Abstract
In this work a new distal interlocking system has been developed which is easy to use, allows a reduction of the operating time and consequently the exposure to radiations both for surgeon and patient. The main goal of this study has been the design of a new intramedullary nail for tibial fractures able to simplify and speed up the distal locking operation phases. After a preliminary stage during which several candidate concepts have been proposed and analysed, the best solution has been developed and deeply investigated. The new system, called “expansion nail”, has been firstly modelled by setting up a full parametric CAD model and, then, tested by running non linear FEM analyses to evaluate stresses and stability of the joining during normal working conditions. The new design has shown very high mechanical stability in the axial compression and torsional load cases. Since its very simple self-locking system, the new expansion intramedullary nail would reduce the operating time and the exposure to radiations for the surgeons as well as the patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Intramedullary nails are increasingly applied in stabilization of long bone fractures because of their advantages with regard to conventional approaches [1, 2]. Even if the optimal treatment for severe bone fractures represents a debated question [3], stabilization of long bones fractures has been obtained more and more through intramedullary nails. That because this kind of approach is minimally invasive thus allowing patient early full weigh-bearing and reduces the long time immobilization problems [4]. Intramedullary nails, moreover, compared with other types of fixator, like the external implants (plates for osteosynthesis [5], present the advantage of reducing trauma to the soft tissues [6]. This surgical technique, based on special nails (Fig. 1), is largely used for the long bones fractures, especially in the diaphyseal humeral, tibial and femoral ones, when the fracture involves the region between the two extremes (epiphyses) [7]. It consists of metal nails inserted into the medullary canal of the bone, that can be reamed if necessary. In the past, several designs have been proposed depending on the particular clinical requirements. One of the most common solution is the locked nail, used to prevent any relative rotation or sliding movements between the two bone extremities [8]. The static proximal and distal locking, in fact, maintains length and alignment of the system, provides good stability for soft tissue and bone healing, and allows early mobilisation.
Usually, two kind of fixing techniques are used: static and dynamic [9]. In static fixing, the ends of the nail are locked, both in the proximal and the distal parts (Fig. 2) of the fractured bone. In dynamic fixing, instead, the nail is fixed only at one end of the bone (proximal or distal depending on the location of the fracture); whereas the opposite extreme is free to slightly slide inside the bone [10]. The locking, generally, is obtained using screws positioned at the proximal and distal extremes of the bone (Fig. 3). Nevertheless, even if the problem of the proximal locking is solved, the distal locking technique still needs improvements. Usually, in fact, it is made manually, through a centering framework fitted to the proximal end of the nail. Due to the implant deformation during the insertion through the medullary canal, it is quite difficult to place the screws correctly. This procedure requires very long operating times and, consequently, a long exposure to ionizing radiation for surgeon, medical staff and patient. Thus, many times, surgeons are forced to leave the nail unstable reducing, in this way, the effectiveness of the intramedullary nailing technique. Moreover, the use of transversal screws can increase the risk of neuro-vascular damage slowing down the healing process [11].
Many solutions have been proposed to simplify the insertion of the distal screws [12, 13] but, unfortunately, none of them has been able to fully solve the locking problems. For these reasons some alternative devices have been developed basing on the expansion of anchoring fins or flanges [14–16]. Also these solutions, nevertheless, have shown some problems related to the system stability and high stress peaks at the bone-nail interface [17].
To overcome these problems, in this paper a new intramedullary nail is presented. The so-called “expansion nail” allows to lock the system in a very effective way, to reduce the operation time and to optimize the nail-bone surface interaction so reducing the contact stress at the interface.
2 Designing method
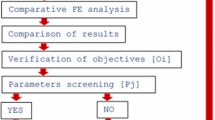
The new nail concept design has been developed following the classical redesign guidelines [18] and the principles of the simultaneous engineering approach [19]. First of all, basing on the main redesign process requirements and constraints, a large number of concepts have been proposed; after, some of the most promising solutions have been evaluated through the concept screening and concept scoring methods [18]. During the whole redesign process, in agreement with the simultaneous engineering principles, several standpoints related to the surgeons requirements, the manufacturing problems, the constraints on the nail functionality, etc., have been taken into account.
2.1 Nail concepts
First of all, a preliminary study of the state of the art has been carried out, through the analysis of the main advantages and drawbacks of the standard solutions. After, different nail concepts have been proposed by considering the following main requirements:
-
easiness of the distal locking;
-
stability of the intramedullary nail; this characteristic (in terms of torsional and sliding stability), in fact, ensures a fast and active mobilization of the injured limb, which permits, in some cases, an immediate full loading;
-
reduction of the radioscopical exposure time;
-
reduction of the surgical time;
-
possibility to use a guide-wire, that simplifies the insertion and centering operations of the nail inside the bone (that can be easily achieved using a holed nail to allow the wire insertion);
-
anatomic (ergonomic) shape of the nail to facilitate both insertion and extraction.
The most interesting concepts proposed (mainly obtained through the brainstorming technique) can be grouped into the following main typologies that make use of nails with:
-
fixed, removable or sliding guides (A);
-
internal screws (B);
-
expansion flanges (C).
Some sketches related to the concepts A, B and C are shown in Figs. 4, 5 and 6. The concepts A are quite similar to current standard solutions [20, 21]. They also use screws fixed through the bone for the distal locking but, unlike existing nails, they propose improved centering guides to drill the distal part of the bones. Concept B, instead, does not need to drill the bone for distal locking. In this solution, in fact, four screws, placed at the distal part of the nail, can be screwed in the internal part of the bone only acting on a rotating bar. The penetration of the screws tips on the bone should allow the implant locking. The sketch of the concept C is shown in Fig. 6. This solution makes use of four expanding flanges to lock the distal part of the nail-bone system.
After the analysis of the proposed concepts, carried out using two different selection matrices (concept screening and scoring), the expansion nail (concept C) has been chosen as the best solution.
3 Characteristics of the new intramedullary nail
The new intramedullary nail is composed of two main parts: an ergonomic cylindrical body and an internal screw. The ergonomic cylindrical body represents the core of the nail. It has an axial hole to allow the use of a guide-wire that simplifies the insertion of the nail. The distal side of the nail (Fig. 7) has four expanding flanges, whose external surfaces are knurled to increase the friction with the inner surface of the tibia ensuring high sliding and torsion stability. These flanges are long enough to allow a large contact area at the nail/bone interface, avoiding, in this way, high stress peaks. The expansion of the flanges is made by a particular holed screw (Fig. 8) with a taper pin on its lower end. The upper end of the screw, instead, has a hexagonal shaped hole for the insertion of a flexible Allen key. The pin is pulled inside the nail by means of the screw and, consequently, the nail expands itself as shown in Fig. 9.
Before to insert the nail, the tibia is bored (by a milling tool) in order to obtain a better (more regular) shape of its inner surface. When the milling phase is completed, the nail is inserted in the tibia, using a particular aid-tool, similar to a handle. Once positioned, the nail can be fixed at the upper and the lower ends. The proximal (upper) fixing is performed by radial screws, inserted through skin incisions and holes made on the bone. In the standard nails, the same procedure is used for the distal fixation. Through the new designed nail, instead, it is possible to fix the lower end without any skin incision or bone hole. In fact, by using a flexible hexagonal torque key, the screw is rotated until the flanges expand themselves. The expansion ensures that the external surfaces of the nail get in contact with the internal surface of the tibia, producing the required pressure for the stability of the distal locking. The nail expansion, then, must assure the suitable values of the friction forces able to eliminate any sliding or rotation of the implant under the usual working loads but, also, it should avoid any damage of the bone structure whose mechanical properties are highly variable according to species, age, etc... In particular, a maximum torque value of about 20 Nm is needed to fix the nail in a young healthy bone, which has very good mechanical characteristics.
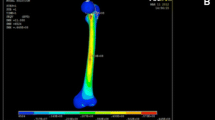
4 Virtual prototyping of the expansion nail
A virtual prototype of the designed nail has been set up to deeply investigate the new system. At first, a full parametric CAD model has been created with Solid Edge. The CAD model of the tibia, instead, has been created through computerised tomography images. This model is also available at the 3dcontentcentral web site [22], an online free CAD models library. The model of the bone has been subdivided into two parts to simulate a full fracture in the middle of the tibia. The screws used to fix the proximal part of the bone have been also modelled in a simplified way (only considering the cylindrical part of the stem) (Fig. 10).
A preliminary interference analysis to verify the coupling between the nail and the bone has been made with Solid Edge. Several sections of the assembly (Fig. 11) have been checked to exclude compenetrations between the components of the implant and the tibia.
Successively, a FEM model of the assembly has been carried out with the aim of estimating the structural behaviour of the nail and evaluating the performances of the system under the normal working conditions.
4.1 Finite element models set up
The new designed “expansion nail” has been studied by means of non linear FEM analyses using the numeric code ANSYS. The FEM analyses have been set up to verify the effectiveness of the distal locking, to define the right nail positioning inside the bone and to evaluate the nail behaviors (in terms of mechanical resistance) under the usual working loads [23] to which the tibia is subject after the surgery.
The first step has been the importing of the CAD models in the FEM package. Thus, the nail components and the bone models have been meshed by using solid elements with ten nodes and 3 degrees of freedom for each node. Because of the particular shape of the tibia, tetrahedral elements have been used for the mesh (Fig. 12); nevertheless, to obtain all the same very accurate results, the quadratic formulation of the displacement function has been used for the finite elements. After meshing the models, the contact surfaces among different components have been identified. In particular, the contact surfaces nail/internal screw with taper pin, nail/tibia, nail/distal screws and tibia/distal screws have been defined. Moreover, to reduce the simulation time without reducing the result accuracy, only particular select areas (and not the whole components surfaces) have been used as contact pairs, as shown in Fig. 13, where only restricted parts of the nail (flanges) and the internal screw (taper pin) have been selected to consider the nail/internal screw contact couple.
The material used for the nail is the Ti6Al4V (90 % titanium, 6 % aluminum, 4 % vanadium), a titanium alloy largely employed for medical implants but also used in several industrial sectors like aerospace, chemical, marine and automotive. Ti6Al4V alloy is a very favourable material for medical implants thanks to its mechanical characteristics (e.g. good tensile strength and compression, good resistance to fatigue and corrosion) and, especially, its excellent biocompatibility level which represents an essential property for orthopaedic implants. Table 1 shows some of the main mechanical properties of a common Ti6Al4V alloy, whose values also depend on the technological processes and heat treatments.
Basing on previous works [24–26] on the characterization and modeling of the mechanical properties of a bone structure, the tibia material has been considered having a linear, elastic, orthotropic behavior, following the Hooke’s laws. Moreover, to simplify the FEM analyses, the layered structure of the bone has been neglected by only considering the cortical bone. This simplification does not introduce any remarkable error because the trabecular bone structure has very low mechanical properties but, also, because most of the trabecular parts in the bone-implant interface are removed during the regularization drilling phase. The main mechanical properties of the bone material are shown in Table 2. Concerning the radial screws used for the proximal locking, common steel mechanical properties have been used (Young modulus = 210 Gpa and Poisson coefficient = 0.3).
Finally, to complete the FEM model, the suitable boundary conditions (loads and displacements) have been imposed on the nail components and the tibia. This step was carefully carried out to correctly simulate the real working conditions but also to simplify the assembly FEM model.
4.2 Simulating the working conditions
Three different load cases have been considered. In the first one, the expansion of the flanges due to the taper pin insertion has been analysed, the second and third load cases, instead, have been defined to simulate, respectively, a compression and torsion testing.
4.2.1 Expansion load case
To simulate the insertion of the taper pin needed to expand the nail flanges, a z-axis displacement equal to 30 mm has been imposed on the lower end surface of the taper pin simulating, in this way, its total insertion inside the nail. Moreover, additional boundary conditions have been imposed on the external surface of the bone to avoid any irregular movement of the assembly. Figure 14 shows the obtained expansion of the nail according to the imposed boundary conditions. Two different sections of the nail/tibia assembly, before and after the expansion of the flanges, are shown in Fig. 15. One can note that the inner surface of the bone (even if the tibia is reamed) has an irregular shape and that causes a not uniform contact between the external surface of the nail and the tibia, but also not symmetrical displacements of the flanges in radial directions (Fig. 16). For this reason, the pressure distribution generated at the contact surfaces between nail/screw and nail/tibia is not uniform. Despite this, the contact pressure distribution (Fig. 17), even if irregular, ensures admissible stress values and it is enough to guarantee the distal locking of the tibia, as verified in the following compression and torsion tests. The maximum pressure value at the nail-bone interface is comparable with the one calculated in the contact between the screws (used for the proximal locking) and the bone.
4.2.2 Compression load case
Starting from the expansion load case, which represents the initial working condition, additional boundary conditions have been imposed to the FEM models. The compression analysis is useful to verify the stability of the distal locking as well as calculating the stress distribution on the nail components and on the bone. It is very important, in fact, to know the stresses distribution on the tibia, to be sure that the new nail is safe and does not cause, under the usual working loads, any new post-fracture of the tibia. The compression test has been set up by imposing 700 N of axial load (equivalent to the weight of a patient of approximately 70 kg) [27] on the upper (plane) surface of the tibia. On the opposite side, a constraint on the axial displacement (z-axis direction) has been applied on the tibia to impose a pure compression load on the nail/tibia assembly. The boundary conditions and the reactions forces acting on the FEM model are shown in Fig. 18. Some reaction forces can be noted on the distal part of the assembly: this confirms the correct contact between the nail and the tibia. The obtained results, moreover, show no relative axial displacements of the bone parts so demonstrating the effectiveness of the distal locking. As regards the contact pressure at the nail/tibia interface, its distribution is almost unchanged in comparison with the expansion load case results. Only a slight increase of the maximum values has been noted. Figures 19 and 20 show the Von Mises stress maps on the tibia and the nail. In the bone the most stressed regions are those far from the fracture; the middle of the tibia is practically unloaded. This confirms the efficacy of the locking obtained through the expansion nail. As expected, in fact, loads are transmitted from the bone to the nail through the proximal screws but also by the interface between the flanges and the distal part of the tibia.
The obtained results show the range of stress values on the distal part of the bone are largely admissible, they, in fact, vary from 50 to 70 Mpa. The calculated safety factor is higher than 2, considering the ultimate strength of the cortical bone as about 150 MPa. Also in the nail, as expected, the proximal and distal areas are the most stressed. The range of stress values, in this case, vary from 130 to 250 Mpa. These values are largely lower than the yield strength (760–895 MPa) of the Ti6Al4V alloy used for the nail. Finally, the maximum Von Mises stress calculated on the proximal locking screws is about 130 Mpa.
4.2.3 Torsion load case
Usually, even if the normal working condition of a fractured tibia should only be a cyclical compression load, accidental torsional loads can also occur. For this reason, a torsion test has been executed on the new expansion nail to evaluate the implant performances when subjected to torsional loads. This kind of test, moreover, is experimentally performed when real nail prototypes must be verified. In this case the setup of a torsion testing machine has been modelled. In particular, the device shown in Fig. 21 has been modelled and connected to the upper surface of the tibia. The opposite side of the bone, instead, has been constrained along the x, y and z directions. To simulate a torque value equal to 8 Nm (this value is commonly used during stiffness tests of long bones [27]), a pressure of 1.42 MPa was applied on the four faces of the device. The obtained results, in terms of Von Mises stress distributions, are presented in Figs. 22 and 23.
The maximum stress value measured on the distal part of the bone is about 70 Mpa; this value, as noted in the previous section, is largely lower than the ultimate strength of the cortical bone material (about 150 Mpa) and this represents a good result in terms of tibia resistance under accidental torsional loads. Figure 22, moreover, shows another very interesting result: the middle part of the fractured bone is fully unstressed. This event demonstrates the effectiveness of the expansion nail; external loads, in fact, are transmitted from the distal part to the proximal one of the tibia (by means of the nail) without stressing the fractured region of the tibia itself.
Concerning the nail, the obtained results show some differences in terms of stress distribution in comparison with the compression load case. In particular, a slight stress values increasing has been noted near the proximal screw holes. Also in this case, nevertheless, the most stressed areas are those related to the proximal and distal locking regions but, in a similar way, the maximum evaluated Von Mises stress (about 280 MPa) is much smaller than the material yield strength. During the torsion load case, the proximal screws are more stressed than the compression test but the maximum Von Mises stress is still lower than the yield strength of the used steel.
The contact pressures at the nail/tibia interface are similar to the ones obtained in the compression testing. No relative movement has been noted between the implant and the bone, so demonstrating how the friction tangential forces are enough to avoid any rotation of the nail, ensuring a good distal locking and an optimal load transmission between the nail and the tibia.
5 Conclusions
The intramedullary nail technique has the advantage to reduce the period of immobilisation of patients with fractured bones allowing the partial use of the limb as soon as after the operation. Moreover, this surgical technique is quite simple to adopt and it is not particularly invasive. The main disadvantages are related to the distal locking of the nail that requires long operation times and exposition to radiations for the surgeon as well as the patient.
In this paper a new tibial intramedullary nail has been designed. The new designed system, called “expansion nail”, thanks to its innovative distal locking system, ensures the axial stability of the system and simplifies the surgical procedure.
In order to test the mechanical properties of the new nail, a virtual prototyping approach has been used. The implemented fully parametric CAD model has been created to allow fast and easy changes of the shape, whereas the FEM model of the nail/tibia assembly has been set up in order to evaluate the system performances under the usual working conditions.
Three different load conditions (expansion, compression and torsion) have been investigated. From the obtained results emerge the extension of the nail-bone interface area and the produced contact stress are enough to ensure the system stability. No longitudinal or rotational sliding, in fact, has been noted during the numerical simulations.
Moreover, as regards the stress distributions, in all the analysed load cases, both the tibia and the nail have a maximum Von Mises stress largely lower than the materials yield strengths.
Finally, based on the results of this study, it has been shown that the new expansion nail represents an improvement over the standard systems.
The proposed surgical implant is simple and needs only a short time to learn the new distal locking technique. Moreover, unlike standard solutions, this procedure is mainly independent on the expertise of the surgeon. Given the handling advantages by the new self-locking intramedullary nail, the use of this system would reduce the surgical operating times and consequently the exposure to radiation for the surgeon as well as the medical staff and the patient.
Future works would be addressed to clinical trials (performed through real prototypes) to evaluate the performances of the nail under normal working conditions. Moreover, additional tests could be carried out to estimate the fatigue life of the implant subjected to cyclic loads.
References
Brumback, R.J.: The rationales of interlocking nailing of the femur, tibia, and humerus: an overview. Clin. Orthop. 324, 292–320 (1996)
Leung, I.: Practice of Intramedullary Locked Nails. Scientific Basis and Standard Techniques. Springer, Berlin (2002)
Amin, A., Mahaluxmivala, J., Ramkumar, U., Hill, R.: Failure of the spiral blade and intramedullary nail in the treatment of ipsilateral femoral neck and shaft fractures. Injury Extra 38, 84–87 (2007)
Griza, S., Zimmer, C.G., Reguly, A., Strohaecker, T.R.: A case study of subsequential intramedullary nails failure. Eng. Failure Anal. 16, 728–732 (2009)
Bell, M.J., Beauchamp, C.G., Kellam, J.K., McMurtry, R.Y.: The results of plating humeral shaft fractures in patients with multiple injuries. J. Bone Joint Surg. 67B, 293–296 (1985)
Lin, J., Hou, S.M., Inoue, N., Chao, E.Y.S., Hang, Y.S.: Anatomic considerations of locked humeral nailing. Clin Orthop. Relat. Res. 368, 247–254 (1999)
Babin, S., Graf, P., North, J., Schvingt, E.: Le risqué septique de l’ostéosynthése à foyer fermé d’aprés une série continuede 1059 enclouages selon G. Kuntscher, Intern. Orthop. (1981)
Johnson, K.D., Tencer, A.F., Blumenthal, S., August, A., Johnston, U.: Biomechanical performance of locked intramedullary nail systems in comminuted femoral shaft fractures. Clin. Orthop. Relat. Res. 206, 84 (1986)
Wu, C.C., Tai, C.L.: A biomechanical comparison of unlocked or locked reamed intramedullary nails in the treatment of mid-third simple transverse femoral shaft fractures. Chang Gung Med. J. 29, 275–282 (2006)
Russell, T.A., Taylor, J.C.: Interlocking intramedullary nailing of the femur: current concepts. Semin. Orthop. 1, 217–231 (1986)
Rupp, R.E., Chrissos, M.G., Ebraheim, N.A.: The risk of neurovascular injury with distal locking screws of humeral intramedullary nails. Orthopedics 19, 593–595 (1996)
Arlettaz, Y., Akiki, A., Chevalley, F., Leyvraz, P.F.: Targeting device for intramedullary nails: a new high-stable mechanical guide; Injury. Int. J. Care Inj. 39, 170–175 (2008)
Abdlslama, Kalid M., Bonnaire, F.: Experimental model for a new distal locking aiming device for solid intramedullary tibia nails. Inj. Int. J. Care Inj. 34, 363–366 (2003)
Seidel, H.: Humeral locking nail: a preliminary report. Orthopedics 12, 219–226 (1989)
Knothe, U., Knothe, M.L., Klaue, K., Perren, S.M.: Development and testing of a new self-locking intramedullary nail system: testing of handling aspects and mechanical properties. Injury. Int. J. Care Inj. 31, 617–626 (2000)
Jovanovic, A., Pirpiris, M., Semirli, H., Doig, S.G.: Fixion™nails for humeral fractures. Injury 35(11), 1140–1142 (2004)
Giudice, F., La Rosa, G., Russo, T., Varsalona, R.: Evaluation and improvement of the efficiency of the Seidel humeral nail by numerical-experimental analysis of the bone-implant contact. Med. Eng. Phys. 28, 682–693 (2006)
Otto, K., Wood, K.: Product Design—Techniques in Reverse Engineering and New Product Development. Prentice-Hall, New Jersey (2001)
Parasaei, H.R., Sullivan, W.G.: Concurrent Engineering Contemporary Issues and Modern Design Tools. Chapman and Hall, Melbourne (1993)
http://www.bioimpianti.it/linea_trauma_omero-Clos.html (2009). Accessed 22 March 2009
http://www.synthes.com/ (2011). Accessed 17 Jan 2011
http://www.3dcontentcentral.com/ (2008). Accessed 18 Oct 2008
Goldstein, S.A., Choi, K.: A comparison of the fatigue behavior of human trabecular and cortical bone tissue. J. Biomech. 25, 1371–1381 (1992)
Seeley, R.R., Stephens, T.D., Tate, P.: Anatomy and Physiology, 3Rev Ed edn. Mosby College (1995)
Thibodeau, G.A.: Anatomy and Physiology, 6th edn. Mosby (2006)
Ionescu, I., Conway, T., Schonning, A, Almutairi, M., Nicholson, D.W.: Solid modeling and static finite element analysis of the human tibia. Mechanical, Materials and Aerospace Engineering Department, College of Engineering University of Central Florida, Orlando, Florida (2003)
Wang, G., Pan, T., Peng, X., Wang, J.: A new intramedullary nailing device for the treatment of femoral shaft fractures: a biomechanical study. Clin. Biomech. 23, 305–312 (2008)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ingrassia, T., Mancuso, A. Virtual prototyping of a new intramedullary nail for tibial fractures. Int J Interact Des Manuf 7, 159–169 (2013). https://doi.org/10.1007/s12008-012-0175-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12008-012-0175-7