Abstract
Although zinc was known to be associated with insulin metabolism and diabetes, the relationship of serum zinc concentration with insulin resistance (IR) and metabolic syndrome (MetS) was not well investigated in general population. The aim of this study is to evaluate the relationships of serum zinc concentration with IR and MetS in a nondiabetic adult population. This cross-sectional study included 656 men and 825 women who were nondiabetic adults from the fifth Korea National Health and Nutrition Examination Survey conducted in 2010. Serum zinc concentration and metabolic parameters were measured. IR was estimated by homeostatic model assessment (HOMA2). MetS was defined according to the National Cholesterol Education Program Adult Treatment Panel III criteria. Serum zinc concentration was negatively correlated with homeostasis model assessment for insulin resistance (HOMA2-IR) in men (r = −0.104, P = 0.008), but not in women. After adjusting for conventional cardiovascular risk factors, the inverse correlation was significant in both men and women (B = −0.262, SE = 0.060 for men, and B = −0.129, SE = 0.052 for women). However, serum zinc concentration was not different between the groups with and without MetS (P = 0.752 for men and P = 0.371 for women). In conclusion, serum zinc concentration was inversely associated with IR but not related to MetS in nondiabetic adult population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Zinc is an essential trace element for the synthesis, storage, and release of insulin [1, 2]. This mineral is also a fundamental component for the synthesis of antioxidant enzymes such as superoxide dismutase and glutathione peroxidase [3]. Therefore, zinc deficiency may induce abnormal insulin metabolism and oxidative stress, which are important factors for the pathophysiology of diabetes and metabolic syndrome (MetS) [4–6].
In diabetic patients, altered zinc metabolism has been observed. Comparing with controls, lower serum zinc concentration and higher urinary zinc excretion were reported [7–9]. In addition, a large population-based longitudinal study revealed that a low intake of zinc is a risk factor of diabetes, suggesting that zinc is closely associated with diabetes [10].
The relationship between zinc and MetS is controversial. Higher zinc intake had protective effect against MetS in specific populations [11, 12]. Inverse relationship between serum zinc concentration and MetS was also reported in women [13]. In contrast, a longitudinal study reported that higher zinc concentration was a predictive factor for MetS [14].
Although insulin resistance is a connecting link between zinc and MetS, only a few studies investigated the relationship between serum zinc concentration and insulin resistance [9, 15–18]. The subjects of these studies have their own characteristics of age group, race, and region. Until now, there have not been any studies evaluating the relationship between serum zinc status and insulin resistance (IR) for East Asian population including Korean. Since the subjects of the Korea National Health and Nutrition Examination Survey (KNHANES) were recruited from a nationwide population, they are representative of Korean population. Therefore, we investigated the relationship of serum zinc concentrations with insulin resistance and MetS in a nondiabetic adult population using the Korean representative data from the fifth KNHANES V-1 conducted in 2010.
Methods
Study Population
This study was based on the data acquired in the first year (2010) of KNHANES V which was a cross-sectional and nationally representative survey conducted by the Division of Chronic Disease Surveillance, Korea Centers for Disease Control and Prevention. The overall survey consisted of a health interview survey, a nutrition survey, and a health examination survey. Data were collected via household interviews and by physical measurements and blood sampling in specially equipped mobile examination centers. The sampling frame was designed based on the 2005 population and housing census in Korea.
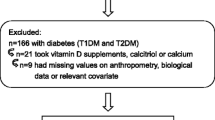
Among a total of 6,740 adults subjects (2,958 men and 3,782 women) aged 19 or older, 1,676 subjects (767 men and 909 women) were available for anthropometric measurements, serum glucose, insulin, zinc concentrations, and dietary survey. To choose the nondiabetic subjects, 71 men and 37 women who had history of diabetes were excluded.
We also excluded 40 men and 47 women who had a history of stroke, myocardial infarction, angina, thyroid disease, liver cirrhosis, or any kind of cancer. Finally, our study consisted of 1,481 subjects (656 men and 825 women).
Medical History and Lifestyle Habits
Medical history information and lifestyle habits were collected using self-reported questionnaires. Smoking history was categorized into the three groups: current smoker, ex-smoker, and nonsmoker. Drinking was classified into rarely (<once a month), occasionally (monthly to weekly), and frequently (≥once a week). Exercise was categorized into routine (moderate to strenuous intensity, three times a week or more frequently) and nonroutine.
Measurements
Heights and weights were measured in the standing position without shoes. Heights and weights were measured to the first decimal point in centimeters and kilograms, respectively. Body mass index was calculated as the weight in kilograms divided by the square of the height in meters. Waist circumference was measured midway between the lower rib margin and the iliac crest in a standing position. Blood pressure (BP) was measured three times on the right arm while the individual was in a seated position after at least 5 min of rest using a mercury sphygmomanometer (Baumanometer; Baum, Copiague, NY, USA).
Blood samples, after an 8-h fast, were collected year-round. They were immediately processed, refrigerated, and transported in the cold storage to the central testing institute (NeoDin Medical Institute, Seoul, South Korea), followed by analysis within 24 h. Glucose, liver enzymes, and lipid profile were tested using an automatic analyzer (ADIVIA 1650; Siemens, NY, USA). Serum zinc concentration was measured by inductively coupled plasma mass spectrometry (ICP-MS) assay using PerkinElmer ICP-MS (PerkinElmer, MA, USA). Insulin was analyzed by immunoradiometric assay using INS-IRMA (Biosource, Nivelles, Belgium). Beta cell function and insulin resistance were estimated using homeostatic model assessment (HOMA2) calculator version 2.2.3 (Oxford Centre for Diabetes, Endocrinology and Metabolism, UK, available at http://www.dtu.ox.ac.uk).
Definition of MetS
The presence of MetS was defined by the National Cholesterol Education Program Adult Treatment Panel III criteria [19]. The cutoff values for central obesity were adopted from a well-validated previous Korean study [20]. The MetS was defined by the presence of three of more of the following components: (1) central obesity (WC ≥ 90 cm for men and 85 cm for women), (2) systolic BP ≥130 mmHg or diastolic BP ≥85 mmHg or antihypertensive medication use, (3) high-density lipoprotein (HDL) cholesterol <1.04 mmol/L for men and 1.29 mmol/L for women, (4) triglyceride >1.69 mmol/L, and (5) elevated fasting blood glucose ≥6.11 mmol/L or taking hypoglycemic agents.
Dietary Survey
Nutrient intakes, including total calorie, and the intakes of macronutrients and some of micronutrients were assessed with a 24-h dietary recall questionnaire administered by a trained dietician. However, the daily intake of zinc was not calculated. The results were calculated using the food composition table developed by the National Rural Resources Development Institute (seventh revision) [21]. Supplement use was divided into user and nonuser according to a questionnaire whether to take supplements once a week or more frequently for 1 month recently.
Statistical Analysis
All analyses were conducted separately according to sex. Because variables of zinc, glucose, insulin, triglyceride, homeostasis model assessment for insulin resistance (HOMA2-IR), and homeostasis model assessment for beta cell function (HOMA2-%B) showed a right-skewed distribution, log-transformed values were used in all analyses. Most of these variables achieved a normality of distribution statistically. For this reason, these variables were described as geometric mean and 95 % confidence interval (CI). Other variables were described as mean ± SD or number (proportion).
Sex-specific receiver operating characteristic curves of HOMA2-IR were generated for MetS. The cutoff values of HOMA2-IR were determined, considering sensitivity and specificity [22] that were 1.41 for men and 1.57 for women, respectively.
To compare the variables between men and women, the independent t test (continuous variables) or chi-square test (categorical variables) was used. Pearson correlation analysis was used to evaluate the relationship between serum zinc concentration and metabolic parameters. Serum zinc concentrations were compared between the groups with and without MetS and its components. P values were calculated by t test.
To control the influence of the potential confounders on the relationship between serum zinc concentration and HOMA2-IR, multiple linear regression analysis was used. Model 1 adjusted for age, waist circumference, history of hypertension, and female factors (menopause and hormone replacement therapy); model 2 additively included HDL cholesterol, triglyceride, systolic BP, and habitual variables such as smoking, drinking, and exercise. In model 3, dietary variables such as calorie and protein intake and supplement use were added to model 2.
We considered P < 0.05 to be statistically significant. All statistical analyses were performed using SPSS 19.0 (IBM, Armonk, NY, USA).
Results
The baseline characteristics of the subjects are presented in Table 1. Men tended to have higher BMI, fasting glucose levels, and BP than women. Lifestyle habits were also different between men and women. Serum zinc concentrations were significantly higher in men (geometric mean 21.4 μmol/L; 95 % CI 21.1–21.8) than in women (geometric mean 19.6 μmol/L; 95 % CI 19.3–19.9). HOMA2-%B was higher in women than in men. No significant difference was found in age, insulin HOMA2-IR, and HOMA2-%S between sexes. However, the proportion of the insulin resistance differed according to sexes (34.5 % for men and 23.6 % for women). The prevalence of MetS was significantly higher in men (17.4 %) than in women (10.7 %).
The relationship between serum zinc concentration and the metabolic parameters was analyzed (Table 2). Serum zinc concentration was negatively correlated with HOMA2-IR in men (r = −0.104, P = 0.008), but no significant relationship was found in women (r = −0.056, P = 0.105). HDL cholesterol was negatively correlated with serum zinc concentration in both sexes. However, other metabolic parameters were not related with serum zinc concentration. Daily calorie and protein intakes were not related with zinc concentration.
The mean of serum zinc concentration was not significantly different between the groups with and without MetS (Table 3). No difference was found between the groups with and without the diabetes-related component of MetS. Men with obesity-related and triglyceride (TG) component of MetS had a significantly higher zinc concentration than men without.
The relationship between serum zinc concentration and HOMA2-IR was evaluated after adjusting for the potential confounders (Table 4). Serum zinc concentration and HOMA2-IR were significantly related to each other in all of the models. The variables of waist circumference, HDL cholesterol, TG, and history of hypertension were significantly related with HOMA2-IR. Systolic BP was positively related with HOMA2-IR only in women. Supplement intake did not influence HOMA2-IR in both men and women. Calorie and protein intakes were not associated with HOMA2-IR in both sexes.
Discussion
In our study, the serum zinc concentration was correlated with HOMA2-IR in nondiabetic adults. This relationship was independent of age, obesity, hypertension, and lipid profiles. In contrast, serum zinc concentration was not associated with the prevalence of MetS.
Previous studies evaluated the relationship between the glucose metabolism and the zinc intake or supplementation. A diabetic mouse model had shown that zinc supplementation attenuated hyperglycemia in db/db mice [23]. For diabetic patients, zinc supplementation showed beneficial effects in the metabolic control [24, 25]. Another intervention study was conducted for 56 nondiabetic obese women [9]. This study demonstrated that 30 mg of zinc daily for 4 weeks improved insulin resistance. According to a long-term observation of Nurses’ Health Study, higher zinc intake reduced the risk of diabetes [10]. These studies suggest that zinc has favorable effects on the metabolism of glucose and insulin in both diabetic and nondiabetic subjects.
The relationship between zinc and other metabolic parameters is controversial. Several studies evaluated the association of MetS with serum zinc concentration. In a few studies, men and women with MetS had a higher and lower level of serum zinc than those without, respectively [13, 26]. In contrast, other studies reported no relationship between serum zinc concentration and MetS [27, 28]. Furthermore, baseline serum zinc concentrations were positively related with the risk of developing MetS, independent of providing supplements [14]. Consistently, our study showed that serum zinc concentration was not associated with MetS. Thus, the serum zinc concentration may be differently associated with the insulin resistance or MetS. Therefore, the relation of zinc with the components of MetS should be considered. Our study showed a higher concentration of serum zinc in men with obesity-related and TG components than in men without. This finding is consistent with a recent study [13]. Meanwhile, HDL cholesterol had inversely linear relationship with serum zinc concentration in both men and women. In spite of an old report of positive correlation between serum zinc level and HDL cholesterol [29], a negative association between HDL cholesterol and serum zinc concentration was reported in a longitudinal study [14]. Moreover, zinc supplementation reduced the level of HDL cholesterol [30, 31]. Thus, zinc has partially unfavorable effects on metabolic parameters except glucose metabolism.
Two studies have shown the inverse relationship between serum zinc concentration and insulin resistance in adolescents and children [15, 16]. In the same way, a cross-sectional study from Bangladesh showed that serum zinc concentration is associated with insulin resistance in 142 normoglycemic adults [17]. Our study also demonstrated the linear relationship between serum zinc concentration and insulin resistance in a large nondiabetic adult population. These various studies including our results suggest that low serum zinc concentration is closely associated with insulin resistance.
The association between zinc and insulin resistance can be explained by several mechanisms. The protein tyrosine phosphatase 1B, a key regulator of the phosphorylation state of the insulin receptor, is known to be a target of zinc ions [32]. Zinc is also reported to promote the glucose transport and to improve the peripheral insulin sensitivity [33]. In addition, oxidative stress can contribute to the initiation and progression of insulin resistance and diabetes [4]. The pancreatic β cells are known to be vulnerable to free radical. Since zinc is a cofactor of superoxide dismutase, zinc deficiency can aggravate the oxidative stress and induce the insulin resistance [34].
Our study has several limitations. First, because this study employed a cross-sectional design, we could not determine the cause-effect relationship between serum zinc concentrations and insulin resistance. However, previous studies have demonstrated that lower zinc intake precedes insulin resistance or diabetes risk [9, 10]. An additional longitudinal study will contribute to verifying the cause-effect relationship between serum zinc concentrations and insulin resistance. Second, we had limited accesses to the participants’ zinc intake data. However, the bioavailability of zinc varied according to the chemical forms; it was not clear how much dietary zinc intake would increase the bioavailable zinc level [35]. Although included in our study, 24-h recall is not enough to estimate the average intake of trace minerals. Dietary survey in depth should be conducted in the future study. In addition, our study includes limited information of the supplement use. However, although the amount of trace mineral intake from the supplements was not surveyed, the serum zinc concentrations were not different between the groups with and without supplement use (data not shown). Third, we used HOMA2-IR as an index of the insulin resistance. Although the gold standard of evaluating the insulin resistance is the euglycemic-hyperinsulinemic clamp test that measures IR both directly and accurately, it is an invasive and time-consuming procedure [36]. HOMA2-IR is a less invasive and inexpensive method to measure IR, and it has been widely validated and applied for quantifying insulin resistance [37]. Finally, our study was conducted for Korean subjects; studies for the subjects with different ethnic backgrounds can be compared to our results.
In conclusion, serum zinc concentration is inversely associated with insulin resistance in nondiabetic adult population. However, it is not related with MetS. Further prospective studies on the relationship of serum zinc concentrations with insulin resistance and metabolic risk factors should be performed in a large cohort of various ethnic groups. Furthermore, zinc-based intervention study in patients with metabolic disease or insulin resistance will be helpful for the clinical application of zinc supplementation.
References
Zalewski PD, Millard SH, Forbes IJ, Kapaniris O, Slavotinek A, Betts WH, Ward AD, Lincoln SF, Mahadevan I (1994) Video image analysis of labile zinc in viable pancreatic islet cells using a specific fluorescent probe for zinc. J Histochem Cytochem 42(7):877–884
Chimienti F (2013) Zinc, pancreatic islet cell function and diabetes: new insights into an old story. Nutr Res Rev 26(1):1–11. doi:10.1017/S0954422412000212
Roussel AM, Kerkeni A, Zouari N, Mahjoub S, Matheau JM, Anderson RA (2003) Antioxidant effects of zinc supplementation in Tunisians with type 2 diabetes mellitus. J Am Coll Nutr 22(4):316–321
Wiernsperger NF (2003) Oxidative stress as a therapeutic target in diabetes: revisiting the controversy. Diabetes Metab 29(6):579–585
Lann D, LeRoith D (2007) Insulin resistance as the underlying cause for the metabolic syndrome. Med Clin N Am 91(6):1063–1077. doi:10.1016/j.mcna.2007.06.012, viii
Yubero-Serrano EM, Delgado-Lista J, Pena-Orihuela P, Perez-Martinez P, Fuentes F, Marin C, Tunez I, Tinahones FJ, Perez-Jimenez F, Roche HM, Lopez-Miranda J (2013) Oxidative stress is associated with the number of components of metabolic syndrome: LIPGENE study. Exp Mol Med 45:e28. doi:10.1038/emm.2013.53
Anetor JI, Senjobi A, Ajose OA, Agbedana EO (2002) Decreased serum magnesium and zinc levels: atherogenic implications in type-2 diabetes mellitus in Nigerians. Nutr Health 16(4):291–300
Xu J, Zhou Q, Liu G, Tan Y, Cai L (2013) Analysis of serum and urinal copper and zinc in Chinese northeast population with the prediabetes or diabetes with and without complications. Oxidative Med Cell Longev 2013:635214. doi:10.1155/2013/635214
Marreiro DN, Geloneze B, Tambascia MA, Lerario AC, Halpern A, Cozzolino SM (2006) Effect of zinc supplementation on serum leptin levels and insulin resistance of obese women. Biol Trace Elem Res 112(2):109–118
Sun Q, van Dam RM, Willett WC, Hu FB (2009) Prospective study of zinc intake and risk of type 2 diabetes in women. Diabetes Care 32(4):629–634. doi:10.2337/dc08-1913
Hashemipour M, Kelishadi R, Shapouri J, Sarrafzadegan N, Amini M, Tavakoli N, Movahedian-Attar A, Mirmoghtadaee P, Poursafa P (2009) Effect of zinc supplementation on insulin resistance and components of the metabolic syndrome in prepubertal obese children. Hormones (Athens) 8(4):279–285
Suarez-Ortegon MF, Ordonez-Betancourth JE, Aguilar-de Plata C (2013) Dietary zinc intake is inversely associated to metabolic syndrome in male but not in female urban adolescents. Am J Hum Biol 25(4):550–554. doi:10.1002/ajhb.22408
Ghasemi A, Zahediasl S, Hosseini-Esfahani F, Azizi F (2014) Gender differences in the relationship between serum zinc concentration and metabolic syndrome. Ann Hum Biol. doi:10.3109/03014460.2013.870228
Czernichow S, Vergnaud AC, Galan P, Arnaud J, Favier A, Faure H, Huxley R, Hercberg S, Ahluwalia N (2009) Effects of long-term antioxidant supplementation and association of serum antioxidant concentrations with risk of metabolic syndrome in adults. Am J Clin Nutr 90(2):329–335. doi:10.3945/ajcn.2009.27635
Suliburska J, Cofta S, Gajewska E, Kalmus G, Sobieska M, Samborski W, Krejpcio Z, Drzymala-Czyz S, Bogdanski P (2013) The evaluation of selected serum mineral concentrations and their association with insulin resistance in obese adolescents. Eur Rev Med Pharmacol Sci 17(17):2396–2400
Ortega RM, Rodriguez-Rodriguez E, Aparicio A, Jimenez AI, Lopez-Sobaler AM, Gonzalez-Rodriguez LG, Andres P (2012) Poor zinc status is associated with increased risk of insulin resistance in Spanish children. Br J Nutr 107(3):398–404. doi:10.1017/S0007114511003114
Islam MR, Arslan I, Attia J, McEvoy M, McElduff P, Basher A, Rahman W, Peel R, Akhter A, Akter S, Vashum KP, Milton AH (2013) Is serum zinc level associated with prediabetes and diabetes?: a cross-sectional study from Bangladesh. PLoS One 8(4):e61776. doi:10.1371/journal.pone.0061776
Singh RB, Niaz MA, Rastogi SS, Bajaj S, Gaoli Z, Shoumin Z (1998) Current zinc intake and risk of diabetes and coronary artery disease and factors associated with insulin resistance in rural and urban populations of North India. J Am Coll Nutr 17(6):564–570
Expert Panel on Detection E, Treatment of High Blood Cholesterol in A (2001) Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA 285 (19):2486–2497
Lee SY, Park HS, Kim DJ, Han JH, Kim SM, Cho GJ, Kim DY, Kwon HS, Kim SR, Lee CB, Oh SJ, Park CY, Yoo HJ (2007) Appropriate waist circumference cutoff points for central obesity in Korean adults. Diabetes Res Clin Pract 75(1):72–80. doi:10.1016/j.diabres.2006.04.013
Institute NRRD (2006) Food composition table. 7 edn., Suwon Korea
Van der Schouw YT, Verbeek AL, Ruijs JH (1992) ROC curves for the initial assessment of new diagnostic tests. Fam Pract 9(4):506–511
Simon SF, Taylor CG (2001) Dietary zinc supplementation attenuates hyperglycemia in db/db mice. Exp Biol Med (Maywood) 226(1):43–51
Farvid MS, Siassi F, Jalali M, Hosseini M, Saadat N (2004) The impact of vitamin and/or mineral supplementation on lipid profiles in type 2 diabetes. Diabetes Res Clin Pract 65(1):21–28. doi:10.1016/j.diabres.2003.11.009
Gunasekara P, Hettiarachchi M, Liyanage C, Lekamwasam S (2011) Effects of zinc and multimineral vitamin supplementation on glycemic and lipid control in adult diabetes. Diabetes Metab Syndr Obes 4:53–60. doi:10.2147/DMSO.S16691
Yu Y, Cai Z, Zheng J, Chen J, Zhang X, Huang XF, Li D (2012) Serum levels of polyunsaturated fatty acids are low in Chinese men with metabolic syndrome, whereas serum levels of saturated fatty acids, zinc, and magnesium are high. Nutr Res 32(2):71–77. doi:10.1016/j.nutres.2011.12.004
Obeid O, Elfakhani M, Hlais S, Iskandar M, Batal M, Mouneimne Y, Adra N, Hwalla N (2008) Plasma copper, zinc, and selenium levels and correlates with metabolic syndrome components of Lebanese adults. Biol Trace Elem Res 123(1–3):58–65. doi:10.1007/s12011-008-8112-0
Pizent A, Pavlovic M, Jurasovic J, Dodig S, Pasalic D, Mujagic R (2010) Antioxidants, trace elements and metabolic syndrome in elderly subjects. J Nutr Health Aging 14(10):866–871
Koo SI, Ramlet JS (1983) Dietary cholesterol decreases the serum level of zinc: further evidence for the positive relationship between serum zinc and high-density lipoproteins. Am J Clin Nutr 37(6):918–923
Freeland-Graves JH, Friedman BJ, Han WH, Shorey RL, Young R (1982) Effect of zinc supplementation on plasma high-density lipoprotein cholesterol and zinc. Am J Clin Nutr 35(5):988–992
Hooper PL, Visconti L, Garry PJ, Johnson GE (1980) Zinc lowers high-density lipoprotein-cholesterol levels. JAMA 244(17):1960–1961
Haase H, Maret W (2005) Protein tyrosine phosphatases as targets of the combined insulinomimetic effects of zinc and oxidants. Biometals 18(4):333–338. doi:10.1007/s10534-005-3707-9
Tang X, Shay NF (2001) Zinc has an insulin-like effect on glucose transport mediated by phosphoinositol-3-kinase and Akt in 3 T3-L1 fibroblasts and adipocytes. J Nutr 131(5):1414–1420
Levine AS, McClain CJ, Handwerger BS, Brown DM, Morley JE (1983) Tissue zinc status of genetically diabetic and streptozotocin-induced diabetic mice. Am J Clin Nutr 37(3):382–386
Krebs NF (2000) Overview of zinc absorption and excretion in the human gastrointestinal tract. J Nutr 130(5S Suppl):1374S–1377S
DeFronzo RA, Tobin JD, Andres R (1979) Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol 237(3):E214–E223
Wallace TM, Levy JC, Matthews DR (2004) Use and abuse of HOMA modeling. Diabetes Care 27(6):1487–1495
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ahn, BI., Kim, M.J., Koo, H.S. et al. Serum Zinc Concentration Is Inversely Associated with Insulin Resistance but Not Related with Metabolic Syndrome in Nondiabetic Korean Adults. Biol Trace Elem Res 160, 169–175 (2014). https://doi.org/10.1007/s12011-014-0045-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-014-0045-1