Abstract
Background
In studies of TKA, treating each knee as an independent case in patients with bilateral TKAs can lead to errors, because patients with bilateral and unilateral TKAs may achieve different levels of function and because the assumption of statistical independence is violated.
Questions/purposes
We determined whether (1) patients undergoing bilateral TKAs have different demographics and preoperative and postoperative function from those undergoing unilateral TKAs, and (2) means, SEs, and p values change substantially based on how the two cases of bilateral TKAs are treated in statistical analyses.
Methods
We retrospectively compared 513 patients undergoing unilateral TKAs and 602 patients undergoing bilateral TKAs regarding demographics (age, gender, BMI), preoperative and 1-year postoperative function (motion arc, American Knee Society score, patellofemoral score, WOMACTM, SF-36). Each case of a bilateral TKA was treated as independent in the reference analyses. Then changes of mean, SEs, and p values were compared with those of the reference method when three other methods of analysis were used: using mean values of both knees, randomly selecting one side, and using a generalized estimating equation.
Results
Patients undergoing bilateral TKAs had higher female predominance (95% versus 90%) and BMI (27.4 versus 26.1 kg/m2) than those undergoing unilateral TKAs. Although patients undergoing bilateral TKAs had worse preoperative function, they achieved comparable function at 1 year. The mean values did not differ considerably depending on the four methods. The SEs and p values of the reference method were generally the smallest, but the differences appeared negligible.
Conclusions
Our analyses suggest bilaterality can be ignored in the analysis of TKA, since postoperative function is comparable between unilateral and bilateral TKAs and the theoretical errors in statistical analysis had little effect on the results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
TKA is a preferred treatment option for elderly patients with advanced knee osteoarthritis [1, 7, 9, 23], but modifications have been introduced to further improve current surgical techniques and implant designs [21, 56]. To determine whether a modification achieves its intended aims, it is crucial to evaluate the effects of the factor investigated while controlling for potentially confounding factors. Because osteoarthritis, the most common diagnosis in patients undergoing TKA, frequently involves both knees, 27% to 36% of TKAs are performed bilaterally [9, 47]. In the patients undergoing a unilateral TKA, the effect of the contralateral knee should be considered when evaluating the function since the contralateral nonoperated knee influences patient function [12]. In fact, osteoarthritis in the contralateral knee frequently progresses, eventually warranting a subsequent second TKA in 37% to 43% [36, 38, 46]. However, the function of each knee in a patient undergoing bilateral TKAs may be influenced by the replaced contralateral knee, rather than the osteoarthritic joint. Therefore, whether a patient has had one or both knees replaced can be a confounding factor when evaluating patient function after TKA, and it seems that attention needs to be paid to bilaterality if bilateral cases are included in the study subjects.
Whether one or both knees have been replaced was not considered in several studies reporting function following TKA and where bilateral TKAs typically were treated as separate cases in the statistical analyses [18, 19, 33, 47, 52]. This method of analysis inherently violates the principle of independent samples, a key assumption for parametric tests in statistical analyses [43, 59]. Park et al. [40] recently reported that approximately 79% of recent orthopaedic papers containing bilateral cases in one journal possibly had violated statistical independence assumption, including knee-related articles. Furthermore, if the demographic features and preoperative and postoperative function of patients undergoing bilateral TKAs differ from those of patients undergoing unilateral TKAs, the proportion of bilateral TKAs should be taken into consideration, and proper analytical tools should be used during the assessment of the effects of a new surgical technique or implant. However, the previous studies dealing with bilateral TKAs have focused more on mortality and morbidity [8, 10, 26, 29, 37, 44, 47, 53], inpatient costs [29, 35, 45], and early postoperative pain [42, 51], rather than overall features of demographics and preoperative functional status with comprehensive assessment. In addition, whether patient function differs after bilateral and unilateral TKAs has been inconclusive in the literature. Some studies have reported better function in patients after bilateral TKAs than those undergoing a unilateral TKA [15, 19, 35, 47], whereas others found no functional differences in patients having unilateral and bilateral TKAs [10, 26, 50, 52, 57, 58]. Bilateral osteoarthritis of the knee is more frequent in Asian patients than in western patients, consequently bilateral TKAs are more frequently performed [25, 26, 60]. Therefore it is important to clarify whether one must statistically account for bilaterality in studies of Asian patients.
In this study, we asked whether (1) patients undergoing bilateral TKAs have different demographic features and poorer preoperative and postoperative function than patients undergoing unilateral TKAs, and (2) means, SEs, and p values change substantially based on how the knees of a patient undergoing bilateral TKAs are considered in statistical analyses.
Patients and Methods
We retrospectively reviewed 1115 patients who underwent 1717 primary TKAs between December 2003 and December 2009, and all cases were included in the analyses for demographic features and preoperative functional status. When comparing postoperative function, we excluded patients with (1) a diagnosis other than primary osteoarthritis, (2) systemic comorbidities preventing them from benefitting from the replaced knee, (3) postoperative complications affecting postoperative function, and (4) a functional evaluation not performed 1 year after surgery. According to the exclusion criteria, we excluded a total of 293 of the 1115 patients (26%) for various reasons: (1) 62 patients (76 knees) with a diagnosis other than osteoarthritis, such as postinfectious arthritis, posttraumatic and rheumatoid arthritis; (2) 201 patients with systemic comorbidities preventing them from benefitting from the replaced knee (concurrent spine or hip problem [50 knees in 39 patients], death unrelated to the surgery [21 knees in 16 patients], other serious medical problems unrelated to the surgery including cerebrovascular accident, Parkinson’s disease, cancer, dementia, chronic renal failure, and other medical infirmities [171 knees in 113 patients], and other problems [36 knees in 33 patients]); and (3) 30 patients with postoperative complications affecting postoperative outcomes (periprosthetic infection [12 knees in 10 patients], wound complication [11 knees in 10 patients], periprosthetic fracture [five knees in five patients], loosening or instability [five knees in five patients]). In addition, 49 contralateral knees in the patients undergoing bilateral TKAs, whose opposite knees were excluded for one of above reasons, were also excluded to remove confounding effects of the contralateral knees. Consequently, the 293 excluded patients left 822 who had 1281 TKAs, 363 patients undergoing unilateral TKAs and 459 patients undergoing bilateral TKAs (simultaneous or staged). Postoperative function was evaluated at the routine visit 1 year after surgery. No patients were recalled specifically for this study; all data were obtained from medical records and radiographs. This study was approved by the institutional review board of our hospital, and all patients provided preoperative informed consent regarding the use of their medical records.
To determine whether our sample size was adequate, we performed a priori power analysis using the two-sided hypothesis test at an alpha level of 0.05 and statistical power of 80%. Sixty-four knees were required for each group to detect a 5° difference in motion arc between patients with unilateral TKAs and with bilateral TKAs and a 5% difference in functional scores, which we considered to be clinically important [2]. Thus, the sample size used in this study was regarded as adequate.
We selected TKA as the treatment option after discussion with the patient, family members of the patient, and the operating surgeon. While recommending TKA, the operating surgeon considered three criteria, namely, age (typically 60 years or older), radiographic severity of knee osteoarthritis (typically Kellgren-Lawrence Grade 3 or higher [22]), and symptom severity (disabling pain and functional disabilities not responding to any of the nonsurgical treatments provided for more than 3 months) [11, 34]. We recommended bilateral TKAs for patients who satisfied all three criteria in both knees. Bilateral TKAs were performed in a simultaneous or staged manner. The interval between the first and second procedures in staged bilateral TKAs was typically 1 (17%) or 2 weeks (57%), but this interval ranged from 4 to 1207 days. We recommended unilateral TKA for patients who showed radiographic osteoarthritis Kellgren-Lawrence Grade 3 or less or for those who did not have severe symptoms or functional disabilities of the other knee.
All surgeries were performed by one surgeon (TKK) using the standard medial parapatellar approach. We implanted one of two posterior-stabilized TKA systems (Genesis II®; Smith & Nephew, Memphis, TN, USA; and E-motion®; B. Braun-Aesculap, Tuttlingen, Germany) in all knees. The Genesis II® is a fixed-bearing system, whereas the E-motion® is a mobile-bearing system. Implant selection was done at the operating surgeon’s discretion without any specific selection criteria. In all cases, the patella was resurfaced, and implant fixation was performed using cement.
A compressive dressing was applied with an immobilizer during the first 24 hours after surgery, and patients were encouraged to perform quadriceps strengthening exercises after they had returned to the ward from the recovery unit. After the first 24 hours, the patients began using a continuous passive motion (CPM) machine. The CPM machine was used twice a day for 1 to 2 hours until discharge and ROM was increased as tolerated. All patients were allowed to walk as tolerated using a walker and start active and passive ROM exercises on the second postoperative day. From the 3rd postoperative day, the patients underwent a physiotherapy session once daily until discharge, which consisted of the quadriceps strengthening exercise and gait training using a walking aid. Patients were discharged typically on the 7th or 14th postoperative day.
After discharge, patients were followed up at 2 weeks, 6 weeks, 3 months, 6 months, and 1 year, and annually after 1 year. One independent investigator (YGK) prospectively collected all clinical information using predesigned data collection sheets. This information included demographic data and preoperative function and postoperative function evaluated at 12 months after surgery. We evaluated preoperative and postoperative function by obtaining the motion arc, American Knee Society (AKS) knee and function scores [20], the patellofemoral scores including anterior knee pain, ability to rise from a chair, and stair climbing [13], WOMACTM pain, stiffness, and function scores [3], and SF-36 eight subscales and two summary scales [55]. Motion arc was measured from maximum extension to maximum flexion using a standard clinical goniometer (38 cm) to the nearest 5° with the patient supine.
The unilateral and bilateral TKA groups were compared with respect to the demographic data (age, sex, height, weight, and BMI) and preoperative and postoperative functional statuses (motion arc, AKS score, patellofemoral scoring system, and WOMACTM and SF-36 scores). We conducted the analyses in four different ways based on how two knees in a patient undergoing bilateral TKAs were treated in data analyses: (1) each knee in a patient undergoing bilateral TKAs was considered as two separate cases; (2) a mean value of both knees was taken as the representative value; (3) the values of a randomly selected knee from both knees using a computer-generated randomization table were taken as the representative values; and (4) the generalized estimating equation (GEE), an advanced statistical method that is able to address statistical dependency within same subjects [30, 40, 59]. Statistical significance of the differences of demographics between the two groups was determined by the chi-square test for the categorical variables and Student’s t-test for the continuous variables. For comparing preoperative and postoperative motion arc and functional scores, we used analysis of covariance or GEE to adjust for the possible confounding effects such as age, sex, and BMI. The implant type also was controlled as a covariate when analyzing postoperative function. Among the four ways of statistically handling bilateral TKAs, the first method, which treated each knee in bilateral TKAs as two independent unilateral TKAs, was used as the reference method. Changes in summary values such as means, SEs, and p values of other three methods with reference to the first were computed to determine the effects of the four different methods of statistical analyses on the comparisons of function between unilateral and bilateral TKAs. We considered these three parameters as important in data analysis because a mean value typically is used as the representative value, and SE and p value are parameters which determine statistical significance. We performed all statistical analysis with SPSS® for Windows® (Version 15.0; SPSS, Chicago, IL, USA).
Results
The patients undergoing bilateral TKAs had dissimilar demographic features and inferior preoperative functional status but achieved equally good function at 1 year after surgery compared with the patients undergoing unilateral TKAs. Patients undergoing bilateral TKAs had a higher female predominance (95% versus 90%, p = 0.001) and a higher mean BMI (27.4 versus 26.1 kg/m2, p < 0.001) than those undergoing unilateral TKAs (Table 1). Patients with bilateral TKAs had worse AKS scores (function), patellofemoral scores (anterior knee pain, chair rising, and stair climbing), WOMACTM score (pain, function, and total), and SF-36 scores (physical functioning, role-physical, bodily pain, social functioning, and physical component summary) (Table 1). Despite worse preoperative clinical status, the patients undergoing bilateral TKAs achieved comparable function to the patients undergoing unilateral TKAs (Table 2). There were no differences between the two groups in all outcome scales except for maximum flexion (131.9° versus 129.5o, p = 0.006) and AKS function score (93.9 versus 92.5, p = 0.033), which were better in patients with bilateral TKAs than in those with unilateral TKAs; however, the differences in the two outcome scales were smaller than the values of a clinically meaningful difference, that is, a difference of 5o or greater for motion arc and 5% or greater of the maximum points of an outcome scale.
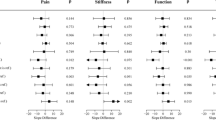
When different analytical methods were used, the results varied in terms of means, SEs, and p values, but the differences were small and clinically unimportant. Maximal difference in the mean values of motion arc and functional scores were 0.4° and 0.3 points, respectively (Table 3). The SEs were generally the smallest when both knees in patients undergoing bilateral TKAs were considered as separate cases, but their maximum changes in motion arc and functional scores were 0.2o and 0.3 points, respectively, when the other analytical methods were used (Table 4). Similarly, the p values were the smallest in most cases when both knees in patients undergoing bilateral TKAs were considered as separate cases. However, these differences were small, and there was a change in the significance of only two variables when 0.05 was regarded as the cutoff value: preoperative SF-36 social functioning score and postoperative AKS function score (Table 5).
Discussion
TKAs can be performed in one or both knees, and whether TKAs are performed unilaterally or bilaterally can be an important confounding factor in evaluating patient function. However, this issue has frequently been ignored in previous studies, and comprehensive information regarding the differences between patients undergoing unilateral or bilateral TKAs is not available. Furthermore, both knees in patients undergoing bilateral TKAs have been commonly considered as separate cases in statistical analyses despite their correlation in the same subject. This method of analysis may have some theoretical problems because it violates the principle of statistical independence, which means that each observation is not affected by another observation [6, 40, 43]. Therefore, we (1) compared the differences between patients undergoing unilateral or bilateral TKAs in terms of preoperative clinical status, including demographics and postoperative functional outcomes, and (2) determined whether the compared results vary based on how two knees in a patient undergoing bilateral TKAs are considered in statistical analyses.
Our findings should be interpreted in light of several limitations. First, female dominance was remarkable in our patients undergoing TKAs. This unique sex composition was reported in previous studies of Korean patients undergoing TKAs [24, 27, 28, 39], and should be taken into consideration if our findings are to be extrapolated to a population with a different sex composition. Second, we performed bilateral TKAs in a simultaneous (46%) or staged manner (54%). Bilateral procedures can be done simultaneously or at varying intervals. Theoretically, early function may vary according to the timing of bilateral TKAs, but we do not believe that function at 1 year after surgery is likely to be affected to the clinically meaningful extent by the timing. Third, two different implants, one fixed-bearing and one mobile-bearing system, were used with different proportions between two groups (Emotion®:Genesis II® = 53:47 in unilateral and 39:61 in bilateral TKA groups, p < 0.001), therefore the choice of implant could be a confounding factor. However, implant selection was made at the operating surgeon’s discretion without any specific selection criteria, and the implant type was controlled as a covariate in the statistical analyses. Furthermore, we identified no differences in postoperative function between the two implants with other factors controlled (data not shown). Fourth, approximately ¼ of all cases were excluded for various reasons in the analyses of postoperative function. This exclusion might limit the representativeness of this study cohort, and the subjects for analyses of postoperative function were different from those for preoperative function and demographics. However, the results of additional analyses of all subjects including patients who were excluded were not remarkably different from those of this study (data not shown). Therefore, we believe the exclusion criteria did not bias our findings substantially.
We found patients undergoing bilateral TKAs had worse preoperative clinical statuses than those undergoing unilateral TKAs with some differences in demographics. Our findings differ from those of previous studies reporting similar preoperative clinical statuses between patients undergoing unilateral or bilateral TKAs [10, 15, 26, 35, 58] (Table 6). However, we believe our findings to be more intuitively reasonable. Functional deterioration can be much greater if the advanced arthritic joints causing severe pain are multiple rather than single lesion. The demographic features also were notable in this study. There was a greater proportion of female patients among patients undergoing bilateral TKAs than among those undergoing unilateral TKAs. A similar sex composition was found in a Korean study reporting female dominance among patients undergoing simultaneous bilateral TKAs than unilateral TKA (94% versus 80%) [26]. In contrast, other studies in Western subjects [15, 29, 45] had a similar sex composition between patients undergoing bilateral TKAs and those undergoing unilateral TKAs. In addition, patients undergoing bilateral TKAs had a higher BMI than those undergoing unilateral TKAs. It is well documented that overweight individuals or obese individuals have an increased risk of knee osteoarthritis [14, 16, 32]. Furthermore, it is conceivable that a higher BMI might not only have contributed to the involvement of both knees but also might have contributed to worse preoperative clinical status in our patients undergoing bilateral TKAs.
We found the function of patients with bilateral TKAs comparable to that of patients with unilateral TKAs. Although the bilateral TKA group had better maximum flexion and AKS function score, the differences were not large enough to be clinically meaningful. Our findings concur with those of previous studies reporting similar [10, 26, 50, 52, 57, 58] or better [15, 19, 35, 47] function of bilateral TKAs compared with unilateral TKAs (Table 6). The patients undergoing bilateral TKAs achieved comparable outcomes despite worse preoperative clinical status. These findings might suggest that the bilateral TKA group achieved greater improvement after TKA than the unilateral TKA group. There are several conceivable explanations for these findings. First, improved function in both knees could have contributed to favorable clinical results in the patients undergoing bilateral TKAs. Second, a possible limb length discrepancy after TKA could affect the function in patients undergoing unilateral TKA. A previous study reported that more frequent and greater limb length discrepancy was observed after unilateral TKA than after bilateral TKAs and that the discrepancy had a major effect on functional outcome in patients undergoing unilateral TKAs [54]. However, we did not evaluate leg length discrepancy in our study and the effect of the discrepancy was not certain. Third, the contralateral knee in the patients undergoing unilateral TKAs could have a negative effect on the postoperative clinical outcomes. Although there was no case of osteoarthritis severe enough to warrant TKA of the contralateral knee in patients undergoing unilateral TKA, some patients had mild to moderate (Kellgren-Lawrence Grades 1–3) osteoarthritis in the contralateral knee. A previous study found that the nonoperated knee was a major contributor to the functional performance after TKA [12].
Researchers may encounter a dilemma regarding whether both knees in a patient undergoing bilateral TKAs can be considered as independent cases or analyzed in another way. This issue has been ignored in some studies [6, 40]. Some studies have analyzed the function of bilateral TKAs without considering the independent contributions of each knee and regarding only the overall function of patient in the analyses [35, 58], but in others an analysis was done on the assumption that each knee independently contributed to overall function or they did not clearly state how the knees in a patient undergoing bilateral TKAs were treated in the analyses [10, 15, 19, 26, 47, 50, 52, 57] (Table 6). We found the alterations in mean, SE, and p value did not vary substantially depending on the four different methods. Our findings suggest that, despite the theoretical concern, reasonable conclusions would be drawn with any of the four statistical methods when analyzing mixed study subjects including bilateral cases. These findings are coincident with those of previous studies with hip and knee data showing little effect of bilaterality on the results [4, 17, 31, 48, 49]. However, our findings may not be applicable to other study situations that differ from ours which included a large sample size and used only four analytical methods. As our study was retrospective, we were able to include a much larger sample size than the number suggested by sample size estimation. Small changes of statistics depending on different analytical methods might be attributable to a large sample size in this study, since the variability according to different methods reportedly decreases as the number of cases increases [39]. Different results might also be obtained if the sample size was small and different methods were used, such as a mixed-effect model [5]. Therefore, caution should be exercised to choose proper analytical methods when dealing with data from bilateral TKA cases because of the possibility of bias resulting from violation of the statistical independence assumption, as pointed out in the literature [6, 40, 41, 43].
Our study showed that patients undergoing bilateral TKAs have higher female predominance, higher BMI, and worse preoperative functional status but achieve equivalent function after surgery compared with those undergoing unilateral TKAs. Our findings also suggested that reasonable conclusions would be drawn with any of the four statistical methods in the analysis of function after TKA, even though bilaterality was not considered, when unilateral and bilateral cases were included. Therefore, we concluded that bilaterality can be ignored in the analysis of TKAs with little bias despite the theoretical concern.
References
Aglietti P, Buzzi R, De Felice R, Giron F. The Insall-Burstein total knee replacement in osteoarthritis: a 10-year-minimum follow-up. J Arthroplasty. 1999;14:560–565.
Angst F, Aeschlimann A, Stucki G. Smallest detectable and minimal clinically important differences of rehabilitation intervention with their implications for required sample sizes using WOMAC and SF-36 quality of life measurement instruments in patients with osteoarthritis of the lower extremities. Arthritis Rheum. 2001;45:384–391.
Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840.
Bjorgul K, Novicoff WM, Brevig K, Ahlund O, Wiig M, Saleh KJ. Patients with bilateral procedures can be included in total hip arthroplasty research without biasing results. J Arthroplasty. 2011;26:120–123.
Brown H, Prescott R. Applied Mixed Models in Medicine. Chichester, England; Hoboken, NJ: John Wiley; 2006.
Bryant D, Havey TC, Roberts R, Guyatt G. How many patients? How many limbs? Analysis of patients or limbs in the orthopaedic literature: a systematic review. J Bone Joint Surg Am. 2006;88:41–45.
Buechel FF Sr. Long-term followup after mobile-bearing total knee replacement. Clin Orthop Relat Res. 2002;404:40–50.
Bullock DP, Sporer SM, Shirreffs TG Jr. Comparison of simultaneous bilateral with unilateral total knee arthroplasty in terms of perioperative complications. J Bone Joint Surg Am. 2003;85:1981–1986.
Callahan CM, Drake BG, Heck DA, Dittus RS. Patient outcomes following tricompartmental total knee replacement: a meta-analysis. JAMA. 1994;271:1349–1357.
Cohen RG, Forrest CJ, Benjamin JB. Safety and efficacy of bilateral total knee arthroplasty. J Arthroplasty. 1997;12:497–502.
Cross WW 3rd, Saleh KJ, Wilt TJ, Kane RL. Agreement about indications for total knee arthroplasty. Clin Orthop Relat Res. 2006;446:34–39.
Farquhar S, Snyder-Mackler L. The Chitranjan Ranawat Award: The nonoperated knee predicts function 3 years after unilateral total knee arthroplasty. Clin Orthop Relat Res. 2010;468:37–44.
Feller JA, Bartlett RJ, Lang DM. Patellar resurfacing versus retention in total knee arthroplasty. J Bone Joint Surg Br. 1996;78:226–228.
Felson DT, Anderson JJ, Naimark A, Walker AM, Meenan RF. Obesity and knee osteoarthritis: the Framingham Study. Ann Intern Med. 1988;109:18–24.
Fick D, Crane T, Shakespeare D. A comparison of bilateral vs. unilateral total knee arthroplasty mobilised using a flexion regime. Knee. 2002;9:285–289.
Gelber AC, Hochberg MC, Mead LA, Wang NY, Wigley FM, Klag MJ. Body mass index in young men and the risk of subsequent knee and hip osteoarthritis. Am J Med. 1999;107:542–548.
Havelin LI, Espehaug B, Vollset SE, Engesaeter LB. The effect of the type of cement on early revision of Charnley total hip prostheses: a review of eight thousand five hundred and seventy-nine primary arthroplasties from the Norwegian Arthroplasty Register. J Bone Joint Surg Am. 1995;77:1543–1550.
Hickey BA, Kempshall PJ, Metcalfe AJ, Forster MC. Review of Kinemax total knee replacements performed at the NHS treatment centre, Weston-Super-Mare: five-year results. J Bone Joint Surg Br. 2012;94:510–516.
Hooper GJ, Hooper NM, Rothwell AG, Hobbs T. Bilateral total joint arthroplasty: the early results from the New Zealand National Joint Registry. J Arthroplasty. 2009;24:1174–1177.
Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14.
Kalisvaart MM, Pagnano MW, Trousdale RT, Stuart MJ, Hanssen AD. Randomized clinical trial of rotating-platform and fixed-bearing total knee arthroplasty: no clinically detectable differences at five years. J Bone Joint Surg Am. 2012;94:481–489.
Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502.
Kelly MA, Clarke HD. Long-Term Results of Posterior Cruciate-Substituting Total Knee Arthroplasty. Clin Orthop Relat Res. 2002;404:51–57.
Kim JM, Moon MS. Squatting following total knee arthroplasty. Clin Orthop Relat Res. 1995;313:177–186.
Kim TK, Chang CB, Kang YG, Kim SJ, Seong SC. Causes and predictors of patient’s dissatisfaction after uncomplicated total knee arthroplasty. J Arthroplasty. 2009;24:263–271.
Kim YH, Choi YW, Kim JS. Simultaneous bilateral sequential total knee replacement is as safe as unilateral total knee replacement. J Bone Joint Surg Br. 2009;91:64–68.
Kim YH, Sohn KS, Kim JS. Range of motion of standard and high-flexion posterior stabilized total knee prostheses: a prospective, randomized study. J Bone Joint Surg Am. 2005;87:1470–1475.
Koh IJ, Kim TK, Chang CB, Cho HJ, In Y. Trends in use of total knee arthroplasty in Korea from 2001 to 2010. Clin Orthop Relat Res. 2012 Oct 4. [Epub ahead of print].
Lane GJ, Hozack WJ, Shah S, Rothman RH, Booth RE Jr, Eng K, Smith P. Simultaneous bilateral versus unilateral total knee arthroplasty: outcomes analysis. Clin Orthop Relat Res. 1997;345:106–112.
Liang K-Y, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22.
Lie SA, Engesaeter LB, Havelin LI, Gjessing HK, Vollset SE. Dependency issues in survival analyses of 55,782 primary hip replacements from 47,355 patients. Stat Med. 2004;23:3227–3240.
Lohmander LS, Gerhardsson de Verdier M, Rollof J, Nilsson PM, Engstrom G. Incidence of severe knee and hip osteoarthritis in relation to different measures of body mass: a population-based prospective cohort study. Ann Rheum Dis. 2009;68:490–496.
Lozano Calderon SA, Shen J, Doumato DF, Zelicof S. Functional outcomes in high-function-demand patients after total knee arthroplasty. Orthopedics. 2012;35:e681–690.
Mancuso CA, Ranawat CS, Esdaile JM, Johanson NA, Charlson ME. Indications for total hip and total knee arthroplasties: results of orthopaedic surveys. J Arthroplasty. 1996;11:34–46.
March LM, Cross M, Tribe KL, Lapsley HM, Courtenay BG, Cross MJ, Brooks PM, Cass C, Coolican M, Neil M, Pinczewski L, Quain S, Robertson F, Ruff S, Walter W, Zicat B; Arthritis C.O.S.T. Study Project Group. Two knees or not two knees? Patient costs and outcomes following bilateral and unilateral total knee joint replacement surgery for OA. Osteoarthritis Cartilage. 2004;12:400–408.
McMahon M, Block JA. The risk of contralateral total knee arthroplasty after knee replacement for osteoarthritis. J Rheumatol. 2003;30:1822–1824.
Memtsoudis SG, Ma Y, Gonzalez Della Valle A, Mazumdar M, Gaber-Baylis LK, MacKenzie CR, Sculco TP. Perioperative outcomes after unilateral and bilateral total knee arthroplasty. Anesthesiology. 2009;111:1206–1216.
Mont MA, Mitzner DL, Jones LC, Hungerford DS. History of the contralateral knee after primary knee arthroplasty for osteoarthritis. Clin Orthop Relat Res. 1995;321:145–150.
Park KK, Chang CB, Kang YG, Seong SC, Kim TK. Correlation of maximum flexion with clinical outcome after total knee replacement in Asian patients. J Bone Joint Surg Br. 2007;89:604–608.
Park MS, Kim SJ, Chung CY, Choi IH, Lee SH, Lee KM. Statistical consideration for bilateral cases in orthopaedic research. J Bone Joint Surg Am. 2010;92:1732–1737.
Poolman RW, Kerkhoffs GM, Struijs PA, Bhandari M, International Evidence-Based Orthopedic Surgery Working Group. Don’t be misled by the orthopedic literature: tips for critical appraisal. Acta Orthop. 2007;78:162–171.
Powell RS, Pulido P, Tuason MS, Colwell CW Jr, Ezzet KA. Bilateral vs unilateral total knee arthroplasty: a patient-based comparison of pain levels and recovery of ambulatory skills. J Arthroplasty. 2006;21:642–649.
Ranstam J. Problems in orthopedic research: dependent observations. Acta Orthop Scand. 2002;73:447–450.
Restrepo C, Parvizi J, Dietrich T, Einhorn TA. Safety of simultaneous bilateral total knee arthroplasty: a meta-analysis. J Bone Joint Surg Am. 2007;89:1220–1226.
Reuben JD, Meyers SJ, Cox DD, Elliott M, Watson M, Shim SD. Cost comparison between bilateral simultaneous, staged, and unilateral total joint arthroplasty. J Arthroplasty. 1998;13:172–179.
Ritter MA, Carr KD, Keating EM, Faris PM. Long-term outcomes of contralateral knees after unilateral total knee arthroplasty for osteoarthritis. J Arthroplasty. 1994;9:347–349.
Ritter MA, Harty LD, Davis KE, Meding JB, Berend M. Simultaneous bilateral, staged bilateral, and unilateral total knee arthroplasty: a survival analysis. J Bone Joint Surg Am. 2003;85:1532–1537.
Robertsson O, Ranstam J. No bias of ignored bilaterality when analysing the revision risk of knee prostheses: analysis of a population based sample of 44,590 patients with 55,298 knee prostheses from the national Swedish Knee Arthroplasty Register. BMC Musculoskelet Disord. 2003;4:1.
Schwarzer G, Schumacher M, Maurer TB, Ochsner PE. Statistical analysis of failure times in total joint replacement. J Clin Epidemiol. 2001;54:997–1003.
Shah K, Smith J, Jones B, Hullin M. Bilateral total knee replacement under a single anaesthetic, using a cementless implant is not unsafe. Knee Surg Sports Traumatol Arthrosc. 2007;15:269–275.
Shetty GM, Mullaji A, Bhayde S, Chandra Vadapalli R, Desai D. Simultaneous bilateral versus unilateral computer-assisted total knee arthroplasty: a prospective comparison of early postoperative pain and functional recovery. Knee. 2010;17:191–195.
Sofat R, Ramkumar U, Wellsted D, Parmar H. Is there a difference between the ability to kneel after unilateral and bilateral total knee replacement? Acta Orthop Belg. 2006;72:578–582.
Urban MK, Chisholm M, Wukovits B. Are postoperative complications more common with single-stage bilateral (SBTKR) than with unilateral knee arthroplasty: guidelines for patients scheduled for SBTKR. HSS J. 2006;2:78–82.
Vaidya SV, Patel MR, Panghate AN, Rathod PA. Total knee arthroplasty: limb length discrepancy and functional outcome. Indian J Orthop. 2010;44:300–307.
Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med Care. 1992;30:473–483.
Waters TS, Bentley G. Patellar resurfacing in total knee arthroplasty: a prospective, randomized study. J Bone Joint Surg Am. 2003;85:212–217.
Worland RL, Jessup DE, Clelland C. Simultaneous bilateral total knee replacement versus unilateral replacement. Am J Orthop (Belle Mead NJ). 1996;25:292–295.
Zeni JA Jr, Snyder-Mackler L. Clinical outcomes after simultaneous bilateral total knee arthroplasty: comparison to unilateral total knee arthroplasty and healthy controls. J Arthroplasty. 2010;25:541–546.
Zhang Y, Glynn RJ, Felson DT. Musculoskeletal disease research: should we analyze the joint or the person? J Rheumatol. 1996;23:1130–1134.
Zhang Y, Xu L, Nevitt MC, Aliabadi P, Yu W, Qin M, Lui LY, Felson DT. Comparison of the prevalence of knee osteoarthritis between the elderly Chinese population in Beijing and whites in the United States: The Beijing Osteoarthritis Study. Arthritis Rheum. 2001;44:2065–2071.
Acknowledgments
We thank Sung Ju Kim MS, PhD candidate (Department of Statistics, Korea University, Seoul, Korea), for consultations for this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
The institution of one or more of the authors (TKK) received funding from the clinical research fund of Seoul National University Bundang Hospital.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution has approved the human protocol for this Investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent was obtained.
This work was performed at the Joint Reconstruction Center, Seoul National University Bundang Hospital, Gyeonggi-do, Republic of Korea.
About this article
Cite this article
Na, Y.G., Kang, Y.G., Chang, M.J. et al. Must Bilaterality Be Considered In Statistical Analyses of Total Knee Arthroplasty?. Clin Orthop Relat Res 471, 1970–1981 (2013). https://doi.org/10.1007/s11999-013-2810-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-013-2810-4