Abstract
Background
Hip fractures in the elderly are common and associated with considerable mortality and disability. Although well known in industrialized countries, the factors associated with mortality after hip fractures are not reported frequently in developing countries and little is known regarding risk factors in Latin America.
Questions/Purpose
We investigated the rate of 1-year mortality and prefracture and fracture characteristics associated with mortality after a hip fracture in elderly Brazilian patients in a large metropolitan area.
Methods
Two hundred forty-six persons 60 years and older admitted to four hospitals in Rio de Janeiro were included after experiencing fractures and were followed for 1 year. Data were collected on sociodemographic, health, and functional status; type of surgery; length of stay; and complications after surgery. Cox regression analyses were conducted to investigate factors associated with 1-year mortality after hip fracture.
Results
Of the 246 patients, 86 died (35%). Of those 86, 22 died in the hospital (25.6%) and 64 (74.4%) died after discharge. Functional status before fracture, older age, male gender, and higher surgical risk increased the risk of mortality, whereas the use of antibiotics and the use of physical therapy after surgery decreased the risk.
Conclusions
Our mortality rate was higher than those reported from industrialized countries. The use of antibiotics and physical therapy are potentially modifiable factors to improve patients’ survival after fracture in Brazil.
Level of Evidence
Level II, prognostic study. See the Guidelines for Authors for a complete description of the levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hip fracture is one of the most feared consequences of osteoporosis. Hip fractures are associated with high postfracture disability, increased mortality, and high healthcare expenditures [8, 29]. It has been estimated the number of hip fractures will increase by 310% in men and 240% in women by 2025, owing to aging of the population [30]. A large Danish study showed persons with a hip fracture had a hazard ratio of 3.84 of dying in the next year compared with age- and gender-matched control subjects [54]. One study estimated that in 1990 worldwide there were 1.31 million new hip fractures, which led to 736,000 deaths and 2.9 million disability adjusted life-years [29]. Between 1999 and 2002 in the United States, Medicare spent almost $3-billion (USD) per year for health care related to hip fractures [2], and another study showed the costs related to hip fracture were approximately $31,000 (USD) for health care up to 6 months after fracture [34].
Two retrospective chart studies examined mortality after hip fractures in elderly Brazilians. In the first (65 patients) study, the 1-year mortality rate was reported as 30% [15]. In the second study, 89 charts were reviewed and an in-hospital mortality of 14% but no 1-year mortality was reported [38]. In one small prospective study (56 patients), a mortality rate of 23% after 6 months was reported, but factors that predicted mortality were not evaluated [11].
The reasons for the increased mortality attributable to hip fracture have been investigated mostly in developed countries, but they are not reported frequently from developing countries [48]. The additional mortality may be attributable to complications after the fracture such as pulmonary embolism and infections or to comorbid conditions already present before the fracture [32]. Several studies document comorbid diseases and prefracture health status are associated with the 1-year postfracture mortality [28, 46, 52], whereas others show no influence of these factors [10, 55]. Studies from developed countries suggest preoperative factors increasing the risk of mortality are race (nonwhite) [27, 42], old age [10, 12, 28, 52], presence of dementia [24, 42], male gender [12, 24, 33, 42], serious concomitant illness [10, 12, 33, 52], low body mass index (BMI) [24], low handgrip strength [37], not walking outdoors before fracture [37], history of hip fracture [4], delirium at admission [9], postoperative complications [46], high preoperative risk score [24, 44], and postoperative mobility [25]. In developing countries, orthopaedic services are less available. One study suggests the cost of a hospital stay for a patient with a hip fracture in 2004 was 13% of the total expenditures for hospital care for adults in Brazil [41]. The population in Brazil, as in other Latin American countries and other developing countries, is aging rapidly, and the incidence of hip fractures is expected to increase the most in developing countries [19, 29]. Identifying the variables influencing mortality in these countries potentially would allow the development of interventions to improve recovery and reduce mortality [1].
We therefore (1) determined the rate of 1-year mortality and (2) identified prefracture and fracture characteristics associated with mortality after a hip fracture in elderly Brazilian patients.
Patients and Methods
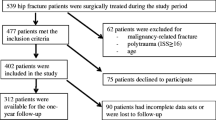
In January 2001, we initiated a longitudinal prospective study at four municipal hospitals in Rio de Janeiro, Brazil. These hospitals accounted for 55% of hip fracture surgeries covered by the Brazilian Public Health System (SUS) in Rio de Janeiro in 2000. These four hospitals were chosen because they deal with the majority of the hip fractures in older patients, as they have an intensive care unit available. Not all hospitals in Rio de Janeiro have an orthopaedics department. Partly these four hospitals were chosen for practical reasons as the study physician (SRMP) coordinated the study, recruited, and interviewed all patients. From April to November 2001, 270 subjects 60 years and older admitted consecutively with a femoral neck or intertrochanteric fracture attributable to a fall were eligible for the study. Patients with a fracture attributable to a traffic trauma or who had a pathologic fracture attributable to cancer were not eligible for inclusion in the study. For patients who for cognitive reasons or physical reasons were unable to participate in the study by themselves, a family member was approached and gave proxy consent. Data were collected for these 270 patients during the first hospital admission attributable to a hip fracture from an interview and from medical charts. During the hospital stay, data on admission, type of fracture, anesthesia and surgery, comorbidities, and medication use were extracted from the medical chart. Eighteen patients were unable to participate in the interview during the hospital admission and a family member responded to questions. Patients needed to provide a valid address when admitted to the hospital to be contacted for the followup interview. In Rio de Janeiro, patients are required to go to the hospital nearest their home to receive treatment. Patients in Rio de Janeiro commonly provide incorrect address information so they can be treated in a certain hospital and 10 patients were excluded because they could not be contacted for followup. Twelve of the 270 patients could not be located in the hospital to conduct the interview. Two individuals refused to participate in the study. Thus, the final sample included 246 of the 270 subjects (91%) from four hospitals. Nonresponse analysis was conducted to compare the participants with the excluded patients and there were no differences regarding age, gender, and marital status. One year after the hip fracture, all living patients were interviewed at home by the study geriatrician (SRMP). The research ethics committees from all four hospitals approved the study and verbal informed consent was obtained from all participants.
After 1 year, 86 patients had died (35.0%). The date of death was reported by a family member when they were contacted for the followup interview. All remaining patients (n = 160) participated in the followup interview. However, for 19 of those patients, a proxy helped to answer questions.
To measure functional status, the Brazil Old Age Schedule questionnaire [53] was used as it was validated in Portuguese in Brazil. The version used has 10 items: can you (1) use public transportation on your own (bus, van, taxi, train, subway, ferry, etc); (2) walk outdoors on your own; (3) feed yourself; (4) dress yourself; (5) walk inside the house on your own; (6) climb stairs on your own; (7) get out of bed on your own; (8) bathe yourself; (9) control your bladder; and (10) go to the toilet on your own. The answer categories are (0) yes or (1) no. Scores ranged from zero, for the patient who was not disabled, to 10, for an individual who was disabled in all these activities. The number of functional limitations was grouped for the analyses.
The following health and sociodemographic variables were obtained from the medical charts. Gender, age, and marital status were recorded. Marital status was classified as single, married, divorced, or widowed, and for analyses, it was grouped into married versus other. Ethnicity was classified as white, black, or not white/not black.
Site of fall, type of fracture, traction used before surgery, number of days between admission and surgery, number of days between fracture and hospital admission, total length of hospital stay, and surgical risk score (American Society of Anesthesiologists [ASA] score [40]) were obtained. Site of fall was classified into two categories: outside the house versus inside the house. Type of hip fracture was classified as neck of the femur versus intertrochanteric for the analyses. The ASA risk scores 1 and 2 were combined into low risk and 3 and 4 into high risk. Type of surgery, anesthesia used during the operation, perioperative or postoperative complications (only bleeding, infection of surgical site, and thrombosis [including cerebrovascular accident, venous thrombosis of legs, pulmonary embolism, and arterial embolism of legs] were available), and traction used before surgery (yes/no) were recorded. Furthermore, medication use before and after surgery (use of antihypertensive, sedatives/antipsychotics/anxiolytics, oral hypoglycemic medication, antiinflammatory medications, antidepressants, antiParkinson, antibiotics, antiarrhythmics, bronchodilators, hormones, anticoagulant/platelet aggregation inhibitors, inotropic medication; all yes/no variables) and comorbid diseases (diabetes mellitus, chronic obstructive pulmonary disease, stroke, cardiovascular disease, depression, cataract, glaucoma, hearing impairment, hypertension, and urinary incontinence; all yes/no variables) were assessed at admission and abstracted from the medical charts. Type of surgery was classified as arthroplasty or osteosynthesis. Anesthesia used during the surgery was classified as general or epidural anesthesia (including spinal anesthesia). Furthermore, from the medical chart, it was assessed where the patient was discharged to and classified as home or other (nursing home, to stay with a family member, or to stay with another person). Delirium after surgery was determined by using information from progress notes of the doctors and nurses in charge or determined during the interview by the study geriatrician (SRMP). No assessment instruments were used.
The following variables were asked of the patient. Education level was assessed by asking the number of years of school attended. Educational level was classified in five groups: illiterate, 1 to 4 years, 5 to 8 years, 9 to 11 years, and 12 years and more. Living arrangements were dichotomized as living alone or not. Patients were asked if they were still working before the fracture (yes/no). Weight was assessed using a calibrated scale. Height was assessed in the hospital for patients who were able to stand up straight. When patients were unable to stand up straight, he or she was asked to lie down on his or her back in the bed and height was estimated using a similar measurement. BMI was calculated and was classified as underweight (BMI < 22.0), normal (BMI = 22–27), and overweight/obesity (BMI > 27) [35]. Asking the patient whether he or she had experienced dizziness and balance problems assessed self-reported dizziness before fracture. Physical therapy (yes/no) was assessed by asking the patients if they had received physical therapy after the hospitalization.
Time until death after fracture was calculated using the date of death given by the family member and the date of fracture obtained from the medical chart. Descriptive t tests and chi square tests were performed to assess differences between patients who died (86) and patients who survived (160) 1 year after hip fracture.
We conducted Cox regression analyses to investigate the risk factors for mortality. The correlations between all factors were examined and were less than 0.6, so all the variables could be combined in a multivariable model. For all single risk factors, the association with mortality was examined using Cox’s proportional-hazards models adjusted for age and gender. All variables associated with mortality with a p value less than 0.10 were entered in one model adjusting for age and gender. A final model was constructed using a manual backward selection method to delete nonsignificant variables from the final model using the −2 log likelihood test. For the variable ASA risk score, there were 35 patients with missing information, and these were classified as missing (separate dummy variable in the analyses). For the other variables, six patients were missing information on location of the fall, 15 were missing information for type of surgery, five were missing information for BMI, and three were missing information for level of education. The univariate analyses were performed on the complete cases for each of the variables. The multivariate model was performed using only the complete cases for all the variables retained from the univariate analyses (n = 240, 97.6% of total sample). All the analyses were performed using the statistical package SPSS® Version 15.0 (SPSS Inc, Chicago, IL).
Results
Eighty-six patients died, resulting in a 1-year mortality of 35.0% (Table 1). Of the 67 men, 29 men died (43.3%), and of the 179 women, 57 women died (31.8%) within the first year after fracture. Of the 86, 22 died in the hospital within 30 days (25.6% of those who died), therefore, the in-hospital mortality rate/30-day mortality rate was 8.9%. Sixty-four patients (74.4% of those who died) died after discharge. Of those who died in the hospital/within 30 days, 50% were women and 50% were men. Fifteen patients died before undergoing surgery.
Seven patients died of pneumonia, one died of pulmonary embolism, one died of cerebral hemorrhagic event, and one died of hypoglycemia. For the five others, no cause of death was noted in the medical chart. Those who died before surgery more often were male (53.8% versus 25.5% of those who had surgery, p = 0.019), slightly older (84.0 years versus 78.8 years, p = 0.036), and had more functional limitations (3.4 versus 1.2, p = 0.025). There were no differences in number of comorbid conditions, type of fracture, or location of the fall. There were no differences in marital status, level of education, or ethnicity.
In the univariate Cox regression analyses, the number of functional limitations, age, gender, having diabetes, having had a cardiovascular accident, and higher surgical risk all were associated with increased risk of mortality (Table 2). The use of antibiotics after surgery and physical therapy after surgery were associated with decreased risk of mortality in the univariate analyses (Table 2). In the multivariable analyses, the hazard ratio (HR) was 1.75 for patients with one to two functional limitations, 1.18 for patients with three to four limitations, and 4.35 for patients with five or more limitations compared with the reference group without limitations (Table 2). The HR was 3.07 for patients 70 to 79 years old and 6.48 for patients 80 years or older compared with the reference group (60–69 years). Men had a HR of 2.04 compared with women. Patients with ASA scores of 3 or 4 had a HR of 2.15 compared with patients with ASA scores of 1 or 2. The use of antibiotics after surgery and the use of physical therapy decreased the risk of mortality (HR for use of antibiotics, 0.51; HR for use of physical therapy, 0.32).
Discussion
Hip fractures in the elderly are common and associated with considerable mortality and disability. The factors associated with mortality after hip fractures have not been studied often in developing countries. In a prospective study, we therefore (1) determined the rate of 1-year mortality and (2) identified prefracture and fracture characteristics associated with mortality after a hip fracture in Brazilian elderly.
We acknowledge several limitations. First, we relied on the reported date of death by family members. We suspect this would not substantially affect the data as family members would not likely misreport the death of another family member. Second is our small sample size, which might lead to our findings being less generalizable to the population in Brazil. Owing to practical reasons, we did not recruit subjects in additional hospitals (particularly outside a metropolitan area) or for a longer time. However, in this study, patients were from the four major hospitals, representing 55% of the total population with hip fractures in Rio de Janeiro annually, and our loss to followup was low; patients died, but no participant refused to do the followup interview, thereby reducing selection bias. Third, some information obtained from the charts had missing data, eg, the ASA risk scores were missing for 35 patients; these patients were grouped as a separate category and kept in the analyses. For the other variables, the amount of missing data was very low. Fourth, use of the charts gave information without having to bother the patient, who usually is in considerable pain and discomfort before the surgery. In addition, we relied on proxy information for some patients unable to participate with interviews, although the number of proxy interviews was small (n = 18). The use of proxies allowed us to follow patients who otherwise would have been lost to followup. Finally, our findings from metropolitan hospitals in Brazil might be less generalizable to developed Western countries with different healthcare systems. However, as the other countries in Latin America have similar healthcare systems and the populations are aging as rapidly as the Brazilian population, our results might be generalizable to other Latin American countries. The strengths of our study are that we used a prospective design, had a 1-year followup, had consecutive recruitment of all patients with first hip fracture, had a high response rate, and examined a wide array of risk factors.
Our first aim was to determine the 1-year mortality rate. Our in-hospital mortality rate was 8.9%, whereas our 1-year mortality rate was 35.0%. The in-hospital mortality varies considerably among countries, which might reflect different inclusion and exclusion criteria. Previous studies in Canada [28] and Italy [12] have had in-hospital mortality rates of 6.3% versus 5.4%, respectively. Studies from the United States have shown low in-hospital mortality rates of 1.6% and 1.8% [7, 23]. In another study from a developing country, Thailand, an in-hospital mortality of only 2.1% and a 1-year mortality of only 17% were reported. Previous retrospective studies from Brazil have reported 6.5% in-hospital mortality [15]. The 1-year mortality of 35% in our study was high compared with the rates in previous studies from developed countries, in which mortality rates were reported between 15% and 25% [6, 16, 18, 20, 21, 31], but in agreement with previous reports from Brazil by Garcia et al. [15] who reported 30% and Fortes et al. [11] who reported 23% after 6 months. Our 1-year mortality rate is in disagreement with that of Vidal et al. [56] who reported a rate of 21.5%. But those analyses were restricted to patients who had undergone surgery, whereas in our prospective study, 15 patients (6.1%) died before the surgery.
The second aim of our study was to examine prefracture and fracture characteristics associated with mortality. Functional status before fracture, older age, male gender, and higher surgical risk increased the risk of mortality, whereas the use of antibiotics and physical therapy after surgery decreased the risk. Previous studies showed functional status before fracture [14, 42, 45, 52], male gender [12, 15, 28, 33, 36, 42, 47], older age [10, 15, 28, 36, 43, 47, 50, 52, 55], and higher ASA scores predicted mortality in older patients [24, 26, 33, 44, 49] (Table 3), which is in agreement with our findings. In our study, we did not see a difference in mortality between patients undergoing arthroplasty versus patients undergoing osteosynthesis, which is in agreement with mortality reported by Garcia et al. [15] and others [18, 33, 37]. However, others have reported an increased mortality rate for patients who had arthroplasties [39, 54]. It has been suggested the reason for this increased mortality after arthroplasty could be higher use of arthroplasty with older age, but so far the evidence is inconclusive [18, 54]. Finally, many authors have reported the impact of comorbid conditions on mortality [10, 12, 14, 28, 36, 37, 42, 46, 47, 50–52], whereas we did not observe this. This might be attributable to our measurement of comorbid conditions. We had to rely on the hospital charts in which the comorbid condition was recorded as yes/no and we did not have the level of severity. However, in our study, functional limitations were a strong predictor of mortality, which might have captured some of the effect of the comorbid conditions.
The use of antibiotics perioperatively [3] and the use of physical therapy postoperatively improves recovery, although the best form of physical therapy has yet to be determined [3, 5, 22, 25]. Only 162 of the 246 patients (66%) received prophylactic antibiotics after surgery, although antibiotics reportedly prevent infections after hip surgery [17]. For our study patients, there was no antibiotic used preoperatively unless there was a clinical diagnosis such as urinary tract infection. The antibiotics were administered to patients within 60 minutes of the surgery in the operating room. The antibiotics were continued for 2 days unless there was an infection in which case they were continued for a longer period. Unfortunately, antibiotics after surgery are not always available. This unavailability of antibiotics in the public health system is not rare. On some days, there are no antibiotics, so none of the patients receive them, whereas on other days, it is available and all patients receive them. Making antibiotics more available in Brazil for older patients after surgery may increase their survival after hip fracture. Fortes et al. [11] reported 46% of the mortality was attributable to infections. In our study, 12 patients who died after surgery died of pneumonia and 14 patients had urinary tract infections after surgery. Furthermore, a previous Brazilian study also reported the use of physical therapy was associated with decreased mortality [38]. Not all the patients undergoing surgery for a hip fracture receive postoperative physical therapy. At the time of our study, in-hospital physical therapy programs were not available in any of the four hospitals. Therefore, this finding might be because only patients with good functional status after discharge and/or patients who lived in better socioeconomic circumstances who could afford physical therapy and the associated costs of transportation received physical therapy. However, these factors are modifiable and could improve survival of patients in Brazil after hip fracture surgery. With the expected increase in the older population in Brazil, these are relevant interventions to prevent morbidity and mortality after a hip fracture.
The 1-year mortality after hip fracture was high, 35%. Men and patients with more prefracture functional limitations and higher surgical risk had an increased risk of mortality. As the population of Brazil ages and orthopaedic services and osteoporosis treatment are not as widely available in Brazil, a large increase in the incidence of hip fractures can be expected. In developed countries, despite the increase in proportion of older persons, the mortality rate attributable to hip fractures has not changed during the last 40 years as a result of improvements in medical management of hip fractures (early surgery, better operative techniques, better nursing and community care for patients) [21]. It is less clear how aging of the population in Brazil and increase in hip fractures will develop with time. Patients who received physical therapy and antibiotics after surgery had a lower risk of mortality, showing potentially modifiable factors to improve survival after hip fracture surgery.
References
Alegre-Lopez J, Cordero-Guevara J, Alonso-Valdivielso JL, Fernandez-Melon J. Factors associated with mortality and functional disability after hip fracture: an inception cohort study. Osteoporos Int. 2005;16:729–736.
Bass E, French DD, Bradham DD. A national perspective of Medicare expenditures for elderly veterans with hip fractures. J Am Med Dir Assoc. 2008;9:114–119.
Beaupre LA, Jones CA, Saunders LD, Johnston DW, Buckingham J, Majumdar SR. Best practices for elderly hip fracture patients: a systematic overview of the evidence. J Gen Intern Med. 2005;20:1019–1025.
Berry SD, Samelson EJ, Hannan MT, McLean RR, Lu M, Cupples LA, Shaffer ML, Beiser AL, Kelly-Hayes M, Kiel DP. Second hip fracture in older men and women: the Framingham Study. Arch Intern Med. 2007;167:1971–1976.
Chudyk AM, Jutai JW, Petrella RJ, Speechley M. Systematic review of hip fracture rehabilitation practices in the elderly. Arch Phys Med Rehabil. 2009;90:246–262.
Cooper C, Atkinson EJ, Jacobsen SJ, O’Fallon WM, Melton LJ III. Population-based study of survival after osteoporotic fractures. Am J Epidemiol. 1993;137:1001–1005.
Cornwall R, Gilbert MS, Koval KJ, Strauss E, Siu AL. Functional outcomes and mortality vary among different types of hip fractures: a function of patient characteristics. Clin Orthop Relat Res. 2004;425:64–71.
Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359:1761–1767.
Dolan MM, Hawkes WG, Zimmerman SI, Morrison RS, Gruber-Baldini AL, Hebel JR, Magaziner J. Delirium on hospital admission in aged hip fracture patients: prediction of mortality and 2-year functional outcomes. J Gerontol A Biol Sci Med Sci. 2000;55:M527–M534.
Farahmand BY, Michaelsson K, Ahlbom A, Ljunghall S, Baron JA; Swedish Hip Fracture Study Group. Survival after hip fracture. Osteoporos Int. 2005;16:1583–1590.
Fortes EM, Raffaelli MP, Bracco OL, Takata ET, Reis FB, Santili C, Lazaretti-Castro M. [High morbidity-mortality and reduced level of osteoporosis diagnosis among elderly people who had hip fractures in Sao Paulo City] [in Portuguese]. Arq Bras Endocrinol Metabol. 2008;52:1106–1114.
Franzo A, Francescutti C, Simon G. Risk factors correlated with post-operative mortality for hip fracture surgery in the elderly: a population-based approach. Eur J Epidemiol. 2005;20:985–991.
Furlaneto ME, Garcez-Leme LE. Delirium in elderly individuals with hip fracture: causes, incidence, prevalence, and risk factors. Clinics. 2006;61:35–40.
Furlaneto ME, Garcez-Leme LE. Impact of delirium on mortality and cognitive and functional performance among elderly people with femoral fractures. Clinics. 2007;62:545–552.
Garcia R, Leme MD, Garcez-Leme LE. Evolution of Brazilian elderly with hip fracture secondary to a fall. Clinics. 2006;61:539–544.
Gdalevich M, Cohen D, Yosef D, Tauber C. Morbidity and mortality after hip fracture: the impact of operative delay. Arch Orthop Trauma Surg. 2004;124:334–340.
Gillespie WJ, Walenkamp G. Antibiotic prophylaxis for surgery for proximal femoral and other closed long bone fractures. Cochrane Database Syst Rev. 2001;1:CD000244.
Giversen IM. Time trends of mortality after first hip fractures. Osteoporos Int. 2007;18:721–732.
Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporos Int. 1997;7:407–413.
Haentjens P, Autier P, Barette M, Venken K, Vanderschueren D, Boonen S; Hip Fracture Study Group. Survival and functional outcome according to hip fracture type: a one-year prospective cohort study in elderly women with an intertrochanteric or femoral neck fracture. Bone. 2007;41:958–964.
Haleem S, Lutchman L, Mayahi R, Grice JE, Parker MJ. Mortality following hip fracture: trends and geographical variations over the last 40 years. Injury. 2008;39:1157–1163.
Handoll HH, Sherrington C. Mobilisation strategies after hip fracture surgery in adults. Cochrane Database Syst Rev.2007;1:CD001704.
Hannan EL, Magaziner J, Wang JJ, Eastwood EA, Silberzweig SB, Gilbert M, Morrison RS, McLaughlin MA, Orosz GM, Siu AL. Mortality and locomotion 6 months after hospitalization for hip fracture: risk factors and risk-adjusted hospital outcomes. JAMA. 2001;285:2736–2742.
Hasegawa Y, Suzuki S, Wingstrand H. Risk of mortality following hip fracture in Japan. J Orthop Sci. 2007;12:113–117.
Heinonen M, Karppi P, Huusko T, Kautiainen H, Sulkava R. Post-operative degree of mobilization at two weeks predicts one-year mortality after hip fracture. Aging Clin Exp Res. 2004;16:476–480.
Hommel A, Ulander K, Bjorkelund KB, Norrman PO, Wingstrand H, Thorngren KG. Influence of optimised treatment of people with hip fracture on time to operation, length of hospital stay, reoperations and mortality within 1 year. Injury. 2008;39:1164–1174.
Jacobsen SJ, Goldberg J, Miles TP, Brody JA, Stiers W, Rimm AA. Race and sex differences in mortality following fracture of the hip. Am J Public Health. 1992;82:1147–1150.
Jiang HX, Majumdar SR, Dick DA, Moreau M, Raso J, Otto DD, Johnston DW. Development and initial validation of a risk score for predicting in-hospital and 1-year mortality in patients with hip fractures. J Bone Miner Res. 2005;20:494–500.
Johnell O, Kanis JA. An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos Int. 2004;15:897–902.
Johnell O, Kanis J. Epidemiology of osteoporotic fractures. Osteoporos Int. 2005;16(suppl 2):S3–S7.
Johnell O, Kanis JA, Oden A, Sernbo I, Redlund-Johnell I, Petterson C, De Laet C, Jönsson B. Mortality after osteoporotic fractures. Osteoporos Int. 2004;15:38–42.
Kanis JA, Oden A, Johnell O, De Laet C, Jonsson B, Oglesby AK. The components of excess mortality after hip fracture. Bone. 2003;32:468–473.
Karagiannis A, Papakitsou E, Dretakis K, Galanos A, Megas P, Lambiris E, Lyritis GP. Mortality rates of patients with a hip fracture in a southwestern district of Greece: ten-year follow-up with reference to the type of fracture. Calcif Tissue Int. 2006;78:72–77.
Kilgore ML, Morrisey MA, Becker DJ, Gary LC, Curtis JR, Saag KG, Yun H, Matthews R, Smith W, Taylor A, Arora T, Delzell E. Health care expenditures associated with skeletal fractures among Medicare beneficiaries, 1999–2005. J Bone Miner Res. 2009 May 19 [Epub ahead of print].
Lipschitz DA. Screening for nutritional status in the elderly. Prim Care. 1994;21:55–67.
Mesquita GV, Abreu Lima MALT, Santos AMR, Alves EM, Brito JNPO, Martins MCC. [Morbid-mortality in elderly due to proximal fractures of the femur] [in Portuguese]. Texto Contexto Enferm, Florianópolis. 2009;18:67–73.
Meyer HE, Tverdal A, Falch JA, Pedersen JI. Factors associated with mortality after hip fracture. Osteoporos Int. 2000;11:228–232.
Muniz CF, Arnaut AC, Yoshida M, Trelha CS. [Characterization of aged patients with proximal femoral fractures in a public school hospital care] [in Portuguese]. Revista Espaco para a Saude. 2007;8:33–38.
Muraki S, Yamamoto S, Ishibashi H, Nakamura K. Factors associated with mortality following hip fracture in Japan. J Bone Miner Metab. 2006;24:100–104.
Owens WD, Felts JA, Spitznagel EL Jr. ASA physical status classifications: a study of consistency of ratings. Anesthesiology. 1978;49:239–243.
Peixoto SV, Giatti L, Afradique ME, Lima-Costa MF. [Costs of public hospitalization among elderly in Brazil’s Unified Health System] [in Portuguese]. Epidemiologia e Servicos de Saude. 2004;13:239–246.
Penrod JD, Litke A, Hawkes WG, Magaziner J, Doucette JT, Koval KJ, Silberzweig SB, Egol KA, Siu AL. The association of race, gender, and comorbidity with mortality and function after hip fracture. J Gerontol A Biol Sci Med Sci. 2008;63:867–872.
Pinheiro RS, Coeli CM, Vidal EI, Camargo KR Jr. [Mortality after hip fracture] [in Portuguese] Cadernos Saúde Coletiva, Rio de Janeiro. 2006;14:327–336.
Rae HC, Harris IA, McEvoy L, Todorova T. Delay to surgery and mortality after hip fracture. ANZ J Surg. 2007;77:889–891.
Rocha MA, Azer HW, Nascimento VG. [Functional evolution of proximal femoral end fractures] [in Portuguese]. Acta Ortop Brás. 2008;17:17–21.
Roche JJ, Wenn RT, Sahota O, Moran CG. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 2005;331:1374.
Sakaki MH, Oliveira AR, Coelho FF, Leme LEG, Suzuki I, Amatuzzi MM. [Study of the proximal femoral fractures mortality in elderly patients] [in Portuguese]. Acta Ortop Brás. 2004;12:242–249.
Shyu YI, Chen MC, Liang J, Wu CC, Su JY. Predictors of functional recovery for hip fractured elders during 12 months following hospital discharge: a prospective study on a Taiwanese sample. Osteoporos Int. 2004;15:475–482.
Smektala R, Endres HG, Dasch B, Maier C, Trampisch HJ, Bonnaire F, Pientka L. The effect of time-to-surgery on outcome in elderly patients with proximal femoral fractures. BMC Musculoskelet Disord. 2008;9:171.
Souza RC, Pinheiro RS, Coeli CM, Camargo KR Jr. [The Charlson comorbidity index (CCI) for adjustment of hip fracture mortality in the elderly: analysis of the importance of recording secondary diagnoses] [in Portuguese]. Cad Saúde Pública, Rio de Janeiro. 2008;24:315–322.
Souza RC, Pinheiro RS, Coeli CM, Camargo KR Jr, Torres TZ. [Risk adjustment measures for mortality after hip fracture] [in Portuguese]. Rev Saúde Pública. 2007;41:625–631.
Tosteson AN, Gottlieb DJ, Radley DC, Fisher ES, Melton LJ III. Excess mortality following hip fracture: the role of underlying health status. Osteoporos Int. 2007;18:1463–1472.
Veras RP. País Jovem com Cabelos Brancos [Young Country with White Hair]. Rio De Janeiro, Brazil: Relume Dumará; 1994.
Vestergaard P, Rejnmark L, Mosekilde L. Has mortality after a hip fracture increased? J Am Geriatr Soc. 2007;55:1720–1726.
Vestergaard P, Rejnmark L, Mosekilde L. Increased mortality in patients with a hip fracture-effect of pre-morbid conditions and post-fracture complications. Osteoporos Int. 2007;18:1583–1593.
Vidal EI, Coeli CM, Pinheiro RS, Camargo KR Jr. Mortality within 1 year after hip fracture surgical repair in the elderly according to postoperative period: a probabilistic record linkage study in Brazil. Osteoporos Int. 2006;17:1569–1576.
Vidal EI, Moreira-Filho DC, Coeli CM, Camargo KR Jr, Fukushima FB, Blais R. Hip fracture in the elderly: does counting time from fracture to surgery or from hospital admission to surgery matter when studying in-hospital mortality? Osteoporos Int. 2009;20:723–729.
Acknowledgments
We thank Rebecca Rupp for careful editing of the article. The design of the study and data collection were performed at the Federal University of Rio De Janeiro and the data analyses and preparation of the manuscript were performed at the Oswaldo Cruz Foundation and at the Solidage Research Group on Frailty and Aging, Montreal, Canada, when Dr. Pereira was a visiting fellow 2007–2008.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved or waived approval for the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
Mario A. Sayeg—Deceased.
About this article
Cite this article
Pereira, S.R.M., Puts, M.T.E., Portela, M.C. et al. The Impact of Prefracture and Hip Fracture Characteristics on Mortality in Older Persons in Brazil. Clin Orthop Relat Res 468, 1869–1883 (2010). https://doi.org/10.1007/s11999-009-1147-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-009-1147-5