Abstract
Background
Aseptic complications such as stress shielding leading to bone loss are major problems associated with revision of cemented and uncemented long-stem tumor endoprostheses. Endoprosthetic reconstruction using compressive osseointegration fixation is a relatively new limb salvage technology designed to enhance osseointegration, prevent stress shielding, and provide fixation for short end-segments.
Questions/purposes
(1) What is the survivorship of this technique at minimum 5-year followup? (2) Were patient factors (age, sex, body mass index), oncological factors, or anatomic locations associated with implant failure? (3) Were there any prosthesis-related variables associated with failure?
Methods
A single-center, retrospective review of patients with a minimum 5-year followup (mean, 8 years; range, 5–12 years) treated with an osseointegration compressive device for endoprosthetic fixation of proximal and distal femoral limb salvage reconstructions was performed. We have previously published the implant survivorship of this patient cohort with a minimum 2-year followup and are now reporting on the 5-year survivorship data. From 2002 to 2008, we performed 22 such procedures in 22 patients. Four patients died of their disease within 5 years of surgery and all surviving patients (n = 18) had complete followup data at a minimum of 5 years. General indications for this device during that time were pediatric and adult patients requiring primary endoprosthetic reconstructions of the proximal or distal femur for benign and malignant bone lesions. The primary outcome was reoperations for mechanical (aseptic) failures. Secondary outcomes included implant removal for nonmechanical failures and any patient-, oncological-, or implant-related variables associated with implant removal.
Results
At a minimum of 5 years followup, overall mechanical (aseptic) implant survivorship was 16 of 18. Survivorship for all modes of failure (oncological failure, infection, arthrofibrosis, and mechanical failure) was 12 of 18. All mechanical failures occurred early, within the first 30 months. We identified no patient-, oncological-, or implant-related features predictive of failure.
Conclusions
Our intermediate-term experience with compressive osseointegration fixation for endoprosthetic limb reconstructions demonstrates with longer clinical followup, no additional mechanical failures were observed as compared with our early analysis. Our experience with this fixation at a minimum of 5-years followup adds to a very limited but increasing body of literature demonstrating that after a transient period of increased risk for implant failures, survivorship stabilizes. Assessment of this fixation strategy beyond 10 years of clinical followup is needed.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the past 20 years the combination of improved systemic therapies, high-resolution cross-sectional imaging modalities, and evolving technological advances in orthopaedic implant design has afforded greater opportunity for limb salvage after the oncological resection of malignant bone neoplasms. Most limb salvage procedures performed today are reconstructed using modular tumor endoprostheses. However, the ideal fixation method for endoprosthetic limb salvage reconstructions of the lower extremity remains controversial. Presently, long-stem cemented and uncemented stems are the standard fixation methods for most endoprosthetic reconstructions [17, 22, 25]. However, the vast majority of patients undergoing limb salvage are children and young adults and therefore in those who survive their disease, revision operations are likely [1, 12, 16].
Revision procedures for stemmed tumor endoprostheses are complicated by numerous variables intrinsic to modern implant designs such as bone resorption secondary to stress shielding, periprosthetic fractures, cement extrication, and fixation of short end-segments [14, 20, 22, 26]. As a consequence of these issues, novel endoprosthetic fixation strategies are needed. The application of compressive osseointegration for the fixation of tumor endoprostheses is a relatively new strategy, which theoretically has the potential to mitigate some of the revision issues associated with contemporary long-stemmed components. Using compressive osseointegration technology, a compressive force is continuously loaded across the bone-implant interface and, in accordance with Wolff’s law [11], bone at the bone-implant interface hypertrophies over time. Potential advantages of this technology, at least in the short term, include bony ingrowth into the porous surface of the component, reduced stress shielding, the ability to fix the implant when a short working length of bone is present, protection of the medullary canal from particulate debris, and preservation of bone stock (Fig. 1) [5, 7, 8, 19]. Many of these attributes may positively influence later revision surgeries as a result of bone stock preservation and short segment fixation.
Radiographs demonstrating some of the advantageous applications associated with compressive osseointegration fixation. Compared with radiographs obtained the day of surgery (A), progressive bone hypertrophy (white arrow) at the bone-implant interface is noted radiographically at the 5-year followup visit of one the patients from this study cohort (B). In a different patient, proximal extension of an osteogenic sarcoma was not compatible with conventional long-stem fixation (C). However, the short working length of compressive osseointegration fixation enabled stable fixation of this short end segment at 5-year clinical followup (D).
Compressive osseointegration fixation for limb salvage reconstructions of the femur has been FDA-approved since 2003. Numerous groups have published their short-term results using this fixation device in patients with primary and revision limb salvage reconstructions for primary bone malignancies of the lower extremity. Implant survival in these studies has been promising, ranging from 80% to 90% at 5 years [7, 15, 23]. These numbers are comparable with results of long-stem cemented and uncemented fixation techniques [1, 12, 16, 22]. Given compressive osseointegration fixation of endoprosthetic reconstructions is a relatively new technology, continued longer-term followup of these devices is required.
We have previously published our minimum 2-year followup of this device [7]; the purpose of the present study was to evaluate the following questions: (1) What is the survivorship of this technique at minimum 5-year followup? (2) Were patient factors (age, sex, body mass index [BMI]), oncological factors, or anatomic locations associated with implant failure? (3) Were there any prosthesis-related variables associated with failure?
Patients and Methods
Patient Selection and Data Collection
A single-center, retrospective cohort of patients was identified from our institutional database and included in the analysis. Institutional review board approval for the study was obtained. We previously reported on this group of patients at a minimum of 2 years followup [7]; here we extend the followup to a minimum of 5 years. At our institute, all patients presenting with a neoplasm of the lower extremity long bones requiring an oncologic resection and an endoprosthetic limb salvage reconstruction are considered for compressive osseointegration fixation. Because osseointegration fixation of long bone endoprostheses requires an intact bone healing response and a transient period of weightbearing restriction, patients with metastatic lesions, prior radiation to the bone, and patients with a limited life expectancy are absolute contraindications to compressive osseointegration. Treatment with postoperative consolidative chemotherapy was not considered a contraindication. Patients older than 50 years of age, patients with systemic medical conditions thought to impair bone healing (diabetes, peripheral vascular disease, smoking, etc), or patients with poor bone density were relative contraindications to compressive osseointegration. During the patient accrual period, all proximal or distal femoral resections in adult or pediatric patients, reconstructed with an articulating endoprosthesis using compressive osseointegration fixation with a minimum 5 years of clinical followup, were included for evaluation. Patients with upper extremity, pelvic, or tibial fixation were excluded as were patients reconstructed using intercalary endoprosthetic devices.
Postoperative followup was performed at 6 weeks, 3 months, and 6 months. Beyond this, followup was every 3 to 6 months depending on individual oncologic surveillance protocols. Operative reports, implant records, clinic notes, and radiographs for each patient were reviewed. Demographic data, diagnoses at presentation, adjuvant oncological therapies, operative details, oncologic outcomes, and subsequent need for reoperation for any reason were recorded.
Patient Demographics and Diagnoses
Twenty-seven patients treated with a compressive osseointegration device before December 2008 were identified. Nine patients were excluded from the final analysis: four patients with fixation of the upper extremity, tibia, or pelvis; four patients died of their disease before 5 years followup; and one patient was treated with an intercalary device. No patients were lost to followup. A total of 18 implants in 18 patients were evaluated in the study cohort (Table 1). Average followup for the entire group was 8 years (range, 5–12 years). The average age of the cohort at the time of surgery was 21 years (range, 7–47 years). The male-to-female ratio was 10:8; osteosarcoma was the oncologic diagnosis in the majority of patients (n = 13) followed by Ewing’s sarcoma (n = 2), undifferentiated pleomorphic sarcoma of bone (n = 2), and chondrosarcoma (n = 1). Anatomic resection levels included the distal femur in 15 patients and the proximal femur in three patients.
Surgical Technique
All operations were performed by our sarcoma team; surgical approach, soft tissue resections, and bone resection length were individualized based on the imaging and clinical characteristics of the specific tumors. The Compress® (Biomet, Warsaw, IN, USA) osseointegration fixation device was used in all cases in accordance with the manufacturer’s recommended techniques. All bone cuts were carefully made perpendicular to the long axis of the bone under continuous irrigating to minimize thermal necrosis. Care was taken to avoid excessive periosteal stripping at the level of bone resection. A spindle-sizing guide was used to select the appropriate spindle diameter (small or large) based on the diameter of the femur at the resection level. Custom spindles were used in cases in which the postresection bone end available for fixation was anticipated to be a shape or size not complimentary to the standard manufacturer spindle sizes (small, 38 cm diameter; large, 44 cm diameter). In one patient, in whom fixation was required at the metadiaphysis of the proximal femur, a custom spindle was used. In two other cases, a custom spindle was used for fixation to a small-diameter pediatric femoral diaphysis. Compressive force at the implant-bone interface was determined based on the cortical thickness of the bone per the manufacturer’s guidelines. Antirotation pins were used at the discretion of the surgeon and were not used in all cases. For all distal femoral reconstructions, the Biomet® Orthopaedic Salvage System (OSS™) rotating hinge knee articulation was used. Bipolar hemiarthroplasty components were used for resections of the proximal femur. For all patients, irrespective of chemotherapy status, the postoperative weightbearing protocol was 6 weeks of strict nonweightbearing followed by progression to weightbearing as tolerated. Oral and intravenous antiinflammatories were not administered in the hospital and strongly discouraged after discharge from the hospital.
Statistical Analysis
The primary endpoints evaluated in this analysis were implant removal for either mechanical (aseptic) failures, defined as implant bending/breakage, implant rotational instability, catastrophic implant failure, and periprosthetic fractures, or nonmechanical failures such as infection, unacceptable leg length discrepancy, joint dislocations, chronic pain, arthrofibrosis, or local disease recurrence. For each failure subgroup (mechanical and nonmechanical failures), survival was estimated using a Kaplan-Meier survival analysis [18] starting on the date of the operation and ending on the date of implant removal or latest followup. Cox proportional hazards models were used to assess whether any patient, implant, or oncological variables were associated with mechanical failure or any mode of failure. Fisher’s exact tests (for categorical variables) and logistic regression models (for continuous variables) were used to assess whether those same variables were associated with failure independent of time to failure. All statistical analyses were performed using the computing environment R (Version 2.8.0; R Statistical Computing Software, Vienna, Austria).
Results
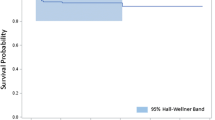
Implant survivorship, using component removal for any reason, was 12 of 18 at minimum 5-year followup (Fig. 2A). Using mechanical (aseptic) failure as an endpoint, implant survivorship was 16 of 18 at minimum 5-year followup (Fig. 2B). A total of six implants were removed for reasons including infection (n = 2) arthrofibrosis (n = 1), local recurrence of disease (n = 1), and mechanical (aseptic) failure (n = 2). The mean time to component removal for all causes of failure was 21 months (range, 4–44 months). All mechanical failures (n = 2) occurred at the osseointegration site; one case was associated with bending of the traction bar and loosening of the spindle and the other case was the result of loosening and malrotation at the bone-implant interface. Both mechanical failures occurred in pediatric patients, ages 9 and 13 years, and were associated with an activity-related ground-level fall. No periprosthetic fractures were observed. Both mechanical failures occurred within the first 30 months postoperatively: one at 17 months and the other at 29 months.
Kaplan-Meier plots demonstrating survivorship of compressive osseointegration fixation at a minimum 5 years clinical followup. When considering all modes of implant failure (infection, oncological failure, arthrofibrosis, and aseptic failures), survivorship was 67% (A). Looking only at aseptic (mechanical) failures, survivorship was 89% at a minimum 5 years clinical followup (B). All mechanical failures occurred within 30 months and survivorship was stable afterward.
With the numbers available, no measured patient, oncological, or implant factors were associated with implant removal or mechanical failure (Tables 2, 3). The average BMI of this study cohort was low, which is not surprising given the young age and cancer diagnosis in this population. Sixteen of 18 patients received neoadjuvant and adjuvant chemotherapy as part of their systemic cancer therapy; of the two mechanical failures, one received chemotherapy, whereas the other patient did not. Antirotation pins were used in 11 of 18 patients; of the two mechanical failures, one implant had antirotation pins, whereas the other did not. The average bone resection length was 19 cm (range, 10–31 cm). Both mechanical failures were in patients with a resection length close to the mean (16 and 18 cm, respectively). In 10 of 18 cases, a large spindle size was used and in three of 18 cases, a custom spindle was used. One of the three custom spindles experienced a mechanical failure with the other mechanical failure occurring in a patient with a large spindle size.
Discussion
Compressive osseointegration fixation is an appealing novel technology for the fixation of tumor endoprostheses of the lower extremity. The principal potential advantages of this technique include preservation of bone stock, prevention of stress shielding, and a short working length of bone necessary for fixation of the implant. These potential benefits have been observed in human and animal studies [5, 8, 19]; however, given that this is relatively new technology for lower extremity limb salvage procedures, there is a paucity of studies documenting the intermediate- and long-term survivorship of these devices. We previously evaluated this group of patients at a minimum of 2 years [7]; here we sought to evaluate the survivorship of these implants at a minimum 5-year clinical followup. In this series, we observed aseptic (mechanical) failures in two of 18 patients with no additional mechanical failures beyond 30 months of clinical followup.
This was a retrospective evaluation of a single-center patient cohort with inherent limitations given this study design. First, the small sample size of the study population potentially introduces a source of Type II error in the assessment of patient-, oncologic-, and implant-related factors associated with failure and revision. It is likely that our inability to demonstrate any patient-, oncological-, surgical-, or implant-related factors predictive of implant failure was simply the result of an insufficiently large sample size; larger studies are called for to evaluate those parameters, some of which might well be clinically important. Second, patient outcomes were not evaluated in this study; therefore, correlating survivorship data to outcome metrics such as patient satisfaction and functional performance was not possible. This is relevant given that a potential drawback of compressive osseointegration fixation for tumor endoprostheses is the required period of postoperative nonweightbearing. Finally, a clinical and economic comparison to conventional long-stem endoprosthetic devices was not incorporated into this study design. However, outcome data and a direct comparison of this technology to conventional stem designs were not the intent of this investigation. Given the promising short- and intermediate-term followup with this device, well-designed prospective studies evaluating the latter two shortcomings of this study would be justified and valuable.
We have previously reported on the survivorship of compressive osseointegration fixation of tumor endoprostheses with minimum 2 years followup [7]. This previous study included 51 patients from two centers and four surgeons and reported an aseptic (mechanical) survivorship of 86%. In the present cohort limited to 18 patients with now longer clinical followup of at least 5 years, no additional (late) failures were noted. Our overall survivorship for all modes of failure was 12 of 18, which, in addition to the two mechanical failures, included two implants removed for late periprosthetic infection, one implant removed for local recurrence, and another implant removed in favor of a turn-up-plasty procedure in a pediatric patient who developed a severe knee contracture after multiple lengthening procedures. These types of nonmechanical complications are unfortunate but expected observations after large endoprosthetic reconstructions for bone malignancies in pediatric and adult patients [9, 16].
Similar to previous studies with this implant, all failures occurred within the first 30 months [7, 10, 15]. In the largest published series using the Compress® osseointegration implant, Healey et al. [15] reported their followup of a cohort of 82 patients and of the 26 patients with greater than 5-year followup, only one failure was noted. Their overall 5- to 10-year implant survivorship was 83% at a minimum 5-year followup. We feel these observations highlight an important characteristic of compressive osseointegration for fixation of limb salvage endoprostheses: after a transient period of risk for early mechanical failures, survival of these implants stabilizes beyond 5 years. Most comprehensive survivorship studies evaluating conventional long-stem devices show progressive aseptic failures over time with aseptic implant survival ranging from 60% to 75% at 10- to 15-year followup [12, 14, 16, 20]. However, it should be noted that 10- to 15-year survivorship of > 90% has been reported for both cemented [24] and uncemented [21] distal femoral endoprostheses in select centers. These studies demonstrate that durable survival with these implants is possible, although these results may not be generalizable to all centers performing this type of joint reconstruction.
The results of this study and others suggest compressive osseointegration is an acceptable alternative for the fixation of tumor endoprostheses with intermediate-term mechanical survivorship ranging from 84% to 89% [7, 15]. However, at present, there is little evidence to suggest this technology is superior to conventional long-stemmed components. In two retrospective comparative studies [10, 23], early to intermediate survivorship of compressive osseointegration fixation for distal femoral limb salvage arthroplasties was equivalent to both cemented and uncemented long-stemmed distal femoral arthroplasties. Similar to our data and others, the osseointegration failures in these comparative studies occurred early, whereas the traditional stems progressively failed over time. A prospective comparison of these fixation technologies is needed as are studies documenting the efficacy of compressive osseointegration in revision situations. In a recent report [3], compressive osseointegration fixation was used for revision of failed endoprostheses with massive segmental bone defects. In their series, 93% of implants achieved stable osteointegration at a mean followup of 17 months, highlighting the potential use of these implants for complex revision procedures.
With the relatively small numbers of patients in this report, we found no predictive patient- or implant-related factors that were associated with failure. However, the small sample size precludes any relevant conclusions. Other evaluations of this technology have also failed to demonstrate patient- or implant-related factors predictive of implant failure [4, 7, 10, 15]. This could be an ongoing manifestation of underpowered study designs or related to a predictive variable difficult to measure in such a heterogeneous patient population. A proposed advantage of compressive osseointegration technology is fixation into short end-segments. In oncological bone resections, short end-segments are often the result of large resection lengths. Increased femoral resection length beyond 14 cm or > 40% of total length has been associated with early failures in cemented and uncemented long-stem prostheses [6, 13]. Although underpowered to properly evaluate this with the present cohort, other assessments of this technology have demonstrated that resection length is not associated with implant failure [2, 7].
In conclusion, compressive osseointegration fixation remains a new technology for the fixation of lower extremity endoprosthetic limb salvage reconstructions. To date, the literature on intermediate to late outcomes is extremely limited. Increasing experience with these devices demonstrates that intermediate-term outcomes may be comparable to conventional long-stemmed fixation, but this has not been demonstrated in controlled trials. Although our numbers are small, our experience with this fixation at a minimum of 5 years followup adds to a very limited but increasing body of literature demonstrating that after a transient period of increased risk for implant failures, survivorship stabilizes. Evaluation of these devices beyond 10 years is needed to further understand the role of this fixation strategy in limb salvage surgery as compared with alternative conventional methods, the latter of which are demonstrating an increasing propensity for late failure and associated loss of bone stock.
References
Ahlmann ER, Menendez LR, Kermani C, Gotha H. Survivorship and clinical outcome of modular endoprosthetic reconstruction for neoplastic disease of the lower limb. J Bone Joint Surg Br. 2006;88:790–795.
Avedian RS, Goldsby RE, Kramer MJ, O’Donnell RJ. Effect of chemotherapy on initial compressive osseointegration of tumor endoprostheses. Clin Orthop Relat Res. 2007;459:48–53.
Beauchamp CP, Schwartz AJ, Rose PS, Sim FH, Harmson S, Hattrup SJ. Revision of failed megaprosthetic reconstructions using compressive osseointegration. J Bone Joint Surg Br. 2013;95:132.
Bhangu AA, Kramer MJ, Grimer RJ, O’Donnell RJ. Early distal femoral endoprosthetic survival: cemented stems versus the Compress implant. Int Orthop. 2006;30:465–472.
Bini SA, Johnston JO, Martin DL. Compliant prestress fixation in tumor prostheses: interface retrieval data. Orthopedics. 2000;23:707–711; discussion 711–712.
Blunn GW, Briggs TW, Cannon SR, Walker PS, Unwin PS, Culligan S, Cobb JP. Cementless fixation for primary segmental bone tumor endoprostheses. Clin Orthop Relat Res. 2000;372:223–230.
Calvert GT, Cummings JE, Bowles AJ, Jones KB, Wurtz LD, Randall RL. A dual-center review of compressive osseointegration for fixation of massive endoprosthetics: 2- to 9-year followup. Clin Orthop Relat Res. 2014;472:822–829.
Cristofolini L, Bini S, Toni A. In vitro testing of a novel limb salvage prosthesis for the distal femur. Clin Biomech (Bristol, Avon). 1998;13:608–615.
Eckardt JJ, Kabo JM, Kelley CM, Ward WG, Sr., Asavamongkolkul A, Wirganowicz PZ, Yang RS, Eilber FR. Expandable endoprosthesis reconstruction in skeletally immature patients with tumors. Clin Orthop Relat Res. 2000;373:51–61.
Farfalli GL, Boland PJ, Morris CD, Athanasian EA, Healey JH. Early equivalence of uncemented press-fit and Compress femoral fixation. Clin Orthop Relat Res. 2009;467:2792–2799.
Frost HM. Wolff’s Law and bone’s structural adaptations to mechanical usage: an overview for clinicians. Angle Orthod. 1994;64:175–188.
Gosheger G, Gebert C, Ahrens H, Streitbuerger A, Winkelmann W, Hardes J. Endoprosthetic reconstruction in 250 patients with sarcoma. Clin Orthop Relat Res. 2006;450:164–171.
Guo W, Ji T, Yang R, Tang X, Yang Y. Endoprosthetic replacement for primary tumours around the knee: experience from Peking University. J Bone Joint Surg Br. 2008;90:1084–1089.
Ham SJ, Schraffordt Koops H, Veth RP, van Horn JR, Molenaar WM, Hoekstra HJ. Limb salvage surgery for primary bone sarcoma of the lower extremities: long-term consequences of endoprosthetic reconstructions. Ann Surg Oncol. 1998;5:423–436.
Healey JH, Morris CD, Athanasian EA, Boland PJ. Compress knee arthroplasty has 80% 10-year survivorship and novel forms of bone failure. Clin Orthop Relat Res. 2013;471:774–783.
Henderson ER, Groundland JS, Pala E, Dennis JA, Wooten R, Cheong D, Windhager R, Kotz RI, Mercuri M, Funovics PT, Hornicek FJ, Temple HT, Ruggieri P, Letson GD. Failure mode classification for tumor endoprostheses: retrospective review of five institutions and a literature review. J Bone Joint Surg Am. 2011;93:418–429.
Hwang JS, Mehta AD, Yoon RS, Beebe KS. From amputation to limb salvage reconstruction: evolution and role of the endoprosthesis in musculoskeletal oncology. J Orthop Traumatol. 2014;15:81–86.
Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481.
Kramer MJ, Tanner BJ, Horvai AE, O’Donnell RJ. Compressive osseointegration promotes viable bone at the endoprosthetic interface: retrieval study of Compress implants. Int Orthop. 2008;32:567–571.
Mittermayer F, Krepler P, Dominkus M, Schwameis E, Sluga M, Heinzl H, Kotz R. Long-term followup of uncemented tumor endoprostheses for the lower extremity. Clin Orthop Relat Res. 2001;388:167–177.
Mittermayer F, Windhager R, Dominkus M, Krepler P, Schwameis E, Sluga M, Kotz R, Strasser G. Revision of the Kotz type of tumour endoprosthesis for the lower limb. J Bone Joint Surg Br. 2002;84:401–406.
Myers GJ, Abudu AT, Carter SR, Tillman RM, Grimer RJ. Endoprosthetic replacement of the distal femur for bone tumours: long-term results. J Bone Joint Surg Br. 2007;89:521–526.
Pedtke AC, Wustrack RL, Fang AS, Grimer RJ, O’Donnell RJ. Aseptic failure: how does the Compress® implant compare to cemented stems? Clin Orthop Relat Res. 2012;470:735–742.
Schwartz AJ, Kabo JM, Eilber FC, Eilber FR, Eckardt JJ. Cemented distal femoral endoprostheses for musculoskeletal tumor: improved survival of modular versus custom implants. Clin Orthop Relat Res. 2010;468:2198–2210.
Veth R, van Hoesel R, Pruszczynski M, Hoogenhout J, Schreuder B, Wobbes T. Limb salvage in musculoskeletal oncology. Lancet Oncol. 2003;4:343–350.
Wirganowicz PZ, Eckardt JJ, Dorey FJ, Eilber FR, Kabo JM. Etiology and results of tumor endoprosthesis revision surgery in 64 patients. Clin Orthop Relat Res. 1999;358:64–74.
Acknowledgments
We thank Susie Crabtree RN, our research coordinator, for her assistance with study approval and data collection.
Author information
Authors and Affiliations
Corresponding author
Additional information
Two of the authors certify that they (NMB, RLR), or a member of their immediate family, has or may receive payments or benefits, during the study period, an amount of less than USD 10,000 from Biomet (Warsaw, IN, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Primary Children’s Medical Center and the Huntsman Cancer Institute at the University of Utah, Salt Lake City, UT, USA.
About this article
Cite this article
Monument, M.J., Bernthal, N.M., Bowles, A.J. et al. What Are the 5-year Survivorship Outcomes of Compressive Endoprosthetic Osseointegration Fixation of the Femur?. Clin Orthop Relat Res 473, 883–890 (2015). https://doi.org/10.1007/s11999-014-3724-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-014-3724-5