Abstract
Objectives
This study has three aims: (1) validate a new radiographic measure of acetabular version, the transverse axis distance (TAD) by showing equivalent TAD accuracy in predicting CT equatorial acetabular version when compared to a previously validated, but more cumbersome, radiographic measure, the p/a ratio; (2) establish predictive equations of CT acetabular version from TAD; (3) calculate a sensitive and specific cut point for predicting excessive CT acetabular anteversion using TAD.
Materials and methods
A 14-month retrospective review was performed of patients who had undergone a dedicated MSK CT pelvis study and who also had a technically adequate AP pelvis radiograph. Two trained observers measured the radiographic p/a ratio, TAD, and CT acetabular equatorial version for 110 hips on a PACS workstation. Mixed model analysis was used to find prediction equations, and ROC analysis was used to evaluate the diagnostic accuracy of p/a ratio and TAD.
Results
CT equatorial acetabular version can accurately be predicted from either p/a ratio (p < 0.001) or TAD (p < 0.001). The diagnostic accuracies of p/a ratio and TAD are comparable (p =0.46). Patients whose TAD is higher than 17 mm may have excessive acetabular anteversion. For that cutpoint, the sensitivity of TAD is 0.73, with specificity of 0.82.
Conclusion
TAD is an accurate radiographic predictor of CT acetabular anteversion and provides an easy-to-use and intuitive point-of-care assessment of acetabular version in patients with hip pain.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Abnormal acetabular version has been correlated with pathologic hip conditions including femoroacetabular impingement (FAI) and developmental hip dysplasia. Acetabular version refers to the anteroposterior orientation of the acetabular opening relative to the true horizontal axis of the pelvis. Normally, the acetabular opening is oriented anteriorly by 13–20° when measured at the center of the acetabulum [1–3]. This is referred to as central, or equatorial acetabular version. A retroverted acetabulum opens more posteriorly (less than 13°) and an anteverted acetabulum opens more anteriorly (greater than 20°). The spiral orientation of the acetabular opening results in increasing acetabular version in a cranial to caudal direction, with cranial acetabular version averaging 12° less than central acetabular version [2].
The association between acetabular retroversion and femoroacetabular impingement has been well established in recent years as a source of hip pain contributing to early hip osteoarthrosis and labral tears [1, 4–8]. Acetabular anteversion has classically been associated with developmental dysplasia of the hip, an additional cause of early osteoarthritis [9–11]. Recognition and appropriate treatment of abnormal acetabular version is crucial to preventing irreversible damage to the hip.
Although an AP pelvis radiograph is often the first radiographic exam obtained in the evaluation of hip pain, no well-established quantitative radiographic tool exists to assess acetabular version. Several radiographic signs have been established as secondary indicators of acetabular retroversion, including the crossover sign, ischial spine sign, and posterior wall sign [12, 13]. Multiple investigators have proposed radiographic assessments to measure acetabular version or acetabular coverage in the past but none have gained widespread use [2, 3, 14]. The lack of traction of these radiographic assessments is likely due to their rather tedious and time-consuming nature. An objective radiographic tool which provides measurements comparable in accuracy to CT measurements would help both physicians and patients.
In this study, conducted in a population of patients with hip pain presenting to a hip preservation center, we aim to define a new radiographic measure of acetabular version, the transverse axis distance (TAD), and establish its equivalent accuracy to a previously validated radiographic assessment, the p/a ratio [3]. In addition, we demonstrate that CT acetabular version can be accurately predicted from TAD. Finally, we compare ROC measures of diagnostic accuracy for TAD and p/a ratio for the diagnosis of excessive acetabular anteversion, using CT equatorial acetabular version of greater than 20° as a gold standard.
Materials and methods
This study was approved by the institutional review board at our institute, and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. We searched PACS for CT scans of the pelvis performed according to a dedicated MSK protocol between August 1, 2012 and October 17, 2013. A total of 151 studies (302 hips) were initially identified. Patients were included if they were at least 10 years of age and had a technically adequate AP pelvis radiograph in PACs. Fifty-two hips were excluded for having no AP pelvis radiograph available, while 10 hips were excluded for having prior surgical alteration of the acetabulum including periacetabular osteotomy (4), acetabular rim shaving (2), slipped capital femoral epiphysis repair (1), and total hip arthroplasty (3). Each hip was evaluated and analyzed separately.
The MSK CT pelvis protocol is routinely obtained at our institution for patients presenting with hip pain to our orthopaedic center of hip preservation. The MSK CT pelvis protocol is used to determine acetabular version and other measurements for preoperative planning of patients being evaluated for impingement or hip dysplasia surgical correction. This protocol has been previously described elsewhere [15]. Briefly, the patient is placed supine on the gantry with feet placed in a foot binder in neutral, toes up position. Care is taken to square the pelvis on the CT gantry. Whole pelvis 1-mm acquisitions with 2-mm reconstructions in axial, sagittal and coronal planes as well as axial images of the distal femurs for evaluation of femoral torsion are obtained. Oblique axial reconstructions along the long axis of the femoral neck, and 3D surface rendered reconstructions are generated from the axial acquisition.
AP pelvis radiographs are obtained at our institute according to standard protocol [16] with the patient supine and legs in 15° of internal rotation. The X-ray beam is centered midway between the anterior superior iliac spine and the pubic symphysis, with an X-ray tube-to-film distance of 120 cm. Occasionally, the AP pelvis radiograph was performed at an outside institution and was uploaded onto our local PACS. These studies were included in the analysis if the image met criteria for technical adequacy.
All AP pelvis radiographs were evaluated for technical adequacy by assessing pelvic rotation and pelvic tilt. Degree of pelvic tilt was determined by measuring the vertical distance between the coccygeal tip and upper margin of the pubic symphysis, with acceptable distances ranging from 1–3 cm [16]. Pelvic rotation was determined by measuring the transverse distance between lines dividing the center of pubic symphysis and center of the sacrum. Distances between 0 (no rotation) and 1 cm of pelvic rotation were allowed.
One hundred sixteen hips were excluded for coccygeal to pubic symphysis distance of less than 1 cm or greater than 3 cm, whereas 14 hips were excluded for pelvic rotation of greater than 1 cm. These exclusions left 110 hips included in the final analysis (Fig. 1), of which 72 hips were female and 38 were male. The average age was 32 years with a range of 14–55 years (Table 1).
Trained observers performed all measurements on a PACS workstation. Observer A, a second year radiology resident, measured the radiographic p/a ratio and CT acetabular version for all hips. Observer B, a MSK radiologist with 10 years of experience, measured the radiographic TAD for all hips. Observers were not strictly blinded to other imaging studies available for the patient in PACS.
The p/a ratio was calculated from the distance between the acetabular articular surface to the posterior wall (P) and the distance from the acetabular articular surface to the anterior wall (A), both measured along the perpendicular bisector of a line connecting the lateral edge of the acetabulum and the teardrop, as described by Koyama et al. [3]. If the perpendicular bisector fell within the acetabular fossa, the point on a circle of best fit of the acetabulum drawn along the sourcil was used as the acetabular articular surface from which to measure P and A (Fig. 2).
Method for calculating p/a ratio. The p/a ratio was calculated from the distance between the acetabular articular surface to the posterior wall (P) and the distance from the acetabular articular surface to the anterior wall (A), both measured along the perpendicular bisector of a line connecting the lateral edge of the acetabulum and the teardrop
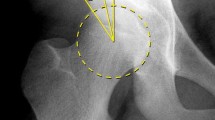
TAD was measured by first drawing a line (T) connecting the inferior acetabular teardrops. This line represented the true transverse axis of the radiographic pelvis. Next, a circle of best fit was approximated around the femoral head. Line T was moved superiorly until it bisected the equator of the best fit circle of the femoral head. The distance between the anterior and posterior acetabular walls was measured along line T, yielding the TAD measurement in mm (Fig. 3).
Method for measuring the transverse axis distance (TAD). True pelvis horizontal line (T) was drawn connecting the inferior aspects of the acetabular teardrops. The line (T) was then moved superiorly until it intersected the center of a best fit circle drawn around the femoral head of the hip being measured. The distance, measured in mm, between the anterior and posterior walls was the TAD
CT equatorial acetabular version was measured at the level of the mid femoral head on axial CT images, correlating to the center of a best fit circle drawn around the femoral head on the central coronally reconstructed cut [4]. The version angle was measured between a line drawn tangent to the anterior and posterior walls of the acetabulum and the true sagittal plane (Fig. 4).
CT acetabular version measurement technique. The axial cut extending through the center of a best fit circle on the central coronal reconstructed cut (inset image) was used to calculate the equatorial acetabular version. The angle between a line drawn tangent to the anterior and posterior walls of the acetabulum and a true sagittal line was the CT acetabular equatorial version angle (20° in this example)
Statistical analysis
We used a similar analysis strategy for both p/a ratio and TAD. We describe the one for TAD, as the one for p/a ratio is parallel. We fit a general linear mixed model with an unstructured covariance, CT equatorial version as the outcome, and hip, TAD and hip by TAD interaction as predictors, in the full model in every cell. We used planned, backwards, stepwise analysis to examine the utility of including hip, and hip by TAD interaction in the model. In the final and best fitting model, we used a Wald test with Kenward Roger degrees of freedom [17] to assess whether TAD was significantly associated with CT equatorial version, and to estimate the strength of the association between TAD and CT equatorial version, to produce 95 % prediction intervals, and to provide the prediction equation.
To assess the ability of TAD and p/a ratio to predict the gold standard of CT-measured excessive acetabular anteversion (>20°), we used paired receiver operating characteristic (ROC) curve analysis. We estimated the accuracy of both methods, relative to CT, using the area under the ROC curve (AUC), as a measure of diagnostic accuracy. We compared the accuracy of TAD and p/a ratio using a test for the difference in AUC [18]. We used the Youden index to determine the best cut points for categorizing excessive acetabular anteversion [19] by p/a ratio and TAD, respectively. For each radiographic measure, we report the optimal cut point and its associated specificity and sensitivity.
Results
The average acetabular version in our study group was 20.36° (range, 10–34°). Fifty-five hips had normal equatorial version (13–20°), 49 hips were anteverted (>20°) and 6 hips were retroverted (<13°). The average TAD in our study group was 15.87 (range, 0–32). The average p/a ratio in our study group was 1.98 (range, 1–8.37).
There was no significant difference between TAD measurements for right hips compared to left hips (F = 0.94, ndf = 1, ddf = 37.2, p = 0.34), and the association between TAD and CT acetabular version was independent of which hip (right versus left) was measured (F = 0.91, ndf = 1, ddf = 43.3, p = 0.35). TAD was significantly associated with CT equatorial version (β = 0.46, 95 % CI = (0.33, 0.60), t = 6.80, p < 0.0001). The mixed model fit (Fig. 5a) demonstrates good accuracy for the prediction of CT equatorial version from TAD (Fig. 5b). For every one unit increase in TAD, CT equatorial version increases by 0.46. The predictive model is:
There was no significant difference between p/a ratio measurements for right hips compared to left hips (F = 0.12, ndf = 1, ddf = 50.3, p = 0.73), and the association between p/a ratio and CT acetabular version was independent of which hip (right versus left) was measured (F = 1.40, ndf = 1, ddf = 49.7, p = 0.24). P/a ratio was significantly associated with CT equatorial version (β = 3.49, 95 % CI = (2.42, 4.57), t = 6.49, p < 0.0001). The mixed model fit (Fig. 6a) demonstrates good accuracy for the prediction of CT equatorial version from p/a ratio (Fig. 6b). For every one-unit increase in p/a ratio, CT equatorial version increases by 3.49. The predictive model is:
Figure 7 shows the ROC curves for p/a ratio and TAD. The ROC AUC for TAD was 0.81 (0.72, 0.89), and AUC for p/a ratio was 0.84 (0.76, 0.91). The AUCs for TAD and p/a ratio were not significantly different (χ 2 = 0.55, p = 0.46).For TAD, a cutpoint of 17 mm had a sensitivity of 0.73 and a specificity of 0.82 in predicting CT derived-excessive acetabular anteversion.
Discussion
Recognition of abnormal acetabular version in patients with hip pain is critical in forming an appropriate treatment plan. Although CT of the pelvis and hip has gained acceptance from hip preservation surgeons and MSK radiologists for accurate assessment of acetabular version, reliable and quantitative radiographic measures have not been widely adopted. Several measurement techniques have reported accurate predictive power when compared to CT acetabular version [2, 3, 14] but clinical, point of care assessment has not been widely adopted related to the complicated nature of these measurements. There is a need for intuitive, easy, and easily quantitated radiographic assessments.
Our results validate a new and simple radiographic method, TAD, for assessing acetabular equatorial version. In addition, we wanted to compare the performance of TAD to an existing, but more complex, radiographic assessment of acetabular version, the p/a ratio [3]. Both techniques are predictors of CT acetabular version and ROC curve analyses of these techniques demonstrate high accuracy approaching 85 % of the gold standard, CT acetabular version. No statistically significant difference exists between the two tools in the ability to predict CT acetabular version, however some intrinsic differences between the measurements themselves became apparent during our study. For example, it was recognized that the p/a ratio is partially dependent on the shape of the acetabular articular surface in addition to its anteroposterior orientation, while TAD is not as susceptible to this factor. Therefore, dysplastic, flattened acetabula with underdeveloped anterior walls will have an abnormally high ratio (normal P divided by abnormally small A, resulting in a larger ratio), skewed out of proportion to the actual degree of acetabular version. This accounted for our outlier p/a ratio of 8.75 in a patient with severe hip dysplasia. The TAD measurement, in contrast to the p/a ratio, reflects only the absolute distance between the anterior and posterior walls, and is not affected by the shape of the acetabular articular surface. Because of this, p/a ratio may overpredict the degree of acetabular anteversion in patients with severe hip dysplasia. Our study did not include enough patients with severe dysplasia to fully evaluate this phenomenon.
Several previously described radiographic tools have shown accuracy in predicting acetabular version. In 2006, Jamali et al. investigated a radiographic measurement adapted from a method originally described by Meunier in 1987 [2]. In their study of cadaveric specimens, radiographic acetabular version was measured on AP pelvis radiograph by first drawing a horizontal line (C) connecting the center of the two acetabula and drawing a circle of best fit outlining the acetabular diameter. The intersection of the posterior wall and anterior wall and line C were identified as P and A, respectively. Vertical lines intersecting points P and A were drawn perpendicular to line C. The superior and inferior intersection points of the vertical lines with the circle of best fit of the acetabular diameter were labeled A′, A″, P′ and P″, respectively. An angle (A″-P′-P″) formed by connecting these points was the radiographic acetabular version [2]. Although this method produced an angle that highly correlated with CT acetabular version, its complicated and confusing nature has limited its use. In their analysis, Jamali et al. also analyzed a simpler measurement, the ratio of the distance between the anterior and posterior walls, and the diameter of the acetabulum. This less complicated measurement was also reported to highly correlate with CT acetabular version in their study, and is similar to our TAD measurement.
In 2012, Siebenrock introduced two radiographic measurements of total anterior wall coverage and total posterior wall coverage, the anterior wall index (AWI) and the posterior wall index (PWI) [14]. These were obtained by first drawing a circle of best fit around the femoral head and drawing a line down the axis of the femoral neck. The distance between the points along the line intersecting the center of the circle and the anterior wall, and the distance between the points along the line intersecting the center of the circle and the posterior wall was determined. These distances were each divided by the radius of the circle to yield the respective AWI and PWI. The AWI and PWI measurements highly correlated with the total anterior and posterior coverage as determined by a validated computer model in their study population of patients with symptomatic hip disease. These tools may represent a less direct measure of acetabular version compared to TAD and the p/a ratio.
In 2013, Koyama et al. examined the p/a ratio among a population of patients with idiopathic osteonecrosis [3]. This was also shown to highly correlate with central acetabular version, and is more straightforward than the A″-P′-P′″ angle proposed by Jamali et al. Therefore, we chose this existing tool to include in our study as a measure of validated performance against which TAD could be compared. Also, by assessing this tool in our distinct patient population, we showed that the p/a ratio is generalizable to symptomatic patients with FAI and hip dysplasia. However, we felt that the p/a ratio, although an improvement on prior radiographic tools in terms of complexity of the measurement, was still somewhat cumbersome and time-consuming. In our experience, TAD was significantly quicker and easier to perform compared to the p/a ratio.
One of the strengths of our study is the development of a conversion equation that could be applied in the clinic to allow a semiquantitative estimate of acetabular version based on TAD. A slight rounding of the TAD conversion factor as reported in the previous, allows an easily memorable conversion of:
The signs of acetabular overcoverage and acetabular retroversion (acetabular cross over, posterior wall sign, and ischial spine sign) have been well described and can point the treating physician towards femoroacetabular impingement as a contributing etiology to hip pain. Although these signs have clinical utility, they lack sensitivity and specificity and are focused on local or global acetabular retroversion. Excessive acetabular anteversion is being increasingly recognized as an important finding in adolescent and adult hip pain. Excessive acetabular anteversion can contribute to anterior femoral head undercoverage and allow excessive anterior force from the femoral head on the anterior hip constraints (capsule, labrum and iliopsoas tendon), contributing to iliopsoas (IP) impingement [20–22]. This subset of patients is important to recognize as typical treatment of anterior IP tendon pain (tenotomy) can have profound, and sometimes catastrophic, effects in those patients who are undercovered anteriorly and relying on the IP tendon as a constraint to dislocation or subluxation. In these patients with excessive acetabular anteversion, the TAD measurement is particularly useful, and could be easily applied at the point of clinical care, avoiding mistreatment in this increasingly recognized subset of patients. Using limits of acetabular anteversion established by a number of authors [1, 2, 23], we defined excessive acetabular anteversion as greater than 20°, and used cutpoint analysis to optimize sensitivity and specificity of TAD for detecting excessive acetabular anteversion. Our analysis yielded an optimum TAD cutpoint of 17 mm.
Of note, the average acetabular version in our study was 20.36°, minimally anteverted. This may reflect that our study population consisted of symptomatic patients being evaluated by our hip surgeon. This population is more likely to have abnormalities of acetabular version, specifically acetabular dysplasia and FAI, compared to the general public.
Our study has several limitations. First, the observers were not strictly blinded to the associated CT or radiograph for a given hip, potentially introducing bias. Second, no evaluation of inter- or intraobserver variability was performed, therefore the reliability and reproducibility of these tools are unknown. Third, although care was taken to account for pelvic tilt in the axial or coronal plane to arrive at a true pelvic horizontal, no correction was performed for sagittal plane pelvic tilt for CT studies. Correction of sagittal pelvic tilt, through multiplanar reformatting to align the anterior superior iliac spine with anterior margin of the pubic bodies, has been suggested to increase accuracy of acetabular version measurements [5, 23, 24]. Fourth, although our initial study population had several patients with equatorial acetabular version of less than 10° (equatorial acetabular retroversion), none of these patients had AP pelvic radiograph that passed quality measures. As a result, our final study cohort did not contain any patients with significant equatorial acetabular retroversion so the performance of these measurements in cases of equatorial acetabular retroversion is unknown. Finally, our population consisted of patients being evaluated for hip pain, specifically for suspected femoroacetabular impingement or hip dysplasia. Therefore, the results of this study may not be generalizable to asymptomatic patients or patients with alternative etiologies of hip pain.
Our study has validated a new and easy radiographic measure of acetabular version. TAD shows excellent correlation to CT version measurements, is equivalent in performance to the previously validated but more cumbersome p/a ratio, and is easy to measure at the point of clinical care. TAD is particularly well suited to assess excessive acetabular anteversion as there is no current radiographic sign or tool to alert the clinician to this important subset of hip pain patients. A TAD of greater than 17 mm has excellent sensitivity and specificity in detecting equatorial acetabular anteversion of greater than 20°.
References
Dolan MM, Heyworth BE, Bedi A, Duke G, Kelly BT. CT reveals a high incidence of osseous abnormalities in hips with labral tears. Clin Orthop Relat Res. 2011;469(3):831–8.
Jamali AA, Mladenov K, Meyer DC, Martinez A, Beck M, Ganz R, et al. Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of the “cross-over-sign”. J Orthop Res. 2007;25(6):758–65.
Koyama H, Hoshino H, Suzuki D, Nishikino S, Matsuyama Y. New radiographic index for evaluating acetabular version. Clin Orthop Relat Res. 2013;471(5):1632–8.
Reikeras O, Bjerkreim I, Kolbenstvedt A. Anteversion of the acetabulum and femoral neck in normals and in patients with osteoarthritis of the hip. Acta Orthop Scand. 1983;54(1):18–23.
Tonnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81(12):1747–70.
Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis—what the radiologist should know. AJR Am J Roentgenol. 2007;188(6):1540–52.
Wenger DE, Kendell KR, Miner MR, Trousdale RT. Acetabular labral tears rarely occur in the absence of bony abnormalities. Clin Orthop Relat Res. 2004;426:145–50.
Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87(7):1012–8.
Salter RB. The classic. Innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip by Robert B. Salter, J. Bone joint surg. (Brit) 43B:3:518, 1961. Clin Orthop Relat Res. 1978;137:2–14.
Beltran LS, Rosenberg ZS, Mayo JD, De Tuesta MD, Martin O, Neto LP, et al. Imaging evaluation of developmental hip dysplasia in the young adult. AJR Am J Roentgenol. 2013;200(5):1077–88.
Li PL, Ganz R. Morphologic features of congenital acetabular dysplasia: one in six is retroverted. Clin Orthop Relat Res. 2003;416:245–53.
Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum: a cause of hip pain. J Bone Joint Surg Br. 1999;81(2):281–8.
Kalberer F, Sierra RJ, Madan SS, Ganz R, Leunig M. Ischial spine projection into the pelvis: a new sign for acetabular retroversion. Clin Orthop Relat Res. 2008;466(3):677–83.
Siebenrock KA, Kistler L, Schwab JM, Buchler L, Tannast M. The acetabular wall index for assessing anteroposterior femoral head coverage in symptomatic patients. Clin Orthop Relat Res. 2012;470(12):3355–60.
Jesse MK, Petersen B, Strickland C, Mei-Dan O. Normal anatomy and imaging of the hip: emphasis on impingement assessment. Semin Musculoskelet Radiol. 2013;17(3):229–47.
Clohisy JC, Carlisle JC, Beaule PE, Kim YJ, Trousdale RT, Sierra RJ, et al. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am Vol. 2008;90 Suppl 4:47–66.
Kenward M, Roger J. An improved approximation to the precision of fixed effects from restricted maximum likelihood. Comput Stat Data Anal. 2009;53(7):2583–95.
Zhou X-h, McClish DK, Obuchowski NA. Statistical methods in diagnostic medicine. 2nd ed. Hoboken: Wiley; 2011. p. 184.
Perkins NJ, Schisterman EF. The inconsistency of “optimal” cutpoints obtained using two criteria based on the receiver operating characteristic curve. Am J Epidemiol. 2006;163(7):670–5.
Domb BG, Lareau JM, Baydoun H, Botser I, Millis MB, Yen YM. Is intraarticular pathology common in patients with hip dysplasia undergoing periacetabular osteotomy? Clin Orthop Relat Res. 2014;472(2):674–80.
Blankenbaker DG, Tuite MJ, Keene JS, del Rio AM. Labral injuries due to iliopsoas impingement: can they be diagnosed on MR arthrography? AJR Am J Roentgenol. 2012;199(4):894–900.
Aly AR, Rajasekaran S, Obaid H. MRI morphometric hip comparison analysis of anterior acetabular labral tears. Skelet Radiol. 2013;42(9):1245–52.
Maruyama M, Feinberg JR, Capello WN, D’Antonio JA. The Frank Stinchfield award: morphologic features of the acetabulum and femur: anteversion angle and implant positioning. Clin Orthop Relat Res. 2001;393:52–65.
Chong le R, Too CW. Comparison of acetabular version angle measurements between prone and reformatted supine computed tomography images. Skelet Radiol. 2014;43(3):289–95.
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nitschke, A., Lambert, J.R., Glueck, D.H. et al. Validation of a new radiographic measurement of acetabular version: the transverse axis distance (TAD). Skeletal Radiol 44, 1679–1686 (2015). https://doi.org/10.1007/s00256-015-2225-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-015-2225-2