Abstract
Parkin was originally identified as a protein associated with Parkinson's disease. Recently, numerous research studies have suggested that parkin acts as a tumor suppressor. In accordance with these studies, we previously reported that overexpression of parkin in HeLa cells induced growth inhibition. To elucidate possible mechanisms by which parkin may inhibit cell growth, HeLa cells were infected with adenoviruses expressing either the parkin gene or adenovirus alone for 72 h and a total proteomic analysis was performed using 2-D gel electrophoresis followed by LC-MS/MS. We identified three proteins whose expression changed between the two groups: the 40S ribosomal protein SA (RPSA) was downregulated in parkin virus-infected cells, and cytokeratins 8 and 18 exhibited an acid shift in pI value without a change in molecular weight, suggesting that these proteins became phosphorylated in parkin virus-infected cells. The changes in these three proteins were first observed at 60 h postinfection and were most dramatic at 72 h postinfection. Because upregulation of RPSA and dephosphorylation of cytokeratins 8/18 have been linked with tumor progression, these data suggest that parkin may inhibit cell growth, at least in part, by decreasing RPSA expression and inducing phosphorylation of cytokeratin 8/18.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mutations in the parkin gene, located on chromosome 6q25.2-27, are associated with the development of Parkinson's disease [1]. Thus, initial studies on the parkin gene were focused on elucidating the role of parkin in neuronal degeneration [2–5]. Later studies identified a potential correlation between the loss of parkin gene expression and cancer development. Results from one early study showed that the parkin gene is either absent or inactivated in malignant tumors and tumor-derived cell lines, suggesting that parkin possesses tumor suppressor activity [6]. Furthermore, aberrant expression of the parkin gene has been identified in a wide range of cancers [5, 7–14]. For example, hypermethylation of the parkin promoter region resulted in diminished expression of parkin in acute lymphoblastic leukemia, chronic myeloid leukemia, and colorectal cancers [12]. In addition, mutations in both the parkin gene and the adenomatous polyposis coli (APC) gene accelerated the development of colorectal carcinoma [9], and parkin overexpression resulted in growth inhibition in hepatocarcinoma, glioblastoma, lung cancer, breast cancer, and colon cancer cells [9, 11, 13–15]. Collectively, these reports suggest that parkin acts as a tumor suppressor in part by inhibiting cellular growth. However, the mechanism by which this growth inhibition is mediated remains unclear.
To investigate the mechanism by which parkin inhibits cell growth, we performed a proteomic analysis to identify protein(s) whose expression levels were affected when HeLa cells, which express little or no endogenous parkin, were induced to express parkin using adenoviral expression vectors. First, we separated cellular proteins by 2-D gel electrophoresis, which resolves proteins by molecular size and pI, and then used LC-MS/MS to identify protein(s) of interest.
Materials and Methods
Cell Culture and Parkin Expression
HeLa cells were infected using parkin-expressing adenovirus vectors, as described previously [2]. In brief, HeLa cells (2 × 105) were seeded into 100-mm cell culture dishes and infected 24 h later with parkin-expressing or mock virus (150 multiplicity of infection, MOI) in serum-free Dulbecco's Modified Eagle Medium (DMEM). After 90 min, 10 % fetal bovine serum (FBS)–DMEM was added to each well. The cell lysates were collected for 2-D gel analysis at different times.
Cell Proliferation Assay
HeLa cells (2 × 105) were seeded into each well of a six-well plate and infected 24 h later with parkin or mock virus (150 MOI) in serum-free DMEM. After 90 min, 10 % FBS-DMEM was added to each well. At selected intervals, the cells were trypsinized and viable cells were enumerated using trypan blue dye.
Sample Preparation
HeLa cells were washed once with 1× phosphate-buffered saline (PBS) and once with 0.5× PBS and then harvested by scraping in the presence of 5 mL 0.5× PBS. The cell suspension was transferred into a 50-mL conical tube and centrifuged, and the resulting pellet was resuspended in 1 mL of 0.5× PBS. The cell suspension was transferred to a microfuge tube and centrifuged at 3,000 rpm for 5 min. After the supernatant was discarded, the cell pellet was frozen with liquid nitrogen and stored at −80 °C.
2-D Gel Electrophoresis
Proteins were extracted from cell samples using a sample preparation solution (7 M urea, 2 M thiourea, 4 % CHAPS, and 40 mM DTT) followed by a short sonication step. After clarification, soluble proteins were precipitated with ice-cold acetone. The protein precipitate was briefly dried and resuspended in a sample preparation solution. Protein concentration was determined by Bradford assay. Proteins (50 μg) were diluted in 0.5 % (v/v) ampholyte buffer (pH 3.0–5.6NL, GE Healthcare) and adjusted to a final volume of 100 μL with DeStreak™ rehydration solution (GE Healthcare). Protein samples were separated on a 7-cm Immobiline™ DryStrip gel with a pH range of 3–5.6NL (GE Healthcare) using an Ettan IPGphor™ 3 isoelectrofocusing unit, followed by 10 % SDS-PAGE (Bio-Rad). The gels were stained using Colloidal Coomassie Blue Staining Kit (Invitrogen).
LC-MS/MS Analysis
Protein spots of interest were digested in-gel with sequencing grade trypsin (Promega). Extracted peptides were injected into a NanoLC system (Eksigent). Peptides were separated using a C18 micro column, ionized via a nano-spray module, and analyzed with an LTQ XL™ ion trap mass analyzer (Thermo Scientific). For MS/MS analysis, parent ions were fragmented by the CID method.
Database Searching and Protein Identification
The MS/MS results for each sample were analyzed using Sorcerer™ solo (Sage-N), which was set up to search the ipi.HUMAN v3.86 database. MS/MS-based peptide and protein identification was further validated with Scaffold™3 software (Proteome Software).
Statistical Analysis
P values were calculated using the Student's t test. Values are shown as the mean and SEM. Data were collected from three independent experiments.
Results and Discussion
Previously, we showed that HeLa cells overexpressing parkin exhibited a slight decrease in cell growth at 48 h [16]. To gain further insight into parkin-mediated inhibition of cell growth, HeLa cells were infected with either a parkin-expressing virus or mock virus for up to 72 h. Cell viability was assessed at 12, 24, 48, 60, and 72 h postinfection. We found that inhibition of cell growth began at 48 h postinfection (P < 0.01) in cells infected with the parkin-expressing virus, and the difference in cell proliferation between parkin virus-infected and mock virus-infected cells persisted for up to 72 h (Fig. 1). This suppression of cell growth is attributed to both cell growth arrest and induction of apoptosis [11, 15, 16].
Inhibition of cell growth in HeLa cells infected with mock or parkin-expressing viruses. HeLa cells were infected with either the parkin virus or mock virus (150 MOI), and the surviving cells were enumerated using a trypan blue dye exclusion assay. The cell number at time 0 h was set as 100 %. Data are from three independent experiments. P values were determined by Student's t test. **P < 0.01, ***P < 0.001
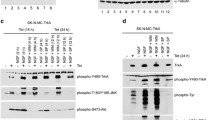
To identify protein(s) that may be responsible for parkin-induced inhibition of cell growth, HeLa cells were infected with parkin-expressing or mock virus for 72 h and the cell lysates were compared using 2-D gel electrophoresis (Fig. 2). We identified several proteins whose expression was altered in parkin virus-infected cells compared to mock virus-infected cells. Protein #1, Protein #2, and Protein #3 detected in mock-infected cells were not detected in parkin-infected cells at 72 h postinfection (Fig. 2). By contrast, Protein #4 and Protein #5 were detected in parkin-infected cells but not in mock-infected cells. These five proteins were excised and subjected to LC-MS/MS analysis followed by a database search. Based on the results of this search, we identified Protein #1 as the 40S ribosomal protein SA (RPSA, sequence coverage 36 %). This result suggests that RPSA is downregulated in parkin-infected cells. Both Protein #2 and #4 were identified as cytoskeletal keratin 18 (CK18, sequence coverage 81 %), and both Protein #3 and Protein #5 were identified as cytoskeletal keratin 8 (CK8, sequence coverage 59 %) (Figs. 3 and 4). These results suggest that CK18 and CK8 exhibited a left shift in pI value, but no change in molecular weight.
A 2-D gel image of cell extracts from mock (a) and parkin (b) virus-infected HeLa cells. Circles indicate the protein spots that were excised and examined by mass spectrometry analysis: RPSA (spot 1), cytokeratin 8 (spots 3 and 5), and cytokeratin 18 (spots 2 and 4). HeLa cells infected with mock or parkin-expressing virus at 72 h postinfection were subjected to 2-D gel electrophoresis and stained with Colloidal Coomassie Blue
Representative LC-MS/MS spectrum of identified proteins. a RPSA. The parent ion has an m/z of 456.99. The spectrum was identified as the tryptic peptide LLVVTDPR from RPSA. b Cytokeratin 18. The parent ion has an m/z of 790.90. The spectrum was identified as the tryptic peptide PVSSAASVYAGAGGSGSR from cytokeratin 18. c Cytokeratin 8. The parent ion has an m/z of 896.98. The spectrum was identified as the tryptic peptide LEAELGNMQGLVEDFK from cytokeratin 8
Since these results were obtained from mock and parkin virus-infected cells at 72 h postinfection, we conducted a time course experiment to determine at what point following parkin expression RPSA was downregulated and when the shift in CK8/18 occurred. HeLa cells were infected with either mock virus or the parkin virus for 0, 12, 48, 60, and 72 h, and the cell lysates were analyzed by 2-D gel electrophoresis. We found that RPSA protein expression showed a slight decrease at 60 h postinfection and was dramatically downregulated at 72 h postinfection (Fig. 5). Similarly, the spots correlating to CK8/18 maintained their initial positions for up to 60 h and then left-shifted at 72 h postinfection. Taken together with the cell viability data, our results ostensibly indicate that the changes in these three proteins occurred after the onset of cell growth inhibition. However, these findings can also be interpreted as indicating that the percentage of infected cells was low and thus protein changes were only evident after 72 h. Therefore, it is unclear at this time whether the changes observed in RPSA and CK8/18 were the cause or result of cell growth inhibition.
2-D gel images of cell extracts from mock and parkin-infected HeLa cells in a time course experiment. Cells were infected with mock or parkin-expressing virus and lysates were collected at different time intervals and examined by 2-D gel electrophoresis. The positions of RPSA (a) and CK8/18 (b) are indicated
RPSA is a multifunctional protein present in several cellular compartments. It is alternatively called the laminin receptor-1 due to its ability to bind the extracellular protein laminin-1 [17, 18], a component of the ECM and the predominant glycoprotein in the basement membrane of all types of tissues. RPSA is also known to be associated with the 40S subunit of ribosomes in the cytoplasm [19, 20]. In human heart tissue, RPSA is a subunit of the mitochondrial proteome, where it functions as a mitochondrial ribosomal protein [21]. In addition, evidence suggests that RPSA associates with the histones H2A, H2B, and H4 in the nucleus [22–24], and it is known to bind to prions [25], viruses [26, 27], and bacteria [28]. RPSA has also been shown to be a receptor for epigallocatechin gallate (EGCG), a major component of green tea [29]. Finally, RPSA can influence the phosphorylation status of the signaling proteins extracellular signal-regulated kinase (ERK), c-Jun NH2-terminal kinase (JNK), and p38 MAPK [30]. Thus, it is becoming increasingly clear that RPSA is a multifunctional protein.
RPSA has been shown to be overexpressed in a variety of cancers, and increased expression of RPSA positively correlates with tumor progression [18, 31–34]. In vitro siRNA-mediated silencing of RPSA in human cancer cell lines (Hep3B and HeLa) induces apoptosis, suggesting that RPSA is required for maintaining cell viability [35, 36]. In an in vivo mouse model, siRNA-mediated silencing of RPSA reduced tumor growth by inducing G1 phase cell-cycle arrest [37]. Our observation that RPSA levels decrease in parkin-infected HeLa cells suggests that parkin, at least in part, may decrease RPSA expression, thereby dampening cell growth.
Dynamic alterations in cytokeratin networks have been implicated in the response of cells to external stimuli and cellular cues such as apoptosis and mitosis [38–42]. In epithelial cells, type 1 acidic cytokeratins (CK9-22) and type 2 basic cytokeratins (CK1-8) dimerize to form intermediate filaments [43]. Cells derived from epithelial cells produce CK8 and CK18, as well as several other cytokeratins. In the current study, CK8/18 exhibited a left shift in pI value without exhibiting a change in molecular weight. For most proteins, this shift is often correlated to protein modification [44]. In particular, phosphorylation events can shift the pI value, and the extent of the shift can vary depending upon the protein and the amount of phosphorylation. Phosphorylation affects the pI of intact proteins by substituting the neutral hydroxyl groups on serine, threonine, or tyrosine residues with negatively charged phosphate groups, thus inducing a left shift on the pI axis.
To date, serine phosphorylation is the most investigated phosphorylation event in CKs [45]. Serine phosphorylations have been demonstrated to occur on Ser 431, Ser 73, and Ser 23 of CK8 and on Ser 33 and Ser 52 of CK18 [46]. Multiple kinases have been shown to phosphorylate CKs [47]. Ser73 of CK8 is a substrate for phosphorylation by p38 kinase and JNK [48–51], while Ser431 of CK8 is phosphorylated by ERK1/2 [46, 52]. In contrast to serine phosphorylation, tyrosine phosphorylation of CKs is a significantly less investigated event. In one study, however, the phosphatase inhibitor pervanadate was shown to induce tyrosine phosphorylation of CK8 but not CK18 in several cultured human cell lines and in the mouse colon [53]. Many types of stimuli have been reported to induce phosphorylation of CK8 and CK18. For example, phorbol acetate has been shown to induce phosphorylation of CK8 and CK18 in human colonic epithelial cells [45]. In addition, forskolin-treated Caco-2 colon cancer cells exhibited changes in the phosphorylation status of CK8/18 without changing the protein levels of CK8/18 compared to nontreated cells [54]. In this report, forskolin treatment of these cells induced phosphorylation of CK8/18 but not of vimentin, suggesting that the phosphorylation of CK was a specific response. Finally, both CK8 and CK18 have been shown to undergo phosphorylation during cellular apoptosis [55, 56].
The persistence of CK8/18 in epithelial cell-derived tumors correlates with tumor invasiveness [47, 57]. In addition, dephosphorylation of CK8 in colorectal cancer tumor cells is associated with tumor progression and increased tumor aggressiveness [58]. There is increasing evidence that cytokeratins influence cell death signaling pathways, in particular apoptosis mediated by TNF-α and Fas [59], and it has been shown that epithelial cells lacking CK8/18 are significantly more sensitive to TNF-α-mediated apoptosis [55]. In agreement with this, our previous data showed that overexpression of parkin in HeLa cells enhanced the cytotoxicity of TNF-α treatment in these cells [16]. These observations suggest that another mechanism by which parkin may inhibit tumor cell growth is by dephosphorylating CK8/18, which would eventually lead to cell death. However, the mechanism by which the pI value of CK8/18 is changed in response to parkin overexpression in HeLa cells remains unknown and is currently under investigation.
In conclusion, we show that parkin overexpression in HeLa cells induces inhibition of cell growth. This growth inhibition correlates with a downregulation of RPSA expression and an acidic shift of the pI of CK8 and CK18. These events may be the mechanisms by which parkin acts as a tumor suppressor.
References
Kitada, T., Asakawa, S., Hattori, N., Matsumine, H., Yamamura, Y., Minoshima, S., et al. (1998). Nature, 392, 605–608.
Kim, Y. S., Patel, S., & Lee, S. J. (2006). Experimental Neurology, 197, 538–541.
Shimura, H., Hattori, N., Kubo, S., Mizuno, Y., Asakawa, S., Minoshima, S., et al. (2000). Nature Genetics, 25, 302–305.
Xu, J., Kao, S. Y., Lee, F. J., Song, W., Jin, L. W., & Yankner, B. A. (2002). Nature Medicine, 8, 600–606.
Morris, L. G., Veeriah, S., & Chan, T. A. (2010). Oncogene, 29, 3453–3464.
Cesari, R., Martin, E. S., Calin, G. A., Pentimalli, F., Bichi, R., McAdams, H., et al. (2003). Proceedings of the National Academy of Sciences of the United States of America, 100, 5956–5961.
Denison, S. R., Callahan, G., Becker, N. A., Phillips, L. A., & Smith, D. I. (2003). Genes, Chromosomes & Cancer, 38, 40–52.
Denison, S. R., Wang, F., Becker, N. A., Schule, B., Kock, N., Phillips, L. A., et al. (2003). Oncogene, 22, 8370–8378.
Poulogiannis, G., McIntyre, R. E., Dimitriadi, M., Apps, J. R., Wilson, C. H., Ichimura, K., et al. (2010). Proceedings of the National Academy of Sciences of the United States of America, 107, 15145–15150.
Veeriah, S., Taylor, B. S., Meng, S., Fang, F., Yilmaz, E., Vivanco, I., et al. (2010). Nature Genetics, 42, 77–82.
Wang, F., Denison, S., Lai, J. P., Philips, L. A., Montoya, D., Kock, N., et al. (2004). Genes, Chromosomes & Cancer, 40, 85–96.
Agirre, X., Roman-Gomez, J., Vazquez, I., Jimenez-Velasco, A., Garate, L., Montiel-Duarte, C., et al. (2006). International Journal of Cancer, 118, 1945–1953.
Picchio, M. C., Martin, E. S., Cesari, R., Calin, G. A., Yendamuri, S., Kuroki, T., et al. (2004). Clinical Cancer Research, 10, 2720–2724.
Tay, S. P., Yeo, C. W., Chai, C., Chua, P. J., Tan, H. M., Ang, A. X., et al. (2010). Journal of Biological Chemistry, 285, 29231–29238.
Ikeuchi, K., Marusawa, H., Fujiwara, M., Matsumoto, Y., Endo, Y., Watanabe, T., et al. (2009). International Journal of Cancer, 125, 2029–2035.
Lee, K., Lee, M. H., Kang, Y. W., Rhee, K.-J., Kim, T. U., & Kim, Y. S. (2012). BMB Reports, 45, 526–531.
Lesot, H., Kuhl, U., & Mark, K. (1983). The EMBO Journal, 2, 861–865.
Nelson, J., McFerran, N. V., Pivato, G., Chambers, E., Doherty, C., Steele, D., et al. (2008). Bioscience Reports, 28, 33–48.
Auth, D., & Brawerman, G. (1992). Proceedings of the National Academy of Sciences of the United States of America, 89, 4368–4372.
Bortoluzzi, S., d’Alessi, F., Romualdi, C., & Danieli, G. A. (2001). Bioinformatics, 17, 1152–1157.
Taylor, S. W., Fahy, E., Zhang, B., Glenn, G. M., Warnock, D. E., Wiley, S., et al. (2003). Nature Biotechnology, 21, 281–286.
Sato, M., Kinoshita, K., Kaneda, Y., Saeki, Y., Iwamatsu, A., & Tanaka, K. (1996). Biochemical and Biophysical Research Communications, 229, 896–901.
Salama, R. H., Muramatsu, H., Zou, K., Inui, T., Kimura, T., & Muramatsu, T. (2001). Experimental Cell Research, 270, 13–20.
Kinoshita, K., Kaneda, Y., Sato, M., Saeki, Y., Wataya-Kaneda, M., & Hoffmann, A. (1998). Biochemical and Biophysical Research Communications, 253, 277–282.
Gauczynski, S., Peyrin, J. M., Haik, S., Leucht, C., Hundt, C., Rieger, R., et al. (2001). The EMBO Journal, 20, 5863–5875.
Wang, K. S., Kuhn, R. J., Strauss, E. G., Ou, S., & Strauss, J. H. (1992). Journal of Virology, 66, 4992–5001.
Thepparit, C., & Smith, D. R. (2004). Journal of Virology, 78, 12647–12656.
Kim, K. J., Chung, J. W., & Kim, K. S. (2005). Journal of Biological Chemistry, 280, 1360–1368.
Umeda, D., Yano, S., Yamada, K., & Tachibana, H. (2008). Journal of Biological Chemistry, 283, 3050–3058.
Givant-Horwitz, V., Davidson, B., & Reich, R. (2004). Cancer Research, 64, 3572–3579.
Li, D., Chen, J., Gao, Z., Li, X., Yan, X., Xiong, Y., et al. (2009). European Surgical Research, 42, 168–173.
Sanjuan, X., Fernandez, P. L., Miquel, R., Munoz, J., Castronovo, V., Menard, S., et al. (1996). Journal of Pathology, 179, 376–380.
al-Saleh, W., Delvenne, P., van den Brule, F. A., Menard, S., Boniver, J., & Castronovo, V. (1997). Journal of Pathology, 181, 287–293.
Viacava, P., Naccarato, A. G., Collecchi, P., Menard, S., Castronovo, V., & Bevilacqua, G. (1997). Journal of Pathology, 182, 36–44.
Susantad, T., & Smith, D. R. (2008). Cellular & Molecular Biology Letters, 13, 452–464.
Kaneda, Y., Kinoshita, K., Sato, M., Saeki, Y., Yamada, R., Wataya-Kaneda, M., et al. (1998). Cell Death & Differentiation, 5, 20–28.
Scheiman, J., Tseng, J. C., Zheng, Y., & Meruelo, D. (2010). Molecular Therapy, 18, 63–74.
Schutte, B., Henfling, M., Kolgen, W., Bouman, M., Meex, S., Leers, M. P., et al. (2004). Experimental Cell Research, 297, 11–26.
Marceau, N., Loranger, A., Gilbert, S., Daigle, N., & Champetier, S. (2001). Biochemistry and Cell Biology, 79, 543–555.
Omary, M. B., Ku, N. O., Strnad, P., & Hanada, S. (2009). Journal of Clinical Investigation, 119, 1794–1805.
Ku, N. O., Zhou, X., Toivola, D. M., & Omary, M. B. (1999). The American Journal of Physiology, 277, G1108–G1137.
Toivola, D. M., Strnad, P., Habtezion, A., & Omary, M. B. (2010). Trends in Cell Biology, 20, 79–91.
Chang, L., & Goldman, R. D. (2004). Nature Reviews. Molecular Cell Biology, 5, 601–613.
Zhu, K., Zhao, J., Lubman, D. M., Miller, F. R., & Barder, T. J. (2005). Analytical Chemistry, 77, 2745–2755.
Chou, C. F., & Omary, M. B. (1991). FEBS Letters, 282, 200–204.
Omary, M. B., Ku, N. O., Liao, J., & Price, D. (1998). Sub-Cellular Biochemistry, 31, 105–140.
Majumdar, D., Tiernan, J. P., Lobo, A. J., Evans, C. A., & Corfe, B. M. (2012). International Journal of Experimental Pathology, 93, 305–318.
Ku, N. O., Azhar, S., & Omary, M. B. (2002). Journal of Biological Chemistry, 277, 10775–10782.
Kyriakis, J. M., & Avruch, J. (1996). Journal of Biological Chemistry, 271, 24313–24316.
Ip, Y. T., & Davis, R. J. (1998). Current Opinion in Cell Biology, 10, 205–219.
Davis, R. J. (2000). Cell, 103, 239–252.
Ku, N. O., & Omary, M. B. (1997). Journal of Biological Chemistry, 272, 7556–7564.
Feng, L., Zhou, X., Liao, J., & Omary, M. B. (1999). Journal of Cell Science, 112(Pt 13), 2081–2090.
Baricault, L., de Nechaud, B., Sapin, C., Codogno, P., Denoulet, P., & Trugnan, G. (1994). Journal of Cell Science, 107(Pt 10), 2909–2918.
Caulin, C., Salvesen, G. S., & Oshima, R. G. (1997). The Journal of Cell Biology, 138, 1379–1394.
Oshima, R. G. (2002). Cell Death and Differentiation, 9, 486–492.
Oshima, R. G., Baribault, H., & Caulin, C. (1996). Cancer Metastasis Reviews, 15, 445–471.
Mizuuchi, E., Semba, S., Kodama, Y., & Yokozaki, H. (2009). International Journal of Cancer, 124, 1802–1810.
Paramio, J. M., & Jorcano, J. L. (2002). Bioessays, 24, 836–844.
Acknowledgments
This study was supported by the KIST Gangneung Institute intramural grant (2Z03850) program and the Basic Science Research Program through the National Research Foundation (NRF) of Korea funded by the Ministry of Education, Science and Technology (2010–0024063).
Author information
Authors and Affiliations
Corresponding authors
Additional information
Dae-Geun Song and Yoon Suk Kim authors contributed equally to this manuscript.
Rights and permissions
About this article
Cite this article
Song, DG., Kim, Y.S., Jung, B.C. et al. Parkin Induces Upregulation of 40S Ribosomal Protein SA and Posttranslational Modification of Cytokeratins 8 and 18 in Human Cervical Cancer Cells. Appl Biochem Biotechnol 171, 1630–1638 (2013). https://doi.org/10.1007/s12010-013-0443-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12010-013-0443-4