Abstract
The optimal surgical treatment of displaced proximal humeral fractures is controversial. New implants providing angular stability have been introduced to maintain the intraoperative reduction. In a multi-institutional study, we prospectively enrolled and followed 152 patients with unilateral displaced and unstable proximal humeral fractures treated either with an antegrade angular and sliding stable proximal interlocking nail or an angular stable plate. Fractures were classified according to the Neer four-segment classification. Clinical, functional, and radiographic followups were performed 3, 6, and 12 months after surgery. Absolute and relative (to the contralateral shoulder) Constant-Murley scores were used to assess postoperative shoulder function. Using age, gender, and fracture type, we identified 76 pairs (152 patients) for a matched-pairs analysis. Relative Constant-Murley scores 12 months after treatment with an angular and sliding stable nail and after plate fixation were 81% and 77%, respectively. We observed no differences between the two groups. Stabilization of displaced proximal humeral fractures with either an angular stable intramedullary or an extramedullary implant seems suitable with both surgical treatment options.
Level of Evidence: Level III, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The variety of operative fixation techniques for displaced proximal humeral fractures described in the literature suggests the optimum surgical treatment for this fracture type has not yet been developed [1, 2, 8–10, 13, 15, 23, 30]. The goals of surgery are to obtain anatomic fracture reduction and stable primary fixation to ensure rapid fracture healing and immediate postoperative functional therapy without prolonged immobilization [9, 12, 21, 25]. Frequently applied methods to treat displaced proximal humeral fractures include minimally invasive techniques with Kirschner wires/sutures and/or screw fixation, plate fixation, intramedullary interlocking nailing, and hemiarthroplasty. The choice of surgical technique depends on the fracture type and the patient’s age, bone quality, and functional expectation [2, 12, 13, 22, 29, 33–36].
Two devices have been introduced to treat displaced proximal humeral fractures: an antegrade angular stable intramedullary nail [26, 32, 33] and an angular stable plate [13, 18, 22]. Both devices are intended to achieve maximum primary angular stability by three-dimensionally arranged interlocking screws at the humeral head level. However, implant-related complications such as impingement of the locking proximal humerus plate (LPHP) in as much as 3% of cases [22], cutout of angular stable screws in 7% to 20% of cases [12, 24], or rotator cuff tears after antegrade nailing (3%) [12] may badly influence the final functional outcome. Humeral head osteonecrosis, pseudarthrosis, secondary fracture displacement, and glenohumeral screw cutout, are known major risk factors for poor postoperative shoulder function [8, 9, 12]. It is unknown whether either of these two devices results in higher healing rates or lower complication rates or whether these various risk factors influence outcome with these devices.
We therefore raised the following questions: (1) Does the shoulder function determined by the relative Constant-Murley score differ depending on the choice of implant? (2) Is the angular stable intramedullary nail superior to plate fixation with differing fracture severity? (3) Does the operative strategy of humeral head fracture fixation influence the occurrence of minor and major complications? (4) Is the incidence of humeral head osteonecrosis, pseudarthrosis, secondary fracture displacement, and glenohumeral screw cutout, known major risk factors for poor postoperative shoulder function, higher in intramedullary nailing than in plate fixation?
Materials and Methods
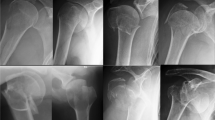
Three Level I trauma centers participated in the study. Between August 2001 and August 2004, 236 patients with fractures of the proximal humerus were seen. The decision for operative treatment was based on the presence of primary fracture displacement and subsequent instability using the criteria of Neer [26]: 45° humeral head angulation and 1-cm displacement of the proximal humeral head fragments (head, tubercles and shaft). We considered 5-mm displacement of the tubercles a sign of fracture instability and an indication for surgery [13, 17, 30]. Fracture type classification based on the radiographs of the shoulder in true anteroposterior (AP) and y-views initially was performed in each trauma center and retrospectively reviewed by the first author (GG) (senior registrar orthopaedic surgery, Rostock) to ensure a more consistent application of the Neer fracture classification [27]. We included patients with (1) displaced two-part and three-part fractures (Fig. 1), (2) four-part fractures (Fig. 2), and (3) dislocated four-part fractures of the humeral head. We excluded patients with fractures extending into the humeral shaft and patients with fractures extending in the articular surface (head split fractures); after these exclusions 203 patients were remaining. Of these, 91 were treated with a locking plate (Locking Proximal Humerus Plate; Mathys AG, Bettlach, Switzerland) and 112 with an antegrade angular and sliding stable interlocking nail (Targon® PH; B. Braun-Aesculap, Tuttlingen, Germany). In the LPHP group, two patients died from nonsurgery-related causes and eight patients had moved or did not respond for followup, leaving 81 available patients for matching. In the Targon® PH group, eight patients died from nonsurgery-related causes and 16 were lost to followup, contributing 88 patients for the matched-pairs analysis. Of these 169 patients, 152 (76 pairs, 24 males, 52 females) could be selected for a retrospective matched-pairs analysis according to age (± 2 years), gender, and fracture type with a minimum followup of 12 months (range, 12–14 months; mean ± standard deviation, 12.8 ± 0.4 months). Seventeen patients could not be included in the analysis owing to missing a corresponding matching partner. Based on the four-segment classification, the 152 patients (mean age, 63 ± 16 years) were grouped for analysis [27] as follows: 52 patients had two-part fractures, which were exclusively displaced surgical neck fractures; 60 had three-part fractures with head fragment and either displaced major or minor tubercle; 32 had four-part fractures, which were mainly laterally displaced with head, shaft, and both tubercles separated by fracture lines; and eight patients had four-part dislocation fractures in which there was total contact between the humeral head and glenoid.
For both surgical techniques, the patient was placed in the beach chair position on a radiolucent table fitted with a standard armrest. For implantation of the Targon® PH nail, we used a deltoid splitting approach with an incision averaging 4 cm (or extended as appropriate) at the anterolateral margin of the acromion. After a longitudinal transection of the clavipectoral fascia and the subacromial bursa, we achieved reduction of the head fragment by indirect manipulation of the head fragments using Kirschner wires, an elevator, or a Schanz screw for the joystick technique, and subsequently securing the fragments with Kirschner wires. After a longitudinal split of the supraspinatus tendon, we placed a guide pin at the apex of the humeral head in both planes and inserted the nail 3 to 4 mm below the cartilage level. Then, a minimum of three to four angular and sliding stable fixation screws were inserted into the head fragments, depending on the fracture pattern, degree of instability, and bone quality. We inserted single or duplicate distal interlocking of the nail via stab incisions, depending on individual bone quality. Each step of nail placement and locking screw insertion was controlled by fluoroscopy in true AP and axial views.
For the LPHP, we generally used a deltopectoral approach. The fracture fragments were directly and/or indirectly reduced with traction sutures, then temporarily fixed with Kirschner wires. When an acceptable reduction was obtained, the LPHP was placed against the lateral proximal humerus through the surgical incision under fluoroscopic control to avoid a too-proximal plate position provoking subacromial impingement. The proximal and distal locking screws were inserted, and the temporary fixation devices removed. In fractures with displaced and comminuted tuberosities or primary dislocation, a wider surgical incision and dissection of the fracture elements was necessary with both techniques to achieve adequate reduction. Finally, we also fixed fragments of comminuted tuberosities with tension banding using nonabsorbable sutures. The affected arm was placed in a sling after wound closure [11].
Postoperative passive physiotherapy without limitation of range of motion without wearing the sling began the first day after surgery. During hospitalization, the sling was taken off for supervised passive shoulder mobilization sessions lasting approximately 25 minutes per day. Shoulder immobilization (except during physiotherapy) did not extend beyond 14 days postsurgery. The protocol for outpatient physiotherapy scheduled 3 intervals of 10 sessions, each lasting 25 minutes per day. In addition, patients were trained particularly in self-assisted shoulder abduction and elevation with the uninjured arm guiding the arc of motion of the injured upper extremity. Loadbearing and resistive strengthening exercises were not allowed until at least 6 weeks after surgery after radiographs confirmed fracture union.
We performed functional and radiographic assessments 3, 6, and 12 months after surgery. Functional evaluation of the surgically treated shoulder was based on the Constant-Murley score [3]. In addition to the absolute Constant-Murley scores, the relative Constant-Murley score in percent of the contralateral, noninjured side was assessed, as patients had deteriorated shoulder function ranging from an absolute Constant-Murley score of 69 points to 100 points (mean: LPHP, 86 ± 9; Targon® PH, 93 ± 7).
All complications and their management were documented. Based on the consequences for the affected patient, they were divided into minor and major complications; major complications were defined as those leading to any sort of additional surgery.
We determined differences in relative Constant-Murley scores among the LPHP and the Targon® PH groups according to the Neer fracture types at the three followups using the Mann-Whitney U test. The exact Fisher tests were implemented to compare the complication and reoperation rates between the LPHP and the Targon® PH groups. Statistical analysis was performed using the SPSS® statistical software package (Version 12.0; SPSS Inc, Chicago, IL). Based on a post hoc power analysis, the statistical study power was calculated with G*power software. For the comparison between Neer fracture type subgroups, the effect size ranged from 0 to 2, and the statistical power ranged from 70% to 90%.
Results
The functional result after plate fixation was similar to that for intramedullary nailing, although we noted a trend toward better shoulder function shortly after surgery and 12 months postsurgery after intramedullary nailing. The relative Constant-Murley score did not exceed 75% after angular stable plating but reached 81% after intramedullary nailing (Table 1). The severity of the fracture pattern as determined by the Neer classification had no influence on the functional outcome in the LPHP group, whereas in the Targon® PH group, two-part and three-part fractures had better functional results than four-part fractures. Furthermore, there was a tendency toward better shoulder function in four-part fractures when treated with plate fixation, although these differences did not reach statistical significance (Table 1). Of interest, patients were not able to obtain a full Constant-Murley score on the contralateral uninjured shoulder, clearly showing movement limitations that may be traced back to degenerative changes of the glenohumeral joint.
The numbers of complications were similar (p = 0.458) in both groups: 22 complications in the LPHP group and 17 in the Targon® PH group (Table 2). Major complications requiring surgical revision occurred more often (p = 0.490) in the Targon® PH than in the LPHP group (13 versus nine). The higher number of additional operations did not affect the final functional result in a deleterious way. Glenohumeral cutout of angular stable fixation screws seemed to be one major disadvantage of both implants, whereas secondary fracture displacement was more frequent in the LPHP group.
Discussion
The major goal of surgical therapy in displaced proximal humeral fractures is to obtain anatomic fracture reduction, stable fixation, and early functional rehabilitation. Angular stable implants were considered to provide fixation stability and at the same time limit surgical exposure and thus enhance revascularization of fracture fragments and bony healing [13, 18, 19, 21, 31]. Angular stable implants are available for extramedullary and intramedullary fracture fixation, and until now it has been unclear whether plate fixation from an anterior (deltopectoral) approach or intramedullary nailing from a delta-split approach is superior in terms of fixation stability, maintenance of fracture reduction, and functional outcome. We prospectively evaluated the functional outcome and complication rates in patients with unilateral displaced and unstable proximal humeral fractures who underwent operative treatment with an antegrade angular and sliding stable proximal interlocking nail or an angular stable plate.
We studied patients with humeral head fractures in three Level I trauma centers. Specific fracture patterns, such as head split fractures or fractures extending in the humeral shaft, were excluded, thus reducing the number of patients. We believe articular fractures may not be appropriate for fixation owing to a high risk of osteonecrosis [8, 10, 30]. Although patients were evaluated prospectively, differences between groups were analyzed retrospectively using a matched-pairs analysis, which is one major limitation of the study design. A prospective randomized trial may have determined differences between groups to a higher level of evidence [28]. Another disadvantage of the study is the reduction of the sample size from 236 patients initially to 152 patients who could be matched successfully according to the study design. Finally, the short followup may have limited the functional result of the shoulder, especially when the occurrence of complications prolonged the functional recovery. Thus, Constant-Murley scores may have been underestimated; however, they are still in line with those in other studies with equivalent or longer followup times [2, 9, 14, 18].
Relative Constant-Murley scores after plate fixation did not substantially exceed 75% in the last followup 12 months postsurgery. Also, there was no difference in the functional results according to the severity of the fracture pattern. Reported functional results after LPHP plate fixation range between 74% and 89%, equal to or marginally better than our results (Table 3). Whereas we observed no important functional differences between the Neer fracture types, Björkenheim et al. [2] reported better functional outcome in two- and three-part fractures than in four-part fractures using the Philos® plate (Synthes, Paoli, PA) fixation. Studies of antegrade angular stable nailing of proximal humerus fractures are infrequent and have not included a large number of patients. The mean relative Constant-Murley score of 80% in our study is similar to the 84% reported by Mathews and Lobenhoffer [24]. In four-part fractures we found the mean relative Constant-Murley score was 10% less than in two- and three-part fractures; however, Mathews and Lobenhoffer [24] described an inverse trend with four-part fractures having the best functional outcome among the Neer fracture types. In another study, Adedapo and Ikpeme [1] described a substantially lower Neer score during a 1-year followup period and continuous impairment in four-part fractures compared with three-part fractures treated with a Polarus® nail (Acumed, Inc, Beaverton, OR) (Table 3). There is one nonrandomized comparative study of plate fixation using the Philos® plate and antegrade nailing (Targon® PH) for proximal humeral fractures by Krivohlavek et al. [20]. They also reported no difference in the functional outcome between both surgical techniques; however, four-part fractures treated with antegrade nailing had lower functional shoulder scores [20].
In the surgical treatment of displaced proximal humeral fractures, the occurrence of osteonecrosis, pseudarthrosis/nonunion, secondary fracture displacement, and implant cutout reportedly have a negative impact on functional outcome [7, 9, 13, 30]. In our study, all fractures united. In a recent study, Dimakopoulos et al. [4] reported a nonunion rate of just 1% (two of 165 patients followed), which may show stable fracture fixation is possible using angular stable implants. We did not find complete or partial humeral head osteonecrosis frequently. In published studies, for 12 to 15 months’ followup for LPHP fixation, osteonecrosis was reported to occur in 0% to 5% of the patients [2, 14, 19]. For short-term followup after intramedullary nailing, osteonecrosis rarely was described [16, 24, 32]. The radiographic incidence of osteonecrosis of the humeral head in displaced proximal humeral fractures using standard nonangular stable implants for intermediate- and long-term followups reportedly is between 7% and 25% [2, 4, 6, 8, 22, 35]. The higher incidence may be attributable to the longer followup. One major disadvantage of both surgical techniques is the occurrence of glenohumeral cutout of angular stable fixation screws in as much as 13% (Targon® PH) and 7.8 % (LPHP). Egol et al. [5] found glenohumeral cutout after angular stable plate fixation in 16% of patients, whereas only ½ of these patients had revision surgery. The high rate of screw penetration may be attributable to fracture setting in the case of poor bone stock, according to the authors [5]. Mittlmeier et al. [25] suggested, in the case of antegrade nailing, not to overdrill the medial cartilage and select fixation screws 2 to 3 mm shorter than estimated. Furthermore, we found fracture setting without implant failure exclusively in the LPHP group, suggesting the maintenance of initial fracture reduction is more effective using a central load carrier. Although clinical data could not confirm this presumption, biomechanical data revealed a higher axial and bending stiffness of humeral nails when compared with plate fixation in experimental humeral fractures [16].
We found no differences in the functional outcome of humeral head fracture treatment using either an angular stable plate (LPHP) or an angular stable antegrade nail (Targon® PH). Although there is a trend toward better shoulder function of two- and three-part fractures treated with antegrade nailing, a certain treatment strategy could not be recommended. The overall complication rate is comparable in both groups, whereas secondary fracture displacement without implant failure and consecutive malunion were seen exclusively in patients after plate fixation. Glenohumeral cutout of angular stable fixation screws and humeral head osteonecrosis most frequently determined revision surgery and thus remain unsolved problems in angular stable fixation of humeral head fractures.
References
Adedapo AO, Ikpeme JO. The results of internal fixation of three- and four-part proximal humeral fractures with the Polarus nail. Injury. 2001;32:115–121.
Bjorkenheim JM, Pajarinen J, Savolainen V. Internal fixation of proximal humeral fractures with a locking compression plate: a retrospective evaluation of 72 patients followed for a minimum of 1 year. Acta Orthop Scand. 2004;75:741–745.
Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164.
Dimakopoulos P, Panagopoulos A, Kasimatis G. Transosseous suture fixation of proximal humeral fractures. J Bone Joint Surg Am. 2009;91:8–21.
Egol KA, Ong CC, Walsh M, Jazrawi LM, Tejwani NC, Zuckerman JD. Early complications in proximal humerus fractures (OTA Types 11) treated with locked plates. J Orthop Trauma. 2008;22:159–164.
Fankhauser F, Boldin C, Schippinger G, Haunschmid C, Szyszkowitz R A new locking plate for unstable fractures of the proximal humerus. Clin Orthop Relat Res. 2005;430:176–181.
Gardner MJ, Griffith MH, Dines JS, Lorich D. A minimally invasive approach for plate fixation of the proximal humerus. Bull Hosp Jt Dis. 2004;62:18–23.
Gerber C, Hersche O, Berberat C. The clinical relevance of posttraumatic avascular necrosis of the humeral head. J Shoulder Elbow Surg. 1998;7:586–590.
Gerber C, Werner CM, Vienne P. Internal fixation of complex fractures of the proximal humerus. J Bone Joint Surg Br. 2004;86:848–845.
Gierer P, Simon C, Gradl G, Ewert A, Vasarhelyi A, Beck M, Mittlmeier T. [Complex proximal humerus fractures: management with a humeral head prosthesis?] [in German]. Orthopäde. 2006;35:834–840.
Gilchrist DK. A Stockinette-Vaelpeau for immobilization of the shoulder girdle. J Bone Joint Surg Am. 1967;49:750–751.
Gradl G, Dietze A, Arndt D, Beck M, Gierer P, Börsch T, Mittlmeier T. Angular and sliding stable antegrade nailing (Targon PH) for the treatment of proximal humeral fractures. Arch Orthop Trauma Surg. 2007;127:937–944.
Habermeyer P. [Fracture of the head of the humerus] [in German]. Unfallchirurg. 1997;100:820–837.
Hessler C, Schmucker U, Matthes G, Ekkernkamp A, Gütschow R, Eggers C. [Results after treatment of instable fractures of the proximal humerus using a fixed-angle plate] [in German]. Unfallchirurg. 2006;109:867–874.
Hessmann MH, Blum J, Hofmann A, Küchle R, Rommens PM. Internal fixation of proximal humeral fractures: current concepts. Eur J Trauma. 2003;29:253–261.
Hessmann MH, Hansen WS, Krummenauer F, Rommens PM. Locked plate fixation and intramedullary nailing for proximal humerus fractures: a biomechanical evaluation. J Trauma. 2005;58:1194–1201.
Hintermann B, Trouillier HH, Schäfer D. Rigid internal fixation of fractures of the proximal humerus in older patients. J Bone Joint Surg Br. 2000;82:1107–1112.
Kettler M, Biberthaler P, Braunstein V, Zeiler C, Kroetz M, Mutschler W. [Treatment of proximal humeral fractures with the PHILOS angular stable plate: presentation of 225 cases of dislocated fractures] [in German]. Unfallchirurg. 2006;109:1032–1040.
Kollig E, Kutscha-Lissberg F, Roetman B, Mielke E, Muhr G, Hahn MP. [Primary hemiarthroplasty after complex fracture of the humeral head: functional late results] [in German]. Zentralbl Chir. 2003;128:125–130.
Krivohlavek M, Lukas R, Taller S, Sram J. [Use of angle-stable implants for proximal humeral fractures: prospective study] [in Czech]. Acta Chir Orthop Traumatol Cech. 2008;75:212–220.
Lill H, Hepp P, Korner J, Kassi JP, Verheyden AP, Josten C, Duda GN. Proximal humeral fractures: how stiff should an implant be? A comparative mechanical study with new implants in human specimens. Arch Orthop Trauma Surg. 2003;123:74–81.
Lill H, Hepp P, Rose T, König K, Josten C. [The angle stable locking-proximal-humerus-plate (LPHP) for proximal humeral fractures using a small anterior-lateral-deltoid-splitting-approach: technique and first results] [in German]. Zentralbl Chir. 2004;129:43–48.
Lill H, Josten C. [Conservative or operative treatment of humeral head fractures in the elderly?] [in German]. Chirurg. 2001;72:1224–1234.
Mathews J, Lobenhoffer P. [The Targon® PH Nail as an internal fixator for unstable fractures of the proximal humerus] [in German]. Oper Orthop Traumatol. 2007;19:255–275.
Mittlmeier TW, Stedtfeld HW, Ewert A, Beck M, Frosch B, Gradl G. Stabilization of proximal humeral fractures with an angular and sliding stable antegrade locking nail (Targon-PH). J Bone Joint Surg Am. 2003;85(suppl 2):136–146.
Neer CS. Displaced proximal humeral fractures. II. Treatment of three part and four part displacement. J Bone Joint Surg Am. 1970;52:1090–1103.
Neer CS. Four-segment classification of proximal humeral fractures. J Shoulder Elbow Surg. 2002;11:389–400.
Phillips B, Ball C, Sackett D, Badenoch D, Straus D, Haynes B, Dawes. Levels of evidence and grades of recommendation. Oxford, UK: Oxford-Centre for Evidence Based Medicine; 2001. Available at: http://www.cebm.net/levels_of_evidence.asp. Accessed February 13, 2009.
Resch H. [Fractures of the humeral head] [in German]. Unfallchirurg. 2003;106:602–617.
Resch H, Povacz P, Fröhlich R, Wambacher M. Percutaneous fixation of three- and four-part fractures of the proximal humerus. J Bone Joint Surg Br. 1997;79:295–300.
Sonderegger J, Simmen HP. [Epidemiology treatment and results of proximal humeral fractures: experience of a district hospital in a sports- and tourism area] [in German]. Zentralbl Chir. 2003;128:119-124.
Stedtfeld HW, Attmanspacher W, Thaler K, Frosch B. [Fixation of humeral head fractures with antegrade intramedullary nailing] [in German]. Zentralbl Chir. 2003;128:6–11.
Stedtfeld HW, Mittlmeier T. Fixation of proximal humeral fractures with an intramedullary nail: tips and tricks. Eur J Trauma Emerg Surg. 2007;4:367–374.
Tamai K, Ohno W, Takemura M, Mashitori H, Hamada J, Saotome K. Treatment of proximal humeral fractures with an intramedullary nail. J Orthop Sci. 2005;10:180–186.
Wijgman AJ, Roolker W, Patt T, Raaymakers E, Marti R. Open reduction internal fixation of three and four part fractures of the proximal part of the humerus. J Bone Joint Surg Am. 2002;84:1919–1925.
Zyto K, Kronberg M, Brostrom LA. Shoulder function after displaced fractures of the proximal humerus. J Shoulder Elbow Surg. 1995;4:331–336.
Acknowledgments
We thank Helga Krentz, Institute of Biostatistics, University of Rostock, for assistance in the statistical data analysis.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was performed at University of Rostock and the Campus Virchow and Campus Benjamin Franklin of Humboldt University.
About this article
Cite this article
Gradl, G., Dietze, A., Kääb, M. et al. Is Locking Nailing of Humeral Head Fractures Superior to Locking Plate Fixation?. Clin Orthop Relat Res 467, 2986–2993 (2009). https://doi.org/10.1007/s11999-009-0916-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-009-0916-5