Abstract
Background
Different patterns of stress shielding may lead to differences in periprosthetic bone preservation around cemented and uncemented hips in the long term?
Questions/purposes
The purpose of this study is to compare the difference in periprosthetic bone density between cemented Charnley total hip and uncemented hydroxyapatite-coated Furlong® THAs at a minimum followup of 12 years (mean, 16 years; range, 12–24 years).
Methods
We studied a cohort of 17 patients who had bilateral THAs with a cemented Charnley THA on one side and an uncemented Furlong® hydroxyapatite-coated THA on the other side. At a minimum followup of 12 years, Harris and Oxford hip scores were used to determine the function, and dual-energy x-ray absorptiometry was used to quantify bone mineral density adjacent to the prosthesis. The results of the dual-energy x-ray absorptiometry scan for cemented and uncemented hips were analyzed using paired-sample two-tailed t-tests. To compare the Harris hip scores, a nonparametric Wilcoxon test was used.
Results
Bone mineral density was higher on the uncemented Furlong® side in Gruen Zones 2, 3, 5, and 6 of the proximal femur and DeLee and Charnley Zone 1 of the acetabulum. In all other zones, there was no difference. Comparison of Harris and Oxford hip scores showed no differences between the two hips.
Conclusion
Bone density is better preserved around the uncemented hydroxyapatite-coated Furlong® stem compared with the Charnley cemented stem.
Level of Evidence
Level III, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Periprosthetic bone behavior is complex and poorly understood. Numerous studies have enumerated various patterns of bone remodeling around cemented or uncemented hip prostheses. There exists a major difference in bone remodeling between them [1, 8, 11, 13, 21]. Alterations of the physiologic stresses around the hip contribute to the development of subsequent adaptive remodeling to determine the quality of the periprosthetic bone. Preoperative bone density and mechanical characteristics of the implant, which includes stiffness, rigidity, load transmission characteristics, and the surface coating of the prosthesis determine the homeostasis of the remodeled periprosthetic bone [3, 13, 16].
Commonly, there is a loss of 10% to 45% of the periprosthetic bone mass during the first years after THA. Studies have suggested this bone loss is not necessarily progressive and some degree of restoration of bone density around implants occurs usually by 2 years [13, 19]. However, some studies have shown up to 40% loss in average bone mineral content inside the lesser trochanter and 28% loss in average bone mineral content 4.8 cm distal to the lesser trochanter in the medial cortex. The data suggest that the loss in mineral content may progress and could account for as much as a 50% decrease in bone mass in the long term [17]. The quality of periprosthetic bone determines the risk of periprosthetic fracture and also defines the complexity of revision surgery if needed. Better periprosthetic bone preservation can decrease the need for complex reconstruction. Most studies reporting bone remodeling around cemented or uncemented hip prostheses do not make a direct comparison between them. Studying the long-term difference in periprosthetic bone density between the cemented or uncemented hip prostheses could help in choosing the bone-preserving prosthesis for hip arthroplasty.
Dual-energy x-ray absorptiometry (DEXA) scans have been widely accepted as a reliable tool with high reproducibility to quantify bone mineral density (BMD) changes adjacent to a THA [20]. It is a precise and an accurate method of measurement for small changes in BMD around femoral implants [4, 13–15, 26, 27].
We studied a cohort of patients who had bilateral THAs with a cemented Charnley prosthesis on one side and an uncemented hydroxyapatite (HA)-coated Furlong® (JRI Limited, London, UK) prosthesis on the other side. The aims of this study were (1) to compare the difference in periprosthetic bone density between cemented Charnley and uncemented HA-coated Furlong® prostheses at a minimum followup of 12 years (range, 12–24 years); (2) to assess if differences in periprosthetic bone density were associated with differences in Harris or Oxford hip scores; and (3) to compare radiographic signs of loosening.
Patients and Methods
Between 1980 and 1994, 22 patients had bilateral hip arthroplasties with the cemented Charnley prosthesis on one side and an uncemented Furlong® prosthesis on the other side. The Furlong® prosthesis is fully HA-coated, and the coating is applied by plasma spray with thickness of 200 μm and bond strength of 40 Mpa. All surgeries were performed by two senior authors (MA, JGB) using a similar technique. At the time of study, five patients had died and 17 were alive and were invited to participate in the study. Seven of the patients were males. The mean age of all patients at the time of assessment was 78 years (range, 62–93 years). The average time from cemented hip arthroplasty to assessment was 18 years (range, 13–24 years), and the time from uncemented hip arthroplasty to assessment was 14 years (range, 12–17 years) (Table 1). We obtained local and regional ethical committee approval.
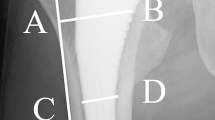
We clinically assessed all patients by recording Oxford and Harris hip scores. Standardized AP and lateral radiographs were taken. The AP projection was centered on the symphysis pubis and was taken at a standard distance of 1 m. We used Gruen zones [9] for the femoral component and DeLee and Charnley [6] zones for the acetabular component as references. The radiographs were assessed for radiolucent lines, osteolysis, and endosteal bone formation (spot welds) by one observer (PC); pedestal formation was used to assess fixation and stability of the uncemented stem (Fig. 1).
All patients had DEXA scans of both hips to determine the quality of bone around the prosthesis. We collected data regarding bone density and remodeling patterns. The DEXA scanner used was a GE LUNAR prodigy orthopaedic scanner (GE Medical Systems Lunar, Milwaukee, WI, USA), a narrow-angle fan-beam densitometer. We used validated orthopaedic analysis software (GE Medical Systems Lunar) solely to measure the periprosthetic bone density excluding metal and cement artifacts; Gruen and DeLee-Charnley zones were used as references and were quantified in mg/cm2.
We analyzed the results from the DEXA scans using paired-sample two-tailed t-tests. To compare the Harris hip scores, a nonparametric Wilcoxon test was used. Pearson correlations were done to examine the relationship between the bone density measures (averaged for each zone) and the quality-of-life measures.
Results
DEXA scans showed the BMD was significantly higher (p < 0.05) on the Furlong® side in Gruen Zones 2, 3, 5, and 6 of the proximal femur and DeLee and Charnley Zone 1 of the acetabulum (Table 2). In all other zones, there was no difference. Age was negatively correlated with bone density in Gruen Zones 6 and 7 and acetabular Zones 2 and 3.
Comparison of Harris and Oxford hip scores showed no statistically significant difference between the two hips (p = 0.108).
All prostheses were well fixed, which included both stems and the cups on either side. Radiographs showed radiolucent lines in two Gruen zones in two cases around the femur on the cemented Charnley prosthesis side. No osteolysis, loosening, or migration of the prosthesis was seen in any of the hips. In addition, 13 patients in the Furlong® uncemented group showed endosteal bone formation (spot welds), and pedestal formation was observed in 12.
Discussion
Periprosthetic bone remodeling is complex and poorly defined, particularly with relation to the different cemented or uncemented prostheses currently in use. In our study, the comparative results revealed better preservation of periprosthetic bone with the uncemented HA-coated Furlong® prosthesis in Gruen Zones 2, 3, 5, and 6 on the femoral side and DeLee and Charnley Zone 1 on the acetabular side when compared with the cemented Charnley prosthesis.
Our study has several limitations. It lacks the baseline preoperative, postoperative BMD, and serial postoperative measurements of bone density; these data would have helped to identify longitudinal long-term changes resulting from the implantation and subsequent remodeling and also helped us to determine if the prosthesis has better preserved or increased the BMD in the periprosthetic region. Our primary aim was to compare the long-term difference in periprosthetic bone density between the cemented and uncemented HA-coated implants and the available data helped us to make that comparison. The followup of the patients who underwent cemented hip arthroplasties is approximately 4 years longer than for the patients who had the uncemented arthroplasties. Theoretically, the cemented hip prostheses have been in place longer and therefore, it might be expected that more bone was lost. Some studies have shown remodeling in the periprosthetic region varies with time and reaches homeostasis by approximately 2 years [1, 10] and few changes are expected later. Our study involves observing long-term homeostasis in bone remodeling and we believe the difference in timing of implantation of cemented and uncemented implants would not skew our results. Age has been found to negatively correlate with bone densities in femoral Zones 6 and 7 and acetabular Zones 2 and 3, suggesting older age is associated with lower bone densities. The small sample size in our study gives little power to detect such relationships. All radiologic observations were made once by one observer (PC), which could introduce interobserver and intraobserver bias and adds to the limitation of the radiologic findings.
There are no long-term studies that directly compare cemented and uncemented periprosthetic bone remodeling. In the short term, up to 4 years [12], studies show that on the femoral side, the cemented prosthesis induced bone mass reduction in the lesser trochanter area and in the distal lateral cortex and with the uncemented stem produced significant bone resorption in the area of the lesser trochanter and in the medial and the lateral distal cortex of the femur; both induced an increase in the bone mass in the greater trochanter area. In comparison, our study showed a different pattern of bone remodeling with greater preservation of bone density in the distal medial and the distal lateral cortex with the uncemented stem. Longitudinal noncomparison studies with Charnley cemented prostheses [5] have observed that at 1 year, there was a reduction in BMD of 6.7% in the calcar region and an increase of 5.3% in the femoral shaft distal to the tip of the implant [22]. Studies with an uncemented HA-coated prosthesis [19] showed that the BMD was lower in Gruen Zones 1 and 7 and concluded prosthesis design influences periprosthetic bone loss. Similar studies with HA-coated ABG prostheses showed bone density values averaged between 96% and 113.8% for Gruen Zones 1 to 6, and in Zone 7, there was a decline to an average of 72.1% at 24 months [24]. In contrast, one study [17] showed a 40% loss of bone proximally and 49% distally at 7 to 14 years [10]. In our study with the HA-coated Furlong® prosthesis, we observe preservation in the BMD in Gruen Zones 2, 3, 5, and 6 of the proximal femur. The difference in periprosthetic bone density observed in our study could be the result of the mechanical properties and load transmission characteristics of the prosthesis [25]. The femoral stems in the Furlong® prosthesis transmit load largely in the metaphyseal-diaphyseal region as compared with the Charnley prosthesis, suggesting a stress-related remodeling pattern for long-surviving prostheses.
On the acetabular side, the uncemented socket induced bone resorption at the medial and caudal zones, and the cemented socket showed significantly increased BMD in the cranial zone [12]. Other studies with the cemented acetabular component observed the periacetabular bone mass returned to baseline values at 2 years with a pattern suggesting uniform transmission of load to the acetabulum [5]. Our study showed the BMD was better preserved in DeLee and Charnley Zone 1 of the acetabulum. These observations reflect the difference in load transmission of the different socket designs suggesting a more uniform load distribution with the Charnley cups as compared with the screw-in design of the uncemented Furlong® cups, which probably had a higher load transmission in Zone 1 [23].
HA coatings induce bony ingrowth onto the surface of the prosthesis; its influence on the periprosthetic BMD is not clear. Although a fully HA-coated stem is expected to induce greater bone apposition, wider trabecular struts, and more connectivity compared with half HA-coated stems [2], or tapered corundum-blasted titanium stems [1], it is not clear if the HA coating has any role in better preserving bone stock, with studies showing good bony integration with uncemented nonbioactive surface implants [7, 18].
With good survival of the HA-coated Furlong® cup and stem [22], better preservation of periprosthetic bone would potentially make revision surgery less complex and also possibly decrease the risk of periprosthetic fracture. Additional long-term studies of remodeling and periprosthetic bone density between cemented and uncemented implants can help us understand preservation and behavior of periprosthetic bone stock.
Bone density is better preserved around the uncemented HA-coated stem in Gruen Zones 2, 3, 5, and 6 on the femoral side and Zone 1 on the acetabular side compared with the Charnley cemented stem.
References
Aldinger PR, Sabo D, Pritsch M, Thomsen M, Mau H, Ewerbeck V, Breusch SJ. Pattern of periprosthetic bone remodeling around stable uncemented tapered hip stems: a prospective 84-month follow-up study and a median 156-month cross-sectional study with DXA. Calcif Tissue Int. 2003;73:115–121.
Al Hertani W, Waddell JP, Anderson GI. The effect of partial vs. full hydroxyapatite coating on periprosthetic bone quality around the canine madreporic femoral stem. J Biomed Mater Res. 2000;53:518–524.
Ang KC, Das De S, Goh JC, Low SL, Bose K. Periprosthetic bone remodelling after cementless total hipreplacement: a prospective comparison of two different implant designs. J Bone Joint Surg Br. 1997;79:675–679.
Cohen B, Rushton N. Accuracy of DEXA measurement of bone mineral density after total hip arthroplasty. J Bone Joint Surg Br. 1995;77:479–483.
Cohen B, Rushton N. Bone remodelling in the proximal femur after Charnley total hip arthroplasty. J Bone Joint Surg Br. 1995;77:815–819.
DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20–32.
Engh CA, Bobyn JD, Glassman AH. Porous-coated hip replacement: the factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg Br. 1987;69:45–55.
Giannikas KA, Din R, Sadiq S, Dunningham TH. Medium-term results of the ABG total hip arthroplasty in young patients. J Arthroplasty. 2002;17:184–188.
Gruen TA, McNeice GM, Amstutz HC. “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979;141:17–27.
Kilgus DJ, Shimaoka EE, Tipton JS, Eberle RW. Dual-energy X-ray absorptiometry measurement of bone mineral density around porous-coated cementless femoral implants: methods and preliminary results. J Bone Joint Surg Br. 1993;75:279–287.
Kobayashi S, Eftekhar NS, Terayama K. Long term bone remodeling around the Charnley femoral prostheses. Clin Orthop Relat Res. 1996;326:162–173.
Korovessis P, Piperos G, Michael A. Periprosthetic bone mineral density after Mueller and Zweymueller total hip arthroplasties. Clin Orthop Relat Res. 1994;309:214–221.
Kroger H, Venesmaa P, Jurvelin J, Miettinen H, Suomalainen O, Alhava E. Bone density at the proximal femur after total hip arthroplasty. Clin Orthop Relat Res. 1998;352:66–74.
Laursen MB, Nielsen PT, Soballe K. DXA scanning of acetabulum in patients with cementless total hip arthroplasty. J Clin Densitom. 2005;8:476–483.
Lekamwasam S, Lenora RS. Effect of leg rotation on hip bone mineral density measurements. J Clin Densitom. 2003;6:331–336.
Maistrelli GL, Fornasier V, Binnington A, McKenzie K, Sessa V, Harrington I. Effect of stem modulus in a total hip arthroplasty model. J Bone Joint Surg Br. 1991;73:43–46.
McCarthy CK, Steinberg GG, Agren M, Leahey D, Wyman E, Baran DT. Quantifying bone loss from the proximal femur after total hip arthroplasty. J Bone Joint Surg Br. 1991;73:774–778.
Park YS, Lee JY, Yun SH, Jung MW, Oh I. Comparison of hydroxyapatite- and porous-coated stems in total hip replacement. Acta Orthop Scand. 2003;74:259–263.
Rahmy AI, Gosens T, Blake GM, Tonino A, Fogelman I. Periprosthetic bone remodelling of two types of uncemented femoral implant with proximal hydroxyapatite coating: a 3-year follow-up study addressing the influence of prosthesis design and preoperative bone density on periprosthetic bone loss. Osteoporos Int. 2004;15:281–289.
Sabatier JP, Guaydier-Souquieres G. Noninvasive methods of bone-mass measurement. Clin Rheumatol. 1989;8(suppl 2):41–45.
Sharkey PF, Barrack RL, Tvedten DE. Five-year clinical and radiographic follow-up of the uncemented long-term stable fixation total hip arthroplasty. J Arthroplasty. 1998;13:546–551.
Shetty AA, Slack R, Tindall A, James KD, Rand C. Results of a hydroxyapatite-coated (Furlong) total hip replacement: a 13- to 15-year follow-up. J Bone Joint Surg Br. 2005;87:1050–1054.
Shetty NR, Hamer AJ, Kerry RM, Stockley I, Eastell R, Wilkinson JM. Bone remodelling around a cemented polyethylene cup: a longitudinal densitometry study. J Bone Joint Surg Br. 2006;88:455–459.
Theis JC, Beadel G. Changes in proximal femoral bone mineral density around a hydroxyapatite-coated hip joint arthroplasty. J Orthop Surg (Hong Kong). 2003;11:48–52.
Turner AW, Gillies RM, Sekel R, Morris P, Bruce W, Walsh WR. Computational bone remodelling simulations and comparisons with DEXA results. J Orthop Res. 2005;23:705–712.
Venesmaa PK, Kröger HP, Miettinen HJ, Jurvelin JS, Suomalainen OT, Alhava EM. Monitoring of periprosthetic BMD after uncemented total hip arthroplasty with dual-energy X-ray absorptiometry: a 3-year follow-up study. J Bone Miner Res. 2001;16:1056–1061.
Wahner H. Technical aspects and clinical interpretation of bone mineral measurements. Public Health Rep. 1989;104(suppl):27–30.
Acknowledgment
We thank Dr Jeremy Miles, senior lecturer in biostatistics, University of York, for assistance with the statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of their immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
About this article
Cite this article
Chandran, P., Azzabi, M., Andrews, M. et al. Periprosthetic Bone Remodeling after 12 Years Differs in Cemented and Uncemented Hip Arthroplasties. Clin Orthop Relat Res 470, 1431–1435 (2012). https://doi.org/10.1007/s11999-011-2134-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-011-2134-1