Abstract
Background
Unloading knee braces often are used after tibiofemoral articular cartilage repair. However, the experimental basis for their use in patients with normal tibiofemoral alignment such as those undergoing cartilage repair is lacking.
Questions/purposes
The purpose of this study was to investigate the effect of varus and valgus adjustments to one commercially available unloader knee brace on tibiofemoral joint loading and knee muscle activation in populations with normal knee alignment.
Methods
The gait of 20 healthy participants (mean age 28.3 years; body mass index 22.9 kg/m2) was analyzed with varus and valgus knee brace conditions and without a brace. Spatiotemporal variables were calculated as were knee adduction moments and muscle activation during stance. A directed cocontraction ratio was also calculated to investigate the relative change in the activation of muscles with medial (versus lateral) moment arms about the knee. Group differences were investigated using analysis of variance. The numbers available would have provided 85% power to detect a 0.05 increase or decrease in the knee adduction moment (Nm/kg*m) in the braced condition compared with the no brace condition.
Results
With the numbers available, there were no differences between the braced and nonbraced conditions in kinetic or muscle activity parameters. Both varus (directed cocontraction ratio 0.29, SD 0.21, effect size 0.95, p = 0.315) and valgus (directed cocontraction ratio 0.28, SD 0.24, effect size 0.93, p = 0.315) bracing conditions increased the relative activation of muscles with lateral moment arms compared with no brace (directed cocontraction ratio 0.49, SD 0.21).
Conclusions
Results revealed inconsistencies in knee kinetics and muscle activation strategies after varus and valgus bracing conditions. Although in this pilot study the results were not statistically significant, the magnitudes of the observed effect sizes were moderate to large and represent suitable pilot data for future work. Varus bracing increased knee adduction moments as expected; however, they produced a more laterally directed muscular activation profile. Valgus bracing produced a more laterally directed muscular activation profile; however, it increased knee adduction moments.
Clinical Relevance
When evaluating changes in knee kinetics and muscle activation together, this study demonstrated conflicting outcomes and questions the efficacy for the use of unloader bracing for people with normally aligned knees such as those after articular cartilage repair.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Three-point leverage systems have been adopted in knee bracing devices to unload the medial or lateral tibiofemoral compartment during weightbearing [3]. Valgus unloading braces are designed to reduce knee adduction moments during stance [12, 18], which contribute to medial tibiofemoral loading [2, 19, 34]. Therefore, they have been used extensively in osteoarthritic populations to unload the medial compartment and reduce knee pain [9, 17, 20, 26, 27, 31, 33, 34]. More recently, in vivo analysis has demonstrated a reduction in medial tibiofemoral joint load during weightbearing activities with valgus bracing using an instrumented knee implant [28]. Unloader braces are often recommended in the postoperative management of tibiofemoral articular cartilage repair surgeries [21, 36, 37] such as autologous chondrocyte implantation. Although excessive loading may be detrimental to the surgical repair and, therefore, increase the risk of some of the characteristic complications associated with autologous chondrocyte implantation [23, 30, 38], these braces may also provide a more favorable mechanical environment for tissue maturation [1, 6, 22, 25].
The experimental basis for use of unloader braces in patients with normal tibiofemoral alignment such as those undergoing articular cartilage repair surgery of the knee is lacking. Research that supports the efficacy of valgus unloading braces has been undertaken in patients with medial compartment osteoarthritis and varus malalignment. In addition, recent research suggests autologous chondrocyte implantation to address chondral defects on the lateral compartment of the tibiofemoral joint makes up 25% to 35% of all tibiofemoral grafts [13, 15, 16]. There is currently no empirical research demonstrating the biomechanical efficacy of varus bracing to unload the lateral compartment of the knee in a healthy or pathological population.
Furthermore, the degree of tibiofemoral joint loading during gait is also influenced by the support of the muscles crossing the knee. Although an increased total activation of muscles will increase tibiofemoral compression, increasing the activation of muscles with moment arms that can produce knee adduction moments [5, 29] such as the medial quadriceps, hamstrings, and gastrocnemius has the potential to mitigate the effects of external valgus knee bracing. The opposite may exist for increased activation of laterally directed muscles in the presence of varus bracing. To the best of our knowledge, there is no research on the effect of varus or valgus unloading bracing on knee muscle activity during gait.
Accordingly, we sought to investigate the effect of varus and valgus adjustments to a commercially available unloader knee brace on knee biomechanics during gait in populations with normal knee alignment. First, we hypothesized that the unloader knee brace with varus and valgus adjustments would increase and decrease knee adduction moments, respectively, during gait. Second, we hypothesized that both bracing conditions would decrease total muscle activation about the knee during the stance phase of gait. Third, we hypothesized that varus bracing would provide a more medially directed muscle activation profile through the increased activation of muscles that can produce knee adduction moments, whereas valgus bracing would have the reverse effect in producing a more laterally directed activation profile.
Materials and Methods
Twenty healthy participants with normal knee alignment (10 men, 10 women) participated in this trial. Subjects were enrolled after a visual assessment by an orthopaedic surgeon (DJW) in a supine and standing position, which confirmed that each subject was not malaligned to the degree that would normally warrant further investigation should it be a patient undergoing chondrocyte implantation for a tibiofemoral cartilage defect. Participants had a mean age of 28.3 years (range, 20–43 years), height of 1.75 m (range, 1.61–1.91 m), weight of 70.8 kg (range, 50.1–96.0 kg), and body mass index of 22.9 kg/m2 (range, 18.4–27.5 kg/m2). None of these participants had worn a knee brace before and had no history of lower limb joint dysfunction. Ethics approval was obtained from the University of Western Australia. All participants provided their informed, written consent before participation.
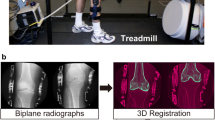
Gait analyses were conducted at the School of Sport Science, Exercise and Health Gait Laboratory at the University of Western Australia. A seven-camera VICON motion analysis system (VICON MX; Oxford Metrics Limited, Oxford, UK) operating at 100 Hz synchronized with two AMTI force plates (MCA-6; Advanced Mechanics Technology Incorporated, Watertown, MA, USA) recording at 2000 Hz was used to monitor participants’ motion. To measure lower body motion, 12-mm retroreflective markers were attached to the pelvis, thigh, shank, foot, and trunk of the participant as per the University of Western Australia marker set [4]. The modeling protocol (including the marker set) used in this study has been assessed for repeatability and reliability previously by Besier et al. [4]. The kinematics and kinetics were shown to be reliable within and between testers. Apart from the markers on the patient’s shoe, all other markers were attached to the skin of the patient (Fig. 1). These were initially attached to the skin with the brace fitted and then not removed for the duration of the testing procedures, therefore avoiding inconsistencies that would arise through marker detachment and reattachment, or by having limb markers attached to the knee brace.
During each gait trial, surface electromyographic (sEMG) data were collected using a 16-channel tethered, double differential EMG system (Delsys, Boston, MA, USA) at 2000 Hz with a 16-bit A/D card. Input impedance was > 100 MΩ and common mode rejection ratio was > 100 dB. Data were synchronized with ground reaction force data in the Vicon MX-Net control box and within the workstation software (Vicon Peak; Oxford Metrics Limited). The skin was prepared by shaving, exfoliating, and then cleaning with alcohol. Bipolar 30-mm disposable surface electrodes (Cleartrace™ Ag/AgCl; ConMed, Utica, NY, USA) with an interelectrode distance of 30 mm were placed over rectus femoris (RF), vastus lateralis (VL), vastus medialis (VM), biceps femoris (BF), semimembranosus (SM), medial gastrocnemius (MG), lateral gastrocnemius (LG), and tensor fasciae latae (TFL) of the left lower limb in line with the muscle fibers [24]. A ground electrode was placed over the iliac crest.
The knee brace used in this trial (OAsys®; Össur, Reykjavik, Iceland) is designed for both the left or right knee and manufactured in small, medium, and large sizes. For convenience, the left lower limb was assessed in all participants. After the appropriate brace was selected for each participant (small, medium, or large), an experienced physical therapist (JRE) customized the fit of the brace using a selection of specialized interior pads that accompany the unloader knee brace kit. Although the experienced therapist had been using these braces for over 10 years, the brace was fitted according to the product instruction manual. Full knee flexion and extension were permitted in the brace.
Participants initially completed a series of calibration trials for subject scaling [4]. These included weightbearing squats to define functional knee axes and hip flexion/extension, abduction/adduction, and circumduction movements to define functional hip center positions [4, 10]. For subject-specific modeling, ankle centers were defined using anatomical landmarks on the medial and lateral malleoli. A six-marker pointer was used to digitize the medial and lateral femoral condyles with a functional knee axis to define knee centers and knee axes orientation [4]. A functional method was also used to define the hip centers [4]. A custom foot alignment rig was used to measure calcaneus inversion/eversion and foot abduction/adduction to define the foot segment anatomical coordinate system [4].
Participants then undertook a series of exercises for sEMG normalization. These included dynamic squats through 75° of active knee flexion and dynamic heel raises through full ankle plantarflexion using individual body weight only and isometric maximal voluntary hamstring curls undertaken in 20° of knee flexion. The choice to use these muscle normalization tasks was the result of ethical considerations associated with applying these procedures to an autologous chondrocyte implantation clinical population. Simply, we chose tasks that targeted the muscles we were recording while ensuring we would not compromise the integrity of the chondral graft after an autologous chondrocyte implantation surgical procedure.
After these calibration procedures, participants were asked to walk at a natural, self-selected speed under three different conditions. These included: (1) walking with the unloader knee brace set to apply an external adduction moment through a 10° knee brace varus alignment (varus knee bracing); (2) walking with the unloader knee brace set to apply an external abduction moment through a 10° knee brace valgus alignment (valgus knee bracing) (Fig. 1); and (3) walking without the brace. These three gait conditions were undertaken in random order. Before each condition, participants conducted a series of practice or familiarization gait trials. The familiarization timeline for each condition varied among participants, lasting no longer than 10 minutes for any condition. After familiarization of each condition, participants were required to complete six “good” trials, which were defined as a participant contacting the force plate with their whole foot without targeting.
Marker trajectories and ground reaction force data were both low pass-filtered at 8 Hz using a zero-lag fourth-order Butterworth filter, selected based on a residual analysis and visual inspection of the kinematic data [14]. Using a custom Matlab function (Matlab 7.8; The Math Works, Inc, Natick, MA, USA), joint centers, marker trajectories, and ground reaction force data were exported into OpenSim 2.1.0 (OpenSim, simtk.org, Stanford, CA, USA). An eight-segment, 17 degree-of-freedom (df) rigid-linked skeletal model was used for kinematic and kinetic modeling (Fig. 2). This model is a condensed version of the 14-segment, 37-df model previously described [11]. Using the scale tool in OpenSim, segment lengths were scaled to each participant’s joint center positions, whereas segment masses and inertial properties were scaled to each participant’s total body mass. The inverse dynamics tool in OpenSim [7] was used to calculate external knee moments during the stance phase of gait.
Depiction of the eight-segment, 17-df rigid-linked skeletal model used for kinematic and kinetic modeling. This model is a condensed version of the 14-segment, 37-df model described in Donnelly et al. [11].
Using custom software in MatLab (Matlab 7.8; The Math Works, Inc), sEMG data were processed by first removing any direct current offsets, then high pass-filtered with a fourth-order Butterworth digital filter at 30 Hz. The signal was then full wave-rectified and then linear enveloped by low-pass filtering with a zero-lag fourth-order Butterworth at 6 Hz. After linear enveloping, peak muscle activation from each muscle recorded during the squat, heel raise, or maximal isometric hamstring trials was used to normalize each muscle’s sEMG signal to 100% effort produced during these functional normalization tasks.
Of the six gait trials that were collected for each condition, four were selected based on similarity in gait velocity across all three gait conditions. An ensemble average was created by the four nominated trials for each condition and specific biomechanical variables were analyzed.
Spatiotemporal variables included mean gait velocity, cadence, stride length, and width. Gait velocity (m/s) was calculated from the displacement of the pelvis origin over one complete stride in the direction of travel divided by stride time. Cadence was calculated as the number of steps per minute. Stride length (m) was calculated as the distance between subsequent heel strikes on the same leg. Stride width (m) was calculated as the perpendicular distance between the origin of the left and right foot’s anatomical coordinate system. Knee kinetic variables of interest included the peak and mean knee adduction moments (Nm/kg*m) over the entire stance phase of gait as well as specifically for the first and second half of stance.
Mean total muscle activation and a mediolateral-directed cocontraction ratio were calculated over the entire stance phase as well as specifically for the first and second halves of stance [24]. Total muscle activation was calculated by taking the sum of the normalized activation of all muscles crossing the knee. A directed cocontraction ratio is a ratio between 1 and −1, which provides directionality between agonist muscles (medial moment arms) and antagonist muscles (lateral moment arms). A directed cocontraction ratio > 0 would indicate cocontraction is directed toward muscles with medial (SM, VM, MG) moment arms, whereas a directed cocontraction ratio < 0 is directed toward muscles with lateral moment arms (BF, VL, LG, TFL). A directed cocontraction ratio = 0 indicates equal activation of agonist and antagonist muscle groups.
When comparing the self-selected gait velocities of participants from the four selected trials within each gait condition, there were no significant spatiotemporal differences between the no brace condition and either the varus or valgus brace conditions (Table 1).
Statistical analysis was performed using SPSS software (SPSS, Version 17.0; SPSS Inc, Cary, NC, USA). An analysis of variance was used to investigate differences among the three gait conditions in spatiotemporal, kinetic, and sEMG dependent variables. To account for multiple comparisons within each group of dependent variables (Tables 1, 2), a Bonferroni adjustment was applied to the alpha accordingly (ie, kinetic variables, 0.05/10 = 0.005; sEMG variables, 0.05/9 = 0.006). A protected Bonferroni post hoc was used to assess any significant findings (α = 0.05). Cohen’s effect sizes were calculated to investigate any potential clinically relevant findings between the brace and no brace conditions for nonsignificant findings. A sample of 20 participants gave 85% power to detect increases or decreases in the knee adduction moment of 0.05 (Nm/kg*m) in the braced condition compared with the no brace condition using a one-tailed test with α = 0.05 and assuming a SD of the difference between conditions of 0.08.
Results
With the numbers available, there were no differences between the braced and nonbraced conditions in the peak or mean knee adduction moments (Table 1) nor any of the sEMG parameters (Table 2). Moderate to large effect sizes were observed for mean total muscle activation through the first (0.59–0.82) and second (0.69–0.91) halves of stance (Table 2).
With the numbers available, there were no differences between the braced and nonbraced conditions in the mediolateral-directed cocontraction ratio results (Table 2). Large effect sizes were observed for the mean mediolateral-directed cocontraction ratio (0.93–0.95) for both brace conditions when compared with no brace (Table 2).
Discussion
Unloader knee braces have been recommended after articular cartilage repair surgery in the tibiofemoral joint [21, 36, 37] to partially unload the repair site and reduce the risk of cell damage or graft delamination. Although these braces have been investigated in osteoarthritic patients with preexisting varus malalignment [8, 9, 12, 18, 27, 32], patients undergoing articular cartilage repair surgery have normal knee alignment [16], limiting the application of these findings. Furthermore, the degree of tibiofemoral loading is also influenced by muscular activation, which has not been investigated in conjunction with external knee moments in existing bracing studies. This study investigated the effect of varus and valgus adjustments to a commercially available unloader knee brace on knee biomechanics during gait in populations with normal knee alignment.
This study had a number of limitations. First, this pilot evaluation was clearly underpowered to detect significant differences resulting from a small sample size. With the numbers provided, this pilot study was powered to detect increases or decreases in the knee adduction moment of 0.05 (Nm/kg*m) in the braced condition compared with the no brace condition with 85% power. Despite the potential clinical significance of these results, a larger sample size may have provided us the power to attain significant findings, especially given the large effect sizes calculated for some of the sEMG-based parameters. Second, the use of healthy participants limited the wide applicability of outcomes. We chose healthy participants in this pilot evaluation, because using a valgus brace in a patient after lateral articular cartilage repair surgery would pose ethical issues and, therefore, a healthy cohort enabled evaluation of all three conditions. Third, the length of time required for appropriate brace acclimatization is unknown, and it is difficult to predict how the duration of wear affects periodic changes in gait and muscular activation patterns. Fourth, based on these results, it would appear that many of the biomechanical changes observed occurred with knee bracing, irrespective of whether it was varus or valgus. Therefore, a fourth condition that involved walking with the brace, set to a neutral alignment, may have allowed us to investigate the influence that wearing a brace alone has on joint biomechanics. Fifth, although every concerted effort was made to best fit the brace to each subject (and condition) by an experienced physical therapist, we were unable to evaluate the actual effectiveness of each brace fit in providing the desired effect. Admittedly, this would also be the case in a real-life setting involving patients undergoing cartilage repair, who are responsible for the adequate fitting and adjustment of their own postoperative unloader brace on a daily basis. Finally, it has been suggested that not all braces are equally effective [12], and differences in braces make it necessary to test each brace design individually [18, 28]. Unfortunately, studies frequently only state that bracing was used and do not specify what type of brace. Future research should specify the type, model, settings, and rationale for brace use during cartilage repair clinical trials.
With the subject numbers available, no significant knee adduction moment changes were observed in this cohort after varus or valgus bracing. Valgus unloading braces have previously demonstrated reduced knee pain [9, 17, 20, 26, 27, 31, 33, 34] and knee adduction moments during stance [12, 18] in varus-aligned osteoarthritic populations as well as reduced medial tibiofemoral joint loading during weightbearing activities recorded using an instrumented total knee replacement implant [28]. However, the current study does not provide biomechanical evidence in support of their use in normally aligned healthy subjects, particularly if reducing the knee adduction moment is the purpose of such brace use. As alluded to earlier, this finding may be the result of the underpowered nature of this trial in which these results may serve as hypothesis-generating pilot data for a larger prospective trial investigating these unloader braces in normally aligned healthy and pathological populations (such as those following autologous chondrocyte implantation). Alternatively, given the low effect sizes observed for the knee adduction moment variables, it may reflect that these unloader braces are not effective in a patient group with normal lower limb alignment. Richards et al. [35] have debated the efficacy of unloader bracing as a result of the large resistive moments that would be required, suggesting that increased proprioception and/or a placebo effect may produce the improvements in gait and function. Furthermore, Kutzner et al. [28] reported large differences in load changes between subjects as well as between different unloader braces. Further investigation is warranted to evaluate the clinical relevance of any observed changes.
In addition to external moments, the contribution of muscular forces during stance must be considered when estimating knee articular loading. However, there were also no differences between the braced and nonbraced conditions for any of the sEMG parameters, including total muscle activation and the mediolateral-directed cocontraction ratio. Unfortunately, comparison of our data with other research on the effect of varus or valgus unloading bracing on knee muscle activity cannot be undertaken, because, to our knowledge, there are no other such studies. As discussed for the knee adduction moments observed, this pilot trial may have been underpowered to detect significant changes in these sEMG variables. Given the large effect sizes observed for the mean mediolateral-directed cocontraction ratio (with varus and valgus knee bracing), it would appear that muscle activation was directed less toward muscles with medial moment arms, representing a more laterally directed muscle activation strategy. Although a more laterally directed activation profile was expected for valgus bracing, which would redirect tibiofemoral knee load away from the medial compartment, it was not expected for the varus brace condition. A relative increase in the activation of the lateral musculature with varus bracing would likely increase compressive loads on the lateral compartment. Again, we believe these results may serve as hypothesis-generating pilot data for a larger prospective trial. Nevertheless, should a total reduction in knee articular load be related solely to a reduction in muscular activation, as opposed to a reduction in the knee adduction moment, the efficacy of these unloader braces in a postoperative articular cartilage repair cohort can be questioned.
In conclusion, the results of this study do not support the use of these unloader braces in subjects with normally aligned knees, particularly if the purpose of the brace is to reduce the knee adduction moment and/or alter muscle activation patterns to reduce compartmental knee load. Nevertheless, these results will serve as hypothesis-generating pilot data in the development of larger prospective trials investigating these unloader braces in normally aligned healthy and pathological populations (such as those after autologous chondrocyte implantation). Ongoing research investigating the use of unloader bracing must evaluate muscular activation in addition to knee kinetics to provide a more accurate representation of the influence of bracing on articular loading.
References
Arokoski J, Jurvelin J, Vaatainen U. Normal and pathological adaptations of articular cartilage to joint loading. Scand J Med Sci Sports. 2000;10:186–198.
Barrios JA, Higginson JS, Royer TD, Davis IS. Static and dynamic correlates of the knee adduction moment in healthy knees ranging from normal to varus-aligned. Clin Biomech (Bristol, Avon). 2009;24:850–854.
Beaudreuil J, Bendaya S, Faucher M, Coudeyre E, Ribinik P, Revel M, Rannou F. Clinical practice guidelines for rest orthosis, knee sleeves, and unloading knee braces in knee osteoarthritis. Joint Bone Spine. 2009;76:629–636.
Besier TF, Sturnieks DL, Alderson JA, Lloyd DG. Repeatability of gait data using a functional hip joint centre and a mean helical knee axis. J Biomech. 2003;36:1159–1168.
Buchanan TS, Lloyd DG. Muscle activation at the human knee during isometric flexion-extension and varus-valgus loads. J Orthop Res. 1997;15:11–17.
Carter DR, Beaupre GS, Wong M, Smith RL, Andriacchi TP, Schurman DJ. The mechanobiology of articular cartilage development and degeneration. Clin Orthop. 2004:S69–77.
Delp SL, Anderson FC, Arnold AS, Loan P, Habib A, John CT, Guendelman E, Thelen DG. OpenSim: open-source software to create and analyze dynamic simulations of movement. IEEE Transactions on Bio-Medical Engineering. 2007;54:1940–1950.
Dennis AD, Komistek RD. An in vivo analysis of the effectiveness of the osteoarthritic knee brace during heel strike and midstance of gait. Acta Chir Orthop Traumatol Cech. 1999;66:323–327.
Dennis DA, Komistek RD, Nadaud MC, Mahfouz M. Evaluation of off-loading braces for treatment of unicompartmental knee arthrosis. J Arthroplasty. 2006;21:2–8.
Donnelly CJ, Elliott BC, Doyle TL, Finch CF, Dempsey AR, Lloyd DG. Changes in knee joint biomechanics following balance and technique training and a season of Australian football. Br J Sports Med. 2012;46:917–922.
Donnelly CJ, Lloyd DG, Elliott BC, Reinbolt JA. Optimizing whole-body kinematics to minimize valgus knee loading during sidestepping: implications for ACL injury risk. J Biomech. 2012;45:1491–1497.
Draganich L, Reider B, Rimington T, Piotrowski G, Mallik K, Nasson S. The effectiveness of self-adjustable custom and off-the-shelf bracing in the treatment of varus gonarthrosis. J Bone Joint Surg Am. 2006;88:2645–2652.
Ebert JR, Fallon M, Ackland TR, Wood DJ, Janes GC. Arthroscopic Matrix-Induced Autologous Chondrocyte Implantation: 2-Year Outcomes. Arthroscopy. 2012.
Ebert JR, Lloyd DG, Ackland T, Wood DJ. Knee biomechanics during walking gait following matrix-induced autologous chondrocyte implantation. Clin Biomech (Bristol, Avon). 2010;25:1011–1017.
Ebert JR, Robertson WB, Lloyd DG, Zheng MH, Wood DJ, Ackland T. A prospective, randomized comparison of traditional and accelerated approaches to postoperative rehabilitation following autologous chondrocyte implantation: 2-year clinical outcomes. Cartilage. 2010:1947603510362907.
Ebert JR, Robertson WB, Woodhouse J, Fallon M, Zheng MH, Ackland T, Wood DJ. Clinical and magnetic resonance imaging-based outcomes to 5 years after Matrix-Induced Autologous Chondrocyte Implantation to address articular cartilage defects in the knee. 39. 2011;4:753–763.
Fantini Pagani CH, Hinrichs M, Bruggemann GP. Kinetic and kinematic changes with the use of valgus knee brace and lateral wedge insoles in patients with medial knee osteoarthritis. J Orthop Res. 2012;30:1125–1132.
Fantini Pagani CH, Potthast W, Bruggemann GP. The effect of valgus bracing on the knee adduction moment during gait and running in male subjects with varus alignment. Clin Biomech (Bristol, Avon). 2010;25:70–76.
Foroughi N, Smith R, Vanwanseele B. The association of external knee adduction moment with biomechanical variables in osteoarthritis: a systematic review. Knee. 2009;16:303–309.
Gaasbeek RD, Groen BE, Hampsink B, van Heerwaarden RJ, Duysens J. Valgus bracing in patients with medial compartment osteoarthritis of the knee. A gait analysis study of a new brace. Gait & Posture. 2007;26:3–10.
Hambly K, Bobic V, Wondrasch B, Van Assche D, Marlovits S. Autologous Chondrocyte Implantation Postoperative Care and Rehabilitation: Science and Practice. Am J Sports Med. 2006;34:1–19.
Hambly K, Silvers HJ, Steinwachs M. Rehabilitation after articular cartilage repair of the knee in the football (soccer) player. Cartilage. 2011;3:50S–56S.
Harris JD, Siston RA, Brophy RH, Lattermann C, Carey JL, Flanigan DC. Failures, re-operations, and complications after autologous chondrocyte implantation - A systematic review. Osteoarthritis Cartilage. 2011;19:779–791.
Heiden TL, Lloyd DG, Ackland TR. Knee joint kinematics, kinetics and muscle co-contraction in knee osteoarthritis patient gait. Clin Biomech (Bristol, Avon). 2009;24:833–841.
Khan KM, Scott A. Mechanotherapy: how physical therapists’ prescription of exercise promotes tissue repair. Br J Sports Med. 2009;43:247–252.
Kirkley A, Webster-Bogaert S, Litchfield R, Amendola A, MacDonald S, McCalden R, Fowler P. The effect of bracing on varus gonarthrosis. J Bone Joint Surg Am. 1999;81:539–548.
Komistek RD, Dennis DA, Northcut EJ, Wood A, Parker AW, Traina SM. An in vivo analysis of the effectiveness of the osteoarthritic knee brace during heel-strike of gait. J Arthroplasty. 1999;14:738–742.
Kutzner I, Kuther S, Heinlein B, Dymke J, Bender A, Halder AM, Bergmann G. The effect of valgus braces on medial compartment load of the knee joint - in vivo load measurements in three subjects. J Biomech. 2011;44:1354–1360.
Lloyd DG, Buchanan TS. Strategies of muscular support of varus and valgus isometric loads at the human knee. J Biomech. 2001;34:1257–1267.
Niemeyer P, Pestka JM, Kreuz PC, Erggelet C, Schmal H, Suedkamp NP, Steinwachs M. Characteristic Complications After Autologous Chondrocyte Implantation for Cartilage Defects of the Knee Joint. Am J Sports Med. 2008;36:2091–2099.
Pollo FE, Otis JC, Backus SI, Warren RF, Wickiewicz TL. Reduction of medial compartment loads with valgus bracing of the osteoarthritic knee. Am J Sports Med. 2002;30:414–421.
Raja K, Dewan N. Efficacy of knee braces and foot orthoses in conservative management of knee osteoarthritis: a systematic review. Am J Phys Med Rehabil. 2011;90:247–262.
Ramsey DK, Briem K, Axe MJ, Snyder-Mackler L. A mechanical theory for the effectiveness of bracing for medial compartment osteoarthritis of the knee. J Bone Joint Surg Am. 2007;89:2398–2407.
Rannou F, Poiraudeau S, Beaudreuil J. Role of bracing in the management of knee osteoarthritis. Curr Opin Rheumatol. 2010;22:218–222.
Richards J, Sanchez-Ballester J, Jones R, Darke N, Livingstone B. A comparison of knee braces during walking for the treatment of osteoarthritis of the medial compartment of the knee. J Bone Joint Surg Br. 2005;87-B:937–939.
Saris DB, Vanlauwe J, Victor J, Haspl M, Bohnsack M, Fortems Y, Vandekerckhove B, Almqvist KF, Claes T, Handelberg F, Lagae K, van der Bauwhede J, Vandenneucker H, Yang KG, Jelic M, Verdonk R, Veulemans N, Bellemans J, Luyten FP. Characterized chondrocyte implantation results in better structural repair when treating symptomatic cartilage defects of the knee in a randomized controlled trial versus microfracture. Am J Sports Med. 2008;36:235–246.
Van Assche D, Staes F, Van Caspel D, Vanlauwe J, Bellemans J, Saris DB, Luyten FP. Autologous chondrocyte implantation versus microfracture for knee cartilage injury: a prospective randomized trial, with 2-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2010;18:486–495.
Wood JJ, Malek MA, Frassica FJ, Polder JA, Mohan AK, Bloom ET, Braun MM, Cote TR. Autologous Cultured Chondrocytes: Adverse Events Reported to the United States Food and Drug Administration. J Bone Joint Surg Am. 2006;88:503–507.
Acknowledgments
We thank Mr James Dunne and Mr Denny Wells for their assistance in data processing. We also thank Winthrop Professor David J. Wood for his assistance in the appropriate selection and stratification of healthy subjects to fulfill the study inclusion criteria and Drs Ben Jackson and Anne Smith for statistical assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
Funding provided by the Hollywood Private Hospital Research Foundation (JRE, TRA) and the National Health and Medical Research Council (JRE).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the School of Sport Science, Exercise and Health, University of Western Australia, Crawley, Perth, Western Australia.
About this article
Cite this article
Ebert, J.R., Hambly, K., Joss, B. et al. Does an Unloader Brace Reduce Knee Loading in Normally Aligned Knees?. Clin Orthop Relat Res 472, 915–922 (2014). https://doi.org/10.1007/s11999-013-3297-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-013-3297-8