Abstract
Background
A number of reconstructive procedures are available for the management of hip osteoarthritis. Hip resurfacing arthroplasty is now an accepted procedure, with implant survivorship comparable to THA at up to 10 years’ followup in certain series. Most reports focus on implant survivorship, surgeon-derived results, or complications. Fewer data pertain to patient-reported results, including validated measures of quality of life (QoL) and satisfaction and baseline measures from which to determine magnitude of improvement. Validated patient-reported results are essential to guide patients and surgeons in the current era of informed and shared decision making.
Questions/purposes
We determined whether patients reported improvement in disease-specific, joint-specific, and generic QoL after hip resurfacing arthroplasty; whether patients were satisfied with the results of the procedure; and latest activity level and return to sport.
Methods
We retrospectively reviewed 127 patients (100 men, 27 women) who underwent 143 hip resurfacing procedures between 2002 and 2006. Mean patient age was 52 years. Patients completed the WOMAC, Oxford Hip Score, and SF-12 at baseline and again at minimum 2-year followup (mean, 2.5 years; range, 2–6 years). At latest followup, patients completed a validated satisfaction questionnaire and UCLA activity score.
Results
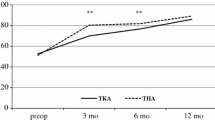
All QoL scores improved (normalized to a 0–100 scale, where 100 = best health state). WOMAC improved from 46 to 95, Oxford Hip Score from 42 to 95, SF-12 (physical) from 34 to 54, and SF-12 (mental) from 46 to 56. Patient satisfaction score was 96. UCLA activity score was 8.
Conclusions
The majority of patients reported improvement in QoL, were very satisfied with their outcome, and returned to a high level of activity after hip resurfacing arthroplasty.
Level of Evidence
Level IV, therapeutic study. See the Instructions for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis of the hip in young active patients remains a difficult problem. Metal-on-metal hip resurfacing has reemerged as an attractive option for treatment of hip osteoarthritis in this group of patients, as an alternative to THA, unless they are suitable candidates for an osteotomy [1, 2]. The modern era of hip resurfacing began in 1990, and it became clear by 1996 a metal-on-metal device with hybrid fixation could produce results comparable to THA [46]. Total hip resurfacing arthroplasty with a metal-on-metal articulation has perceived advantages: the preoperative anatomy is better replicated than with the more traditional THA [34]; proximal femoral bone stock is preserved under a physiologic loadbearing pattern [4, 37]; metal-on-metal articulations have a low wear rate, thus potentially eliminating osteolysis [48]; and the large femoral heads minimize the risk of dislocation [14, 15]. It is currently estimated resurfacing arthroplasty accounts for up to 9% to 11% of all THAs in countries where this technology has been readily available for the last 5 years [12, 23, 35, 50, 62–64].
Recognized complications unique to this procedure are femoral neck fracture (1%–5%), avascular necrosis of the femoral head (1%–2%), increased incidence of heterotopic ossification (2%–5%) compared to THA, raised serum cobalt and chromium metal ion levels, metal hypersensitivity or toxicity (< 1%), osteolysis, pseudotumor (1%–4%), and mutagenesis (< 1%) [3, 5, 10, 45, 46, 54, 55, 59, 60, 62]. Recently published data suggest implant survivorship of 89% to 97% at 10-year followup [5, 6, 17, 30, 47, 67]. Clinical results reported by these authors also suggest a high level of function using various scores and questionnaires. However, there are limitations in these reports in that some patients were missing baseline data from which to determine overall change from preoperative status and some used nonvalidated outcome instruments and surgeon-derived rather than patient-reported results. A number of different implants and surgical procedures are available for the management of osteoarthritis of the hip. Validated patient-reported results are essential to guide patients and surgeons in the current era of informed and shared decision making.
We therefore determined (1) whether patients with well-functioning hip resurfacing arthroplasty systems reported improvement across all domains of disease-specific (WOMAC), joint-specific (Oxford Hip Score), and generic (SF-12) quality of life (QoL) after hip resurfacing arthroplasty; (2) whether patients were satisfied with the results of the procedure (validated satisfaction questionnaire); and (3) latest activity level and return to sport (UCLA activity score).
Patients and Methods
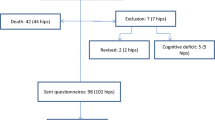
Between June 2002 and May 2006, we performed 143 total hip resurfacing procedures (111 unilateral, 16 bilateral) in 127 patients (100 men, 27 women). The indications for resurfacing arthroplasty were the presence of adequate bone stock judged by plain radiographs and an expectation that they would return to an active lifestyle. Contraindications included renal impairment or history of metal sensitivity, preoperative leg length discrepancy of greater than 1 cm, deficiency of bone stock on the acetabulum or femoral head that would preclude 100% support of the implant, or preexisting hardware in the affected hip. The mean age was 52.1 years (SD, 4.1 years; range, 22–82 years) and patients demonstrated a relatively low BMI (mean < 30) and comorbidity profile (72% Charnley Class A or B1) (Table 1). The minimum followup was 2 years (mean, 2.5 years; range, 2–6 years). All patients were brought in for review during that time period and there was no loss to followup. Informed consent was obtained from all patients, and ethics approval from our university and hospital ethics boards was obtained before the study.
All patients completed the following preoperative QoL questionnaires: the Oxford 12-Item Hip Score [20], WOMAC osteoarthritis index [11], and the SF-12 [71]. At latest followup, patients completed the same questionnaires, privately and independently, as well as the satisfaction questionnaire and the UCLA activity level score [7]. The WOMAC score is a self-administered multidimensional index containing dimensions for pain (five items), stiffness (two items), and function (17 items). Each item is represented by a Likert scale response from 0 (best health state) to 4 (worst health state). The raw scores were transformed into a so-called normalized 0 to 100 scale, with 0 being the worst QoL and 100 the best QoL [11]. The Oxford Hip Score is a 12-item questionnaire for hip outcome assessment and has demonstrated validity in patients with hip arthroplasty [20]. It is a self-administered assessment tool, which, unlike the WOMAC, is designed specifically to capture joint arthroplasty outcomes. A global score is summed from 12 Likert item responses (scores of 1–5) concerning joint pain, function, and mobility. The SF-12 is a generic QoL measure that includes 12 questions from the SF-36 Health Survey (Version 1) [71]. These include two questions concerning physical functioning, two questions on role limitations because of physical health problems, one question on bodily pain, one question on general health perceptions, one question on vitality (energy/fatigue), one question on social functioning, two questions on role limitations because of emotional problems, and two questions on general mental health (psychologic distress and well-being). It is a commonly reported health outcomes measure with reported reliability and validity. The self-administered patient satisfaction scale for primary hip and knee arthroplasty of Mahomed et al. [43, 44] is a four-question instrument specifically for patients with total joint arthroplasty. Satisfaction is questioned for (1) pain, (2) work activity, (3) recreational activity, and (4) overall satisfaction with the procedure. This questionnaire is a scale designed to assess satisfaction with joint arthroplasty. The scale score is the mean of the scores from the individual items, ranging from 25 (least satisfied) to 100 (most satisfied) per item. The instrument is reportedly reliable and valid [43, 44]. All scores with the exception of the UCLA activity score were normalized to a 0 to 100 scale (100 = best health state). The UCLA activity score [7] has been used to ascertain activity level after hip arthroplasty and has been well cited in publications pertaining to activity after prosthetic reconstruction.
The surgery was performed under spinal or general anesthesia using a standard posterolateral approach, to which was added a circumferential capsulotomy in every case and a partial release of the gluteus maximus tendon in most cases. The acetabulum and femoral head were prepared using the recommended technique with each system. Simplex® low-viscosity cement (Stryker Orthopaedics, Mahwah, NJ, USA) was used for fixation of all the femoral components. The Birmingham Hip™ Resurfacing (BHR™) system (Smith & Nephew, Memphis, TN, USA) was used in 39 hips, while the Durom® hip resurfacing system (Zimmer, Inc, Warsaw, IN, USA) was used in 104 hips. The BHR™ has been available for the treatment of the young active patient with osteoarthritis since 1997. The system is composed of a porous cobalt-chromium cup with hydroxyapatite coating for cementless fixation and a cobalt-chromium femoral component for cemented fixation. Early results with this implant have been encouraging, with an overall survival of 98% at 5 years [18, 66]. We began using the Durom® system in 2001. The Metasul® articulation (Zimmer, Inc) has been used since 1988 [29, 61].
The postoperative protocol was the same throughout the study, which included prophylactic antibiotics for 24 hours and low-molecular-weight heparin for 10 days. No specific prophylaxis for heterotopic ossification was used. An immediate postoperative progressive physiotherapy program with full weightbearing with crutches was allowed, followed by rapid discontinuation of walking aids as tolerated.
Patients were reviewed at postoperative checkpoints of 6 weeks, 3 months, 12 months, and 24 months. Clinical assessment included clinical and radiographic review, as well as interview for complications, including deep venous thrombosis, infection, femoral neck fracture, revision surgery, or dislocation. At the latest followup assessment, patients were invited to complete the same set of questionnaires obtained preoperatively, along with the patient-reported satisfaction score and UCLA activity score. The UCLA score was not obtained preoperatively at our center as it was not part of our routine data collection at baseline at the time these surgical procedures were performed. However, as activity may be associated with QoL and satisfaction scores, we obtained activity scores at the time of latest followup in all postoperative questionnaires. Questionnaires were sent to patients with instructions to complete them independently and privately and they were returned directly to the research coordinator. Analysis of patient-reported QoL scores, activity level, and satisfaction scales was limited to patients with a minimum of 2-year followup with a complete set of pre- and postoperative questionnaires. Therefore, the probability of implant survival and complication rates were based on analysis of the entire cohort of 143 hips in 127 patients, while the statistical analyses of the QoL scores and patient satisfaction were based on the subgroup of 131 hips in 127 patients with QoL outcome measures at minimum 2-year followup. Of the 12 hips not included in the final statistical analysis of the QoL scores, 10 had less than 2 years’ followup and two were excluded because of conversion to THA within 2 months of the hip resurfacing due to fracture of the femoral neck. Complications data were obtained from an independent assessment of the readmission and inpatient audit data, as well as hospital and office chart review.
Radiographic evaluation was performed using AP radiographs of the pelvis and Johnson crosstable lateral radiographs [2, 14, 22, 28, 32, 51] at 6 weeks, 3 months, and then annually.
We performed descriptive and comparative analyses using SAS® software (Version 9.1; SAS Institute Inc, Cary, NC, USA). Tests for normality were performed for QoL measures, satisfaction, and UCLA activity score using the Kolmogorov-Smirnov test. To determine differences between preoperative and latest postoperative values, we analyzed variables not demonstrating normality (p < 0.05) (SF-12) using the Mann-Whitney U test and variables demonstrating normality (WOMAC, Oxford Hip Score) using t-tests. The patient satisfaction score and UCLA activity score demonstrated nonnormality in distribution, but since they were recorded only at latest followup, these values could not be compared with preoperative values. All tests were two-sided. The probability of implant survival was calculated with two end points: from the time of surgery to the conversion to a THA for any reason and from the time of surgery to presentation with symptoms necessitating revision.
Results
All QoL scores (normalized to a 0–100 scale) improved (p < 0.001) from baseline (Table 2). Disease-specific QoL as measured by the WOMAC global score improved from a preoperative score of 46 to 95 at most recent followup. The WOMAC pain, function, and stiffness scores improved from 47 to 97, from 47 to 95, and from 40 to 89, respectively. Joint-specific QoL as measured by the Oxford Hip Score improved from 42 to 95. Generic QoL as measured by the SF-12 improved from 34 to 54 on the physical component and from 47 to 57 on the mental component. The patients were very satisfied with the result of the surgery, with an overall patient-reported satisfaction score of 96 of 100 (Table 3). The patients maintained a very high level of activity, with a mean UCLA activity level of 8 (range, 3–10). Eighty-eight percent of the patients had a UCLA activity level of higher than 6.
There were two intraoperative complications, including an intraoperative injury of the profunda femoris vein that was repaired with no sequelae. There was also a sciatic nerve injury with incomplete recovery. Five of 143 hips (3.5%) in five patients were converted to a large-head metal-on-metal THA with maintenance of the existing well-fixed acetabular socket, two for femoral neck fracture, and two for unexplained pain attributed to avascular necrosis. One patient underwent a second socket revision to a metal-on-crosslinked polyethylene articulation for persistent pain after investigations showed a 7-cm cystic mass, which was deemed to be a pseudotumor. His function improved after removal of the metal-on-metal articulation. One hip was revised to THA due to recurrent dislocation that occurred in a horse jockey involved in a fall. If we define failure as the end point with definition of failure as revision of component to date, five of 143 hips were revised. The probability of implant survival was 138 of 143 hips or 0.97 (95% CI, 0.935–0.995) at 2 years’ followup. Three more hips required reoperation, including a cup exchange in the first week after the operation due to change in the position of the acetabular cup. The second hip developed early infection that was managed successfully with open drainage and 6 weeks of intravenous antibiotics, the surface replacement was retained, and the infection was controlled, with good functional outcome at latest followup. The third patient suffered an ipsilateral intertrochanteric fracture in a cycling accident 3 months after the hip resurfacing, which was managed by internal fixation using a gamma nail; the fracture healed uneventfully, and the fracture fixation implants were removed 2 years later. The total number of complications requiring reoperation including previous revisions, pending revision, and all other reoperations was 11 of 143 hips. The probability of not requiring an additional procedure was therefore 132 of 143 hips or 0.92 (95% CI, 0.879–0.967) at 2 years postoperatively.
Discussion
A number of reconstructive procedures are available for the management of hip osteoarthritis. Hip resurfacing arthroplasty is now an accepted procedure, with implant survivorship comparable to that of THA at up to 10 years’ followup in certain series. Most historical reports focus on implant survivorship, surgeon-derived results, or complications. Fewer data exist pertaining to patient-reported results, including validated measures of QoL and satisfaction and baseline measures from which to determine magnitude of improvement. We therefore determined (1) whether patients with well-functioning hip resurfacing arthroplasty systems reported improvement across all domains of disease-specific (WOMAC), joint-specific (Oxford Hip Score), and generic (SF-12) QoL after hip resurfacing arthroplasty; (2) whether patients were satisfied with the results of the procedure (validated satisfaction questionnaire); and (3) latest activity level and return to sport (UCLA activity score).
We acknowledge some potential limitations to our study. First, this is a retrospective cohort study using prospectively collected data; it was not a randomized controlled trial. We allowed patients to choose this procedure after reviewing the potential differences, along with risks and benefits, between resurfacing versus THA. Therefore, there is the potential that some volunteer bias could be influencing the scores as patients who feel extremely keen on the resurfacing procedure are the only ones who would have received the implant at our center. This potential for bias is evident if we compare the WOMAC scores from the randomized controlled trial by Garbuz et al. [25] where a similar cohort of patients received resurfacing or large-diameter-head THA and had WOMAC scores at latest followup that are a mean 5 points less than those in our series. However, we sought to reduce the potential for interviewer bias or other biases that could arise from the surgeon obtaining the scores directly from the patients. We asked our patients to complete their questionnaires independently and privately and then mail them to our research coordinator. An additional potential limitation of our study is attributable to our study design. The defined purpose of our study was to only evaluate those patients who were a minimum 2 years from surgery and had intact resurfacing implants. Therefore, we are unable to comment on the QoL, satisfaction, and activity scores of the patients revised due to fracture, loosening, or pseudotumor. This will contribute bias whereby our results demonstrate a so-called best-case-scenario rather than an intent-to-treat analysis, which would be typically reported in a randomized clinical trial. Nevertheless, our cohort includes patients with demographic characteristics comparable to those seeking hip resurfacing arthroplasty in North America [6, 52, 68–70]. Therefore, we believe our observations and results should be considered generalizable. We are currently conducting a study to comprehensively evaluate patients who underwent revision of resurfacing procedures to determine outcome but are unable to report on those patients at this time.
The primary objective of our study was to evaluate patient-reported improvement in QoL after hip resurfacing arthroplasty. Our assessment of disease-specific QoL (WOMAC) demonstrated improvement in global status of the arthritic hip, as well as in domains of pain and function, resulting in scores of 95, 97, and 95, as compared to baseline 46, 47, and 47, respectively (on a scale of 0–100). These values rival those reported for the normal nonarthritic population. Patients reported an improvement in WOMAC stiffness from 40 to 89. Our assessment of joint-specific QoL (Oxford Hip Score) demonstrated improvement from baseline to a most recent score of 95 of 100. Our assessment of generic QoL (SF-12) demonstrated improvements on the physical and mental component scores comparable to the nonarthritic population. These outcomes support and underscore recent reports on WOMAC scores [25, 38, 39, 41, 57, 59, 69, 70] and Oxford Hip Scores [31, 36, 56–58] from other authors and patient populations. Our SF-12 results are in agreement with published SF-12 and SF-36 outcomes, which demonstrate restoration of generic QoL approaching that of the normal population [16, 41, 56, 58] (Table 4). Until recently, most reports focused on implant survivorship and did not consistently include validated patient-reported outcome measures that refer to QoL or other dimensions of patient-perceived results of surgery, such as patient satisfaction and activity [16, 41]. Patient perception of the results of surgery and patient preferences are an increasingly important component of patient-informed and shared decision making in elective surgical procedures [13]. Our study used validated patient-reported outcomes rather than surgeon-derived questionnaires, implant survivorship, or radiographic features as end points to determine successful outcome. Our results indicated patients who had surviving implants at minimum 2 years postoperatively were functioning at a level that rivals the nonarthritic population.
Recent 10-year survivorship publications have an arthritis- or hip-specific QoL score but do not have these scores on all patients at baseline preoperatively, which precludes determination of so-called improvement from preoperative status [2, 5, 6, 17, 18, 30, 47, 54, 67]. Previous reports demonstrate the fixation of implants is excellent with low rates of implant failure [8, 27, 28, 34, 66].
Our study demonstrated patients with resurfacing were highly satisfied with their procedure and attained a high level of satisfaction across multiple domains including pain relief, function, and ability to participate in recreation. Few series to date report on a validated patient-reported satisfaction score. Coulter et al. [17] and Lingard et al. [41] reported high levels of satisfaction, with results comparable to our cohort of patients with resurfacing.
Our patients reported a mean UCLA activity score of 8 (range, 3–10), which supports activity-related results reported from other centers [2, 6, 9, 16–18, 30, 33, 47, 53, 54, 66]. Eighty-eight percent of our study patients attained a UCLA activity level of greater than 6, indicating a return to vigorous sporting activities.
There are two main modes of femoral failure after surface arthroplasty: neck fracture and aseptic loosening. The latter has a relatively low incidence of 1.2% [1, 2, 62, 63]. The incidence of fracture of the femoral neck in our study was 1.3% (two of 143 hips), which is relatively low and similar to the range of 0% to 2.5% reported in the literature [2, 5, 6, 8, 12, 16, 18, 25, 30, 33, 35, 48, 62, 67].
We observed a minority of patients in the study reported unexplained pain. All of them had a Durom® hip resurfacing. Revision to large-head metal-on-metal arthroplasty was performed in two patients. Component orientation was satisfactory and there was no radiographic or intraoperative evidence of loosening. Pathologic examination did not reveal femoral head osteonecrosis. The outcome after revision was disappointing in one patient who underwent a second socket revision to a metal-on-crosslinked polyethylene articulation for persistent pain after investigations showed a 7-cm cystic mass, which was deemed to be a pseudotumor. His function improved after removal of the metal-on-metal articulation. The other three patients were doing well in the first 4 years after the surgery, but then they started to experience activity-related pain. This was mild in one patient and severe in the other two patients. Infection was excluded and radiographs were unremarkable. These patients are currently under investigation and exploration will be performed if the symptoms increase or if there is MRI evidence of a reactive synovial cyst or pseudotumor. We classified these patients as at risk of failure and revision in keeping with our experience with this implant design in other patients outside of this study cohort. The late onset of similar symptoms in the nonstudy group, leading to exploration of the hip, revealed a loose cup due to fibrous fixation of the socket, although the radiographs were unremarkable with no signs of loosening. We have learned from this experience that the cup can be loose despite evidence of interface stability using conventional radiographic criteria. Similar experience with painful fibrous fixation of the Durom® cup, despite radiographic evidence of stability, has been reported from another center [42].
We remain cautious in the evaluation of these patients, as a number of concerns are beginning to emerge with metal-on-metal hip resurfacing, such as aseptic lymphocytic vasculitis-associated lesions (ALVALs) and pseudotumors [19, 21, 55, 72, 73]. It has to be stated the majority of complications in our series involved the Durom® system rather than the BHR™, suggesting there are substantial differences between implants and subtle implant design changes may lead to different outcomes. Nevertheless, the concerns regarding ALVAL and pseudotumor formation may be associated with any metal-on-metal hip arthroplasty system.
In conclusion, our patient-reported data demonstrated improvement from baseline preoperatively across domains of hip function, pain, stiffness, and generic QoL. In addition, the vast majority of patients remained highly satisfied and returned to a high level of sport and activity. Nevertheless, the rates of major complications and early revisions are certainly causes for concern. We recommend patients be advised of these risks alongside the benefits when considering hip resurfacing arthroplasty.
References
Amstutz HC. Present state of metal-on-metal hybrid hip resurfacing. J Surg Orthop Adv. 2008;17:12–16.
Amstutz HC, Beaulé PE, Dorey FJ, Le Duff MJ, Campbell PA, Gruen TA. Metal-on-metal hybrid surface arthroplasty: two to six-year follow-up study. J Bone Joint Surg Am. 2004;86:28–39.
Amstutz HC, Grigoris P. Metal on metal bearings in hip arthroplasty. Clin Orthop Relat Res. 1996;329(suppl):S11–S34.
Amstutz HC, Grigoris P, Dorey FJ. Evolution and future of surface replacement of the hip. J Orthop Sci. 1998;3:169–186.
Amstutz HC, Le Duff MJ, Campbell PA, Gruen TA, Wisk LE. Clinical and radiographic results of metal-on-metal hip resurfacing with a minimum ten-year follow-up. J Bone Joint Surg Am. 2010;92:2663–2671.
Amstutz HC, Takamura KM, Le Duff MJ. The effect of patient selection and surgical technique on the results of Conserve Plus Hip Resurfacing—3.5 to 14 year follow-up. Orthop Clin North Am. 2011;42:133–142.
Amstutz HC, Thomas BJ, Jinnah R, Kim W, Grogan T, Yale C. Treatment of primary osteoarthritis of the hip: a comparison of total joint and surface replacement arthroplasty. J Bone Joint Surg Am. 1984;66:228–241.
Back DL, Dalziel R, Young D, Shimmin A. Early results of primary Birmingham hip resurfacings: an independent prospective study of the first 230 hips. J Bone Joint Surg Br. 2005;87:324–329.
Baker RP, Pollard TC, Eastaugh-Waring SJ, Bannister GC. A medium-term comparison of hybrid hip replacement and Birmingham hip resurfacing in active young patients. J Bone Joint Surg Br. 2011;93:158–163.
Beaulé PE, Dorey FJ, LeDuff M, Gruen T, Amstutz HC. Risk factors affecting outcome of metal-on-metal surface arthroplasty of the hip. Clin Orthop Relat Res. 2004;418:87–93.
Bellamy N, Buchman WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: health status instrument for measuring clinically important patient relevant outcomes to anti-rheumatic drug therapy in patients with osteoarthritis of the hip and the knee. J Rheumatol. 1988;15:1833–1840.
Bozic KJ, Browne J, Dangles CJ, Manner PA, Yates AJ Jr, Weber KL, Boyer KM, Zemaitis P, Woznica A, Turkelson CM, Wies JL. Modern metal-on-metal implants. J Am Acad Orthop Surg. 2012;20:402–406.
Bozic KJ, Chiu V, Slover JD, Immerman I, Kahn JG. Patient preferences and willingness to pay for arthroplasty surgery in patients with osteoarthritis of the hip. J Arthroplasty. 2012;27:503–507.
Brooker AF, Bowerman JW, Robinson RA, Riley LH Jr. Ectopic ossification following total hip replacement: incidence and a method of classification. J Bone Joint Surg Am. 1973;55:1629–1632.
Burroughs BR, Hallstrom B, Golladay GJ, Hoeffel D, Harris WH. Range of motion and stability in total hip arthroplasty with 28-, 32-, 38-, and 44-mm femoral head sizes. J Arthroplasty. 2005;20:11–19.
Costa ML, Achten J, Parsons NR, Edlin RP, Foguet P, Prakash U, Griffin DR; Young Adult Hip Arthroplasty Team. Total hip arthroplasty versus resurfacing arthroplasty in the treatment of patients with arthritis of the hip joint: single centre, parallel group, assessor blinded, randomized controlled trial. BMJ. 2012;344:e2147.
Coulter G, Young DA, Dalziel RE, Shimmin AJ. Birmingham hip resurfacing at a mean of ten years: results from an independent centre. J Bone Joint Surg Br. 2012;94:315–321.
Daniel J, Pynsent PB, McMinn DJ. Metal-on-metal resurfacing of the hip in patients under the age of 55 years with osteoarthritis. J Bone Joint Surg Br. 2004;86:177–184.
Davies AP, Willert HG, Campbell PA, Learmonth ID, Case CP. An unusual lymphocytic perivascular infiltration in tissues around contemporary metal-on-metal joint replacements. J Bone Joint Surg Am. 2005;87:18–27.
Dawson J, Fitzpatrick R, Carr AJ, Murray D. Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg Br. 1996;78:185–190.
De Haan R, Pattyn C, Gill HS, Murray DW, Campbell PA, De Smet K. Correlation between inclination of the acetabular component and metal ion levels in metal-on-metal hip resurfacing replacement. J Bone Joint Surg Br. 2008;90:1291–1297.
DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20–32.
Dimanji SR, Vendittoli PA, Lavigne M. Hip resurfacing vs metal-on-metal total hip arthroplasty. In: Bhandari M, ed. Evidence Based Orthopaedics. Oxford, UK: Blackwell Publishing Ltd; 2012:137–152.
Fowbie VA, de la Rosa MA, Schmalzried TP. A comparison of total hip resurfacing and total hip arthroplasty—patients and outcomes. Bull NYU Hosp Jt Dis. 2009;67:108–112.
Garbuz DS, Tanzer M, Greidanus NV, Masri BA, Duncan CP. The John Charnley Award. Metal-on-metal hip resurfacing versus large-diameter head metal-on-metal total hip arthroplasty: a randomized clinical trial. Clin Orthop Relat Res. 2010;468:318–325.
Girard J, Vendittoli PA, Roy AG, Lavigne M. [Femoral offset restoration and clinical function after total hip arthroplasty and surface replacement of the hip: a randomized study] [in French]. Rev Chir Orthop Reparatrice Appar Mot. 2008;94:376–381.
Glyn-Jones S, Gill HS, McLardy-Smith P, Murray DW. Roentgen stereophotogrammetric analysis of the Birmingham hip resurfacing arthroplasty: a two-year study. J Bone Joint Surg Br. 2004;86:172–176.
Gold R, Nasser S, Stall S. Conventional roentgenography with special techniques for follow-up of hip arthroplasty. In: Amstutz HC, ed. Hip Arthroplasty. New York, NY: Churchill Livingstone; 1991:121–131.
Grigoris P, Roberts P, Panousis K, Bosch H. The evolution of hip resurfacing arthroplasty. Orthop Clin North Am. 2005;36:125–134.
Gross TP, Liu F, Webb LA. Clinical outcome of the metal-on-metal hybrid Corin Cormet 2000 hip resurfacing system: an up to 11-year follow-up study. J Arthroplasty. 2012;27:533–538.e1.
Hall D, Srikantharajah D, Anakwe R, Gaston P, Howie C. Patient-reported outcome following metal-on-metal resurfacing of the hip and total hip replacement. Hip Int. 2009;19:245–250.
Hing CB, Young DA, Dalziel RE, Bailey M, Back DL, Shimmin AJ. Narrowing of the neck in resurfacing arthroplasty of the hip: a radiological study. J Bone Joint Surg Br. 2007;89:1019–1024.
Holland JP, Langton DJ, Hashmi M. Ten-year clinical, radiological and metal ion analysis of the Birmingham Hip Resurfacing: from a single, non-designer surgeon. J Bone Joint Surg Br. 2012;94:471–476.
Itayem R, Arndt A, Nistor L, McMinn D, Lundberg A. Stability of the Birmingham hip resurfacing arthroplasty at two years. J Bone Joint Surg Br. 2005;87:158–162.
Jiang Y, Zhang K, Die J, Shi Z, Zhao H, Wang K. A systematic review of modern metal-on-metal total hip resurfacing vs standard total hip arthroplasty in active young patients. J Arthroplasty. 2011;26:419–426.
Killampalli VV, Kundra RK, Chaudhry J, Chowdhry M, Fisher NE, Reading AD. Resurfacing and uncemented arthroplasty for young hip arthritis: functional outcomes at 5 years. Hip Int. 2009;19:234–438.
Kishida Y, Sugano N, Nishii T, Miki H, Yamaguchi K, Yoshikawa H. Preservation of the bone mineral density of the femur after surface replacement of the hip. J Bone Joint Surg Br. 2004;86:185–189.
Lavigne M, Masse V, Girard J, Roy AG, Vendittoli PA. [Return to sport after hip resurfacing or total hip arthroplasty: a randomized study] [in French]. Rev Chir Orthop Reparatrice Appar Mot. 2008;94:361–367.
Lavigne M, Therrien M, Nantel J, Roy A, Prince F, Vendittoli PA. The John Charnley Award. The functional outcome of hip resurfacing and large-head THA is the same: a randomized, double-blind study. Clin Orthop Relat Res. 2010;468:326–336.
LeDuff MJ, Wisk LE, Amstutz HC. Range of motion after stemmed total hip arthroplasty and hip resurfacing—a clinical study. Bull NYU Hosp Jt Dis. 2009;67:177–181.
Lingard EA, Muthumayandi K, Holland JP. Comparison of patient-reported outcomes between hip resurfacing and total hip replacement. J Bone Joint Surg Br. 2009;91:1550–1554.
Long WT, Dastane M, Harris MJ, Wan Z, Dorr LD. Failure of the Durom Metasul acetabular component. Clin Orthop Relat Res. 2010;468:400–405.
Mahomed N, Gandhi R, Daltroy L, Katz JN. The self-administered patient satisfaction scale for primary hip and knee arthroplasty. Arthritis. 2011;2011:591253.
Mahomed NN, Liang MH, Cook EF, Daltroy LH, Fortin PR, Fossel AH, Katz JN. The importance of patient expectations in predicting functional outcomes after total joint arthroplasty. J Rheumatol. 2002;29:1273–1279.
McKellop H, Park SH, Chiesa R, Doorn P, Lu B, Normand P, Grigoris P, Amstutz H. In vivo wear of three types of metal on metal hip prostheses during two decades of use. Clin Orthop Relat Res. 1996;329(suppl):S128–S140.
McMinn D, Treacy R, Lin K, Pynsent P. Metal on metal surface replacement of the hip: experience of the McMinn prosthesis. Clin Orthop Relat Res. 1996;329(suppl):S89–S98.
McMinn DJ, Daniel J, Ziaee H, Pradhan C. Indications and results of hip resurfacing. Int Orthop. 2011;35:231–237.
Migaud H, Jobin A, Chantelot C, Giraud F, Laffargue P, Duquennoy A. Cementless metal-on-metal hip arthroplasty in patients less than 50 years of age: comparison with a matched control group using ceramic-on-polyethylene after a minimum 5-year follow-up. J Arthroplasty. 2004;19(suppl 3):23–28.
Mont MA, Marker DR, Smith JM, Ulrich SD, McGrath MS. Resurfacing is comparable to total hip arthroplasty at short-term follow-up. Clin Orthop Relat Res. 2009;467:66–71.
Mont MA, Schmalzried TP. Modern metal-on-metal hip resurfacing: important observations from the first ten years. J Bone Joint Surg Am. 2008;90(suppl 3):3–11.
Moore MS, McAuley JP, Young AM, Engh CA. Radiographic signs of osteointegration in porous coated acetabular components. Clin Orthop Relat Res. 2006;444:176–183.
Newman MA, Barker KL, Pandit H, Murray DW. Outcomes after metal-on-metal hip resurfacing: could we achieve better function? Arch Phys Med Rehabil. 2008;89:660–666.
Nishii T, Sugano N, Hidenobu MH, Takao M, Tsuyoshi KT, Yoshikawa H. Five-year results of metal-on-metal resurfacing arthroplasty in Asian patients. J Arthroplasty. 2007;22:176–183.
Ortiguera CJ, Pulliam IT, Cabanela ME. Total hip arthroplasty for osteonecrosis: matched-pair analysis of 188 hips with long-term follow-up. J Arthroplasty. 1999;14:21–28.
Pandit H, Glyn-Jones S, McLardy-Smith P, Gundle R, Whitwell D, Gibbons CL, Ostlere S, Athanasou N, Gill HS, Murray DW. Pseudotumours associated with metal-on-metal hip resurfacings. J Bone Joint Surg Br. 2008;90:847–851.
Pollard TC, Baker RP, Eastaugh-Waring SJ, Bannister GC. Treatment of the young active patient with osteoarthritis of the hip: a five to seven year comparison of hybrid total hip arthroplasty and metal-on-metal resurfacing. J Bone Joint Surg Br. 2006;88:592–600.
Rahman L, Muirhead-Allwood SK, Alkinj M. What is the midterm survivorship and function after hip resurfacing? Clin Orthop Relat Res. 2010;468:3221–3227.
Sandiford NA, Muirhead-Allwood SK, Skinner JA, Hua J. Metal on metal hip resurfacing versus uncemented custom total hip replacement—early results. J Orthop Surg Res. 2010;5:8.
Schmalzried TP. Metal-on-metal resurfacing arthroplasty: no way under the sun!—in opposition. J Arthroplasty. 2005;20(suppl 2):70–71.
Schmalzried TP, Peters PC, Maurer BT, Bragdon CR, Harris WH. Long-duration metal-on-metal total hip arthroplasties with low wear of the articulating surfaces. J Arthroplasty. 1996;11:322–331.
Schmidt M, Weber H, Schon R. Cobalt chromium molybdenum metal combination for modular hip prostheses. Clin Orthop Relat Res. 1996;329(suppl):S35–S47.
Shimmin AJ, Back D. Femoral neck fractures following Birmingham hip resurfacing. J Bone Joint Surg Br. 2005;87:463–464.
Shimmin AJ, Baré JV. Comparison of functional results of hip resurfacing and total hip replacement: a review of the literature. Orthop Clin North Am. 2011;42:143–151.
Smith TO, Nichols R, Donell ST, Hing CB. The clinical and radiological outcomes of hip resurfacing versus total hip arthroplasty: a meta-analysis and systematic review. Acta Orthop. 2010;81:684–695.
Smolders JM, Hol A, Rijnberg WJ, van Susante JL. Metal ion levels and functional results after either resurfacing hip arthroplasty or conventional metal-on-metal hip arthroplasty. Acta Orthop. 2011;82:559–666.
Treacy RB, McBryde CW, Pynsent PB. Birmingham hip resurfacing arthroplasty: a minimum follow-up of five years. J Bone Joint Surg Br. 2005;87:167–170.
Treacy RB, McBryde CW, Shears E, Pynsent PB. Birmingham hip resurfacing: a minimum follow-up of ten years. J Bone Joint Surg Br. 2011;93:27–33.
Vail TP, Mina CA, Yergler JD, Pietrobon R. Metal-on-metal hip resurfacing compares favorably with THA at 2 years follow-up. Clin Orthop Relat Res. 2006;453:123–131.
Vendittoli PA, Ganapathi M, Roy AG, Lusignan D, Lavigne M. A comparison of clinical results of hip resurfacing arthroplasty and 28 mm metal on metal total hip arthroplasty: a randomised trial with 3–6 years follow-up. Hip Int. 2010;20:1–13.
Vendittoli PA, Lavigne M, Roy AG, Lusignan D. A prospective randomized clinical trial comparing metal-on-metal total hip resurfacing in patient less than 65 years old. Hip Int. 2006;16(suppl 4):73–81.
Ware JE, Kosinski M, Keller SD. SF-12: How to Score the SF-12 Physical and Mental Health Summary Scales. 2nd ed. Boston, MA: The Health Institute, New England Medical Center; 1995.
Willert HG, Buchhorn GH, Fayyazi A, Flury R, Windler M, Köster G, Lohmann CH. Metal-on-metal bearings and hypersensitivity in patients with artificial hip joints: a clinical and histomorphological study. J Bone Joint Surg Am. 2005;87:28–36.
Willert HG, Buchhorn GH, Fayyazi A, Lohmann CH. Histopathological changes around metal/metal joints indicates delayed type hypersensitivity: preliminary results of 14 cases. Osteologie. 2000;9:2–16.
Zywiel MG, Marker DR, McGrath MS, Delanois RE, Mont MA. Resurfacing matched to standard total hip arthroplasty by preoperative activity levels—a comparison of postoperative outcomes. Bull NYU Hosp Jt Dis. 2009;67:116–119.
Acknowledgments
We thank Daphné Savoy for her assistance in the preparation of this manuscript and Abdul Aziz for his participation with patient followup and data collection for this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
The institution of one or more of the authors (WAR, CPD, NVG, BAM, DSG) has received funding, during the study period, from Zimmer, Inc (Warsaw, IN, USA). One or more of the authors (BAM, CPD, DSG) certify that each has received or may receive payments or benefits, during the study period, an amount in excess of $10,000, from Zimmer, Inc. Each remaining author certifies that he or she, or a member of his or her immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the University of British Columbia, Vancouver, British Columbia, Canada.
About this article
Cite this article
Rahman, W.A., Greidanus, N.V., Siegmeth, A. et al. Patients Report Improvement in Quality of Life and Satisfaction After Hip Resurfacing Arthroplasty. Clin Orthop Relat Res 471, 444–453 (2013). https://doi.org/10.1007/s11999-012-2645-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-012-2645-4