Abstract
Background
The role of the synovial biopsy in the preoperative diagnosis of a periprosthetic joint infection (PJI) of the hip has not been clearly defined.
Questions/purposes
We asked whether the value of a biopsy for a PJI is greater than that of aspiration and C-reactive protein (CRP).
Methods
Before revision in 100 hip endoprostheses, we obtained CRP values, aspirated the joint, and obtained five synovial biopsy samples for bacteriologic analysis and five for histologic analysis. Microbiologic and histologic analyses of the periprosthetic tissue during revision surgery were used to verify the results of the preoperative diagnostic methods. The minimum followup was 24 months (median 32; range, 24–47 months).
Results
Forty-five of the 100 prostheses were identified as infected. The biopsy, with a combination of the bacteriologic and histologic examinations, showed the greatest diagnostic value of all the diagnostic procedures and led to a sensitivity of 82% (95% CI, ± 11%), specificity of 98% (95% CI, ± 4%), positive predictive value of 97% (95% CI, ± 5%), negative predictive value of 87% (95% CI, ± 8.3%), and accuracy of 91%.
Conclusions
The biopsy technique has a greater value than aspiration and CRP in the diagnosis of PJI of the hip (Masri et al. J Arthroplasty 22:72–78, 2007). In patients with a negative aspirate, but increased CRP or clinical signs of infection, we regard biopsy to be preferable to just repeating the aspiration.
Level of Evidence
Level II prognostic study. See Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A periprosthetic joint infection (PJI) is a severe complication of hip replacement surgery, with an incidence ranging between 1% and 3%, and has many consequences [3, 18, 22]. Thus, accuracy of the preoperative diagnosis of possible infection becomes especially important in patients with loosened and painful hip endoprostheses [12].
Whereas early infections (occurring within the first 4 weeks after implantation) usually cause local and systemic inflammatory reactions, these responses do not always occur in patients with late infection [52]. This makes the diagnosis of late periprosthetic infections more difficult. The AAOS Work Group has developed guidelines for the diagnosis of PJI and pointed out that C-reactive protein (CRP) and aspiration are important methods in the diagnosis of PJI [1]. Aspiration allows precise identification of bacteria and their antibiotic resistance pattern and provides information for planning antibiotic therapy before surgery. It also gives the surgeon the opportunity to add bacteria-specific antibiotics to the bone cement during one-stage or two-stage revision operations [5, 13, 15, 16, 20, 29, 30, 47, 49]. However, the literature reveals a large variance in the diagnostic value of this method. Sensitivity varies from 12% to 89% and specificity from 50% to 100% (Table 1). Lower sensitivities and specificities have been attributed to contamination of the aspirated fluid with microorganisms of the skin, for example, to bacteria that are difficult to grow in culture, or to failure to discontinue antibiotic therapy before the fluid was aspirated [30, 44]. Moreover, the method of joint aspiration analysis varies among authors, namely in the choice of culture medium and, in particular, in the duration of the incubation period [5, 21, 26, 40, 49].
In a previous study, 145 knee prosthesis exchanges were studied and preoperative synovial biopsy was superior to joint aspiration and CRP for diagnosing periprosthetic infections [17]. Even though the AAOS Work Group has developed guidelines for the diagnosis of PJI [1], it is unclear what choices or combinations of testing methods provide the highest sensitivity, specificity, and positive predictive value (PPV) for periprosthetic hip infections.
Therefore we asked: (1) which diagnostic procedure (laboratory blood test of CRP, aspiration, or operative biopsy with the combination of bacteriologic and histologic analyses of the synovial tissue) has the highest diagnostic value, (2) what is the diagnostic value of CRP, aspiration, and bacteriologic and histologic examinations of the synovial tissue alone, (3) does combining different analyzing techniques (CRP, aspiration, and operative biopsy) improve the value in diagnosing PJI of hip endoprostheses, and (4) what complication rate is associated with the biopsy technique.
Patients and Methods
We prospectively followed all 100 patients who underwent revision surgery of a hip endoprosthesis owing to component loosening between January 2008 and June 2009. Prosthetic loosening was defined when the patient had pain and when the radiographic images fulfilled the criteria defined by Brand et al. [8] and Manaster [32]: (1) progressive widening of the lucent zone in sequential studies, (2) greater than 2 mm lucency at the cement-bone interface or metal-bone interface (in noncemented prostheses), (3) any cement fracture, or (4) changes of component position of a minimum of 4 mm or 4°. Of the 100 patients, three had local clinical signs of infection with an accompanying fistula. The mean age of the patients was 68 ± 11 years (range, 42–88 years); 49 patients were female and 51 were male. The BMI was 27 ± 4 (range, 17–44). The primary diagnosis was osteoarthritis in 93 patients and rheumatoid arthritis in seven. Before revision all patients underwent a diagnostic operation that involved aspiration of the hip and synovial biopsy using a mini-incision anterolateral approach. The diagnostic operation was performed a median of 41 months (range, 4–312 months) after the primary implantation (77 patients) or the last revision operation (23 patients; 16 cup revisions, five stem revisions, and two total revisions because of aseptic component loosening). The minimum followup was 24 months (median, 32 months; range, 24–47 months). All subjects gave informed consent to participate in the study and the protocol was approved by the research ethics board of our hospital.
CRP values were determined before surgery. None of the patients was given any antibiotics during the 4 weeks preceding the aspiration and biopsy according to the recommendation of Lonner et al. [31] and Fink [15] to minimize the risk of antibiotic-induced false-negative results. For the three patients with fistulae who had been prescribed antibiotics for a suspected late infection of the hip prosthesis, the antibiotic treatment was withdrawn and the patients examined at weekly intervals until the date of the operation. They also were informed of the required management should a systemic infection arise, although none occurred in any of the patients.
The joint aspiration and biopsy were performed under sterile conditions in the operating room with the patient under general anesthesia. The aspiration was performed using an anterolateral approach under image intensifier control as described by Kilcoyne and Kaplan [27]. If no fluid was aspirated, the aspiration was repeated using a superolateral approach according to McCurdy et al. [35] (10 times), and if this second aspiration was unsuccessful, 10 mL of normal saline was injected and aspirated according to Ali et al. [2] and Williams et al. [53] (two times). The harvested fluid was immediately injected into vials containing BD BACTEC-PEDS-PLUSTM/F-Medium (Becton Dickinson, Heidelberg, Germany). Originally designed to optimize blood culturing from pediatric patients, this medium was used because it has proven superior to standard blood culture media in recovery and time to detection of clinically important microorganisms in samples of low volumes [17, 39]. The biopsy samples were obtained using arthroscopic biopsy forceps introduced via a mini-incision anterolateral approach of 1 cm under image intensifier control, and were taken from the synovial lining and the periprosthetic tissue in five different areas of the hip, close to the prosthesis. Afterward five tissue samples were obtained for histologic examinations. Prophylactic perioperative antibiotics as a single dose of cephalosporin (2 g of cefazolin) were administered once all samples had been obtained.
The biopsy samples were each placed in sterile tubes and transferred together with the aspirated fluid to the microbiologic laboratory within an hour of sampling. Patient specimens were processed immediately after arrival at the laboratory. The culture vials were treated with Fastidious Organism Supplement (FOS) (Becton Dickinson), a growth enhancer that improves cultivation of fastidious organisms from normally sterile body fluids other than blood, according to the manufacturer’s instructions and incubated using the BD BACTECTM 9050 automatic blood culture system (Becton Dickinson). Cultures were discontinued and considered negative if no growth was reported after 14 days according to previous studies [24, 45, 49]. Cultivation of tissue samples was performed essentially as previously described [4, 24, 42, 49, 52]. Media were checked daily for bacterial growth. Broths that remained clear were incubated for 14 days until the specimen was considered negative as previously described [24, 45, 49]. Turbid broth was subcultured on appropriate agar plates. Microorganisms were identified by standard microbiologic procedures including biochemical characterization with the API system (BioMerieux, Nuertingen, Germany). Antibiotic susceptibility testing was performed by disk diffusion or dilution methods according to the Clinical and Laboratory Standards Institute (CLSI) guidelines [10].
The results of each series of tests (aspiration, bacteriology of the biopsy, histology of the biopsy, and CRP) were evaluated individually. A hip was regarded as bacteriologically positive if the same microorganism was identified in at least two samples [6]. The hip was considered histologically positive when at least five polymorphonuclear leukocytes per high power field (×400) were identified in one of 10 such fields [37, 38, 42]. A CRP value greater than 10 mg/L was regarded as positive [9, 46, 51].
For interpretation of the biopsy data using combined bacteriology and histology results, a synovial membrane sample was regarded as positive (infected hip arthroplasty) when at least one of the following conditions had been fulfilled: (1) observation of the same microorganism in at least two of the cultures, and (2) observation of a microorganism in at least one sample and of at least five polymorphonuclear leukocytes per high power field (×400) in the associated histologic preparation as previously described [4, 31, 37, 38, 42, 52].
In accordance with Virolainen et al. [52], the growth of a microorganism in only one culture without any histologic signs of infection (less than five polymorphonuclear leukocytes per high power field) was regarded as a contamination.
During the revision surgery we took samples from five areas close to the prosthesis (synovial lining and periprosthetic connective tissue membrane) and incubated the samples for 14 days as described above. In addition, we obtained five samples from the same areas for histologic assessment. Perioperative antibiotics were administered once all the samples had been taken. The histologic analysis and interpretation of the microbiologic and histologic results alone and in combination were the same as for the diagnostic biopsy technique.
The diagnosis obtained from the revision surgery samples was regarded as the definitive result with respect to periprosthetic infection and was used to evaluate the diagnostic methods (joint aspiration, biopsy, and CRP). Of the 100 revision operations, 55 were classified during surgery as aseptic and 45 as septic, whereby the three patients with fistulae were rated as having PJI by the tissue analyses of the revision surgery. In 42 cases one microorganism was identified (Table 2). In three patients, the prosthesis was infected with two microorganisms (Propionibacterium acnes and Streptococcus zooepidemicus, Propionibacterium acnes and Staphylococcus capitis, and Staphylococcus epidermidis and Staphylococcus capitis).
During followup, we examined the patients for possible complications of the biopsy like injury of nerve of vessels, delayed wound healing, or infection (every 3 months in the first year and thereafter every 6 months). Recurrence of infection after septic revisions and occurrence of infection for aseptic revisions also were analyzed using the published criteria (to be judged infection-free at the followup, a patient had to be free of clinical signs for infection [elevated temperature, local pain, redness, warmth, sinus tract infection], have a CRP level less than 10 mg/L, and no radiographic sign of osteolysis) [21, 34, 54, 55].
The sensitivity (true positives/[false negatives + true positives]), the specificity (true negatives/[false positives + true negatives]), PPV (true positives/[true positives + false positives]), and negative predictive value (NPV) (true negatives/[true negatives + false negatives]) of each diagnostic method (aspiration, microbiologic examination, histologic examination, CRP, and microbiologic and histologic examinations in combination for the biopsy method, and the combination of the aspiration and biopsy method as a diagnostic operation) and combination of all diagnostic methods were determined. Bayes’ equation was used to calculate these statistics [23]. The accuracy of the techniques was calculated from the sum of the true positives and true negatives divided by the number of tests that were done. All calculations were performed using SPSS for Windows (Version 10.0; SPSS, Chicago, IL, USA).
Results
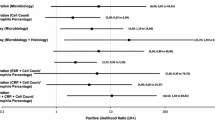
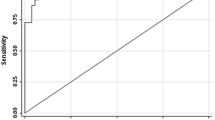
The biopsy, with a combination of the bacteriologic and histologic examinations, showed the greatest diagnostic value of all the diagnostic procedures (laboratory blood test, aspiration, or operative biopsy) investigated for identification of PJI. The combination of the bacteriologic and histologic results of the biopsy samples using previously described criteria [4, 42, 52], led to a sensitivity of 82% (95% CI, ± 11%), specificity of 98% (95% CI, ± 4%), PPV of 97% (95% CI, ± 5%), NPV of 87% (95% CI, ± 8.3%) and accuracy of 91% (Table 3).
Analyzing each test alone, we observed that, in the case of CRP, 28 patients from the infected group had a CRP of at least 10 mg/L, 17 did not and in nine of these 17, the CRP level was at a normal level. In the group with noninfected joints, 13 patients had a CRP of at least 10 mg/L and 42 had a CRP less than 10 mg/L (Table 4). These data calculated to a sensitivity of 64% (95% CI, ± 14%), specificity of 75% (95% CI, ± 12%), PPV of 67% (95% CI, ± 14%), NPV of 72% (95% CI, ± 12%), and accuracy of 70% (Table 3). Aspiration had a sensitivity of 64% (95% CI, ± 14%), specificity of 96% (95% CI, ± 5%), PPV of 94% (95% CI, ± 9%), NPV of 77% (95% CI, ± 10%), and accuracy of 82% (Table 3). The bacteriologic examination of the biopsy samples alone (identification of the same microorganism in at least two samples [6]) and the histologic examinations alone [31, 37, 38, 42] showed better diagnostic values than either CRP or aspiration (Tables 3, 4).
When combining the results of the biopsy with those of the aspiration, the result changed for two patients from false negative to a true positive result which slightly increased the diagnostic value of combining these two diagnostic methods (Tables 3, 4). An additional combination of the CRP analysis or other combinations of the diagnostic methods did not improve the results (Table 3).
No complications occurred during this study; in particular, no infections, wound healing problems, and nerve or vascular injury were associated with this procedure. The 45 patients with infected hip prostheses subsequently underwent two-stage revision surgery whereby bacteria-specific antibiotics were added to the bone cement of the spacer and bacteria-specific systemic antibiotic therapy was initiated. During the subsequent followup from 24 to 47 months (median, 32 months), none of the patients had a recurrent infection.
Discussion
Before revising loosened or painful hip prostheses an examination for PJI should be done because the presence of PJI would result in substantial changes in the subsequent therapeutic procedures [15, 45]. The AAOS Work Group has developed guidelines for methods to diagnose PJI [1]. However, it is unclear what choices or combinations of testing methods provide the highest sensitivity, specificity, and PPV for periprosthetic hip infections. Therefore we asked: (1) which diagnostic procedure (CRP, aspiration, or operative biopsy with combination of bacteriologic and histologic analyses of the synovial tissue) has the highest diagnostic value, (2) what is the diagnostic value of CRP, aspiration, bacteriologic and histologic examinations of the synovial tissue alone, (3) does combining different analyzing techniques (CRP, aspiration, and operative biopsy) improve the value in diagnosing PJI of loosened hip endoprostheses, and (4) what complication rate is associated with the biopsy technique.
We recognize some limitations of our study. First, seven patients with rheumatoid arthritis were included in this study and three of them had, owing to the nature of their disease, increased levels of CRP which may influence the diagnostic value of CRP in our study for detecting or ruling out PJI. However, the value of a diagnostic test also is related to its usefulness on a daily basis and this would be greatly reduced if particular patient groups had to be excluded from such a test. Moreover, the AAOS Work Group did not exclude patients with rheumatoid arthritis from their recommendations [1]. In our study, four patients with rheumatoid arthritis had infected hip endoprostheses, but only one of them had an increased CRP level greater than 10 mg/L. Of the three patients with rheumatoid arthritis with aseptic loosening, two had elevated CRP levels greater than 10 mg/L. Second, the fluid cell count of the aspirated synovial fluid, which also seems to be a sensitive diagnostic tool for PJI, was not performed in our study [1, 12, 20]. The reason for this was because the volume of fluid obtained from the aspiration was not always sufficient for both investigations (bacteriologic analysis and cell count) to be performed. Because we wanted to compare the microbiologic analyses of the aspirates and the biopsies, we decided to forego the cell count. In general, it seems that the more diagnostic tools that can be combined to investigate the presence of PJI, the better, because none of the methods alone has 100% accuracy whereas the combination of several methods clearly increases the accuracy [1, 17]. In addition to its diagnostic value, bacteriologic examination of the aspirated fluid, like that of the tissue obtained during biopsy, has the advantage that the microorganisms can be identified before revision surgery and antibiotic susceptibility testing is possible. This means that local and systemic antibiotic therapy specific for the microorganisms can be chosen for the revision surgery.
In our study of 100 hip prosthesis revision operations we found a synovial biopsy has the greatest diagnostic value and is superior to aspiration and CRP as a preoperative diagnostic method in its ability to accurately confirm or to rule out the presence of PJI of the hip. Thus the results of a previous study for knee arthroplasty were confirmed [17]. However, the validity of the biopsies from the hip was less than that obtained from the earlier study of the knee [17]. In particular, the sensitivity and NPV of the biopsy was less for the hip arthroplasty (84% and 89%) than for the knee arthroplasty (100% each) [17]. One possible reason for this is that biopsy of the knee can be performed at many more places adjacent to the prosthesis than the hip, where only the neck and head of the prosthesis and inlay of the acetabular cup are easily accessible. The results of the biopsies of the hip tissue in this study reflect those reported by Malhorta and Morgan [33] and Williams et al. [53]. Malhotra and Morgan [33] performed biopsies of 41 hip prostheses with biopsy needles and did bacteriologic and histologic examinations of the tissue. They did not report the number of biopsies per joint, the method of examination, or the duration of the incubation. They reported a sensitivity of 80%, specificity of 100%, PPV of 100%, and accuracy of 97%. Williams et al. [53] also used needles to biopsy 273 hip prostheses, taking three biopsy samples from each joint and incubating the tissue for 7 days. No histologic examinations were done. They reported a sensitivity of 80%, specificity of 94%, PPV of 74%, NPV of 94%, and accuracy of 88%. They did not find any advantage in using the biopsy-based analysis rather than the aspiration-based method but this might have been related to the lack of histologic data and the relatively short period of incubation of 7 days [53]. To identify microorganism in biopsy samples or aspirations, the length of the incubation period is important because the bacteria that cause a periprosthetic infection occur only in very low numbers in the biofilm and often are in a sessile form that is very slow growing [11, 41]. The incubation period we used was 14 days and corresponds to the recommendations of others [24, 45, 49].
The predictive power of the CRP value in our study was less than that reported by other authors [9, 46, 51]. At a cut-off point of 10 mg/L Schinsky et al. [46], Tohtz et al. [51], and Buttaro et al. [9] regarded the CRP level as an important diagnostic parameter and found a sensitivity between 58% and 94%, specificity between 80% and 91%, PPV between 55% and 61%, NPV between 82% and 96%, and accuracy between 73% and 78%. Moreover, the AAOS Work Group pointed out in their guidelines that aspiration or biopsy should be done only if the CRP is increased [1]. A possible explanation for the lower value in our study may be that seven patients with rheumatoid arthritis were included in our collective as mentioned in the limitations. However, 17 of the 45 patients with PJIs had CRP levels less than 10 mg/L (including three of the four patients with rheumatoid arthritis) and in nine of these 17, the CRP was at a normal level. Moreover, the cut-off point for the CRP value associated with an infection probably is influenced by actual distribution of the individual values in any one collective, so that different patient collectives will have different cut-off points. The latter might be one explanation for the different levels of importance attached to CRP as a diagnostic tool [52].
Many authors recommend joint aspiration on a regular basis before a revision operation is done, even if there is no indication that infection might be present, as this method has a high diagnostic value and has the advantage that, in addition to screening of periprosthetic infections, the microorganisms can be identified and development of an antibiogram is possible [19, 44, 47–49, 53]. The parameters for the joint aspiration technique in our study were calculated as 64% sensitivity, 96% specificity, 94% PPV, 77% NPV, and 82% accuracy. These results are comparable to those of other studies (Table 1). An inappropriate incubation time may be the reason for the poor sensitivity of tests with preoperative joint aspiration fluids reported in other studies, namely 12% reported by Johnson et al. [26] and 28% by Teller et al. [50]. However, many publications do not comment on the duration of the incubation [2, 13, 25, 28, 29, 40], which suggests that in such cases the samples would have been incubated for 3 days, which is the standard time for bacterial incubations.
Tissue samples also were obtained for histologic examination during the biopsy. Histologic examination is a diagnostic procedure that is associated with high sensitivity and specificity and can provide confirmatory evidence for the presence or absence of an infection. In our study, the sensitivity was 62% and specificity was 100%. Some authors have reported sensitivities and specificities of as much as 100% [4, 14, 51].
Even though we did not see any complications with the biopsy technique, this operative procedure is associated with risks of causing infection and vascular or nerve injury. In the few studies of biopsy techniques, no complications have been described. However, for arthroscopy of the hip in femoroacetabular impingement using a similar approach, a complication rate of 1.7% with nerve injuries of 0.5% have been described, although infection or vascular injuries were not mentioned [7, 33, 54]. Therefore this should be taken into account when biopsy is being considered. Moreover, we cannot totally exclude the possible complication of the biopsy technique causing damage, such as scratches to the prosthetic head that may occur owing to the blind technique. Because our study addressed only patients with loosened components, where revision surgery was indicated, any iatrogenic damage to the prostheses during the biopsy was of lesser importance in our patient collective.
The data and analysis suggest biopsy is superior to aspiration and CRP as a preoperative diagnostic method for PJI of the hip. The diagnostic biopsy technique we used has the advantage that it is a combination of diagnostic methods, that is, bacteriologic and histologic examinations of several samples of synovial and periprosthetic connective tissue. Moreover, precise identification of bacteria and the antibiotic resistance pattern is possible for planning the antibiotic therapy before revision surgery and also gives the surgeon the opportunity to add bacteria-specific antibiotics to the bone cement during one-stage or two-stage revision operations [15, 49]. As only minor surgery is involved in the biopsy and the method is accurate, this has led to its use in our clinic and with the diagnostic algorithm for periprosthetic infection in patients with loosened hip endoprostheses. We perform serologic analysis of CRP, radiographic examinations, and aspiration (for microbiologic and, if enough fluid can be obtained, also for cell count analysis) on a regular basis in loose and painful hip arthroplasties. In patients with negative aspiration, but increased CRP or clinical signs of infection, we regard biopsy to be preferable to repeating an aspiration alone. As the combination of aspiration and biopsy slightly improved diagnostic effectiveness in our study, it seems appropriate to combine diagnostic methods and to perform an aspiration every time a biopsy is performed.
References
AAOS Work Group. The diagnosis of periprosthetic joint infections of the hip and knee: guideline and evidence report. Available at: http://www.aaos.org/research/guidelines/PJIguideline.pdf. Accessed June 21, 2012.
Ali F, Wilkinson JM, Cooper JR, Kerry RM, Hamer AJ, Norman P, Stockley I. Accuracy of joint aspiration for the preoperative diagnosis of infection in total hip arthroplasty. J Arthroplasty. 2006;21:221–226.
Antti-Poika I, Josefsson G, Konttinen Y, Lidgren L, Santavirta S, Sanzén L. Hip arthroplasty infection: current concepts. Acta Orthop Scand. 1990;61:163–169.
Atkins BL, Athanasou N, Deeks JJ, Crook DW, Simpson H, Peto TE, McLardy-Smith P, Berendt AR. Prospective evaluation of criteria for microbiological diagnosis of prosthetic-joint infection at revision arthroplasty. The OSIRIS Collaborative Study Group. J Clin Microbiol.1998;36:2932–2939.
Barrack RL, Harris WH. The value of aspiration of the hip joint before revision total hip arthroplasty. J Bone Joint Surg Am. 1993;75:66–76.
Bori G, Soriano A, García S, Mallofré C, Riba J, Mensa J. Usefulness of histological analysis for predicting the presence of microorganisms at the time of reimplantation after hip resection arthroplasty for the treatment of infection. J Bone Joint Surg Am. 2007;89:1232–1237.
Botser IB, Smith TW Jr, Nasser R, Domb BG. Open surgical dislocation versus arthroscopy for femoroacetabular impingement: a comparison of clinical outcomes. Arthroscopy. 2011;27:270–278.
Brand RA, Pederson DR, Yoder SA. How definition of “loosening” affects the incidence of loose total hip reconstructions. Clin Orthop Relat Res. 1986;210:185–191.
Buttaro MA, Tanoira I, Comba F, Piccaluga F. Combining C-reactive protein and Interleukin-6 may be useful to detect periprosthetic hip infection. Clin Orthop Relat Res. 2010;468:3263–3267.
CLSI. Performance Standards for Antimicrobial Susceptibility Testing. Twentieth Informational Supplement. CLSI document M100-S20. Wayne, PA: Clinical and Laboratory Standards Institute; 2010.
Costerton JW. Biofilm theory can guide the treatment of device-related orthopaedic infections. Clin Orthop Relat Res. 2005;437:7–11.
Della Valle CJ, Zuckermann JD, Di Cesare PE. Periprosthetic sepsis. Clin Orthop Relat Res. 2004;420:26–31.
Fehring TK, Cohen B. Aspiration as a guide to sepsis in revision total hip arthroplasty. J Arthroplasty. 1996;11:543–547.
Feldman DS, Lonner JH, Desai P, Zuckerman JD. The role of intraoperative frozen sections in revision total joint arthroplasty. J Bone Joint Surg Am. 1995;77:1807–1813.
Fink B. Revision of late periprosthetic infections of total hip endoprostheses: pros and cons of different concepts. Int J Med Sci. 2009;6:287–295.
Fink B, Grossmann A, Fuerst M, Schäfer P, Frommelt L. Two-stage cementless revision of infected hip endoprostheses. Clin Orthop Relat Res. 2009;467:1848–1858.
Fink B, Makowiak C, Fuerst M, Berger I, Schäfer P, Frommelt L. The values of synovial biopsy and joint aspiration in the diagnosis of late peri-prosthetic infection of total knee replacements. J Bone Joint Surg Br. 2008;90:874–878.
Fitzgerald RH Jr. Total hip arthroplasty sepsis: prevention and diagnosis. Orthop Clin North Am. 1992;23:259–264.
Frommelt L. [Diagnosis and treatment of foreign-body-associated infection in orthopaedic surgery][in German]. Orthopäde. 2009;38:806–811.
Glithero PR, Grigoris P, Harding LK, Hesslewood SR, McMinn DJ. White cell scans and infected joint replacements: failure to detect chronic infection. J Bone Joint Surg Br. 1993;75:371–374.
Haddad FS, Muirhead-Allwood SK, Manktelow AR, Bacarese-Hamilton I. Two-stage uncemented revision hip arthroplasty for infection. J Bone Joint Surg Br. 2000;82:689–694.
Harris WH, Sledge CB. Total hip and total knee replacement (2). N Engl J Med. 1990;323:801–807.
Heinecke A, Hultsch E, Repges R, eds. Medizinische Biometrie. Berlin, Germany: Springer; 1992.
Ince A, Rupp J, Frommelt L, Katzer A, Gille J, Löhr JF. Is “aseptic” loosening of the prosthetic cup after total hip replacement due to nonculturable bacterial pathogens in patients with low-grade infection? Clin Infect Dis. 2004;39:1599–1603.
Itasaka T, Kawai A, Sato T, Mitani S, Inoue H. Diagnosis of infection after total hip arthroplasty. J Orthop Sci. 2001;6:320–326.
Johnson JA, Christie MJ, Sandler MP, Parks PF Jr, Homra L, Kaye JJ. Detection of occult infection following total joint arthroplasty using sequential technetium-99 m HDP bone scintigraphy and indium-111 WBC imaging. J Nucl Med. 1988;29:1347–1353.
Kilcoyne RF, Kaplan P. The lateral approach for hip arthrography. Skeletal Radiol. 1992;21:239–240.
Kraemer WL, Saplys R, Waddell JP, Morton J. Bone scan, gallium scan, and hip aspiration in the diagnosis of infected total hip arthroplasty. J Arthroplasty. 1993;8:611–616.
Lachiewicz PF, Rogers GD, Thomason HC. Aspiration of the hip joint before revision total hip arthroplasty: clinical and laboratory factors influencing attainment of a positive culture. J Bone Joint Surg Am.1996;78:749–754.
Levitsky KA, Hozack WJ, Balderston RA, Rothman RH, Gluckman SJ, Maslack MM, Booth RE Jr. Evaluation of the painful prosthetic joint: relative value of bone scan, sedimentation rate, and joint aspiration. J Arthroplasty. 1991;6:237–244.
Lonner JH, Desai P, Dicesare PE, Steiner G, Zuckerman JD. The reliability of analysis of intraoperative frozen sections for identifying active infection during revision hip or knee arthroplasty. J Bone Joint Surg Am. 1996;78:1553–1558.
Manaster BJ. From the RSNA refresher courses. Total hip arthroplasty: radiographic evaluation. Radiographics. 1996;16:645–660.
Malhotra R, Morgan DA. Role of core biopsy in diagnosing infection before revision hip arthroplasty. J Arthroplasty. 2004;19:78–87.
Masri BA, Panagiotopoulos KP, Greidanus NV, Garbuz DS, Duncan CP. Cementless two-stage exchange arthroplasty for infection after total hip arthroplasty. J Arthroplasty. 2007;22:72–78.
McCurdy WE, Moore TE, Walker CW. The superolateral approach for aspiration of total hip arthroplasties. Australas Radiol. 2000;44;349–350.
Meermans G, Haddad FS. Is there a role for tissue biopsy in the diagnosis of periprosthetic infection? Clin Orthop Relat Res. 2010;468:1410–1417.
Mirra JM, Amstutz HC, Matos M, Gold R. The pathology of the joint tissues and its clinical relevance in prosthetic failure. Clin Orthop Relat Res. 1976;117:221–240.
Mirra JM, Marder RA, Amstutz HC. The pathology of failed total joint arthroplasty. Clin Orthop Relat Res. 1982;170:175–183.
Morello JA, Matushek SM, Dunne WM, Hinds DB. Performance of a BACTEC nonradiometric medium for pediatric blood cultures. J Clin Microbiol. 1991;29:359–362.
Müller M, Morawietz L, Hasart O, Strube P, Perka C, Tohtz S. Diagnosis of periprosthetic infection following total hip arthroplasty: evaluation of the diagnostic values of pre- and intraoperative parameters and the associated strategy to preoperatively select patients with a high probability of joint infection. J Orthop Surg Res. 2008;3:31
Neut D, van Horn JR, van Kooten TG, van der Mei HC, Busscher HJ. Detection of biomaterial-associated infections in orthopaedic joint implants. Clin Orthop Relat Res. 2003;413:261–268.
Pandey R, Drakouilakis E, Athanasou NA. An assessment of the histological criteria used to diagnose infection in hip revision arthroplasty tissues. J Clin Pathol. 1999;52:118–123.
Panousis K, Grigoris P, Butchler I, Rana B, Reilly JH, Hamblen DL. Poor predictive value of broad-range PCR for the detection of arthroplasty infection in 92 cases. Acta Orthop. 2005;76:341–346.
Saleh KJ, Clark CR, Sharkey PF, Goldberg VM, Rand JA, Brown GA. Modes of failure and preoperative evaluation. J Bone Joint Surg Am. 2003;85(suppl 1):21–25.
Schäfer P, Fink B, Sandow D, Margull A, Berger I, Frommelt L. Prolonged bacterial culture to identify late periprosthetic joint infection: a promising strategy. Clin Infect Dis. 2008;47:1403–1409.
Schinsky MF, Della Valle CJ, Sporer SM, Paprosky WG. Perioperative testing for joint infection in patients undergoing revision total hip arthroplasty. J Bone Joint Surg Am. 2008;90:1869–1875.
Somme D, Ziza JM, Desplaces N, Chicheportiche V, Chazerain P, Leonard P, Lhotellier L, Jacquenod P, Mamoudy P. Contribution of routine joint aspiration to the diagnosis of infection before hip revision surgery. Joint Bone Spine. 2003;70:489–495.
Spangehl MJ, Masri BA, O’Connell JX, Duncan CP. Prospective analysis of preoperative and intraoperative investigations for the diagnosis of infection at the sites of two hundred and two revision total hip arthroplasties. J Bone Joint Surg Am. 1999;81:672–683.
Steinbrink K, Frommelt L. [Treatment of periprosthetic infection of the hip using one-stage exchange surgery][in German]. Orthopäde. 1995;24:335–343.
Teller RE, Christie MJ, Martin W, Nance EP, Haas DW. Sequential indium-labeled leukocyte and bone scans to diagnose prosthetic joint infection. Clin Orthop Relat Res. 2000;373:241–247.
Tohtz SW, Müller M, Morawietz L, Winkler T, Perka C. Validity of frozen sections for analysis of periprosthetic loosening membranes. Clin Orthop Relat Res. 2010;468:762–768.
Virolainen P, Lahteenmaki H, Hiltunen A, Sipola E, Meurman O, Nelimarkka O. The reliability of diagnosis of infection during revision arthroplasties. Scand J Surg. 2002;91:178–181.
Williams JL, Norman P, Stockley I. The value of hip aspiration versus tissue biopsy in diagnosing infection before exchange hip arthroplasty surgery. J Arthroplasty. 2004;19:582–586.
Wilson MG, Dorr LD. Reimplantation of infected total hip arthroplasties in the absence of antibiotic cement. J Arthroplasty. 1989;4:263–269.
Zimmerli W, Widmer AF, Blatter M, Frei R, Ochsner PE. Role of rifampicin for treatment of orthopedic implant-related staphylococcal infections: a randomized controlled trial. Foreign-Body Infection (FBI) Study Group. JAMA. 1998;279:1537–1541.
Acknowledgment
We thank Lars Frommelt MD (Service for Infectious Diseases, Clinical Microbiology and Infection Control, ENDO-Klinik, Hamburg) for recommendations in local and systemic antibiotic therapy for treatment of the infected total hip arthroplasties.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of their immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This study was performed at the Department of Joint Replacement, General and Rheumatic Orthopaedics, Orthopaedic Clinic Markgröningen.
About this article
Cite this article
Fink, B., Gebhard, A., Fuerst, M. et al. High Diagnostic Value of Synovial Biopsy in Periprosthetic Joint Infection of the Hip. Clin Orthop Relat Res 471, 956–964 (2013). https://doi.org/10.1007/s11999-012-2474-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-012-2474-5