Abstract
Background
Compressive osseointegration is a promising modality for limb salvage in distal femoral oncologic tumors. However, few studies have explored short-term survival rates in a large patient cohort of distal femur compressive endoprostheses or highlighted the risk factors for spindle failures.
Questions/purposes
We asked: (1) What is the frequency of compressive osseointegration spindle failure in distal femoral reconstructions? (2) What are the characteristics of rotational failure cases with distal femur compressive osseointegration endoprostheses? (3) What are the risk factors for mechanical and rotational failure of distal femur compressive osseointegration implantation? (4) What are other modalities of failure or causes of revision surgery, which affect patients undergoing distal femur compressive osseointegration implantation for oncologic reconstruction?
Methods
Between 1996 and 2013, 127 distal femoral reconstructions with the Compress® prosthesis were performed in 121 patients. During that time, 116 Compress® prostheses were implanted for aggressive primary tumors of the distal femur and/or failure of previous oncologic reconstruction. This approach represented approximately 91% of the distal femoral reconstructions performed during that time. Of the patients with prostheses implanted, four patients (four of 116, 3%) had died, and 37 (37 of 116, 32%) were lost to followup before 24 months. The median followup was 84 months (range, 24–198 months), and 71 patients (66% of all patients) were seen within the last 3 years. A retrospective chart review was performed to determine failure modality as defined by radiographs, clinical history, and intraoperative findings. Risk factors including age, sex, BMI, resection length, and perioperative chemotherapy were analyzed to determine effect on spindle and rotational failure rates. Survival analysis was determined using the Kaplan-Meier estimator. Differences in survival between groups were analyzed using the log rank test. Risk factors were determined using Cox proportional hazard modeling.
Results
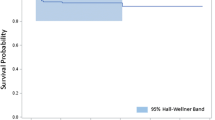
Spindle survival at 5 and 10 years was 91% (95% CI, 82%–95%). Survival rates from rotational failure at 5 and 10 years were 92% (95% CI, 83%–96%); the majority of failures occurred within the first 2 years postoperatively and were the result of a twisting mechanism of injury. With the numbers available, none of the potential risk factors examined were associated with mechanical failure. The 5-year and 10-year all-cause revision-free survival rates were 57% (95% CI, 44%–67%) and 50% (95% CI, 36%–61%), respectively.
Conclusions
Distal femur compressive osseointegration is a viable method for endoprosthetic reconstruction. Rotational failure is rare with the majority occurring early. No variables were found to correlate with increased risk of mechanical failure. More research is needed to evaluate methods of preventing mechanical and rotational failures in addition to other common causes of revision such as infection in these massive endoprosthetic reconstructions.
Level of Evidence
Level IV, therapeutic study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Owing to improvements in systemic treatment and operative techniques, limb salvage surgery is offered to nearly 85% of patients with lower extremity primary bone tumors [8]. Endoprosthetic reconstruction is an effective and mechanically stable method of distal femur reconstruction [17]. Despite initially successful limb salvage, failure rates of as much as 40% at 5 and 10 years have been reported resulting from aseptic loosening, infection, mechanical failure, and local recurrence [11, 15, 24]. With current long-term survival rates of 60% to 70% in patients with chemotherapy-sensitive tumors, device-related failure rates have become a substantial concern, compromising function and quality of life in long-term cancer survivors [6, 21].
The Compress® Compliant Pre-stress implant (Biomet Inc, Warsaw, IN, USA) was designed to limit long-term complications such as aseptic loosening by promoting osseointegration at the bone-prosthesis interface [3, 5, 16]. This is achieved by securing a titanium porous-coated spindle to the bone with 600 to 800 pounds of force through a spring-loaded device anchored to a short traction bar (Fig. 1). Variable intermediate-term outcomes have been reported for distal femur and proximal tibia implants [2, 11, 19, 20] with reported 5-year survival rates ranging from 25% to 85% [3, 5, 16]. However, few studies have focused exclusively on compressive osseointegration technology for distal femoral resections. Although unique instances of failure of compressive osseointegration implants have been documented [11, 25], the incidence of and predictors for rotational failure at the bone-spindle interface have not been reported, to our knowledge. The purpose of our study was to provide further characterization of the nature of compressive osseointegration spindle failure in distal femoral reconstruction for primary oncologic conditions by determining the rate of mechanical failure, and by identifying the risk factors for mechanical and rotational failure of compressive osseointegration implantation.
(A) A photograph of the Compress® Compliant Pre-stress implant preassembly shows the various components, including the anchor plug (a), spindle (b), taper adapter (c), and distal femur replacement (d). (B) This schematic shows the internal components of the spindle, including the Belleville washer apparatus. The spindle (fat arrow) can be preloaded with a force of 400, 600, or 800 pounds, distributed through the series of Belleville washers (asterisk). Postimplantation, this force is transferred to the bone-prosthesis interface to achieve compressive osseointegration. Antirotation pins can be inserted through dedicated angled pin holes into predrilled bone at the bone-prosthesis interface (skinny arrows). (Figure 1B is published with permission from Biomet Inc, Warsaw, IN, USA.).
Specifically, we asked: (1) What is the frequency of compressive osseointegration spindle failure in distal femoral reconstructions? (2) What are the characteristics of rotational failure cases in distal femur compressive osseointegration endoprostheses? (3) What are the risk factors for mechanical and rotational failure of distal femur compressive osseointegration implantation? (4) What are other modalities of failure which affect patients undergoing distal femur compressive osseointegration for oncologic reconstruction?
Patients and Methods
We retrospectively reviewed an institutional surgical database to identify all patients who had undergone implantation of a distal femoral Compress® prosthesis for oncologic reconstruction from March 1, 1996, through December 31, 2013. All cases were performed by one surgeon (RJO) at a tertiary care center. Patients who underwent distal femoral compressive osseointegration implantation for primary or revision oncologic indications were included. Those who had revision of a failed arthroplasty or traumatic indication were excluded. Patients were followed for at least 24 months or until implant removal; those with less than 24 months followup were excluded. Patients who have not been seen in the past 5 years were considered to be lost to followup, however data from the most recent visit were used in the analysis. Institutional review board approval was obtained.
During our defined study period, 127 distal femoral compressive osseointegration endoprostheses were implanted in 121 patients at our institution. During that time, 116 reconstructions using the Compress® prosthesis were performed for aggressive primary tumors of the distal femur and/or failure of previous oncologic reconstruction. This approach represented approximately 91% of the distal femoral reconstructions performed during that time. Of the patients who underwent reconstruction surgery for this indication, four (four of 116; 3%) had died, and 37 (37 of 116; 32%) were lost to followup before 24 months. Two patients experienced implant failure before 24 months followup, and were included in our study. Eleven patients were excluded because they had compressive osseointegration distal femoral replacement for revision arthroplasty or traumatic indications. One patient had an intercalary compressive osseointegration implant, which did not involve the distal-most aspect of the femur, and this patient was not included. Seventy-four patients (with a total of 79 compressive osseointegration endoprostheses implanted) met the inclusion criteria and were part of the study (Fig. 2). The most frequently-occurring tumor diagnoses in the study population included osteosarcoma and giant cell tumor or chondrosarcoma (Table 1).
During the period in question, our general indications for the use of this device were for oncologic reconstruction after resection of (1) a malignant bone tumor, (2) soft tissue malignancy with osseous involvement, or (3) a benign aggressive bone tumor of the distal femur. Distal femur compressive osseointegration also was performed during this time for patients who required revision of an oncologic reconstruction. Patients with diffuse metastatic disease (impending or complete pathologic fracture of the distal femur), poor host bone (including elderly patients with osteoporosis), and patients who could not tolerate a prolonged period of nonweightbearing, or patients who required radiation as part of local control were treated with a cemented stemmed distal femoral endoprosthesis. From 2000 to 2011, which comprised the majority of our study period, approximately 92% (93 of 101) of patients undergoing distal femoral reconstruction ultimately were offered a distal femur compressive osseointegration endoprosthesis in accordance with the above-mentioned criteria; a cemented stem was used in the remaining patients primarily if they were elderly, had poor bone quality or metastatic disease, or previously had received radiation therapy to the operative field.
The distal femoral compressive osseointegration surgical technique has been described [18]. Briefly, during tumor resection, an osteotomy was made perpendicular to the long axis of the femoral diaphysis. The cylindrical reamer was used to sequentially ream the canal to a size that would fit the smallest anchor plug (10 mm) and the appropriately sized centering sleeve that allowed good endosteal contact. Five smooth transverse pins measuring 4 mm longer than the bone diameter were inserted to secure the anchor plug using an outrigger device for placement. The conical reamer was used to prepare the osteotomy surface. A spindle was placed over the traction bar in the appropriate rotation and secured with a nut; most commonly, a large 800-pound force spindle was used (with the rare exception of for younger patients undergoing expandable compressive osseointegration implantation, or in patients with thin cortices, in which cases, per manufacturer recommendations, the lower-force spindles were considered). The modular distal femoral component coupled with a rotating hinge total knee replacement (the Orthopaedic Salvage System [OSS™], Biomet Inc) was impacted over the Compress® spindle. Antirotation pins, which typically are inserted at an oblique angle to secure the spindle to the bone interface, were rarely used owing to the concern that they could give rise to increased stress risers and impaired osseointegration (Fig. 1B).
Postoperatively, gentle ROM exercises and strengthening with active and active-assisted protocols were begun immediately after surgery. Chemotherapy was restarted 3 weeks after surgery unless there was concern for infection or wound healing; adjuvant radiation therapy (five patients) was started 6 weeks after surgery, and the bone-prosthetic interface was excluded, if possible. Patients were instructed to remain strictly nonweightbearing for 6 weeks and to avoid twisting movements at the knee. Knee immobilizers occasionally were used for 1 to 2 weeks postoperatively to allow soft tissue healing. Plain radiographs were obtained in the hospital before discharge and at 6 weeks postoperatively. If the plain radiographs showed no evidence of bone-implant loosening, partial weightbearing was advanced 25% per week thereafter, with the ultimate aim of having patients ambulatory without assistive devices by 3 months postoperatively. In our study population, 49% of patients (34 of 69) were able to walk without assistive devices by that time. By 3 months, patients generally were allowed to engage in recreational activities that avoided repetitive high-impact stress such as long-distance running or contact sports. Clinical examinations and plain films were performed at 3-month intervals through 2 years postoperatively and subsequently every 6 months thereafter. Radiographs were interpreted by the senior surgeon (RJO) at the time of evaluation to assess for completeness of osseointegration, defined as the appropriate degree of bony hypertrophy at the bone-prosthesis interface given the postoperative course.
The mean followup was 84 months (range, 24–198 months), and 71 patients (95% of the 75 patients in this study) were seen within the last 3 years. Three patients were followed until revision of their compressive osseointegration spindle, but there was no followup thereafter. These three patients were not reentered as having a “revision oncologic” procedure.
Medical records were reviewed to obtain information concerning followup, patient age, sex, BMI, perioperative chemotherapy and radiation, diagnosis, need for revision, indication for revision, time between first surgery and revision surgery, periprosthetic or wound infection, need for amputation, local recurrence, and death. The operative reports for each patient were reviewed to determine resection length, spindle size, anchor plug, and the amount of force used. All values for these categories were recorded for each patient. Patients who had revision with a new compressive osseointegration spindle were reentered into the database as “revision oncology” and followed from the time of revision until the date of last followup.
General causes of revision (mechanical: structural failure or aseptic loosening; and nonmechanical: infection, soft tissue failure, and tumor progression) were classified according to endoprosthesis failure modes previously described [12]. Structural failure was further subclassified according to type. Other subtypes of structural failure included failure of the compressive osseointegration spindle or failure external to the spindle. Spindle failure was defined as any internal malfunction of the spindle and/or spindle osseointegrative mechanism (ie, failure of the bone-prosthesis interface) which required subsequent spindle revision or removal. Rotational failure, a subcategory of spindle failure, was further defined as failure at the bone-prosthesis interface that occurred through a torque mechanism with radiographic and/or clinical evidence of rotational instability thereafter. Radiographic evidence of rotational failure (Fig. 3) was largely determined by failure of proper osseointegration in conjunction with observed discrepancy of the distal implant rotational profile with respect to the proximal implant, as assessed at the level of the anchor plug/bone-prosthesis interface. Failure mode was determined via historical review of the electronic medical records system, which included evaluation of clinical notes and radiographs (to determine failure mechanism, where appropriate) and operative reports for in vivo descriptions of failure mechanism (performed by the surgeon at the time of revision). For particularly ambiguous cases, the senior surgeon (RJO) served as a final arbiter to classify the precise failure modality; this was required for five patients (five of 79; 6%).
A radiograph obtained 1 month postoperatively shows (A) reasonable alignment and little osseointegration at the bone-prosthesis interface. The patient was a 17-year-old male who underwent distal femoral Compress® implantation for a distal femur osteosarcoma. Six-months postoperatively, the patient reported persistent thigh pain particularly during periods of activity. (B) A radiograph showed persistent failure of osseointegration at the bone-prosthesis interface (arrows), and rotational discrepancy of the profile of the implant (asterisk) compared with the patient’s postoperative radiograph. He underwent revision surgery and rotational failure was confirmed intraoperatively. (C) Eighteen months after revision surgery, the radiograph shows an appropriate degree of bone hypertrophy (arrows), indicating successful osseointegration.
Survival analysis was determined using the Kaplan-Meier log-rank technique [13]. Age at surgery, diagnosis, perioperative chemotherapy, BMI, sex, and resection length were entered into a Cox proportional hazards model as potential predictors of mechanical failure [10]. All statistical analyses were performed using Stata® software (STATACorp LP, College Station, TX, USA).
Results
Survival of the spindle at 5 and 10 years was 81% (95% CI, 70%–88%). However if spindle removal attributable to infection and amputation are excluded, the survival of the spindle was 91% (95% CI, 82%–95%) (Fig. 4). There were no spindle failures after 5 years. The mean time to spindle failure was 23 months (range, 7–59 months). Eleven patients had removal of the spindle during revision. Eight patients had documented failure at the bone-spindle interface. This included rotational failure (four), fracture of the traction bar (one), periprosthetic fracture (one), aseptic loosening (one), and loss of the spindle-anchor plug space (one). One patient had an infection that involved the bone-prosthesis interface requiring removal of the spindle and anchor plug. Two patients had osseointegration at the bone-prosthesis interface and required revision surgery for fractured taper adapters. In both patients, the taper between the spindle and the adapter had become cold-welded and could not be separated. This resulted in revision of the compressive osseointegration spindle to a more proximal level in the femur in one patient and conversion to a total femoral replacement in the other patient.
Survival rates from rotational failure at 5 and 10 years were 92% (95% CI, 83%–96%) (Fig. 5). Six patients experienced rotational failure, and four of these patients required revision of the compressive osseointegration spindle, whereas in two patients, the spindles had healed in a rotated position at the time of revision and required derotation of the distal segments only (Table 2). Rotational failure occurred at a mean of 10 months after the original surgery (range, 3–22 months). The mean age of patients with rotational failure was 18 years (range, 15–24 years). Four patients had a primary diagnosis of osteosarcoma. All patients were male, and all had received adjuvant chemotherapy treatment. One patient also had received adjuvant radiation. The mean resection length for these patients was 23 cm (range, 18–28 cm). Two patients experienced rotational failure while sitting in a “W” position and twisting while getting up from this position; one patient fell while at a party; one patient had a progressive radiolucent line at the bone-prosthesis interface and was noted to have rotational instability intraoperatively; one patient had clinical rotational instability with progressive pain since the time of surgery; one patient twisted his leg while throwing a football, after being noncompliant with the postoperative recommendation for restricted weightbearing; and one patient experienced symptoms while walking more than usual at a wedding. All were treated successfully with revision of the compressive osseointegration spindle, with a mean postrevision followup of 66 months (range, 15–130 months). In two patients, the spindles osseointegrated after rotational failure. These two patients initially presented with rotational instability after the index procedure. At the time of revision, the spindle was noted to have internally rotated at the bone-prosthesis interface compared with the original position, but there was stable osseointegration as confirmed by operative findings and torque assessment in vivo. The revision involved simply externally rotating the distal femur component, but the spindle was not revised.
Male sex was associated with rotational failure using the log rank test (p = 0.04). However, with the numbers available, none of the variables examined (age at surgery, perioperative chemotherapy, BMI, sex, resection length) was associated with mechanical failure when tested using the Cox proportional hazard model.
The Kaplan-Meier estimate (Fig. 6) shows that at 10 years’ followup, 50% (95% CI, 36%–61%) of patients can expect to undergo revision surgery. Thirty-six patients underwent revision surgery. The most common causes of revision included mechanical failure (n = 21) and infection (n = 10) (Table 3). Causes of mechanical failure included failure of the spindle (rotational failure, aseptic loosening of spindle, and nonrotational spindle failure; nine of 20; 45%), failure of the expansion apparatus (four of 20; 20%), failure or wear of the polyethylene liner or tibial tray (three of 20; 15%), periprosthetic fracture (two of 20; 10%), fracture of the taper adapter (two of 20; 10%), and rotatory failure of the distal modular components (one of 20; 5%). Nonmechanical failures were most commonly attributable to infection (n = 10) or soft tissue failure/arthrofibrosis (n = 4). One other patient required revision surgery owing to persistent knee pain. Males were more likely than females to require an unplanned surgery (hazard ratio, 3.4; 95% CI, 1.3, 8.8; p = 0.010).
Discussion
The Compress® endoprosthesis has become a widely-used implant for distal femoral reconstructions for oncologic conditions since it received FDA clearance in 2003. Since that time, several studies have investigated the relative success rates of compressive osseointegration technology, but these studies have been limited by small cohorts and limited followup [3, 5, 16, 17]. To our knowledge, our study is the largest single-surgeon series evaluating failure at the bone-spindle interface of the distal femur with the Compress® endoprosthesis for oncologic reconstructions. We found that distal femur compressive osseointegration reconstruction has reasonable short-term survival rates for rotational and mechanical spindle failures, and these remain comparatively less-common causes of revision, compared with infection or failure distal to the spindle, in this patient population. With the numbers available, no patient- or implant-specific factors were found to be predictive of mechanical failure.
This study has numerous limitations. Several kinds of biases might have had an effect on our conclusions, and these kinds of biases tend to inflate the apparent benefits of the investigated treatment. First, it is possible that selection bias played a role in our results. Although we have data to indicate that a large percentage of eligible patients were offered compressive osseointegration during the majority of our study period, the precise percentage is unclear (particularly during the early portion of the study period). Therefore it is possible that selection bias during the early part of our study period might cause an overestimation of the overall success of distal femoral compressive osseointegration for the indications described. Additionally, transfer bias or loss to followup may have contributed to limitations in this study. With nearly 29% of the total study population being lost to followup before 2 years, and an additional 5% not having had followup within the past 3 years, there is the possibility that our study might inflate the success rate of distal femoral compressive osseointegration, as this study describes best-case estimates of the success rates. Additionally, many of the cases predate the development of our medical center’s electronic medical record system, making data collection for certain demographic variables (eg, BMI) difficult. Second, despite our ability to access clinical documentation through a retrospective chart review, in some cases there was a certain degree of ambiguity regarding the true cause of implant failure. The surgeon (RJO) was consulted as the final arbiter of the proper failure classification for particularly ambiguous cases. Third, in our study only 68% of patients included had greater than 5 years of followup. This might have contributed to an underestimation of compressive osseointegration failure. Nevertheless, with a median followup of 84 months per patient, our study has a followup that is greater than or comparable to followups in other compressive osseointegration implant studies to date [11, 17, 20, 22]. For this reason, we believe that our study gives a more accurate representation of the true failure rate of this specific device.
Our study showed that the distal femoral compressive osseointegration spindle has an overall retention rate of 91% at 10 years. To our knowledge, this is the first study to date which focuses specifically on spindle failure of distal femoral compressive osseointegration implants for primary oncologic reconstructions and revision oncologic reconstructions. Our results are similar to those of Zimel et al. [25], who reported a 10-year cumulative incidence of mechanical failure (defined as failure at the bone-spindle interface) of 11%. However, their study focused only on revision oncologic procedures. We included patients undergoing index distal femur replacements and therefore many of our patients received adjuvant chemotherapy, which could inhibit bone healing. Despite this, our results are similar. Other studies have elaborated on the role that mechanical failures play in limiting the use of proximal or distal femur compressive osseointegration [11, 17]. Monument et al. [17] described loosening of the spindle resulting from a failed traction bar, without directly referring to failure of the spindle. Another series investigating survival for distal femoral compressive osseointegration described predominantly bone-dependent modalities of failure (ie, periprosthetic fractures, aseptic loosening, and osteonecrosis of the underlying bone at the prosthesis interface); however, it did not specifically make reference to mechanical failure of the spindle [11]. In this respect, our study provides important insight into the concept of internal failure of the compressive osseointegration spindle, which provides biomechanical stability to the implant and ultimately is the driving force behind implant osseointegration. We showed that, while these failures do occur and spindle revision is not an unknown phenomenon, these events are uncommon and the overall survival rate from spindle failure is quite high even at long-term followup.
As the first study, to our knowledge, of distal femoral compressive osseointegration that specifically addresses rotational failure as a cause of compressive osseointegration implant failure, we noted that 10-year survival from rotational failure was relatively high at 92%. Other studies have investigated the rotational stability of this particular implant from a biomechanical standpoint. Avedian et al. [1] investigated the use of antirotation pins for a compressive osseointegration implant in a cadaver model and reported that maximum torque to failure was found in the group with three antirotation pins. Most rotational failures in our study occurred secondary to a twisting mechanism of injury, and antirotation pins were not routinely used owing to the theoretical risk of increased stress risers at the bone-prosthesis interface and impaired osseointegration through additional damage to the adjacent periosteum. A future study to ascertain the effect of antirotation pins on rotational failure would require 714 patients in each group to detect a change in rotational failure from 6% to 3%. The average time to failure for this mode was relatively early, occurring on average 10 months after the index procedure. This is expected, since we hypothesized that patients would be at greater risk of rotational failure during the early stage of osseointegration when bone ongrowth may be incomplete. Additionally, in our study, all patients who experienced rotational failure were able to undergo revision surgery and did not undergo a second revision surgery after an average followup of 66 months. This is consistent with a previous study that showed the relative reliability of revision of compressive osseointegration endoprostheses compared with traditional long-stemmed implants owing to their short intramedullary components [15].
We also wanted to investigate patient characteristics that might contribute to higher risk of implant failure, but with the data and numbers available, we were unable to draw firm conclusions. Resection length has been shown to be a risk factor for endoprosthetic failure in previous studies. In 1998, Kawai et al. [14] reported resection of 40% of the femur to be a risk factor for failure of conventional stemmed distal femoral endoprostheses. Guo et al. [9] also reported an increased failure rate of cemented prostheses with resection greater than 14 cm. However, a more recent compressive osseointegration study by Calvert et al. [4], which was not specific to distal femur endoprostheses, failed to show correlation between resection length and failure risk. A larger resection length causes a larger lever arm and stress across the bone-prosthesis interface, theoretically predisposing patients to higher torque, especially when subject to rotational stresses. However, given the low numbers of rotational failure in our patients, we did not find an association between resection length and rotational failure.
Our study showed the relatively high survival rate of compressive osseointegration implants compared with other limb-salvage modalities. We sought to better understand revisions using the largest distal femoral compressive osseointegration database to date. Aseptic loosening, which historically has been the highest cause of failure for cemented endoprostheses [23], comprised a small portion (two of 36; 6%) of all failures in our study. Previous studies showed rates of aseptic failure of femoral compressive osseointegration implants ranging from 0% to 12% [1, 7]. In 2013, Healey et al. [11] reported survivorship of 85% at 5 years and 80% at 10 years for compressive osseointegration implants about the knee. A multicenter study by Calvert et al. [4] showed that the success rate of compressive osseointegration implants was similarly not confined to the distal femur. They reported a revision rate of approximately 30% after an average 66-month followup and did not find any patient-specific factors to be associated with revision [4]. In our study, the proportion of revisions attributable to mechanical causes (approximately 54%) is higher than that reported by Monument et al. [17]. However, their study involved only 18 patients, and for this reason, we believe that our results might be more generalizable. Moreover, nearly 50% of patients in our study remained revision-free after 10 years. Our results thus confirm those of previous studies; however future studies are needed focusing on other common causes of compressive osseointegration failure such as infection and failure distal to the compressive osseointegration spindle, which limit revision-free survival.
Despite high rates of osseointegration and spindle retention, 50% of patients required some form of revision surgery or unplanned operations at 10 years. Although revision of the polyethylene liner, a fractured expandable apparatus, or an open lysis of adhesions are relatively smaller procedures than revision of the spindle and anchor plug, they are setbacks to the patient, and ultimately place patients at increased risk of deep infection. Patients should be counseled regarding the high likelihood of future procedures when given the option for this implant.
Distal femoral compressive osseointegration is a relatively reliable form of endoprosthetic reconstruction in lower extremity tumors. Our study showed reasonable overall 5- and 10-year survival rates of distal femoral compressive osseointegration implants in terms of spindle failure and rotational failure. However, certain limitations of this study including the shorter followups in some patients and the loss to followup may call into question the degree of success afforded by this treatment option. As is true for all massive endoprostheses, the all-cause 10-year revision rate of distal femoral compressive osseointegration endoprostheses is substantial, suggesting that more research and multicenter studies are needed to elucidate the risk factors influencing other more common causes of revision, including infection and distal implant failure.
References
Avedian RS, Goldsby RE, Kramer MJ, O’Donnell RJ. Effect of chemotherapy on initial compressive osseointegration of tumor endoprostheses. Clin Orthop Relat Res. 2007;459:48–53.
Bhangu AA, Kramer MJ, Grimer RJ, O’Donnell RJ. Early distal femoral endoprosthetic survival: cemented stems versus the Compress® implant. Int Orthop. 2006;30:465–472.
Bini SA, Johnston JO, Martin DL. Compliant prestress fixation in tumor prostheses: interface retrieval data. Orthopedics. 2000:707–711; discussion 711–712.
Calvert GT, Cummings JE, Bowles AJ, Jones KB, Wurtz LD, Randall RL. A dual-center review of compressive osseointegration for fixation of massive endoprosthetics: 2- to 9-year followup. Clin Orthop Relat Res. 2014;472:822–829.
Cristofolini L, Bini SA, Toni A. In vitro testing of a novel limb salvage prosthesis for the distal femur. Clin Biomech (Bristol, Avon). 1998;13:608–615.
Eilber FR, Eckhardt J, Morton DL. Advances in the treatment of sarcomas of the extremity: current status of limb salvage. Cancer. 1984;54(11 suppl):2695–2701.
Farfalli GL, Boland PJ, Morris CD, Athanasian EA, Healey JH. Early equivalence of uncemented press-fit and Compress® femoral fixation. Clin Orthop Relat Res. 2009;467:2792–2799.
Grimer RJ, Carter SR, Pynsent PB. The cost-effectiveness of limb salvage for bone tumours. J Bone Joint Surg Br. 1997;79:558–561.
Guo W, Ji T, Yang R, Tang X, Yang Y. Endoprosthetic replacement for primary tumours around the knee: experience from Peking University. J Bone Joint Surg Br. 2008;90:1084–1089.
Harrell FE Jr, Lee KL, Pollock BG. Regression models in clinical studies: determining relationships between predictors and response. J Natl Cancer Inst. 1988;80:1198–1202.
Healey JH, Morris CD, Athanasian EA, Boland BJ. Compress® knee arthroplasty has 80% 10-year survivorship and novel forms of bone failure. Clin Orthop Relat Res. 2013;471:774–783.
Henderson ER, Groundland JS, Pala E, Dennis JA, Wooten R, Cheong D, Windhager R, Kotz RI, Mercuri M, Funovics PT, Hornicek FJ, Temple HT, Ruggieri P, Letson GD. Failure mode classification for tumor endoprostheses: retrospective review of five institutions and a literature review. J Bone Joint Surg Am. 2011;93:418–429.
Kaplan EL, Meier P. Nonparametric observations from incomplete observations. J Am Stat Assoc. 1958;53:457–481.
Kawai A, Muschler GF, Lane JM, Otis JC, Healey JH. Prosthetic knee replacement after resection of a malignant tumor of the distal part of the femur: medium to long-term results. J Bone Joint Surg Am. 1998;80:636–647.
Kinkel S, Lehner B, Kleinhans JA, Jakubowitz E, Ewerbeck V, Heisel C. Medium to long-term results after reconstruction of bone defects at the knee with tumor endoprostheses. J Surg Oncol. 2010;101:166–169.
Kramer MJ, Tanner BJ, Horval AE, O’Donnell RJ. Compressive osseointegration promotes viable bone at the endoprosthetic interface: retrieval study of Compress® implants. Int Orthop. 2008;32:567–571.
Monument MJ, Bernthal NM, Bowles AJ, Jones KB, Randall RL. What are the 5-year survivorship outcomes of compressive endoprosthetic osseointegration fixation of the femur? Clin Orthop Relat Res. 2015;473:883–890.
O’Donnell RJ. Compressive osseointegration of modular endoprostheses. Curr Opin Orthop. 2007;18:590–603.
O’Donnell RJ. Compressive osseointegration of tibial implants in primary cancer reconstruction. Clin Orthop Relat Res. 2009;467:2807–2812.
Pedtke AC, Wustrack RL, Fang AS, Grimer RJ, O’Donnell RJ. Aseptic failure: how does the Compress® implant compare to cemented stems? Clin Orthop Relat Res. 2012;470:735–742.
Sluga M, Windhager R, Lang S, Heinzl H, Bielack S, Kotz R. Local and systemic control after ablative and limb sparing surgery in patients with osteosarcoma. Clin Orthop Relat Res. 1999;358:120–127.
Tyler WK, Healey JH, Morris CD, Boland PJ, O’Donnell RJ. Compress® periprosthetic fractures: interface stability and ease of revision. Clin Orthop Relat Res. 2009;467:2800–2806.
Unwin PS, Cannon SR, Grimer RJ, Kemp HB, Sneath RS, Walker PS. Aseptic loosening in cemented custom-made prosthetic replacements for bone tumours of the lower limb. J Bone Joint Surg Br. 1996;78:5–13.
Unwin PS, Cobb JP, Walker PS. Distal femoral arthroplasty using custom-made prostheses: the first 218 cases. J Arthroplasty. 1993;8:259–268.
Zimel MN, Farfalli GL, Zindman AM, Riedel ER, Morris CD, Boland PJ, Healey JH. Revision distal femoral arthroplasty with the Compress® prosthesis has a low rate of mechanical failure at 10 years. Clin Orthop Relat Res. 2016;474:528–536.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the University of California, San Francisco, San Francisco, CA, USA.
About this article
Cite this article
Goldman, L.H., Morse, L.J., O’Donnell, R.J. et al. How Often Does Spindle Failure Occur in Compressive Osseointegration Endoprostheses for Oncologic Reconstruction?. Clin Orthop Relat Res 474, 1714–1723 (2016). https://doi.org/10.1007/s11999-016-4839-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-016-4839-7