Abstract
Background
Many surgeons recommend pelvic osteotomy to treat symptomatic hip dysplasia in younger patients. We previously reported a cohort of patients at 10 and 15 years followup in which 65% of the patients showed no progression of osteoarthritis (OA).
Questions/purposes
The purposes of this study were to determine whether the triple osteotomy can provide (1) continuing pain relief and (2) function; and to determine the (3) incidence of OA and (4) number of patients undergoing THAs 23 years or more after triple osteotomy.
Methods
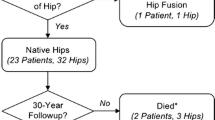
Between 1980 and 1987, 51 pelvic osteotomies were performed in 43 patients (38 females and five males; mean age, 28 years; range, 14–48 years). Followup was obtained for 40 patients (49 of 51 hips; 96%). Clinical evaluation, including pain, mobility, and ROM, was graded according to the subgroups of the modified scoring system of Merle d’Aubigné and Postel. The minimum followup was 23 years (mean, 25 years; range, 23–29 years).
Results
The mean VAS pain score increased from 27 mm to 31 mm at the last followup, but remained substantially lower than before surgery. The mean Merle d’Aubigné-Postel score improved from 13 preoperatively to 15 at a mean of 10 years followup but at last followup, the mean score had decreased to 14, thereby showing a trend to diminish. At 15 years followup, 20 patients showed signs of OA. At 25 years followup, 18 of 33 patients without THAs showed signs of OA (55%). Six patients (six hips) had undergone THAs at 15 years, increasing to 15 patients (16 hips) at 25 years.
Conclusion
While the triple osteotomy for symptomatic developmental dysplasia of the hip in young adults provides substantial pain relief and restores function in most patients, these results deteriorate over decades owing to the development of OA. Even in joints without preoperative OA, a THA cannot always be avoided. The triple osteotomy does not normalize the joint and the incidence of THA in this group of patients (32%) is much higher than in the general population.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In The Netherlands, the incidence of developmental hip dysplasia is estimated at 3.7% and the incidence of hip dislocation at 0.4% [1]. Symptomatic hip dysplasia in adolescence and in young adults can be treated by an osteotomy to reorient the acetabulum. The osteotomies most frequently used in this age group are the triple osteotomy [21] and the Bernese periacetabular osteotomy [9, 13]. Other treatment modalities are the Chiari osteotomy and shelfplasty [18]. We have used a triple osteotomy since 1980 and followup studies of 10 and 15 years have been published [5, 11, 22]. These reports show a Merle d’Aubigné-Postel score of 15 to 18 points (“good” to “excellent”) in 56% of all patients with little progression of osteoarthritis (OA) and only six patients (12%) underwent a THA by 15 years followup. At 15 years followup, 19 patients (21 hips) showed no signs of OA (compared with 34 patients [41 hips] preoperatively), 17 patients (18 hips) showed Grade 1 OA (compared with eight patients [10 hips] preoperatively), and only two patients (two hips) showed Grade 2 OA (no patients preoperatively).
Dungl et al. [7] described Merle d’Aubigné-Postel scores of 18 in 40% and of 15 to 17 in 32% of patients with 146 triple osteotomies. However, their study included patients with avascular necrosis of the femoral head and with dysplastic hips. Janssen et al. [10] described a population of 32 patients with Grade 2 OA [21] secondary to developmental dysplasia treated with triple osteotomies. At a mean followup of 11.5 years, they found a survival rate of 85.3% and an improvement of the Harris hip score. Despite these studies, it remains unclear whether the triple osteotomy provides longer-term pain relief and maintenance of function and to what degree it delays onset of OA.
The purposes of this study were to determine whether the triple osteotomy can provide (1) continuing pain relief and (2) function; and to determine the (3) incidence of OA and (4) number of patients undergoing THAs 23 years or more after triple osteotomy.
Patients and Methods
Between 1980 and 1987, we treated 43 patients with 51 pelvic osteotomies. There were 38 females and five males with a mean age of 28 years (range, 14–48 years) at the time of surgery. Four patients had been treated for dislocation of the hip in infancy and six had undergone surgery to correct the hip dysplasia: four had a previous intertrochanteric osteotomy, one had a Chiari osteotomy, and one had a shelf procedure. The indication for triple osteotomy was symptomatic hip dysplasia with a spherical femoral head and without major damage to the cartilage (OA Grade 0 to 1 according to Tönnis [19]; Fig. 1). Two patients were lost to followup. One patient was followed up at a different hospital because of personal reasons. This patient did not want to participate in clinical followup, but gave permission for radiologic followup. This resulted in a clinical followup of 39 of 43 patients (48 of 51 hips) and a radiographic followup of 40 of 43 patients (49 of 51 hips) who had undergone osteotomies. The minimum followup was 23 years (mean, 25 years; range, 23–29 years). Regional ethical committee permission was granted for this study before the start of the study in 1980.
Examples of the radiographs of two patients with symptomatic hip dysplasia with a spherical femoral head and without radiologic signs of degeneration or OA are shown. (A) The patient’s preoperative radiograph is shown. The patient’s postoperative results after (B) 1, (C) 19, and (D) 25 years show no progression of OA. (E) The preoperative radiograph for the second patient is shown. The patient’s postoperative results after (F) 1, (G) 15, and (H) 25 years show a marked increase in OA between 15 and 25 years.
The operative technique has been described previously [5, 11]. The operation began with a separate posterior approach for the osteotomy of the ischium. Passing bluntly through the gluteus maximus muscle at the medial border, the external rotators of the hip were exposed as they crossed the ischium. The fibers of the external rotators were split in the direction of their fibers to expose the posterior aspect of the ischium. An oblique osteotomy of the ischium was performed using a 2.5-cm wide osteotome. We performed the osteotomy of the pubis and ilium through a partial ilioinguinal approach using the lateral window. The inguinal ligament and sartorius muscle were reflected medially off the anterior superior iliac spine followed by subperiosteal exposure of the inside of the iliac wing and the pubis. The iliopsoas muscle was elevated and the iliopectineal fascia then was elevated off the iliopectineal eminence. We then made the pubic osteotomy with a wide osteotome in the sagittal plane just medial to the iliopectineal eminence. The lateral and medial pelvic muscles were reflected subperiosteally off the iliac wing to gain access to the sciatic notch. The iliac osteotomy was started just above the anterior inferior iliac spine and the origin of the rectus femoris muscle and was aimed at the notch. After completion of the three osteotomies, we reoriented the acetabular fragment and evaluated the position under radiographic control. The degree of correction was evaluated by estimating the center-edge angle and acetabular index on the image intensifier. Using an image intensifier, however, has the limitation that it offers a posteroanterior view centered on the hip with the pubic symphysis and the sacroiliac joint just visible, instead of an AP pelvic radiograph centered on the midline of the pelvis, which gives a little different projection. In the early 1980s there was limited awareness regarding how to estimate the correction. We now know that the image intensifier PA image often gives an underestimation of the degree of correction when compared with the standard AP pelvic radiograph. Next to the image intensifier, the hip rotations are used as an evaluation of correction and to make sure there is no anterior impingement which may be a sign of overcorrection or retroversion, which is a complication in triple osteotomies. Postoperatively, the correction was checked by a standard AP pelvic radiograph. The pelvis was fixed in place by a bone wedge and one or two screws. Preoperatively, the average center-edge angle was 9° (range, −12° to 28°) and postoperatively, the average center-edge angle was 28° (range, 6°–47°).
All patients were invited to the clinic specifically for this study to obtain followup physical examinations and radiographic assessments. Clinical evaluation, including pain, mobility, and ROM, was graded according to subgroups of the modified scoring system of Merle d’Aubigné and Postel [3] and a VAS was used to measure pain. All clinical and radiographic evaluations were performed by one of the authors (RAvS) who was not involved in the original treatment of patients. One patient was followed up at a different hospital because of personal reasons. This patient declined participation in the clinical followups but gave permission for radiographic followup. Potential complications were classified according to the classification system for surgical complications by Dindo et al. [6]. The data regarding THA and the timing of THA were extracted from the patients’ files.
The lateral center-edge angle [23], anterior center-edge angle, and acetabular index were measured by one of us (MdK) [4, 19, 22] at the time of the earlier studies. Broughton et al. [2] described the acetabular index and the center-edge angle to be the most reliable methods to measure the degree of dysplasia. For the acetabular index, they described a 95% prediction interval of ± 6.1 for intraobserver variability and ± 5.5 for interobserver variability. For the center-edge angle, they described a 95% prediction interval of ± 9.3 for intraobserver variability and ± 9.1 for the interobserver variability [2].
The mean VAS scores were compared using a Wilcoxon signed ranks test using SPSS 20 (SPSS Inc, Chicago, IL, USA), since they were not normally distributed. We compared the preoperative with final followup Merle d’Aubigné-Postel scores using a paired samples t-test using SPSS 20. The survival analysis was performed by means of a Kaplan Meier analysis in SPSS.
Results
The mean VAS pain score was 55 mm preoperatively (range, 0–80 mm) and improved to 27 mm immediately postoperatively (range, 0–100 mm) (p < 0.001). The pain score deteriorated (p = 0.352) to 31 mm at the last followup (range, 0–75 mm) and remained lower (p < 0.001) than preoperatively.
The mean Merle d’Aubigné-Postel score for patients without THAs improved from 13 preoperatively to 15 at a mean of 10 years followup, but at last followup, the mean score had decreased to 14, thereby showing a trend (p = 0.23) to diminish. However, the mean scores remained higher (p = 0.002) than preoperatively (Table 1). Preoperatively, 34 of 43 patients showed no signs of OA. At 15 years followup, 19 patients showed signs of OA. At 25 years followup, 16 of 30 patients) without THAs showed signs of OA (53%) (Table 2).
At 20 years the survival was 76% using THA as an end point. After 20 years, however, there was a rapid increase in patients requiring THAs (Fig. 2). At 23 to 29 years followup, THAs had been performed in 16 hips and seven of 30 patients without THAs showed a higher grade of OA (Table 2). Of the patients who underwent THA, five had a preoperative score greater than 15, and the others had a score less than 15. Seven patients (eight hips) had a preoperative Merle d’Aubigné-Postel score less than 14, three patients had a score less than 12, and all had a Merle d’Aubigné-Postel score less than 15 at the 15-year followup. None of the patients who had a THA had a Merle d’Aubigné-Postel score greater than 15 at 15 years followup, although five had a preoperative score greater than 15. Of the 16 THAs, four were performed in other hospitals. All operations were uneventful and there were no additional complications or difficulties with the operative technique (Fig. 3).
Preoperatively the mean center-edge angle was 9° with a SEM of 1.6° [11, 12]. Major complications included transient sciatic nerve palsy (Grade I complication [6]) in one patient and palsy of the lateral femoral cutaneous nerve in nine patients (Grade I). There were three nonunions of the ischium and one of the pubic bone, all of which appeared to be asymptomatic (Grade I). Three patients had a wound infection postoperatively and were treated with antibiotics after which all achieved uneventful healing (Grade II). There was no evidence of persisting infections at the last followup. In 36 cases, screws were removed because of pain at the insertion site on the iliac crest.
Discussion
Despite several studies [7, 10, 20], it remains unclear whether the triple osteotomy provides longer-term pain relief and maintenance of function and to what degree it delays onset of OA. We present a series of patients with a followup of 96% at 23 to 29 years after pelvic osteotomies. This study is a followup study after previous reports on the 8- to 15-year follow-up and a 15-year followup of triple osteotomies of the pelvis [5, 22]. The purposes of this study therefore were to determine whether the triple osteotomy can provide (1) continuing pain relief and (2) function; and to determine the (3) incidence of OA and (4) number of patients undergoing THA 23 years or more after triple osteotomy.
There are some limitations to our study. First, this is a relatively small population. However, compared with the available literature, it is the only population of this size with a homogenous series of patients (spherical femoral heads, congruent joints, limited or no OA), followed prospectively with 96% followup. Second, we did not analyze confounding factors and cannot know how they influence the VAS or Merle d’Aubigné-Postel score. However, because this is a series of 51 hips, dividing this population into smaller subgroups to evaluate certain confounding factors (such as age, gender, obesity, smoking, physical exercise) would lead to over-stratification, making it impossible to distinguish any reliable confounders. In addition, owing to the descriptive nature of the study design we decided not to include an analysis for confounding factors. Third, without a control group without surgery it is not possible to determine the natural course and subsequently impossible to determine the long-term effect of surgery. Developmental dysplasia of the hip occurs in one to two per 1000 births and, when left uncorrected, it may be associated with high long-term morbidity. Furnes et al. [8] reported an incidence of 9% dysplastic hips in patients having THAs and stated that as much as 1/3 of all patients undergoing THA before 65 years of age experience the consequences of developmental hip dysplasia. Surgical correction of residual dysplasia in adults can relieve pain and substantially improve function, but it has not been proven that it can improve the natural history of developmental dysplasia of the hip [7, 10, 12, 14, 17].
The mean VAS score deteriorated slightly with time, but remained higher than preoperatively. Kotz et al. [12] reported patients after Chiari osteotomy with a mean VAS score of 25 mm at an average followup of 32 years, which is comparable to the VAS score for our population.
Comparing the Merle d’Aubigné-Postel scores at 15 years followup with the results at 25 years followup, the following pattern was observed. Up to 15 years postoperatively, the clinical scores showed major improvement compared with preoperatively. However, at 25 years, the clinical scores showed deterioration of 1 point. Nevertheless, the results are better than the Merle d’Aubigné-Postel scores preoperatively. Nakamura et al. [14] described a population of 145 rotational osteotomies of the acetabulum at a mean followup of 13 years, and in this population, the clinical outcome based on the Merle d’Aubigné-Postel score was 15 to 18 in 90 (80%) of the 112 hips which had Stage I or II OA preoperatively and 15 to 18 for nine of the 33 hips which had Stage III or IV OA preoperatively. This shows that when degenerative changes have developed preoperatively, the clinical outcome of acetabular osteotomies and the postoperative Merle d’Aubigné-Postel score can be expected to be lower.
In this population, the development of symptomatic OA did occur with time and could not be avoided by performing triple osteotomies. At most, it was delayed. This also is reported in the literature [7, 10, 12–14, 17]. In the population described by Janssen et al. [10], six radiographs (18.8%) showed radiographic signs of progression of OA at the final followup. Nakamura et al. [14] also described an increase in OA with time, graded according to the Japanese Orthopaedic Association [15, 16]. Of the 112 hips with Grade I or II OA preoperatively, only 70% (79 hips) still had Grade I or II OA at the last followup, and the rest had progressive degenerative changes. The reason for this progression of OA despite an osteotomy may be that the acetabulum is reoriented to a more favorable position, reducing the shear forces in the joint by making the weightbearing zone more horizontal, but it is not enlarged and not normalized; it remains a shallow and suboptimal joint.
The rate of conversion to THA increased in this population after 15 years. Comparing the conversion rate of 31% for this population with the rates reported in the literature remains difficult. Most of the available studies describing results greater than 10 years describe different operative techniques [7, 10, 14, 17] with much lower followup rates (range, 15%–98%). Kotz et al. [12] reported the long-term followup for the Chiari osteotomy and showed a conversion rate of 40% to THA at an average followup of 32 years. However, their population had a followup of only 15% because for most of the patients, the records could not be identified. This makes their study of limited value and difficult to compare with ours because of the different operative technique and because the preoperative degree of OA generally was greater in their population [12]. A major disadvantage of the Chiari osteotomy, compared with the triple osteotomy, is the difficulty it poses when performing a THA. A THA after a triple osteotomy is notably easier than after a Chiari osteotomy. Matheney et al. [13] reported 109 patients (135 hips) treated with a Bernese periacetabular osteotomy. At an average followup of 9 years, 17 hips were converted to THA. However, the preoperative radiographs showed a higher rate of patients with OA than in our population, thus making direct comparison difficult (Table 3).
We report a series of patients with 96% followup at 25 years after triple osteotomy of the pelvis for developmental dysplasia of the hip. In this population of selected patients with a congruent joint and limited preoperative OA (Grades 0–1), the triple osteotomy can provide substantial pain reduction and improved function at 25 years followup. There appeared to be a substantial increase in OA between 15 and 25 years after triple osteotomy and the subsequent number of patients requiring THAs increased to 32%. A triple osteotomy can improve a patient’s symptoms, but it cannot normalize the joint and prevent OA from developing with time. If THA is required, it can be performed uneventfully.
References
Boere-Boonekamp MM, Kerkhoff TH, Schuil PB, Zielhuis GA. Early detection of developmental dysplasia of the hip in The Netherlands: the validity of a standardized assessment protocol in infants. Am J Public Health. 1998;88:285–288.
Broughton NS, Brougham DI, Cole WG, Menelaus MB. Reliability of radiographic measurements in the assessment of the child’s hip. J Bone Joint Surg Br. 1989;71:6–8.
d’Aubigné RM, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am. 1954;36:451–475.
de Kleuver M, Kapitein PJ, Kooijman MA, van Limbeek J, Pavlov PW, Veth RP. Acetabular coverage of the femoral head after triple pelvic osteotomy: no relation to outcome in 51 hips followed for 8–15 years. Acta Orthop Scand. 1999;70:583–588.
de Kleuver M, Kooijman MA, Pavlov PW, Veth RP. Triple osteotomy of the pelvis for acetabular dysplasia: results at 8 to 15 years. J Bone Joint Surg Br. 1997;79:225–229.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications; a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213.
Dungl P, Rejholec M, Chomiak J, Grill F. The role of triple pelvic osteotomy in therapy of residual hip dysplasia and sequel of AVN: long-term experience. Hip Int. 2007;17(suppl 5):S51–S64.
Furnes O, Lie SA, Espehaug B, Vollset SE, Engesaeter LB, Havelin LI. Hip disease and the prognosis of total hip replacements: a review of 53,698 primary total hip replacements reported to the Norwegian Arthroplasty Register 1987–99. J Bone Joint Surg Br. 2001;83:579–586.
Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias: technique and preliminary results. 1988. Clin Orthop Relat Res. 2004;418:3–8.
Janssen D, Kalchschmidt K, Katthagen BD. Triple pelvic osteotomy as treatment for osteoarthritis secondary to developmental dysplasia of the hip. Int Orthop. 2009;33:1555–1559.
Kooijman MA, Pavlov PW. Triple osteotomy of the pelvis: a review of 51 cases. Clin Orthop Relat Res. 1990;255:133–137.
Kotz R, Chiari C, Hofstaetter JG, Lunzer A, Peloschek P. Long-term experience with Chiari’s osteotomy. Clin Orthop Relat Res. 2009;467:2215–2220.
Matheney T, Kim YJ, Zurakowski D, Matero C, Millis M. Intermediate to long-term results following the Bernese periacetabular osteotomy and predictors of clinical outcome. J Bone Joint Surg Am. 2009;91:2113–2123.
Nakamura S, Ninomiya S, Takatori Y, Morimoto S, Umeyama T. Long-term outcome of rotational acetabular osteotomy: 145 hips followed for 10–23 years. Acta Orthop Scand. 1998;69:259–265.
Ninomiya S. Rotational acetabular osteotomy for the severely dysplastic hip in the adolescent and adult. Clin Orthop Relat Res. 1989;247:127–137.
Shindo H, Igarashi H, Taneda H, Azuma H. Rotational acetabular osteotomy for severe dysplasia of the hip with a false acetabulum. J Bone Joint Surg Br. 1996;78:871–877.
Siebenrock KA, Scholl E, Lottenbach M, Ganz R. Bernese periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:9–20.
Staheli LT, Chew DE. Slotted acetabular augmentation in childhood and adolescence. J Pediatr Orthop. 1992;12:569–580.
Tönnis D. Congenital Dysplasia and Dislocation of the Hip in Children and Adults. Berlin, Germany: Springer-Verlag; 1987.
Tönnis D, Arning A, Bloch M, Heinecke A, Kalchschmidt K. Triple pelvic osteotomy. J Pediatr Orthop B. 1994;3:54–67.
Tönnis D, Behrens K, Tscharani F. [A new technique of triple osteotomy for turning dysplastic acetabula in adolescents and adults (author’s transl)][in German]. Z Orthop Ihre Grenzgeb. 1981;119:253–265.
van Hellemondt GG, Sonneveld H, Schreuder MH, Kooijman MA, de Kleuver M. Triple osteotomy of the pelvis for acetabular dysplasia: results at a mean follow-up of 15 years. J Bone Joint Surg Br. 2005;87:911–915.
Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint: with special reference to the complication of osteoarthritis. Acta Chir Scand. 1939;83 (suppl 58):7–135.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of their immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This study was performed at Sint Maartenskliniek, Nijmegen, The Netherlands.
About this article
Cite this article
van Stralen, R.A., van Hellemondt, G.G., Ramrattan, N.N. et al. Can a Triple Pelvic Osteotomy for Adult Symptomatic Hip Dysplasia Provide Relief of Symptoms for 25 Years?. Clin Orthop Relat Res 471, 584–590 (2013). https://doi.org/10.1007/s11999-012-2701-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-012-2701-0