Abstract
Background
Osteoporotic acetabular fractures in the elderly are becoming more common. Regardless of treatment, most patients are managed with a period of protected weightbearing, even if a THA has been performed. We have tried to treat these patients analogously to geriatric femoral neck fractures in a way that allows immediate full weightbearing.
Questions/purposes
We determined return to mobility, length of hospital stay (LOS), radiographic outcomes, and complications in a series of elderly osteoporotic patients treated for acetabular fractures with early fracture fixation and simultaneous THA, allowing full weightbearing immediately postoperatively.
Methods
Since 2009, one surgeon (MR) used a consistent approach for fracture fixation and THA with immediate weightbearing in all patients older than 65 years with acetabular fractures who were fit for surgery and whose injuries were deemed osteoporotic fractures (low-energy mechanisms) meeting particular radiographic criteria (significant marginal impaction or femoral head damage). Twenty-four patients met these criteria and were reviewed at a mean of 24 months (range, 8–38 months). Mean age was 77 years (range, 63–90 years), and eight patients were women. The surgical technique included plate stabilization of both acetabular columns plus simultaneous THA using a tantalum socket and a cemented femoral stem. Clinical and note reviews were conducted to ascertain return to mobility, LOS, and postoperative complications. Component migration and fracture healing were assessed on plain radiographs.
Results
All patients mobilized with full weightbearing by Day 7 postoperatively. Only one patient remained dependent on a frame to mobilize at discharge. At 6 weeks, two patients already required no walking aids. At 6 months, patients were using a single stick at home at most, and all patients had managed stairs. Mean LOS was 18 days (range, 10–36 days). Radiographically, no component migration was seen in any patient. Seventeen of 24 fractures (71%) healed radiographically by 12 weeks, and all healed by 6 months. We recorded one superficial wound infection, one symptomatic deep venous thrombosis, and one in-hospital death from myocardial infarction.
Conclusions
Selected older patients with acetabular fractures may be managed using immediate weightbearing after fracture fixation and THA. However, this surgery is complex and requires a mixed skill set.
Level of Evidence
Level IV, therapeutic study. See Instructions for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is an increasing problem in the United Kingdom and across the developed world [29]. With the population living longer and activity levels rising, osteoporotic fractures are being seen with increasing frequency [14, 15]. Those most commonly seen include proximal femur fractures, distal radius fractures, and compression vertebral fractures, all of which have well-established pathways of management [7, 29]. Worldwide, an estimated 1.66 million hip fractures occurred in 1990; this figure is estimated to rise to 6.3 million by 2050 [7]. In 1999, Mears [24] predicted similarly that by 2010 geriatric patients may represent the largest group of acetabular fractures.
The results of fracture fixation for osteoporotic acetabular fractures are known to be poorer than in the younger patient group [9, 26]. As a result of this, traditional management strategies for osteoporotic acetabular fractures in elderly patients have been either to enforce bed rest until fracture healing, with or without traction, or to ignore the fracture and allow mobilization as pain allows. Both of these methods involve significant delays to mobilization, and in either case, if the patient survives and has hip pain, a THA often is carried out electively at a later date. Other options have been reported, including early fixation and delayed arthroplasty or acute arthroplasty [1, 2, 13, 16, 21, 25, 31, 35], but we are not aware of any series of such patients where initial management has allowed immediate full weightbearing.
This study of a series of elderly osteoporotic patients treated for acetabular fractures with early fracture fixation and simultaneous THA is unique in that it allowed full weightbearing immediately postoperatively. We report outcomes in this patient series, including (1) return to mobility, (2) length of hospital stay (LOS), (3) radiographic outcomes (component migration, fracture healing), and (4) complications.
Patients and Methods
The initial diagnosis of an acetabular fracture was made using a plain AP radiograph in the emergency department, but all patients subsequently underwent CT scanning to identify the extent of the fracture and surrounding impaction. Based on the CT scan and routine clinical information, patients were considered for THA if all of the following criteria were met: (1) patient older than 65 years or older than 60 years with an American Society of Anesthesiologists (ASA) grade of 3 or more; (2) osteoporotic fracture, as identified by a low-energy injury (eg, simple trip or fall from standing height; (3) significant marginal impaction or significant femoral head damage; and (4) patient considered medically fit enough to undergo surgery.
Between October 2009 and December 2012, 48 patients underwent fixation and a simultaneous THA at our unit. The senior author (MR) directly performed 34 operations, of which the first 24 are reported on here. This represented 56% (48 of 86) of the patients with isolated acetabular fractures who were older than 65 years and were treated by our surgical unit during the study period. Routine fixation was employed in cases of simple fracture patterns, with no marginal impaction, in a previously mobile patient who could tolerate a period of mobility using crutches. Fourteen similar operations were done by other specialist pelvic and acetabular trauma surgeons at the same hospital but are not included in this report, as different surgical techniques and postoperative regimes were employed. The mean age for the 24 patients was 77 years (range, 63–90 years), and eight patients were women (Table 1). Three patients had secondary injuries (one ankle fracture, one clavicle fracture, and one elbow fracture). The mean time from fall to surgery was 10 days (range, 1–26 days). One patient died while in the hospital. Minimum followup for the remaining patients was 8 months (mean, 24 months; range, 8–38 months). All 24 patients had complete followup at that interval, other than the one patient who died in the hospital shortly after surgery.
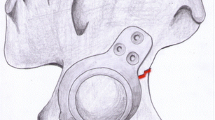
Patients were assessed jointly by surgical and anesthetic teams before consent being taken. All patients underwent balanced general anesthesia, with controlled ventilation via an endotracheal tube with local anesthesia supplementation. All operations were carried out in a single sitting (Table 1). The surgical technique has been reported on in detail previously and was similar in all 24 patients [30]. In all but four patients, the anterior column was stabilized initially through a modified Stoppa approach [6, 33] (Fig. 1) before the posterior column was stabilized (19 of the 24 cases) and a THA was performed through a Kocher-Langenbeck approach. Occasionally, the outer window of the ilioinguinal approach in conjunction with the Stoppa approach was utilized (Fig. 2). Although some attempt was made during surgery to achieve fracture reduction, anatomic reduction of either column was not sought; however, good bone contact was ensured in all patients.
For all patients, a cemented Exeter™ stem (Stryker Orthopaedics, Mahwah, NJ, USA) and a Trabecular Metal™ revision modular shell (Zimmer, Inc, Warsaw, IN, USA) were used. The shell was impacted in whatever position achieved maximal stability of the implant, generally wherever maximum bone coverage was possible. The liner was then cemented into the acetabular shell aiming for 35° to 15° of inclination and 10° to 15° of anteversion. The overall concept is that of creating an A-frame equivalent, by stabilizing both anterior and posterior columns, followed by using the acetabular shell as the cross-piece (Fig. 3). A minimum of two screws was therefore used in every shell and, in most cases, three or four where possible, to add further stability (Fig. 1). In one patient, there was an uncontained defect at the superomedial aspect adjacent to the sciatic notch, and a Trabecular Metal™ augment was used to bridge this defect (Fig. 4).
The mean total operating time was 193 minutes (range, 130–280 minutes), which included the changeover time between approaches, and the mean total blood loss was 1100 mL (range, 500–2500 mL) (Table 1). The only intraoperative complication was a minor greater trochanteric fracture that was wired and went on to heal uneventfully.
For patients with an ASA grade of 3 or 4, postoperative care was delivered in an intensive care or high dependency unit (HDU) where possible for the first 24 to 48 hours. In addition, patients with an ASA grade of 1 or 2 with significant blood loss and replacement were observed for 24 hours in the HDU. Postoperative management included allowing full weightbearing as soon as possible for all patients. All patients were medicated with warfarin for 3 months as thromboprophylaxis, and followup after discharge was in a specialist pelvic and acetabular clinic.
We recorded return to mobility (in-hospital and postdischarge), LOS, and postoperative complications. Component migration and fracture healing were assessed on plain radiographs radiographs at 6 weeks, 12 weeks, 6 months, 1 year, and annually thereafter.
Results
All patients mobilized fully weightbearing by Day 7 after surgery. Only one patient remained dependent on a frame to mobilize at discharge, and at 6 weeks, two patients already required no walking aids. At 6 months, even the frailest patients (Patients 2 and 15) were mobile with no more than a single stick at home, and all patients had managed stairs.
The mean LOS of these patients was 18 days (range, 10–36 days). All 23 patients who left the hospital returned eventually to their preinjury residential status and had done so by 12 weeks after injury.
Radiographically, no component migration was seen in any patient. Seventeen of 24 fractures (71%) were seen to be healed radiographically by 12 weeks, and all were judged to be healed by 6 months.
Two postoperative complications were seen. One patient (Patient 13) had a slowly healing posterior wound, which was treated as a superficial infection. On Day 14, the patient returned to surgery for a wound irrigation, and the wound subsequently healed uneventfully. Microbiology samples were negative throughout, but it was assumed that this was a superficial wound infection. This was the only reoperation in the series. The other patient with a complication (Patient 19) experienced a symptomatic deep venous thrombosis on Day 3 after surgery, which was treated with warfarin for 6 months. There was one perioperative death. Patient 8, a 74-year-old female patient, was operated on 11 days after a fall from a standing height and died on Postoperative Day 8 of cardiac failure secondary to a myocardial infarct; she had a history of severe coronary artery disease. There were no dislocations, nerve palsies, or deep infections. Since leaving hospital, two patients died within 1 year of surgery from unrelated causes. Thus, at 1 year, three of the 21 patients (with 1-year followup) had died, giving an all-cause mortality of 14%.
Discussion
The annual associated cost of osteoporosis in Europe has been estimated at EUR 30 billion [8]. With life expectancies rising and activity levels increasing, the combined effect is a rise in the number of osteoporotic fractures. Among the most difficult of these are elderly osteoporotic acetabular fractures. Surgical fixation has now become common for displaced acetabular fractures, and results have steadily improved [5, 17–19, 23]. A regular finding however has been poorer results from fixation of acetabular fractures in the elderly [19, 20, 22]. Explanations for this are largely based on poor bone quality. Even low-energy injuries cause crushing of osteoporotic bone and subcortical impaction (Fig. 5), making anatomic reduction impossible; however, long-term outcome for acetabular fractures is directly related to accuracy of reduction [22]. In addition, most surgeons employ restricted weightbearing for 6 to 12 weeks after acetabular fracture surgery, something that elderly patients are often not able to adhere to, resulting in secondary loss of fracture reduction. There is little in the literature suggesting good outcomes with fixation of the elderly acetabular fracture [2, 11, 13, 31, 35]. We therefore evaluated a treatment algorithm that involved fracture fixation plus THA and immediate weightbearing in selected older patients with acetabular fractures. Specifically, we were interested in postoperative mobilization, LOS, radiographic results, and complications associated with this technique.
This study had a number of limitations. First, we did not undertake formal hip function outcome scores or validated satisfaction questionnaires. This is justified by the fact that this type of injury in this age group presents the same problems as patients with proximal femur fractures; thus, sensible outcome measures are surgical complications, mortality rates, time in hospital, and return to function. It is notable however that, despite the extent of surgery employed, based on these outcome measures our results are similar or better than those expected from patients with proximal femur fractures. Further limitations are that our followup period is relatively short, and fracture healing and component migration were only assessed on standardized AP radiographs. However, all fractures were seen to be fully healed and therefore no component migration would be expected after this point, and function levels should only improve with time. It is possible however that over time other complications could occur, such as dislocations or late component loosening. Within the time period, not all patients admitted were treated using this method; some were treated nonoperatively and some received more standard surgical fixation. Our results therefore are from a select group of patients and not necessarily applicable to the entire group. However, we believe that the patients included in this paper have the more complex injuries and are patients who are unlikely to manage with nonweightbearing regimes but are still medically fit enough for surgery. This should represent the most challenging subgroup of elderly patients with this type of injury.
We found that patients meeting our criteria for fracture fixation, immediate THA, and immediate full weightbearing indeed mobilized quickly, with all patients achieving full weightbearing mobility by the time of hospital discharge, although most used some form of aids. We are not aware of any large series in the literature where acetabular fractures have been managed surgically, employing early full weightbearing, with the exception of cases where the original fracture was a simple posterior pattern. Helfet et al. [11] managed their patients with conventional fixation, followed by a period of toe touch weightbearing, and Mears [24], despite using primary arthroplasty, also protected weightbearing for 6 weeks. In this select group of patients, we believe that early weightbearing should be a key part of the management strategy, for both patient- and hospital-related reasons. Nonoperative management necessitates protected weightbearing until fracture union has occurred, and long-term functional results in this group have been shown to be poor in many cases [32]. It is some years since elderly patients with neck of femur fractures were managed with bed rest or surgery that did not allow immediate full weightbearing, and current evidence-based guidelines in the United Kingdom are based on the principles of early full weightbearing for this group to maximize outcomes [28].
Mean LOS in this series was 18 days (range, 10–36 days). All 23 patients who left the hospital returned eventually to their preinjury residential status and had done so by 12 weeks after injury. It is difficult to establish whether all patients went directly home from hospital or via a care home or rehabilitation unit, as the final destination is only known from the 12-week followup appointment. This is because many patients left our institution after 5 to 7 days to return to a referring hospital and were discharged home from there. Although 18 days is considerable, it should be noted that some patients were referred from other units and may not have arrived until Day 5 to 7, and furthermore, availability of operating slots was limited to one to two per week and thus may have induced a small delay from diagnosis to treatment.
While it will be important to follow these patients over a longer period, and also to follow more patients using this approach, our initial radiographic results were encouraging, with no implant migration or loosening and no nonunions. All patients were followed radiographically until fracture union, and component migration would not be expected after this point. The initial stability of Trabecular Metal™ appears to be excellent, and in revision hip surgery, it has been shown to osseointegrate exceedingly well [3, 10, 34, 36]. The combination of the biologic behavior of tantalum and the mechanical stability of our A construct appears to have resulted in stability of the shell. Other published series have shown up to a few millimeters of displacement [24, 27], but there are no published series where Trabecular Metal™ has been used.
Despite the patients in this series being nearly 80 years old on average, there were relatively few complications and only one postsurgical death. One patient (5%) with a slowly healing posterior wound was treated as a superficial infection and returned to surgery at Day 14 for a wound irrigation. The wound subsequently healed uneventfully and microbiology samples were negative throughout. One symptomatic deep venous thrombosis (5%) was diagnosed on Day 3 after surgery and was treated with warfarin for 6 months. There was one death postoperatively (5%) on Day 8 due to cardiac failure secondary to a myocardial infarct. There were no dislocations, nerve palsies, or deep infections (0%). Since leaving the hospital, two patients died within 1 year of surgery from unrelated causes. Thus, at 1 year, three of the 21 patients (with 1-year followup) had died, giving an all-cause mortality of 14%. These complication rates compare favorably with other published series treating elderly acetabular fractures. Helfet et al. [11] treated 18 patients with fixation alone and had a complication rate of two pulmonary emboli (11%), one intraoperative fracture (6%), one retained fragment (6%), one loss of reduction (6%), one rapid progression to osteoarthrosis (6%), and one gastrointestinal bleed (6%). Matta’s [22] series of fixations of elderly acetabular fractures saw a rapid postoperative arthrosis rate of 5%. Mears [24] series of 57 patients undergoing arthroplasty alone showed an almost 100% rate of subsidence, with three revisions including two for dislocations (4%), with no infections. Boraiah et al. [4] treated 18 patients in a fashion similar to that in our series, with simultaneous fixation and replacement. Their series had one dislocation needing revision (6%) and one infection (6%). Herscovici et al. [12] had a similar series of 22 patients with five revisions for osteolysis or dislocation (23%) and one wound dehiscence (10%). Their series had a 59% overall complication rate.
In conclusion, osteoporotic acetabular fractures in the elderly are a difficult group of injuries, and there is never going to be a single best way to treat all patients. Surgical fracture fixation alone can yield poor results in certain patents, and nonoperative management is not ideal either. Using a combination of acetabular fracture techniques and modern hip arthroplasty technology, it is possible to manage some of these patients allowing immediate full weightbearing with few complications. However, careful patient selection is required, as well as thorough preoperative planning and surgical skills that include expertise both in acetabular fracture surgery and complex hip arthroplasty. This raises some issues regarding surgical skills, and in some units, it may be necessary to consider a joint procedure with two surgeons. We strongly recommend a combined preoperative workup with an intensive care physician/anesthetist, perioperative high dependency care, and close physiotherapy monitoring for several days postoperatively. Joint management with an orthogeriatrician likewise is important.
References
Beaule PE, Griffin DB, Matta JM. The Levine anterior approach for total hip replacement as the treatment for an acute acetabular fracture. J Orthop Trauma. 2004;18:623–629.
Bellabarba C, Berger RA, Bentley CD, Quigley LR, Jacobs JJ, Rosenberg AG, Sheinkop MB, Galante JO. Cementless acetabular reconstruction after acetabular fracture. J Bone Joint Surg Am. 2001;83:868–876.
Black J. Biological performance of tantalum. Clin Mater. 1994;16:167–173.
Boraiah S, Ragsdale M, Achor T, Zelicof S, Asprinio DE. Open reduction internal fixation and primary total hip arthroplasty of selected acetabular fractures. J Orthop Trauma. 2009;23:243–248.
Briffa N, Pearce R, Hill AM, Bircher M. Outcomes of acetabular fracture fixation with ten years’ follow-up. J Bone Joint Surg Br. 2011;93:229–236.
Cole JD, Bolhofner BR. Acetabular fracture fixation via a modified Stoppa limited intrapelvic approach: description of operative technique and preliminary treatment results. Clin Orthop Relat Res. 1994;305:112–123.
Cooper C, Campion G, Melton LJ 3rd. Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992;2:285–289.
Cooper C, Cole ZA, Holroyd CR, Earl SC, Harvey NC, Dennison EM, Melton LJ, Cummings SR, Kanis JA. Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos Int. 2011;22:1277–1288.
Ferguson TA, Patel R, Bhandari M, Matta JM. Fractures of the acetabulum in patients aged 60 years and older: an epidemiological and radiological study. J Bone Joint Surg Br. 2010;92:250–257.
Flecher X, Sporer S, Paprosky W. Management of severe bone loss in acetabular revision using a trabecular metal shell. J Arthroplasty. 2008;23:949–955.
Helfet DL, Borrelli J Jr, DiPasquale T, Sanders R. Stabilization of acetabular fractures in elderly patients. J Bone Joint Surg Am. 1992;74:753–765.
Herscovici D Jr, Lindvall E, Bolhofner B, Scaduto JM. The combined hip procedure: open reduction internal fixation combined with total hip arthroplasty for the management of acetabular fractures in the elderly. J Orthop Trauma. 2010;24:291–296.
Jimenez ML, Tile M, Schenk RS. Total hip replacement after acetabular fracture. Orthop Clin North Am. 1997;28-3:435–446.
Johnell O, Kanis JA. An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos Int. 2004;15:897–902.
Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17:1726–1733.
Joly JM, Mears DC. The role of total hip arthroplasty in acetabular fracture management. Oper Tech Orthop. 1993;3:80–102.
Judet R, Judet J, Letournel E. Fractures of the acetabulum: classification and surgical approaches for open reduction. Preliminary report. J Bone Joint Surg Am. 1964;46:1615–1646.
Letournel E. The treatment of acetabular fractures through the ilioinguinal approach. Clin Orthop Relat Res. 1993;292:62–76.
Letournel E, Judet R. Fractures of the Acetabulum. 2nd ed. Berlin, Germany: Springer-Verlag; 1993.
Liebergall M, Mosheiff R, Low J, Goldvirt M, Matan Y, Segal D. Acetabular fractures: clinical outcome of surgical treatment. Clin Orthop Relat Res. 1999;366:205–216.
Malkin C, Tauber C. Total hip arthroplasty and acetabular bone grafting for unreduced fracture-dislocation of the hip. Clin Orthop Relat Res. 1985;201:57–59.
Matta JM. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am. 1996;78:1632–1645.
Mayo KA. Open reduction and internal fixation of fractures of the acetabulum: results in 163 fractures. Clin Orthop Relat Res. 1994;305:31–37.
Mears DC. Surgical treatment of acetabular fractures in elderly patients with osteoporotic bone. J Am Acad Orthop Surg. 1999;7:128–141.
Mears DC, Velyvis JH. Acute total hip arthroplasty for selected displaced acetabular fractures: two to twelve-year results. J Bone Joint Surg Am. 2002;84:1–9.
Mears DC, Velyvis JH, Chang CP. Displaced acetabular fractures managed operatively: indicators of outcome. Clin Orthop Relat Res. 2003;407:173–186.
Mouhsine E, Garofalo R, Borens O, Blanc CH, Wettstein M, Leyvraz PF. Cable fixation and early total hip arthroplasty in the treatment of acetabular fractures in elderly patients. J Arthroplasty. 2004;19:344–348.
National Institute for Health and Clinical Excellence. The Management of Hip Fractures in Adults. CG124. London, UK: National Institute for Health and Clinical Excellence; 2011.
National Institute for Health and Care Excellence. Osteoporosis: Assessing the Risk of Fragility Fracture. CG146. London, UK: National Institute for Health and Care Excellence; 2012.
Rickman M, Young J, Bircher M, Pearce R, Hamilton M. The management of complex acetabular fractures in the elderly with fracture fixation and primary total hip replacement. Eur J Trauma Emerg Surg. 2012;38:511–516.
Romness DW, Lewallen DG. Total hip arthroplasty after fracture of the acetabulum: long-term results. J Bone Joint Surg Br. 1990;72:761–764.
Spencer RF. Acetabular fractures in older patients. J Bone Joint Surg Br. 1989;71:774–776.
Stoppa RE, Rives JL, Warlaumont CR, Palot JP, Verhaeghe PJ, Delattre JF. The use of Dacron in the repair of hernias of the groin. Surg Clin North Am. 1984;64:269–285.
Van Kleunen JP, Lee GC, Lementowski PW, Nelson CL, Garino JP. Acetabular revisions using trabecular metal cups and augments. J Arthroplasty. 2009;24(6 suppl):64–68.
Weber M, Berry DJ, Harmsen WS. Total hip arthroplasty after operative treatment of an acetabular fracture. J Bone Joint Surg Am. 1998;80:1295–1305.
Weeden SH, Schmidt RH. The use of tantalum porous metal implants for Paprosky 3A and 3B defects. J Arthroplasty. 2007;22(6 suppl 2):151–155.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
About this article
Cite this article
Rickman, M., Young, J., Trompeter, A. et al. Managing Acetabular Fractures in the Elderly With Fixation and Primary Arthroplasty: Aiming for Early Weightbearing. Clin Orthop Relat Res 472, 3375–3382 (2014). https://doi.org/10.1007/s11999-014-3467-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-014-3467-3