Abstract
Purpose
As progressive hip dislocation causes pain in children with spastic cerebral palsy (CP) and spasticity needs surgical correction, we aimed to describe clinical and radiographic outcomes in CP patients with painful hip deformity treated with the Castle salvage procedure.
Methods
We included all patients operated in the same hospital between 1989 and 2017 with painful spastic hips and femoral head deformity making joint reconstruction unfeasible. We collected clinical and functional data from medical records and evaluated radiographies to classify cases for femoral head shape and migration, type of deformity, spinal deformity, and heterotopic ossification. We investigated quality of life one year after surgery.
Results
We analyzed 41 patients (70 hips) with complete medical records. All had severe function compromise GMFCS V (Gross Motor Function Classification System) and heterotopic ossifications, all but one had scoliosis, and most had undergone other surgeries before Castle procedure. Patients were followed up for 77.1 months (mean) after surgery. The mean initial migration index was 73%. Seven patients had complications, being three patients minor (two femur and one tibial fracture) and four majors (patients requiring surgical revision). Quality of life was considered improved by most of the carers (35 children; 85.3%) as level 4/5 according to CPCHILD instrument. No child was able to stand or walk, but moving in and out of bed, of vehicles, and to a chair, remaining seated, or visiting public places was “very easy.”
Conclusion
We considered most patients (37 patients—90%, 66 hips—94%) as having satisfactory outcomes because they had no or minor complications, absence of pain, free mobility of the lower limbs and were able to sit in a wheelchair.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hip dislocation is the most frequent cause of pain in children with spastic cerebral palsy (CP), and its incidence ranges from 1 to 90%. The severity of dislocation is related to functional level [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17]. The causes of progressive hip dislocation in CP are multifactorial: primitive reflexes, spasticity, muscle imbalance and contractures, coxa valga, femoral anteversion, and delay in walking. However, asymmetrical muscle spasticity especially affects the flexor-adductor muscles of the hip, and it is considered the main contributor for pain [6, 17,18,19,20,21,22,23,24,25,26].
The orthopaedic treatment of the hips of patients with CP starts with procedures to avoid deformities and their progression, trying to keep them stable, flexible, located, painless, and with a symmetrical range of motion. The best way to achieve this is through early identification and intervention; based on the Hip Surveillance Program, an active serial clinical-radiographic monitoring program to identify patients at risk of progressive hip dislocation [5, 23].
However, hip dislocation in patients with spastic CP is challenging to treat, particularly in those with mental disabilities and at the most compromised functional levels, unable to walk. When left untreated, hip dislocation can lead to adduction contractures, difficulties with sitting and hygiene, pelvic obliquity, scoliosis, and decubitus ulcers. There is also a strong association between hip dislocation and pain, affecting sleep and overall quality of life [3, 4, 6, 10, 11, 18, 22, 26].
Salvage surgeries are recommended for painful, subluxated, or dislocated hips with radiographic signs of joint degeneration, where reconstruction has failed or where surgery is not an option due to the degree of joint degeneration [12, 25, 27]. Salvage surgery must meet four recommendations: first, it should be done aiming to facilitate hygiene care in the perineal region. The hip (or its remaining) must be kept mobile so that it does not interfere with the patient’s positioning on the bed and chair. The surgery must be simple and with a short postoperative period. When bilateral, the procedure should preferably be performed in a single operation [10, 25, 28].
The objective of the present study is to describe a group of consecutive patients with spastic CP and painful hip deformity treated with the Castle salvage procedure in the same hospital. As a primary objective, we aimed to describe clinical and radiographic outcomes. A secondary investigation was about improvements in the patient’s quality of life after surgery.
Patients and methods
Study design and ethics
This was a cross-sectional, descriptive study including all patients with painful spastic CP hip deformities consecutively treated in a single centre between 1989 and 2017. The hospital is a specialized orthopaedic centre within the public health system in Brazil. This study was conducted according to the Declaration of Helsinki (1964), and the protocol was approved by the hospital’s Ethics Committee [protocol number 94349118.5.0000.5479]. All patients’ legal guardians signed informed consent forms for the inclusion of data in this study.
Participants and eligibility criteria
The radiographic inclusion criteria for this study were evidence of dysplastic hips and the presence of a femoral head deformity that made joint reconstruction unfeasible. Clinical inclusion criteria were pain when moving the hip and difficulty in sitting down and for hygiene care. We only included patients who had complete medical records for reviewing. We excluded patients who did not return for clinical visits after surgery and who had follow-up periods of less than 12 months.
Outcomes and evaluation methods
We collected data from the medical records on age at the date of surgery, sex, functional grade according to the Gross Motor Functional Classification System (GMFCS) [3], scoliosis presence, previous surgeries and type of surgery, laterality, radiographic evaluation in the preoperative period, immediate postoperative period and final postoperative period, description of the clinical evolution, presence of complications, evaluation of quality of life, and follow-up time. We considered the follow-up time as the interval between the immediate postoperative and the last outpatient evaluation.
Complications were classified, for this study, as major and minor. Minor complications were fractures of the operated lower limb and the presence of heterotopic ossification without limiting range of movement. The major complications were persistent pain, bone exposure requiring hospitalization, and submission to revision surgical procedure. We considered patients in this study as having satisfactory surgical outcomes when they had no complications or only minor complications, with absence of pain, free mobility of the lower limbs, and possible sitting position in the wheelchair. We considered the presence of major complications and persistence of pain as unsatisfactory outcomes.
Postoperative care and clinical evaluation methods
For patients submitted to the Castle operation in our hospital, there was a varied routine postoperative care at the time of the treatments: two cases underwent cutaneous traction of the lower limbs for one week, 16 cases underwent skeletal traction for six weeks, six had an external fixator for six weeks, one with a broomstick cast for three weeks, and 16 patients did not use immobilization.
Pain when moving the affected hip and/or difficulties or intolerance in sitting was recorded in the medical records as present or absent before and after surgery. Pain was registered by the attending clinician during physical examination and as referred by the patient’s carer. No scale of pain was used.
The clinical evaluation in our hospital includes the assessment of quality of life using the Section 2 of the Caregiver Priorities and Child Health Index of Life with Disabilities Questionnaire (CPCHILD) instrument, translated, and validated for Brazilian Portuguese [29]. The tool is used 12 months after surgery. Briefly, in this evaluation, the patient carer grades the difficulty they have to perform activities such as laying the patient down on bed, transfer to a chair, moving around the house, and getting on and off cars. They also indicate how much help they need for these activities.
Radiographic evaluations
All patients underwent preoperative, immediate postoperative, and final postoperative pelvic anteroposterior radiographic evaluations. The preoperative radiographs were analyzed for the percentage of femoral head migration [30], the type of deformity according to the Melbourne Cerebral Palsy Classification Scale (MCPHPS) [31], and the type of femoral head deformity according to Miller et al. classification [33].
The percentage of migration (PM) or Reimers index [30] measures the displacement of the femoral epiphysis in relation to the acetabulum, classifying it as normal when between 0 and 33%, subluxation 40% and 99%, and dislocation above 100%.
MCPHPS [31] is a radiographic classification of the hip for patients with CP close to the age of skeletal maturity (typically between 14 and 19 years). The deformity is described in terms of (1) Shenton’s arch integrity, (2) shape of the femoral head, (3) shape of the acetabulum, and (4) pelvic obliquity. The characteristics of each grade of hip dislocation is detailed in Supplementary Table 1 and classified as percentages of migration, where Grades I and II represent normal and near normal hips, Grade III a dysplastic hip, Grade IV subluxated hip, Grade V moderate to severe subluxation, Grade VI dislocated hip, and Grade VII salvage surgery.
To analyze the shape of the femoral head, Miller et al. [32] classification was adopted and as described, from the pelvic radiographs in frontal view, with grade 1 round, grade 2 with medial or lateral flattening, and grade 3 with both medial and lateral flattening.
To evaluate the migration of the proximal femur, the distance (in centimeters) between two reference lines was measured: a horizontal line on the ossified upper edge of the acetabulum and a second line on the proximal edge of the femur, taking care to identify and not consider in the measure, the possible presence of heterotopic ossification (OH). The distance was transformed into a percentage to quantify the proximal migration of the femur, measured in the immediate and final postoperative periods. The measurement is illustrated in Fig. 1.
If a spinal deformity was present, the curvature was evaluated through radiographies taken during outpatient follow-up, which could be preoperative or in the final postoperative period. The radiographs, from the first thoracic vertebra to the sacral, were taken in the dorsal decubitus on anteroposterior view. The Cobb angle was measured, considering the curve with moderate severity at angles equal to or greater than 40° [33].
To classify heterotopic ossification (HO) in the final postoperative period, we used the criteria by McCarthy et al. [34], which considers three categories:
-
Type I—mushroom-shaped, around the top of the femoral shaft, and generally within the limits of the vastus lateralis.
-
Type II—in the form of a spicule, which projected laterally from the diaphysis and extended beyond the limits of the vastus lateralis, sometimes towards the acetabulum.
-
Type III—with the pattern of diffuse myositis ossificans, that is, it was distributed between the acetabulum and the femur in the adjacent muscle.
We used digital radiographs, except for the X-rays taken before 2011, that we had to scan for visualization and measurement. We used for that the digital system Enterprise Imaging Xero Viewer 8.1.2, Agfa HealthCare. To measure angles and distances, we used the MB-Ruler v.5.3 software for Windows, registering measurements with up to two decimal places. Two experienced evaluators assessed the radiographs independently and we registered for this study the average measurement between them. We also calculated the intraclass correlation coefficient between observers.
Statistical analysis
Data were recorded in Microsoft Excel files and later exported to SPSS for Mac. We performed descriptive statistical analysis, first testing the distribution using the Kolmogorov–Smirnov test and then describing continuous measurements as means and categorical as frequencies and proportions.
Results
In the study period, 112 patients with CP and hip deformity were admitted in our hospital for surgical treatment. Of these, 55 (89 hips) had been operated with the Castle procedure. However, 14 (19 hips) did not return for clinical follow-up and were excluded. The study was based, therefore, on a total sample of 41 patients (70 hips) undergoing the Castle procedure. All patients had a GMFCS functional status classified as Grade V and had scoliosis in the final evaluation. Most had previous surgeries and surgery combinations. They were followed up for 77.1 months on average. Table 1 shows demographic data and previous surgeries, most of which had undergone McHale procedure before (with Castle used as a secondary salvage procedure). Figure 2 shows a case with previous surgery.
Radiographies of a female patient with cerebral palsy, tetraplegic, with GMFCS grade V. A Initial X-ray at age 5 years and 11 months. B Postoperative image 2 months after bilateral McHale procedure, with patient at age 6 years and 6 months. C Immediate postoperative image of bilateral Castle procedure, at age 11 years and 3 months. D Postoperative image taken 15 years and 3 months after bilateral Castle procedure at age 26 years and 6 months
As the ICC between observers was 0.96, we registered the average between observers’ measurements in the radiographical evaluations. Table 2 shows the type of femoral head deformity in the preoperative radiographs and Table 3 shows the acetabular index, the percentage of femoral head migration, and the type of deformity according to MCPHPS. Proximal femoral migration difference between the postoperative periods, immediate and final, was 0% in 7 hips, between 0 and 100% in 32, 100% in 27, and over 100% in 4 hips.
Seven patients operated with the Castle procedure had complications. Complications were minor in three patients (7.32%; six hips), with fractures in the postoperative time: two bilaterally Castle procedure in one with tibia fracture after one month, another with diaphyseal right femur fracture after 18 months. The third patient a revised on the right side presented with a left distal femur fracture 18 months postoperative. All fractures were treated conservatively with cast and had no influence in outcome.
Major complications presented in another four patients operated bilaterally and underwent unilateral revision.
Indication for revision was the presence of massive HO preventing mobility and pain, just in one patient there was pressure sore over the distal femur fragment which is the cause of the revision (case with 216 months postoperative). Time between the initial surgery and revision was four months, 14 months, 51 months, and 216 months. All these patients were in skeletal traction on distal femur for five weeks. After the revisions, there was improvement of the pain and quality of life.
We found heterotopic ossification in all patients (70 hips), 27 type 1, 41 type 2, and two were type 3 (one case shown in Fig. 3) been only in three patients (3 hips) precluding movement and need revisions as discussed. Scoliosis was frequent in the second evaluation, affecting all but one patient (40, 97.6%). No differences in the outcomes were found regarding age at surgical procedure (less than ten years and more than ten years of age) and the gender of the patients.
Radiographies of a female patient with cerebral palsy, tetraplegic, with GMFCS grade V. A Initial X-ray at age 7 years and 1 month. B Immediate postoperative of bilateral Castle procedure, at age 7 years and 5 months. C Postoperative 16 years and 8 months after Castle procedure, taken at age 34 years and 1 month. Bilateral procedure done to promote pelvic symmetry
We considered 37 patients (90%) 66 hips (94%) as having satisfactory outcomes because they were without complications or had minor complications, absence of pain, free mobility of the lower limbs, and being able to sit in a wheelchair. In four patients (10%), three hips (6%) developed major complications therefore considered unsatisfactory outcomes; after the revision surgery, families reported improvement in the pain and easier care (Fig. 4—flowchart).
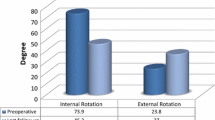
Analysis about function and overall quality of life (from 0 to 5), according to CPCHILD instrument (Table 4), applied one year after surgery. Quality of life was considered by most of the caregivers (35 children, 85.3%) as level 4. When all items were summed, the quality of life ranged from 5 to 25, averaging 21.95, and it was 25 for 36 (87.8%) patients (full results are shown in Supplementary Table 2). Most children needed full help to get in and out of bed and of vehicles, moving to a chair, remain seated, or go to public places. No child was able to remain standing or move around the house.
Discussion
Children with CP are born with anatomically normal hips, with no evidence of dislocation, subluxation, or dysplasia [4, 33], but they evolve with severe hip dislocation, as seen in our cohort. Most (90%) of our patients were over ten years old at the surgical procedure, which indicates the natural history of the spasticity in the hip displacement, even when the patient has been operated before. This finding is according to the literature, where the highest risk of dislocation is found in children between four and 12 years old [25].
Hip deformity in patients with spastic CP, especially among those with GMFCS IV and V, is frequent and affects the overall clinical status. For patients and those responsible for their daily care, the most impactful problem is pain during hip manipulation, which is associated with spastic dislocation of the hip in 70% of cases [6, 35]. This symptom reflects the femoral head deformity seen in radiographs. Hips with percentage of migration over 60% are expected to evolve into complete dislocation, and migration of 50% or over is associated with hip pain [32]. Our cases also show that the functional severity is associated with the hip deformity severity. Without treatment, these patients are candidates for salvage surgery, such as the Castle procedure. Salvage options are resection arthroplasty or valgus osteotomy of the proximal femur with or without resection of the femoral head and neck, hip arthrodesis, total hip arthroplasty, and interposition arthroplasty of a proximal femur prosthesis [4, 6, 8, 12, 14, 19, 22,23,24, 27, 28, 32].
Hip deformity can be even more disastrous when associated with scoliosis. The risk for scoliosis increases with age and with functional severity [13]. The risk of scoliosis is 1% for patients at GMFCS level I at ten years of age and 30% for GMFCS V at the same age [13]. We found that 97.6% of patients developed scoliosis at the second evaluation. Therefore, correcting scoliosis is another surgical challenge in this group.
Postoperative HO was common. The literature has registered ample variation of this complication, reaching 100% of cases in some studies [12, 34, 35]. What we have seen in our patients was that when the HO did not interfere in the movement there was not an impact in the outcome and therefore in quality of life for them.
As shown by Patel et al. [26], the Castle procedure results in improvements in quality of life. Quality of life evaluation is routinely performed in our hospital for all children undergoing the Castle surgery, considered the last salvage resource for patients with CP and spastic hip deformities. As seen in our cohort, many patients had already undergone other surgeries before being submitted to Castle. The CPCHILD tool provides a complete evaluation that complements functional assessments and was responded by parents or caregivers. The average score observed shows these patients still have significant impacts in their daily lives. However, carers reported that procedures such as transferring the patients from and to beds, chairs, wheelchairs, and vehicles became “very easy.” Not standing or moving by themselves around the house certainly affects the overall quality of life score but may not be expected for these patients from the start.
Our study agrees with the literature which shows pain relief after the procedure, as in Koch et al., in a numeric rating scale, the pain score was reduced 5.42 to 2.13; and satisfaction scores reported by caregivers were 8.3 [15]. As described by Chan et al., the Castle procedure is a relatively simple procedure with reliable pain relief [12]. In Shaw et al., the average time to maximal pain relief after surgery was 5.6 months [12]. Souza et al. described in systematic review the postoperative results obtained with this technique were satisfactory in all the studies selected. What most differentiated the studies were the evaluation methods for pre and postoperative pain, given that this is a subjective criterion and many of these patients presented cognitive deficit, and cited the used quantity of analgesic pills that the patient was consuming per day as criteria [8].
As described by Castle and Schneider [28], patients need to be in traction until soft tissues heal. McCarthy et al. also propose six weeks of traction [34], which can be challenging in terms of today hospital costs. As seen in our outcomes, the time in traction postoperative probably did not influence as much as expected.
Limitations of the retrospective study are as follows: first—what was not standardized was the time of the postoperative cast, due to some difficulties in the return of the patients in the outpatient clinic; second—regarding the measurements of the HO done in the last follow-up radiographs and not done in a longitudinal evolution, and finally—the loss of patients with incomplete medical records should be considered.
On the other hand, a strength of this analysis is that all patients were operated on by the same surgical team in our university hospital, using the same technique, which offers some standardization and less bias to the results. The main possible reason for our satisfactory outcomes was to be very strict and careful with the surgical technique, promoting the distal femur fragment a good and bulky coverage with muscles and care with closing the hip capsule.
There is not yet an agreement on the surgical indication when salvage situations arise, but in the view of our outcomes, we can state that the Castle procedure is still an option for these severe hip deformities.
Treating the child with CP and spastic hips is challenging exactly because of the difficulty in standardizing treatment: this is a patient with a severe and painful deformity, and even if classifying them with the same functional level, there will be anatomical, psychological, and social particularities that make the patient unique. Any treatment plan must, therefore, consider all aspects and with the goal of improving the quality of life as a target outcome.
Conclusion
Patients with spastic cerebral palsy and hip deformities undergoing the Castle procedure had a high GMFCS score and scoliosis. After surgery, few of them had major complications requiring new surgical treatments and most had absence of pain and free mobility of the lower limbs and were able to sit in a wheelchair. Quality of life scores after the Castle procedure were considered high by the majority of the families and caregivers as shown by the improvement in level and by the easiness in the care of the patients due to absent of pain.
References
Vidal J, Deguillaume P, Vidal M (1985) The anatomy of the dysplastic hip in cerebral palsy related to prognosis and treatment. Int Orthop 9:105–110. https://doi.org/10.1007/BF00266951
Cooke PH, Cole WG, Carey RP (1989) Dislocation of the hip in cerebral palsy. Natural history and predictability. J Bone Joint Surg Br 71:441–446. https://doi.org/10.1302/0301-620X.71B3.2722938
Palisano R, Rosenbaum P, Walter S et al (1997) Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol 39:214–223. https://doi.org/10.1111/j.1469-8749.1997.tb07414.x
Flynn JM, Miller F (2002) Management of hip disorders in patients with cerebral palsy. J Am Acad Orthop Surg 10:198–209. https://doi.org/10.5435/00124635-200205000-00006
Dobson F, Boyd RN, Parrott J et al (2002) Hip surveillance in children with cerebral palsy. Impact on the surgical management of spastic hip disease. J Bone Joint Surg Br 84:720–726. https://doi.org/10.1302/0301-620x.84b5.12398
Albiñana J, Gonzalez-Moran G (2002) Painful spastic hip dislocation: proximal femoral resection. Iowa Orthop J 22:61–65
Dartnell J, Gough M, Paterson JMH, Norman-Taylor F (2014) Proximal femoral resection without postoperative traction for the painful dislocated hip in young patients with cerebral palsy. A review of 79 cases. Bone Joint J 96–B(5):701–706
Souza RC, Mansano MV, Bovo M, Yamada HH, Rancan DR, Fucs PMMB, Svartman C, Assumpçao RMC (2015) Hip salvage surgery in cerebral palsy cases: a systematic review. Rev Bras Ortop 50(3):254–259
Chougule S, Dabis J, Petrie A et al (2016) Is head-shaft angle a valuable continuous risk factor for hip migration in cerebral palsy? J Child Orthop 10:651–656. https://doi.org/10.1007/s11832-016-0774-0
Ramstad K, Jahnsen RB, Terjesen T (2017) Severe hip displacement reduces health-related quality of life in children with cerebral palsy. Acta Orthop 88:205–210. https://doi.org/10.1080/17453674.2016.1262685
Chan P, Hsu A, Godfrey J, Silvac SS, Goldsteina RY, Ryana D, Choia PD, Kay RM (2019) Outcomes of salvage hip surgery in children with cerebral palsy. J Pediatr Orthop Part B 28:314–319. https://doi.org/10.1097/BPB.0000000000000566
Shaw KA, Hire JM, Cearley DM (2020) Salvage treatment options for painful hip dislocations in nonambulatory cerebral palsy patients. J Am Acad Orthop Surg 28:363–375. https://doi.org/10.5435/JAAOS-D-19-00349
Helenius IJ, Viehweger E, Castelein RM (2020) Cerebral palsy with dislocated hip and scoliosis: what to deal with first? J Child Orthop 14:24–29. https://doi.org/10.1302/1863-2548.14.190099
Yamada HH, Amato Neto DG, Malpaga JMD, Fucs PMDMB (2021) [Spastic hips in cerebral palsy – retrospective study of salvage with the McHale procedure] Quadris espásticos da paralisia cerebral – Estudo retrospectivo do salvamento com a cirurgia de McHale. Rev Bras Ortop 56:244–250. https://doi.org/10.1055/s-0040-1713391
Koch A, Krasny J, Dziurda M, Ratajczyk M, Jozwiak M (2021) Parents and caregivers satisfaction after palliative treatment of spastic hip dislocation in cerebral palsy. Front Neurol 12:635894
Wright PB, Ruder J, Birnbaum MA et al (2013) Outcomes after salvage procedures for the painful dislocated hip in cerebral palsy. J Pediatr Orthop 33:505–510. https://doi.org/10.1097/BPO.0b013e3182924677
Larnert P, Risto O, Hägglund G, Wagner P (2014) Hip displacement in relation to age and gross motor function in children with cerebral palsy. J Child Orthop 8:129–134. https://doi.org/10.1007/s11832-014-0570-7
Kalen V, Bleck EE (1985) Prevention of spastic paralytic dislocation of the hip. Dev Med Child Neurol 27:17–24. https://doi.org/10.1111/j.1469-8749.1985.tb04520.x
McHale KA, Bagg M, Nason SS (1990) Treatment of the chronically dislocated hip in adolescents with cerebral palsy with femoral head resection and subtrochanteric valgus osteotomy. J Pediatr Orthop 10:504–509
Soo B, Howard JJ, Boyd RN et al (2006) Hip displacement in cerebral palsy. J Bone Joint Surg Am 88:121–129. https://doi.org/10.2106/JBJS.E.00071
Robin J, Graham HK, Selber P et al (2008) Proximal femoral geometry in cerebral palsy: a population-based cross-sectional study. J Bone Joint Surg Br 90:1372–1379. https://doi.org/10.1302/0301-620X.90B10.20733
Hwang JH, Varte L, Kim HW et al (2016) Salvage procedures for the painful chronically dislocated hip in cerebral palsy. Bone Jt J 98–B:137–143. https://doi.org/10.1302/0301-620X.98B1.35202
Shore BJ, Graham HK (2017) Management of moderate to severe hip displacement in nonambulatory children with cerebral palsy. JBJS Rev 5:e4. https://doi.org/10.2106/JBJS.RVW.17.00027
Davids JR (2018) Management of neuromuscular hip dysplasia in children with cerebral palsy: lessons and challenges. J Pediatr Orthop 38(Suppl 1):S21–S27. https://doi.org/10.1097/BPO.0000000000001159
Hosseinzadeh P, Baldwin K, Minaie A, Miller F (2020) Management of hip disorders in patients with cerebral palsy. JBJS Rev 8:e0148. https://doi.org/10.2106/JBJS.RVW.19.00148
Patel NK, Sabharwal S, Gooding CR et al (2015) Proximal femoral excision with interposition myoplasty for cerebral palsy patients with painful chronic hip dislocation. J Child Orthop 9:263–271. https://doi.org/10.1007/s11832-015-0662-z
Fucs PMDMB, Yamada HH (2014) Hip fusion as hip salvage procedure in cerebral palsy. J Pediatr Orthop 34(Suppl 1):S32-35. https://doi.org/10.1097/BPO.0000000000000291
Castle ME, Schneider C (1978) Proximal femoral resection-interposition arthroplasty. J Bone Joint Surg Am 60:1051–1054
Pellegrino LA, Ortolan EVP, Magalhães CS et al (2014) Brazilian Portuguese translation and cross-cultural adaptation of the “Caregiver Priorities and Child Health Index of Life with Disabilities” (CPCHILD) questionnaire. BMC Pediatr 14:30. https://doi.org/10.1186/1471-2431-14-30
Reimers J (1980) The stability of the hip in children. A radiological study of the results of muscle surgery in cerebral palsy. Acta Orthop Scand Suppl 184:1–100. https://doi.org/10.3109/ort.1980.51.suppl-184.01
Robin J, Graham HK, Baker R et al (2009) A classification system for hip disease in cerebral palsy. Dev Med Child Neurol 51:183–192. https://doi.org/10.1111/j.1469-8749.2008.03129.x
Miller F (2005) Hip in: cerebral palsy. Springer Science & Business Media, New York, pp 523–666
Murphy RF, Mooney JF (2019) Current concepts in neuromuscular scoliosis. Curr Rev Musculoskelet Med 12:220–227. https://doi.org/10.1007/s12178-019-09552-8
McCarthy RE, Simon S, Douglas B et al (1988) Proximal femoral resection to allow adults who have severe cerebral palsy to sit. J Bone Joint Surg Am 70:1011–1016
Leet AI, Chhor K, Launay F et al (2005) Femoral head resection for painful hip subluxation in cerebral palsy: is valgus osteotomy in conjunction with femoral head resection preferable to proximal femoral head resection and traction? J Pediatr Orthop 25:70–73. https://doi.org/10.1097/00004694-200501000-00016
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yamada, H.H., de Moraes Barros Fucs, P.M. Quality of life and clinical outcomes in severely involved cerebral palsy patients and spastic hips undergoing Castle surgery: a cross-sectional study. International Orthopaedics (SICOT) 48, 1657–1665 (2024). https://doi.org/10.1007/s00264-024-06135-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-024-06135-2