinase-dependent apoptosis in chronic myelogenous leukemic cells. Blood 104:2514–2522. doi:10.1182/blood-2003-11-4065
Trachootham D, Zhou Y, Zhang H, Demizu Y, Chen Z, Pelicano H et al (2006) Selective killing of oncogenically transformed cells through a ROS-mediated mechanism by beta-phenylethyl isothiocyanate. Cancer Cell 10:241–252. doi:10.1016/j.ccr.2006.08.009
Polyak K, Xia Y, Zweier JL, Kinzler KW, Vogelstein B (1997) A model for p53-induced apoptosis. Nature 389:300–305. doi:10.1038/38525
Bortner CD, Cidlowski JA (1999) Caspase independent/dependent regulation of K(+), cell shrinkage, and mitochondrial membrane potential during lymphocyte apoptosis. J Biol Chem 274:21953–21962. doi:10.1074/jbc.274.31.21953
Roy KC, Bandyopadhyay G, Rakshit S, Ray M, Bandyopadhyay S (2004) IL-4 alone without the involvement of GM-CSF transforms human peripheral blood monocytes to a CD1a(dim), CD83(+) myeloid dendritic cell subset. J Cell Sci 117:3435–3445. doi:10.1242/jcs.01162
Gilchrist M, McCauley SD, Befus AD (2004) Expression, localization, and regulation of NOS in human mast cell lines: effects on leukotriene production. Blood 104:462–469. doi:10.1182/blood-2003-08-2990
Xia Z, Liu M, Wu Y, Sharma V, Luo T, Ouyang J et al (2006) N-acetylcysteine attenuates TNF-alpha-induced human vascular endothelial cell apoptosis and restores eNOS expression. Eur J Pharmacol 550:134–142. doi:10.1016/j.ejphar.2006.08.044
Shen HM, Liu Z (2006) JNK signaling pathway is a key modulator in cell death mediated by reactive oxygen and nitrogen species. Free Radic Biol Med 40:928–939. doi:10.1016/j.freeradbiomed.2005.10.056
Corbett JA, McDaniel ML (1996) The use of aminoguanidine, a selective iNOS inhibitor, to evaluate the role of nitric oxide in the development of autoimmune diabetes. Methods 10:21–30. doi:10.1006/meth.1996.0074
Belik J, Jankov RP, Pan J, Tanswell AK (2004) Peroxynitrite inhibits relaxation and induces pulmonary artery muscle contraction in the newborn rat. Free Radic Biol Med 37:1384–1392. doi:10.1016/j.freeradbiomed.2004.07.029
Stricklett PK, Hughes AK, Kohan DE (2006) Endothelin-1 stimulates NO production and inhibits cAMP accumulation in rat inner medullary collecting duct through independent pathways. Am J Physiol Ren Physiol 290:1315–1319. doi:10.1152/ajprenal.00450.2005
Pei DS, Song YJ, Yu HM, Hu WW, Du Y, Zhang GY (2008) Exogenous nitric oxide negatively regulates c-Jun N-terminal kinase activation via inhibiting endogenous NO-induced S-nitrosylation during cerebral ischemia and reperfusion in rat hippocampus. J Neurochem 106(4):1952–1963. doi:10.1111/j.1471-4159.2008.05531.x
Acknowledgments
We thank Mr. Anirban Manna for preparation of the manuscript and Dr. Carlo Gambacorti Passerini for providing KU812 and KCL22 cell lines. The present study was supported by the Council of Scientific and Industrial Research (CSIR), Department of Biotechnology (DBT), New Delhi.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rakshit, S., Bagchi, J., Mandal, L. et al. N-acetyl cysteine enhances imatinib-induced apoptosis of Bcr-Abl+ cells by endothelial nitric oxide synthase-mediated production of nitric oxide. Apoptosis 14, 298–308 (2009). https://doi.org/10.1007/s10495-008-0305-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10495-008-0305-7