Abstract
Background
Multilevel orthopaedic surgery may improve gait in Type IV hemiplegia, but it is not known if proximal femoral osteotomy combined with adductor release as part of multilevel surgery in patients with hip dysplasia improves hip development.
Questions/purposes
We asked whether varus derotational osteotomy of the proximal femur, combined with adductor release, influenced hip development in patients with Type IV hemiplegia having multilevel surgery.
Patients and Methods
We retrospectively reviewed 11 children and adolescents with Type IV hemiplegia who had a proximal femoral osteotomy due to unilateral hip displacement to correct gait dysfunction between 1999 and 2006. The mean age at the time of surgery was 11.1 years (range, 7 to 16 years). We obtained the Movement Analysis Profile and Gait Profile Score before and after surgery. We also measured the Migration Percentage of Reimers and applied the Melbourne Cerebral Palsy Hip Classification System (MCPHCS). The minimum followup was 2 years 3 months (mean, 6 years 6 months; range, 2 years 3 months to 10 years 8 months).
Results
The majority of gait parameters improved but hip development was not normalized. According to the MCPHCS at last followup, no hips were classified as Grade I, two hips were classified as Grade II, and the remainder were Grade III and IV.
Conclusions
Unilateral surgery including a proximal femoral osteotomy improved gait and walking ability in individuals with spastic hemiplegic cerebral palsy. However, hip dysplasia persists.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spastic hemiplegia (SH) is the most common type of cerebral palsy (CP) in large population-based studies [20]. Subjects with spastic hemiplegic CP have a high level of gross motor function, Level I or II according to the Gross Motor Function Classification System (GMFCS) [13, 20, 27]; that is, they are able to walk in the community without assistive devices, which reportedly protects against hip dislocation [19].
Gait patterns in subjects with SH have been classified into four groups by Winters, Gage, and Hicks (WGH) [39]. In Type IV hemiplegia, there is involvement at all three levels: the ankle, knee, and hip. At the hip level, there is increased flexion, adduction, and internal rotation [11, 33]. Clinically there is evidence of increased femoral neck anteversion and there may be associated hip dysplasia [32]. Although not all subjects with hemiplegia can be readily categorized using the WGH system and transitional types may occur, the reliability of the classification is good [9, 30]. Importantly, many clinicians believe the WGH classification provides a useful template on which to base treatment decisions [33].
In a population-based study of children with CP from our state, the prevalence of hip displacement defined as a migration percentage (MP) greater than 30% was 35% [35]. This was similar to the prevalence reported in other population-based studies based on CP registers [5, 17]. Two subjects with SH from this population-based cohort study had hip dysplasia and underwent reconstructive surgery for a prevalence rate of 2% of all individuals with SH at skeletal maturity. However, given that only 19 subjects had Type IV hemiplegia, the prevalence of hip dysplasia in Type IV hemiplegia is much higher (two of 19 [10.5%]) [10].
The treatment of hip displacement in SH is important because such individuals have a normal life expectancy and high demands in comparison to individuals with bilateral CP subtypes. Treatment options for the younger child with SH include injections of botulinum toxin A for spastic equinus and the provision of a suitable ankle-foot orthosis [1, 15]. The older child or adolescent with Type IV SH may benefit from unilateral multilevel surgery based on instrumented gait analysis [25]. We previously found unilateral multilevel surgery, including an external rotation osteotomy of the proximal femur, corrects both sagittal and transverse plane gait deviations, including pelvic retraction [8]. Whether these operations achieve the additional goal of normalizing gait or hip development is not clear. There are currently no studies that address this question in the literature. Hip displacement in hemiplegia is rare and may not be recognized until it becomes symptomatic in adult life [3, 16, 17, 19, 21, 35].
The questions addressed in this study were twofold: (1) does unilateral multilevel surgery improve gait? (2) Does unilateral multilevel surgery normalize hip development?
Patients and Methods
We retrospectively reviewed the records of all 16 children with Type IV hemiplegia who had unilateral multilevel surgery, including an external rotation osteotomy of the proximal femur between January 1999 and December 2006. Eight of the 11 patients have previously been reported in a different format not including Gait Profile Score (GPS), Movement Analysis Profile (MAP), or radiology [8]. The indications for surgery were: (1) deterioration in gait; (2) evidence of contractures and bony torsion on physical examination; and (3) radiographic evidence of hip dysplasia, MP > 30%. The contraindications for surgery were: (1) stable gait; (2) no fixed deformities; and (3) normal hip development. During this time, we performed this procedure on a total of 16 patients. For this study, we included patients with: (1) Type IV hemiplegia confirmed clinically and by instrumented gait analysis; (2) hip displacement with MP greater than 30%; (3) unilateral surgery, which included a proximal femoral osteotomy (PFO) explicitly intended to correct both hip dysplasia and gait dysfunction using tailored combinations of external rotation, varus, and extension; and (4) at least one postoperative gait study and clinical and radiographic followup of more than 2 years. Five children had the surgery but were excluded from the study because they had not had a preoperative gait analysis, leaving 11 children for review. There were six boys and five girls with a mean age of 11.1 ± 2.7 years (range, 7 to 16 years) at the time of surgery. Ten children were GMFCS Level II and one child was GMFCS Level III preoperatively. Four had previous surgical procedures mainly for equinus gait, and one had a PFO at other institutions (Table 1). The minimum followup was 2 years 3 months (mean, 6 years 6 months; range, 2 years 3 months to 10 years 8 months). No patients were lost to followup. No patients were recalled specifically for this study; all data were obtained from medical records and radiographs. This study was approved under the audit provisions of the institution’s Ethics in Human Research Committee, Number CA 29012. The study was performed according to the Declaration of Helsinki (World Medical Association).
Each patient had a comprehensive history, a standardized clinical examination, radiography of the pelvis [40], and examination under general anesthesia immediately before surgery to confirm the presence of fixed contractures [6].
All children had an instrumented three-dimensional gait analysis (3D gait analysis) preoperatively, at short-term (1.0 year postoperatively), and at midterm (6.4 years postoperatively) followup. The gait analysis was carried out using a 50-Hz six-camera Vicon 370 system (Oxford Metrics, Oxford, UK) and two force plates (Advanced Mechanical Technology Inc, Newton, MA). Reflective markers were applied to the bony landmarks of the lower limb using a standardized protocol. Euler angles and inverse dynamics were used to calculate kinematics and kinetics using the Vicon Clinical Manager (Oxford Metrics). Patients were asked to walk barefoot in their usual manner along a 10-m walkway. An experienced physical therapist (JR, PT) and biomechanical engineer (RB) were responsible for all data collection using standardized protocols and data entry.
The MAP and GPS have been developed to summarize the complex information arising from 3D gait analysis. The MAP quantifies the magnitude of an individual subject’s gait deviations, across nine individual kinematic variables, over the whole gait cycle [2]. The GPS is a summary statistic of gait, which quantifies the overall deviation of kinematic data relative to normative data [2]. All data were uploaded into GaitaBase, a web-based repository for gait data [36]. The MAP and GPS were calculated for all subjects. The median value of the GPS for healthy children is 5.2° and one SD is 1.3°. All children had a preoperative and short-term (1.0-year postoperative) 3D gait analysis.
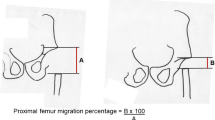
Standardized AP pelvic radiographs were analyzed by measuring the MP of Reimers [29], center-edge angle (CEA) of Wiberg [38], the acetabular angle of Sharp [34], and pelvic obliquity [37]. Hip morphology was classified using the Melbourne Cerebral Palsy Hip Classification System (MCPHCS) preoperatively, at baseline, 1 year after surgery, and at most recent followup in all subjects. The MCPHCS is a categorical classification of hip morphology based on both qualitative features as well as quantitative measures (MP) and has reasonable reliability [24].
The procedures selected for improving gait were based on clinical examination, 3D gait analysis, and examination under anesthesia following published guidelines [1, 12, 25, 26]. Procedures included lengthening of the gastrocsoleus for equinus gait (Botox® injections, gastrocnemius recession, or TAL based on Silfverskiöld test), hamstring lengthening with transfer for the rectus femoris to semitendinosus for flexed-stiff knee gait, and lengthening of the iliopsoas and hip adductors. Percutaneous adductor releases were performed and did not routinely include the iliopsoas lengthening. When indicated, iliopsoas lengthening was performed over the brim of the pelvis. Supramalleolar osteotomy of the tibia was performed in two children with malignant malalignment, ie, an external rotation osteotomy of the proximal femur was combined with an internal rotation osteotomy of the distal tibia. The indications for specific procedures were based on data gathered from kinematics, physical examination in the gait laboratory, and examination under anesthesia immediately before surgery [1, 6, 8].
An intertrochanteric osteotomy of the proximal femur was performed in all subjects and fixed with a 90° or 100° fixed-angle blade plate (Synthes®, Solothurn, Switzerland) [12, 18, 26]. The aim of surgery was to correct the mildly valgus neck shaft angle to a normal range between 120° and 130° by combining 5° to 15° of varus with 25° to 40° of derotation. All femoral osteotomies included external rotation based on clinical and CT measurement of anteversion, transverse plane hip kinematics, and evaluation of the AP hip radiograph [32]. Excessive varus was avoided to minimize abductor weakness and exacerbation of limb length discrepancy. When hip flexion contracture persisted at examination under anesthesia, despite previous or concurrent psoas lengthening, a small amount of extension (10°–20°) was built into the osteotomy by altering the inclination of the seating chisel.
Below-knee plaster casts were used for those subjects who required equinus surgery. Stable fixation was achieved and full weightbearing within 2 weeks of surgery was encouraged in all patients. Casts were removed 6 weeks after surgery and placed by custom-molded, articulated, ankle-foot orthoses. Assistive devices were provided until independent walking was regained. Postoperative physical therapy was provided at a frequency of two to three times per week for 3 to 6 months according to progress [1]. Postoperative progress was monitored by return visits to the gait laboratory for a physical examination and two-dimensional video recording of gait at 3, 6, and 9 months after surgery. At 12 months after surgery, a repeat 3D gait analysis was performed.
All data were normally distributed. We compared pre- and postoperative gait parameters using a paired t-test. We used SPSS® software (Version 15.0; SSPS Inc, Chicago, IL, USA). A power analysis was not carried out.
Results
We observed improvement of overall gait function. The GPS for the affected legs was 16° ± 2.8° and improved (p = 0.0002) by 6° to 11° ± 3° at the short-term followup 3D gait analysis. Kinematic parameters improved in seven of the nine MAP kinematic domains and the improvements were in the transverse plane for pelvic rotation, hip rotation, and foot progression (Fig. 1; Table 2).
Although a small improvement in MP was found at both short-term and medium-term followup, we observed no changes in the CEA of Wiberg or Sharp’s angle (Table 3). Pelvic obliquity averaged 4° ± 5° at baseline and tended to improve to 2° ± 3° at short-term followup with a slight relapse to 2° ± 4° at last followup. According to the MCPHCS (see Appendix 1), all hips on the uninvolved side and none of the hips on the involved side were Grade I at most recent followup. Only two hips on the hemiplegic side were classified as Grade II postoperatively and the rest were Grade III or IV. One hip that was managed by varus derotation osteotomy (VDRO) and a San Diego-type acetabuloplasty improved from Grade IV to Grade II (Fig. 2A–C) [23]. One patient with preoperative Grade II remained postoperatively in the same level (Table 3).
(A) These are the radiographs of a 16-year-old boy with a left Type IV hemiplegia and painful subluxation of his left hip, advanced femoral head deformity, and severe acetabular dysplasia. At presentation, his mobility had declined from Gross Motor Function Classification System (GMFCS) I to GMFCS III and the left hip was Grade IV according to the Melbourne Cerebral Palsy Hip Classification System (MCPHCS). (B) MRI of the left hip showing cartilage loss and femoral head deformity. (C) Eight-year followup after open reduction/adductor lengthening, proximal femoral osteotomy (varus, external rotation, and extension), and San Diego Type Pelvic Osteotomy. Pain was completely abolished and he regained independent walking, GMFCS Level II. (D) This three-dimensional CT reconstruction lateral view shows the extension component of the femoral osteotomy and good femoral head containment.
At most recent followup, none of the patients had hip pain on the hemiplegic side. Apart from implant removal, no additional surgeries were performed (Fig. 3A–B). There were no nonunions, delayed unions, or deep infections after VDRO. No patient required a blood transfusion. There were three superficial wound infections, one in an anterior knee incision for rectus femoris transfer and two in the popliteal fossa after hamstring lengthening. These resolved after administration of oral antibiotics.
(A) These are the radiographs of a 9-year-old boy with Type IV left hemiplegia 1 year after left proximal femoral osteotomy, adductor and psoas lengthening, and surgery for equinus deformity. The osteotomy has united and the femoral head is well contained with good acetabular coverage. (B) At skeletal maturity (after removal of the blade plate), Shenton’s arch is intact but the femoral head is deformed with a flattened area laterally and there is residual acetabular dysplasia. The left hip migration percentage was 42% and was Grade IV according to the Melbourne Cerebral Palsy Hip Classification System (MCPHCS).
Discussion
The literature suggests both single-level and multilevel surgery improve gait and function in spastic hemiplegia. Single-level surgery, for the management of equinus gait, reportedly improves gait in Type II hemiplegia [14]. In Type IV hemiplegia, several recent reports, using gait analysis, have reported improvement in sagittal and transverse plane gait parameters after unilateral, multilevel surgery [4, 8]. We asked whether: (1) unilateral multilevel surgery improves gait and (2) unilateral multilevel surgery normalizes hip development.
We caution readers of the limitations to our study. First, we had a small number of patients. This is a very small subset of patients that has not been previously reported. Our cohort was too small to permit analysis by age at surgery. Surgery at a younger age might run the risk of recurrent limb deformities and regression of the gait improvement component of the surgery. However, surgery at a younger age might encourage more normal acetabular development and provide additional time for monitoring of residual acetabular dysplasia with increased opportunities for pelvic osteotomy before skeletal maturity. However, all included patients were followed with a consistent protocol. Second, we lacked a control group, but MAP and GPS quantify the deviation of kinematic data relative to normative data.
We demonstrated overall improvement in gait using a summary statistic of gait, the GPS. In addition, the use of the MAP shows which kinematic parameters have improved and by how much. From this, some inferences can be made as to which procedures may have been most effective. The focus of our surgery was primarily the correction of gait dysfunction. At the time of presentation, walking, not asymptomatic hip dysplasia, was the patient’s and parents’ concern. However, we noted mild hip dysplasia in all of our patients and modified the gait correction surgery in an attempt to simultaneously improve gait and correct hip displacement. Although we observed an improvement in the MP, we found no changes in the indices of acetabular dysplasia, the CEA of Wiberg, or acetabular angle of Sharp. MP changes are only relevant for the individual and the mean values for a cohort could only indicate a trend. In addition, none of the hips on the affected side were rated as normal on the Melbourne Cerebral Palsy Hip Scale. The hip that improved most was the only one to have a concomitant pelvic osteotomy. Factors that may have contributed to persisting dysplasia include muscle imbalance, pelvic obliquity, and older age at index surgery. Paradoxically, the pelvic obliquity was always high on the affected side despite some degree of shortening of the affected limb. We believe the pelvic obliquity may be centrally or neurologically mediated and this may explain the lack of response to adductor lengthening. We are unsure of the importance of the residual dysplasia in this population. Patients with hemiplegia have a normal life expectancy and relatively high levels of physical functioning. Longer-term followup will be required to determine if their hip dysplasia will become symptomatic.
Hip dysplasia is common in CP and the prevalence is related to walking ability as determined by the GMFCS but not to movement disorder type [5, 17, 35]. The effects of hip displacement are also related to GMFCS level. The high-risk groups are nonambulatory children with spastic quadriplegia, GMFCS IV and V [5, 17, 35]. In these patients, pain and fixed deformities that interfere with sitting are the most important issues. Although hip displacement is relatively rare in SH, the effects may be devastating with early onset of pain, gait difficulties, and loss of walking ability (Fig. 2A–D). As a result of most patients with hemiplegia being at low risk for hip dysplasia, routine screening radiographs are not typically performed. Therefore, the majority of patients did not have initial radiographs until referred for gait analysis. The pathogenesis of hip displacement is different in SH compared with other CP subtypes. Hip displacement develops quite late and may progress slowly and silently until the pubertal growth spurt. Presentation during the pubertal growth spurt may include sudden onset of pain, deterioration in gait, and the need for an assistive device. Increased pelvic obliquity with increased apparent leg length discrepancy may also be features (Fig. 2A–D). We noted a consistent pattern with small leg length discrepancy (LLD) smaller than the apparent LLD and mild pelvic obliquity of 3° to 14° on kinematics (affected side being up and the unaffected side being down). For these reasons, systematic hip surveillance with clinical and radiographic examination at regular intervals is supported in the recent literature [7, 16]. The authors would recommend an initial AP radiograph of the pelvis after the initial diagnosis of Type 4 hemiplegia is made with repeated radiographs every 12 to 24 months until skeletal maturity or until consecutive radiographs have demonstrated normal hip development over a minimum of 2 years.
Although our patients are currently asymptomatic, we radiographically documented substantial acetabular dysplasia in an otherwise high-functioning group of young adolescents. We believe more aggressive management of acetabular dysplasia should be considered in patients with Type IV hemiplegia and hip displacement. Unilateral VDRO, even when combined with adductor and psoas release, improves the migration percentage in these patients but does not result in predictable or complete resolution of acetabular dysplasia. In retrospect, our criteria for acetabular reconstruction, based on MP > 40%, were too lax and this threshold is too high for this CP subtype. However, we believe this threshold is too high, especially in older children, and it may be more appropriate to consider a much lower threshold for pelvic osteotomy, an MP of 20%. Although MP is the most widely used radiographic in CP hip displacement in general, other factors including the acetabular index and the development of the acetabular sourcil should be considered.
Although there is extensive literature on the management of hip displacement in bilateral CP, spastic diplegia, and spastic quadriplegia, there is very little information on the management of hemiplegic hip disease [19, 21, 22, 28]. We presumed correction of hip adduction and flexion contractures combined with a VDRO and appropriate muscle tendon surgery at the knee and ankle would be effective in correcting both the hip displacement and the gait dysfunction in Type IV SH. Fluoroscopic screening before VDRO showed improved femoral head cover and a reduction in MP in all hips. However, although the surgery improved gait, the effects on subsequent hip development were disappointing with a high incidence of residual dysplasia. The VDRO only slightly improved the radiographic parameters (CEA and MP) and did not improve the acetabular angle. The combination of mild pelvic obliquity, which was always high on the affected side, combined with persisting muscle imbalance may have contributed to the persisting hip dysplasia. The only hip that improved by two grades had a concomitant pelvic osteotomy (Fig. 2A–D). Several authors suggest more aggressive management of acetabular dysplasia should be recommended in hemiplegic hip disease [22, 23]. Even mild pelvic obliquity appears to contribute to failure of acetabular development at skeletal maturity (Fig. 3A–B) [3].
The MCPHCS was introduced to describe hip disease at skeletal maturity across the entire spectrum of CP [24, 31]. We found it a useful tool to discriminate and describe normal hip development on the uninvolved side in individuals with SH as well as a broad spectrum of dysplasia on the affected side [24, 31]. Likewise, the GPS was responsive for detecting clinically meaningful improvements in gait and, in conjunction with the MAP, the kinematic domains where we observed most improvements [2]. The improvements in the sagittal plane domains of the MAP were smaller and insignificant because the ankle and knee gait dysfunction was relatively small because of previous surgery, Botox®, and bracing. We did observe improvements in the transverse plane, secondary to the beneficial effects of VDRO on gait, in combination with additional muscle tendon lengthenings and tendon transfers, when indicated [4, 8].
In conclusion, unilateral orthopaedic surgery, which includes a PFO, is effective in improving gait and walking ability in individuals with spastic hemiplegic CP. However, hip dysplasia persists and although none of our patients were currently symptomatic, we are concerned about the longevity of these hips given normal life expectancy and high levels of function.
References
Bache CE, Selber P, Graham HK. Mini-Symposium: Cerebral palsy: the management of spastic diplegia. Curr Orthop. 2003;17:88–104.
Baker R, McGinley JL, Schwartz MH, Beynon S, Rozumalski, Graham HK, Tirosh O. The Gait Profile Score and Movement Analysis Profile. Gait Posture. 2009;30:265–269.
Black BE, Hildebrand R, Sponseller PD, Griffin PP. Hip dysplasia in spastic cerebral palsy. Contemp Orthop. 1994;29:101–108.
Chung CY, Lee SH, Choi IH, Cho T-J, Yoo WJ, Park MS. Residual pelvic rotation after single-event-multilevel surgery in spastic hemiplegia. J Bone Joint Surg Br. 2008;90:1234–1238.
Connelly A, Flett P, Graham HK, Oates J. Hip surveillance in Tasmanian children with cerebral palsy. J Paediatr Child Health. 2009;45:437–443.
Davids JR, Ounpuu S, DeLuca PA, Davis RB. Optimization of walking ability of children with cerebral palsy. Inst Course Lect. 2004;53:511–522.
Dobson F, Boyd RN, Parrott J, Nattrass GR, Graham HK. Hip surveillance in children with cerebral palsy: impact on the surgical management of spastic hip disease. J Bone Joint Surg Br. 2002;84:720–726.
Dobson F, Graham HK, Baker R, Morris MJ. Multilevel orthopaedic surgery in group IV spastic hemiplegia. J Bone Joint Surg Br. 2005;87:548–555.
Dobson F, Morris ME, Baker R, Graham HK. Clinician agreement on gait pattern ratings in children with spastic hemiplegia. Dev Med Child Neurol. 2006;48:429–435.
Dobson F, Morris ME, Baker R, Graham HK. Unilateral cerebral palsy: a population-based study of gait and motor function. Dev Med Child Neurol. 2011;53:429–435.
Dobson F, Morris ME, Baker R, Wolfe R, Graham HK. Gait classification in children with cerebral palsy: a systematic review. Gait Posture. 2007;25:140–152.
Gage JR. Orthopaedic treatment of long bone torsions. In: Gage JR, Schwartz MH, Koop S, Novacheck TF, eds. The Identification and Treatment of Gait Problems in Cerebral Palsy. 2nd ed. London: MacKeith Press; 2009:473–491.
Gorter JW, Rosenbaum PL, Hanna SE, Palisano RJ, Bartlett DJ, Russell DJ, Walter S, Raina P, Galuppi BE, Wood E. Limb distribution, motor impairment, and functional classification of cerebral palsy. Dev Med Child Neurol. 2004;46:461–467.
Graham HK, Fixsen JA. Lengthening of the calcaneal tendon in spastic hemiplegia by the White slide technique. A long-term review. J Bone Joint Surg Br. 1988;70:472–475.
Graham HK, Selber P. Musculoskeletal aspects of cerebral palsy. J Bone Joint Surg Br. 2003;85:157–166.
Hagglund G, Andersson S, Duppe H, Lauge-Pedersen H, Nordmark E, Westbom L. Prevention of dislocation of the hip in children with cerebral palsy: the first ten years of a population-based programme. J Bone Joint Surg Br. 2005;87:95–101.
Hagglund G, Lauge-Pedersen H, Wagner P. Characteristics of children with hip displacement in cerebral palsy. BMC Musculoskelet Disord. 2007;8:101–107.
Hau R, Dickens DRV, Nattrass GR, O’Sullivan M, Torode IP, Graham HK. Which implant for proximal femoral osteotomy in children? A comparison of the AO (ASIF) 90° fixed-angle blade plate and the Richards intermediate hip screw. J Pediatr Orthop. 2000;20:336–343.
Howard CB, Mc Kibbin B, Williams LA, Mackie I. Factors affecting the incidence of hip dislocation in cerebral palsy. J Bone Joint Surg Br. 1985;67:530–532.
Howard J, Soo B, Graham HK, Boyd R, Reid S, Lanigan A, Wolfe R, Reddihough DS. Cerebral palsy in Victoria: motor types, topography and gross motor function. J Pediatr Child Health. 2005;41:479–483.
Miller F, Dias RC, Dabney KW, Lipton GE, Triana M. Soft-tissue release for spastic hip subluxation in cerebral palsy. J Pediatr Orthop. 1997;17:571–584.
Miller F, Girardi H, Lipton G, Ponzio R, Klaumann M, Dabney KW. Reconstruction of the dysplastic spastic hip with peri-ilial pelvic and femoral osteotomy followed by immediate mobilization. J Pediatr Orthop. 1997;17:592–602.
Mubarak SJ, Valencia FG, Wenger DR. One-stage correction of spastic dislocated hip. J Bone Joint Surg Am. 1992;74:1347–1357.
Murnaghan ML, Simpson P, Robin J, Shore BJ, Selber P, Graham HK. The cerebral palsy hip classification is reliable. J Bone Joint Surg Br. 2010;92:436–441.
Novacheck T. Management options for gait abnormalities. In: Neville B, Goodman R, eds. Clinics in Dev Med No 150. Congenital Hemiplegia. London: MacKeith Press; 2000:98–112.
Novacheck TF. Orthopaedic treatment of muscle contractures. In: Gage JR, Schwartz MH, Koop S, Novacheck TF, eds. The Identification and Treatment of Gait Problems in Cerebral Palsy. 2nd ed. London: MacKeith Press; 2009:445–472.
Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997;39:214–223.
Presedo A, Chang-Wug O, Dabney K, Miller F. Soft-tissue releases to treat spastic hip subluxation in children with cerebral palsy. J Bone Joint Surg Am. 2005;87:832–841.
Reimers J. The stability of hip in children. A radiological study of the results of muscle surgery in cerebral palsy. Acta Orthop Scand Suppl. 1980;184:1–100.
Riad J, Haglund-Akerlind Y, Miller F. Classification of spastic hemiplegic cerebral palsy in children. J Pediatr Orthop. 2007;27:758–764.
Robin J, Graham HK, Baker R, Selber P, Simpson P, Symons S, Thomason P. A classification system for hip disease in cerebral palsy. Dev Med Child Neurol. 2009;51:183–192.
Robin J, Graham HK, Selber P, Dobson F, Smith K, Baker R. Proximal femoral geometry in cerebral palsy. A population-based cross-sectional study. J Bone Joint Surg Br. 2008;90:1372–1379.
Rodda J, Graham HK. Classification of gait patterns in spastic hemiplegia and spastic diplegia: a basis for a management algorithm. Eur J Neurol. 2001;8(Suppl 5):S98–108.
Sharp IK. Acetabular dysplasia. The acetabular angle. J Bone Joint Surg Br. 1961;43:13–25.
Soo B, Howard J, Boyd RN, Reid S, Lanigan A, Wolfe R, Reddihough D, Graham HK. Hip displacement in cerebral palsy: a population based study of incidence in relation to motor type, topographical distribution and gross motor function. J Bone Joint Surg Am. 2006;88:121–129.
Tirosh O, Baker R. Gaitabase: new approach to clinical gait analysis. Gait Posture. 2006;24:S52–S53.
Tönnis D. General radiography of the hip joint. In: Tönnis D, ed. Congenital Dysplasia and Dislocation of the Hip in Children and Adults. Berlin: Springer-Verlag; 1987:100–138.
Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint. Acta Chir Scand Suppl. 1939;58:13–25.
Winters TF, Gage JR, Hicks R. Gait patterns in spastic hemiplegia in children and young adults. J Bone Joint Surg Am. 1987;69:437–441.
Wynter M, Gibson N, Kentish M, Love SC, Thomason P, Graham HK. Consensus Statement on Hip Surveillance for Children with Cerebral Palsy. Australian Standards of Care. Available at: http://www.ausacpdm.org.au/activities/hip-surveillance. Accessed April 8, 2011.
Acknowledgments
We thank Mary Sheedy for the help in the preparing and editing the manuscript and the staff of the Hugh Williamson Gait Laboratory for the kinematic data, especially Jill Rodda [JR] and Pam Thomason [PT].
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at The Hugh Williamson Gait Laboratory.
Appendix 1
Appendix 1

About this article
Cite this article
Rutz, E., Passmore, E., Baker, R. et al. Multilevel Surgery Improves Gait in Spastic Hemiplegia But Does Not Resolve Hip Dysplasia. Clin Orthop Relat Res 470, 1294–1302 (2012). https://doi.org/10.1007/s11999-011-2079-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-011-2079-4