Abstract
Background
Many factors affect the blood metal ion levels after metal-on-metal (MOM) hip arthroplasty. The main surgically adjustable variable is the amount of coverage of the head provided by the cup which is a function of the inclination and version angles. However, most studies have used plain radiographs which have questionable precision and accuracy, particularly for version and large diameter metal heads; further, these studies do not simultaneously assess version and inclination. Thus the relationship between version and blood metal ions levels has not been resolved.
Questions/purposes
We determined whether cup inclination and version influence blood metal ion levels while adjusting for age at assessment, gender, body mass index, horizontal femoral offset, head size, manufacturer hip type, and Oxford hip score.
Patients and Methods
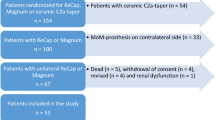
We prospectively followed 100 individuals (51 females, 49 males) with unilateral MOM hip resurfacing who underwent clinical assessment, CT scanning, and blood metal ion measurement. Multiple regression analysis was used to determine which variables were predictors of blood metal ion levels and to model the effect of these variables.
Results
Only cup inclination, version angles, and gender influenced blood cobalt or chromium levels. Cobalt and chromium levels positively correlated with inclination angle and negatively correlated with version angle. The effect of changes in version angle was less than for inclination angle. Based on our observations, we developed a formula to predict the effect of these parameters on metal ion levels.
Conclusions
Our data suggest insufficient cup version can cause high blood metal ions after MOM hip arthroplasty. We were unable to show that excessive version caused high levels.
Level of Evidence
Level II, prognostic study. See Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A recent study showed MOM bearings were used for 35% of patients undergoing hip arthroplasties in the United States [5]. Typically, the levels of circulating metal ions, cobalt (Co) and chromium (Cr), increase to 10 times the levels found in individuals without hip arthroplasties [20]. This prompted the US Food and Drug Administration to insist on prospective monitoring of patient blood levels of Co and Cr when it approved MOM hip resurfacing devices in 2006 [38] and 2007 [39]. The UK Medicines and Health Regulatory Agency recently issued guidelines recommending the use of blood metal ion levels to investigate patients with MOM hip arthroplasties [32].
The clinical effects of elevated metal ion levels include local tissue reactions [34], characterized by increases in T and B cells in the tissues surrounding the hip, and are associated with premature failure of the hip [11]. Systemically, one report suggests reduced numbers of CD8-positive T cells [20]. Therefore, establishing the risk factors for high metal ions levels in patients with MOM hips is clinically important.
The wear rate of MOM implants in hip simulator studies is influenced by patient activity [4], implant design [14], and implant positioning [1], factors that are common in all types of hip arthroplasties. Currently, the known clinical factors that affect metal ion levels include hip design [29], cup inclination angle [12, 18, 28], cup version angle [28, 29], and head size [28]. In the case of version, the effect is uncertain in that it was dependent on femoral head size [28] or hip design and metal ion level used (Co or Cr) [29]. All studies concerning cup angles and metal ions used plain radiographic measurement [12, 18, 28], which reportedly has lower accuracy and precision than CT [25], particularly for version. One study quantifying the error between radiographs and 3-D CT for large-diameter MOM hips found two standard deviation limits of agreements of +7° to −15° for cup inclination angle and +16° to −31° for cup version angle [19]. These were attributed partly to the cup face being obscured by the femoral head on plain radiographs and the accepted error of plain radiographs when compared with CT.
We therefore asked whether (1) the circulating level of blood metal ions was related directly to the 3-D orientation of the acetabular component in MOM hip arthroplasty and (2) these blood levels were related to any other device-specific factors (component position, size, and type) or patient-specific factors (gender, body mass index (BMI), age, and Oxford hip score).
Patients and Methods
We prospectively followed 100 patients attending a MOM hip clinic who had unilateral MOM hip resurfacing from July 2003 to January 2007. These patients were inherited when an adjacent hospital closed. We chose patients who were at least 1 year postoperative to minimize the effect of “running-in” wear, which increases the blood metal ion level, before it reaches a steady state [3]. Our initial exclusion criteria included abnormal glomerular filtration rate (GFR) because the kidney clears the blood of Co and Cr ions. However, no patient had an abnormal GFR. We screened for the following occupations known to result in exposure to metal ions: welders and wood preservers. No patients had these occupations. We planned to recruit at least 10 patients for each variable studied (n = 9), thus aiming for a minimum of 90 patients [34]. The minimum followup was 1.5 years (mean, 3 years, range, 1.5–5 years). No patients were lost to followup. No patients were recalled specifically for this study; all data were obtained from medical records and imaging. The institutional ethical review board approved the study.
The most common type of MOM implant was the Birmingham Hip Resurfacing® (BHR; Smith & Nephew, Warwick, UK) (n = 59). There were 35 patients with Cormet® implants (Corin, Gloucestershire, UK), two with ASR® implants (DePuy, Leeds, UK), one with a Durom® implant (Zimmer, Winterthur, Switzerland), and one with a Magnum® M2a implant (Biomet, Bridgend, South Wales, UK). The number of patients with ASR®, Durom®, and Biomet implants was small so their data were merged with data for patients with the Cormet® implants to generate a nonBHR category for statistical analysis.
Our routine followup consisted of annual clinical review (history and examination) and plain radiographs of the hips (AP and lateral), but for the period of the study (January 2008 to January 2009) we added CT scanning, and whole-blood analysis of Co and Cr. We chose factors reportedly associated with metal ion levels after MOM hip arthroplasty [4, 27, 29, 37]. These factors were those that most orthopaedic surgeons would find relevant to the cause of high wear rates of hip arthroplasties: blood Co and Cr levels, cup inclination angle, cup version angle, component horizontal femoral offset (HFO), femoral head component size (head size), manufacturing type (hip type), Oxford hip score [9] as a measure of activity, age at assessment, gender, and BMI (Table 1).
Whole-blood samples were collected in trace-element blood tubes (K2EDTA; Becton, Dickinson and Co, Franklin Lakes, NJ, USA) using the Vacutainer® system (Becton, Dickinson and Co). These trace-element tubes are certified low for metals. This system uses a stainless steel needle. Stainless steel contains 11% Cr and no Co. A previous study showed there was no measurable metal contamination from the stainless steel needle. Samples were made anonymous and stored at −20°C. Standard operating procedures were established for Co and Cr measurement in biologic fluids using dynamic reaction cell inductively coupled plasma mass spectrometry (DRC-ICPMS) (PerkinElmer Elan® DRCII; PerkinElmer, Waltham, MA, USA).
Low-radiation dose CT scanning was performed with 0.75-mm collimation (high resolution) and artifact minimization software (16 bit data processed on an extended scale), both of which enabled observation of the detail required to separate the metallic cup face from the large-diameter metallic femoral head. The radiation dose of this pelvic CT scan protocol was 1.7 mSv, equivalent to 8 months of background radiation. The radiation dose of a traditional pelvic CT scan is 10 mSv.
Acetabular inclination and version angles were measured using previously validated computer software [23], from Digital Imaging and Communications in Medicine (DICOM) images of CT scans of the pelvis. Using a 3-D reconstruction software package (Robin 3D software©; Robin Richards, London, UK)[7] the position of the pelvis was aligned with the anterior pelvic plane (APP). The plane of the cup face then was labeled using 20 computer-selected points around the edge of the cup face (Fig. 1). The plane of the cup face then was compared with (1) a transverse (or axial) plane orthogonal to the APP to determine the inclination angle (which is seen when viewed AP) and (2) the sagittal plane (also orthogonal to the APP, but also orthogonal to the transverse plane) to determine the version angle (which is seen when viewed axially). There were weak and positive correlations (r = 0.42, R2 = 0.18) between inclination and version (Fig. 2). All patients had well-fixed components observed on plain radiographs. However, some patients had substantial hip pain as shown by the range of values of the Oxford hip score (Table 1). The inclusion of the hip score data in the multiple regression analysis therefore was important to determine whether this was a confounding factor. Only two patients had the combination of low version (< 5°) with high inclination (> 50°).
A graph shows CT-measured 3-D cup positions for 100 unilateral MOM hip arthroplasties. The lowest and highest values of each inclination and version angle are shown. The box delineates the safe zone suggested by Lewinnek et al. [30] that most surgeons aim for.
We determined whether inclination and version angles determine Co and Cr levels adjusting for age at assessment, gender, BMI, component HFO, head size, implant type, and Oxford hip score. The issues of how many variables should be used in the model and what is a good model are complex. There are accepted rules of thumb to estimate sample size. Our chosen method was one of these [35]. Statistical analysis was performed using two separate analyses: one for Co and another for Cr. The models used for analyses were (multiple) linear regression and multivariate linear regression. Co and Cr also were analyzed simultaneously as we assumed the levels would correlate. This procedure provides regression analysis and ANOVA for multiple dependent variables (the outcome variables, Co and Cr) by one or more factor variables or covariates (the variables believed important in determining the wear rate of hip arthroplasties and therefore the blood metal ion level). Variables that were nonsignificant in the multivariate linear regression model were eliminated from the final model. The modeling and estimation of the effects of interest were performed using SPSS® 16 (SPSS Inc, Chicago, IL, USA). The level of significance used was 5%. We used the natural logarithm of Co and Cr. This transformation was needed because the scatterplots of Co and Cr versus inclination and version showed increasing variance with increasing angle, violating the assumption of constant variance in regression analysis.
Results
The circulating level of blood metal ions after MOM hip arthroplasty was related directly to the 3-D orientation of the acetabular component and gender but not BMI, femoral head size, or hip type. Initial inspection of the data using scatterplots revealed a wide range of metal ion levels, inclination, and version with only weak relationships between metal ion levels and either cup angle. Metal ion levels positively correlated with inclination (Table 2) but negatively correlated with version (Table 3). One interpretation is that insufficient version (< 10°) was associated with high metal ion levels, and we were unable to show a positive relationship for excessive version (> 20°). Inclination and version were positively correlated (r = 0.42). The multivariate analysis allowed the effects of the factors and covariates to be tested on the two responses simultaneously. Inclination, version, and gender had a greater estimated effect on Co levels (Table 2) when compared with Cr levels (Table 3).
The relationship between metal ion levels and inclination was exponential, with a sharp increase in metal ions when the inclination angle was greater than 45°. For a unit increase in inclination, the average level of Co changes by a factor of 1.045, or a 4.5% increase (equivalent to an increase of e0.044 or EXP(0.044)) (Fig. 3). For a unit increase in inclination, the average level of Cr changes by a factor of 1.033, or a 3.3% increase (equivalent to an increase of e0.032 or EXP(0.032)) (Fig. 4). The relationship between metal ion levels and version was negatively exponential, with a sharp decrease in metal ions when the version angle was less than 20°. For a unit increase in version, the average level of Co changed by a factor of 0.975, or a 2.5% decrease (equivalent to a decrease of e−0.025 or EXP(−0.025)) (Fig. 3). For a unit increase in version, the average level of Cr changes by a factor of 0.980, or a 2.0% decrease (equivalent to a decrease of e−0.020 or EXP(−0.020)) (Fig. 4).
The relationship between blood Co levels and cup angles is shown by two line plots of the final statistical model. The estimated blood Co levels (ppb) for a given (A) inclination angle with all other explanatory variables kept constant and version set at the median for the data of 24.1°, and (B) for a given version angle with all other explanatory variables kept constant and version set at the median for the data of 48.2° are shown.
The relationship between blood Cr levels and cup angles is shown in line plots of the final statistical model used to estimate blood Cr levels (ppb) for a given inclination angle with all other explanatory variables kept constant and the version set at the median for the data of (A) 24.1°, and (B) 48.2°.
A separate comparison of the BHR and Cormet implants did not improve the borderline effect of hip type on blood metal ion levels.
The formulas for the final statistical models were (with the variable gender equal to 1 for females and 0 for males): Cobalt = EXP(−1.067 +0.517*Gender +0.044*Inclination −0.025*Version); and Chromium = EXP (−0.643 +0.628*Gender +0.032*inclination −0.020*version).
Discussion
MOM hip arthroplasty is a commonly performed operation [5]. Pain and failure of MOM hip arthroplasty, which has been attributed to increased wear rate and pseudotumor formation [25, 26], are associated with higher blood metal ion levels when compared with those of patients with well-functioning hips [20]. The main surgically adjustable variable is cup inclination, but the effect of cup version is much less certain (Table 4), possibly because plain radiographic measurement of version has low validity [25]. We therefore asked whether (1) the circulating level of blood metal ion levels was related directly to 3-D orientation of the acetabular component in a MOM hip arthroplasty, and (2) these blood levels were related to any other device-specific factors (component position, size, and type) or patient-specific factors (gender, body mass index, age, and Oxford hip score).
Our study has limitations. First, not all variables that affect wear rate were studied. However, we did study nine different relevant factors. Second, it is difficult to quantify patient activity. Nevertheless, the Oxford hip score is a surrogate measure of patient activity [9] because it provides information regarding walking time, shopping, housework, and stair climbing. Third, we studied several hip designs with different cup articular arc angles (CAAA) [37]. However, with the exception of the two ASRs, all the remaining hips had a CAAA of 161° ± 4°. The effect on the version will be half this difference and probably is less than the error in measurement method of plain radiographs when compared with CT. Nevertheless, it is difficult to generalize our findings to all types of MOM implants. Fourth, we did not measure the effect of femoral version and combined (femoral and acetabular) version on metal ion levels. Last, studies such as the current one always will be limited by the number of patients with an extreme cup inclination and version. Although we were able to study a wide spread of values, the majority (65 cases) were within 10° of the safe zone suggested by Lewinnek et al. [30].
Our study contributes three findings concerning the relationship between blood metal ion levels and 3-D cup position. First, the association between metal ion levels and cup inclination was exponential (rather than a threshold). This agrees and builds on the current literature (Table 4). Second, cup version was negatively correlated with metal ion levels. Finally, we found no effect of femoral offset, manufacturer type, and head size as a predictor of metal ion levels [33]. Many studies report blood metal ion levels after MOM hip arthroplasty [2, 6, 8, 10, 15–17, 20–22, 24, 29, 36, 40, 41]. Our use of 3-D CT with extended scale scanning distinguished our study from the others and allowed us to view the cup face plane without the large diameter femoral head being obscured and to measure its position relative to the anterior pelvic plane. The exponential relationship between metal ions and inclination angle explains the reported cut-off levels of 55° [12] and 50° [18] cup inclinations. Our findings for insufficient version (< 10°) were similar to those found by Langton et al. [29], but our finding for excessive version (> 20°) was different. However, Desy et al. [13] reported no correlations between acetabular version angle and metal ion levels despite the analysis of many factors. It is possible that their univariate analysis of radiographically calculated version angles limited their interpretation. It is possible to clinically explain our results: high version causes posterior impingement and reduces activity. Hip simulators may clarify the relationship with version/ impingement more completely, but there currently is no published study. Our study is concordant with studies of ceramic-on-ceramic hips: insufficient version (< 15°) was associated with failure [42] and high wear rate [31]. Thus, insufficient or excessive version may contribute to a poor clinical outcome [28], but the mechanism is unlikely to involve increased blood metal ion levels.
Our finding that females had higher blood metal ion levels than males while adjusting for the other eight variables (including femoral head size) is interesting. It is possible that our study is underpowered for the confounding variables of head size and gender (ie, women are smaller than men). The UK National Joint Registry showed females had double the risk of failure of MOM hip resurfacing when compared with males [33]. The optimum cup position will be based on more than blood metal ion results, for example, patient factors such as impingement, distorted femoral anatomy, and pelvic tilt, and design variables. The patient with the highest blood metal ion levels (322 ppb and 151 ppb of Co and Cr, respectively) had an unfortunate combination of risk factors for high metal ion levels: 70° inclination, an ASR hip prosthesis, and female gender. Neurophysiologic and cardiac testing found no abnormalities. Revision was performed for unexplained pain and the patient’s metal ion levels returned to normal by 12 months after surgery.
Our observations of patients with MOM hip arthroplasties help clarify the relationship between cup inclination and version angles on blood metal ion levels: insufficient and not excessive cup version appear to contribute to high blood metal ion levels.
References
Angadji A, Royle M, Collins SN, Shelton JC. Influence of cup orientation on the wear performance of metal-on-metal hip replacements. Proc Inst Mech Eng H. 2009;223:449–457.
Antoniou J, Zukor DJ, Mwale F, Minarik W, Petit A, Huk OL. Metal ion levels in the blood of patients after hip resurfacing: a comparison between twenty-eight and thirty-six-millimeter-head metal-on-metal prostheses. J Bone Joint Surg Am. 2008;90(suppl 3):142–148.
Back DL, Young DA, Shimmin AJ. How do serum cobalt and chromium levels change after metal-on-metal hip resurfacing? Clin Orthop Relat Res. 2005;438:177–181.
Bowsher JG, Hussain A, Williams PA, Shelton JC. Metal-on-metal hip simulator study of increased wear particle surface area due to ‘severe’ patient activity. Proc Inst Mech Eng [H]. 2006;220:279–287.
Bozic KJ, Kurtz S, Lau E, Ong K, Chiu V, Vail TP, Rubash HE, Berry DJ. The epidemiology of bearing surface usage in total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009;91:1614–1620.
Clarke MT, Lee PT, Arora A, Villar RN. Levels of metal ions after small- and large-diameter metal-on-metal hip arthroplasty. J Bone Joint Surg Br. 2003;85:913–917.
Dandachli W, Islam SU, Liu M, Richards R, Hall-Craggs M, Witt J. Three-dimensional CT analysis to determine acetabular retroversion and the implications for the management of femoro-acetabular impingement. J Bone Joint Surg Br. 2009;91:1031–1036.
Daniel J, Ziaee H, Pradhan C, Pynsent PB, McMinn DJ. Blood and urine metal ion levels in young and active patients after Birmingham hip resurfacing arthroplasty: four-year results of a prospective longitudinal study. J Bone Joint Surg Br. 2007;89:169–173.
Dawson J, Fitzpatrick R, Carr A, Murray D. Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg Br. 1996;78:185–190.
De Haan R, Campbell P, Reid S, Skipor AK, De Smet K. Metal ion levels in a triathlete with a metal-on-metal resurfacing arthroplasty of the hip. J Bone Joint Surg Br. 2007;89:538–541.
De Haan R, Campbell PA, Su EP, De Smet KA. Revision of metal-on-metal resurfacing arthroplasty of the hip: the influence of malpositioning of the components. J Bone Joint Surg Br. 2008;90:1158–1163.
De Haan R, Pattyn C, Gill HS, Murray DW, Campbell PA, De Smet K. Correlation between inclination of the acetabular component and metal ion levels in metal-on-metal hip resurfacing replacement. J Bone Joint Surg Br. 2008;90:1291–1297.
Desy NM, Bergeron SG, Petit A, Huk OL, Antoniou J. Surgical variables influence metal ion levels after hip resurfacing. Clin Orthop Relat Res. 2010 Oct 23. [Epub ahead of print].
Dowson D, Hardaker C, Flett M, Isaac GH. A hip joint simulator study of the performance of metal-on-metal joints: Part II: design. J Arthroplasty 2004;19:124–130.
Dunstan E, Sanghrajka AP, Tilley S, Unwin P, Blunn G, Cannon SR, Briggs TW. Metal ion levels after metal-on-metal proximal femoral replacements: a 30-year follow-up. J Bone Joint Surg Br. 2005;87:628–631.
Grover M, Sauve P, Mountney J, Khan T, De Beer J, Higgins B. Metal ion levels after metal-on-metal Ring total hip replacement: a 30-year follow-up study. J Bone Joint Surg Br. 2007;89:586–590.
Grubl A, Weissinger M, Brodner W, Gleiss A, Giurea A, Gruber M, Poll G, Meisinger V, Gottsauner-Wolf F, Kotz R. Serum aluminium and cobalt levels after ceramic-on-ceramic and metal-on-metal total hip replacement. J Bone Joint Surg Br. 2006;88:1003–1005.
Hart AJ, Buddhdev P, Winship P, Faria N, Powell JJ, Skinner JA. Cup inclination angle of greater than 50 degrees increases whole blood concentrations of cobalt and chromium ions after metal-on-metal hip resurfacing. Hip Int. 2008;18:212–219.
Hart AJ, Dandachli W, Schleuter-Brust K, Henckel J, Cobb JP. Large ball metal on metal hips obscure cup angle measurement on plain radiographs. Hip Int. 2009;19:323–329.
Hart AJ, Sabah S, Henckel J, Lewis A, Cobb J, Sampson B, Mitchell A, Skinner JA. The painful metal-on-metal hip resurfacing. J Bone Joint Surg Br. 2009;91:738–744.
Hart AJ, Skinner JA, Winship P, Faria N, Kulinskaya E, Webster D, Muirhead-Allwood S, Aldam CH, Anwar H, Powell JJ. Circulating levels of cobalt and chromium from metal-on-metal hip replacement are associated with CD8+ T-cell lymphopenia. J Bone Joint Surg Br. 2009;91:835–842.
Heisel C, Silva M, Skipor AK, Jacobs JJ, Schmalzried TP. The relationship between activity and ions in patients with metal-on-metal bearing hip prostheses. J Bone Joint Surg Am. 2005;87:781–787.
Henckel J, Richards R, Lozhkin K, Harris S, Baena FM, Barrett AR, Cobb JP. Very low-dose computed tomography for planning and outcome measurement in knee replacement. The imperial knee protocol. J Bone Joint Surg Br. 2006;88:1513–1518.
Jacobs JJ, Skipor AK, Patterson LM, Hallab NJ, Paprosky WG, Black J, Galante JO. Metal release in patients who have had a primary total hip arthroplasty: a prospective, controlled, longitudinal study. J Bone Joint Surg Am. 1998;80:1447–1458.
Kalteis T, Handel M, Herold T, Perlick L, Paetzel C, Grifka J. Position of the acetabular cup: accuracy of radiographic calculation compared to CT-based measurement. Eur J Radiol. 2006;58:294–300.
Kwon YM, Glyn-Jones S, Simpson DJ, Kamali A, McLardy-Smith P, Gill HS, Murray DW. Analysis of wear of retrieved metal-on-metal hip resurfacing implants revised due to pseudotumours. J Bone Joint Surg Br. 2010;92:356–361.
Langton DJ, Jameson SS, Joyce TJ, Hallab NJ, Natu S, Nargol AV. Early failure of metal-on-metal bearings in hip resurfacing and large-diameter total hip replacement: a consequence of excess wear. J Bone Joint Surg Br. 2010;92:38–46.
Langton DJ, Jameson SS, Joyce TJ, Webb J, Nargol AV. The effect of component size and orientation on the concentrations of metal ions after resurfacing arthroplasty of the hip. J Bone Joint Surg Br. 2008;90:1143–1151.
Langton DJ, Sprowson AP, Joyce TJ, Reed M, Carluke I, Partington P, Nargol AV. Blood metal ion concentrations after hip resurfacing arthroplasty: a comparative study of articular surface replacement and Birmingham Hip Resurfacing arthroplasties. J Bone Joint Surg Br. 2009;91:1287–1295.
Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217–220.
Lusty PJ, Watson A, Tuke MA, Walter WL, Walter WK, Zicat B. Wear and acetabular component orientation in third generation alumina-on-alumina ceramic bearings: an analysis of 33 retrievals [corrected]. J Bone Joint Surg Br. 2007;89:1158–1164.
MHRA. Medical Device Alert MDA/2010/033: All metal-on-metal (MOM) hip replacements. Available at: http://www.mhra.gov.uk/Publications/Safetywarnings/MedicalDeviceAlerts/CON079157. Accessed April 29, 2011.
National Joint Registry. 5th Annual report. Available at: www.njrcentre.org.uk . Accessed April 29, 2011.
Pandit H, Glyn-Jones S, McLardy-Smith P, Gundle R, Whitwell D, Gibbons CL, Ostlere S, Athanasou N, Gill HS, Murray DW. Pseudotumours associated with metal-on-metal hip resurfacings. J Bone Joint Surg Br. 2008;90:847–851.
Petrie A. Statistics in orthopaedic papers. J Bone Joint Surg Br. 2006;88:1121–1136.
Sauve P, Mountney J, Khan T, De Beer J, Higgins B, Grover M. Metal ion levels after metal-on-metal Ring total hip replacement: a 30-year follow-up study. J Bone Joint Surg Br. 2007;89:586–590.
Shimmin AJ, Walter WL, Esposito C. The influence of the size of the component on the outcome of resurfacing arthroplasty of the hip: a review of the literature. J Bone Joint Surg Br. 2010;92:469–476.
United States Food and Drug Administration. New Device Approval: Birmingham Hip Resurfacing P040033. May 9, 2006. Available at: http://www.fda.gov/cdrh/mda/docs/p040033.html. Accessed February 24, 2009.
United States Food and Drug Administration. New Device Approval: Cormet Hip Resurfacing P050016. July 3, 2007. Available at: http://www.fda.gov/cdrh/mda/docs/P050016.html. Accessed February 24, 2009.
Vendittoli PA, Ganapathi M, Lavigne M. Blood and urine metal ion levels in young and active patients after Birmingham hip resurfacing arthroplasty. J Bone Joint Surg Br. 2007;89:989.
Vendittoli PA, Mottard S, Roy AG, Dupont C, Lavigne M. Chromium and cobalt ion release following the Durom high carbon content, forged metal-on-metal surface replacement of the hip. J Bone Joint Surg Br. 2007;89:441–448.
Walter WL, O’Toole GC, Walter WK, Ellis A, Zicat BA. Squeaking in ceramic-on-ceramic hips: the importance of acetabular component orientation. J Arthroplasty. 2007;22:496–503.
Acknowledgments
We thank Gwynneth Lloyd for assistance in coordinating the additional investigations for the followup clinics, Prof. Justin Cobb for general support in the hospital for the study, and Prof. Jonathan Powell for assistance in data analysis.
Author information
Authors and Affiliations
Corresponding author
Additional information
The institution of one or more of the authors (AH and JS) has received funding from the British Orthopaedic Association (BOA) through an industry consortium of nine manufacturers: Depuy, Zimmer, Smith & Nephew, Biomet, JRI, Finsbury, Corin, Mathys and Stryker.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Imperial College London.
About this article
Cite this article
Hart, A.J., Skinner, J.A., Henckel, J. et al. Insufficient Acetabular Version Increases Blood Metal Ion Levels after Metal-on-metal Hip Resurfacing. Clin Orthop Relat Res 469, 2590–2597 (2011). https://doi.org/10.1007/s11999-011-1930-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-011-1930-y