Abstract
Purpose
To assess longer-term (> 5 years) function and outcome in patients treated with anatomic locking plates for proximal humerus fractures.
Methods
This retrospective cohort study was conducted at an urban, academic level 1 trauma center and an orthopedic specialty hospital. Patients treated operatively for proximal humerus fractures with an anatomic locking plate by three orthopedic trauma surgeons and two shoulder surgeons from 2003 to 2015 were reviewed. Patient demographics and injury characteristics, disabilities of the arm, shoulder, and hand (DASH) scores, complications, secondary surgeries, and shoulder range of motion were compared at 1 year and at latest follow-up.
Results
Seventy-five of 173 fractures were eligible for analysis. At a minimum 5 years and a mean of 10.0 ± 3.2 years following surgery, DASH scores did not differ from one-year compared to long-term follow-up (16.3 ± 17.4 vs. 15.1 ± 18.2, p = 0.555). Shoulder motion including: active forward flexion (145.5 vs. 151.5 degrees, p = 0.186), internal rotation (T10 vs. T9, p = 0.204), and external rotation measurements (48.4 vs. 57.9, p = 0.074) also did not differ from one year compared to long-term follow-up. By one year, all fractures had healed. After 1-year post-operatively, four patients underwent reoperation, but none for AVN or screw penetration.
Conclusions
Patient-reported functional outcome scores and shoulder range of motion are stable after one year following proximal humerus fracture fixation, and outcomes do not deteriorate thereafter. After one-year, long-term follow-up of fixed proximal humerus fractures may be unnecessary for those without symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Proximal humerus fractures comprise 5% of all diagnosed fractures and present in a bimodal distribution. Commonly associated with osteoporosis, they are the third most frequent fracture in the elderly [1, 2], and their incidence is expected to increase as the elderly population grows, with one estimate predicting a 50% increase from 2008 to 2030 [3]. Younger patients also sustain proximal humerus fractures as a result of high-energy trauma, and these injuries constitute the seventh most frequent fractures in adults overall [4]. Proximal humerus fractures can have significant impact on patients’ function and quality of life—they have been demonstrated to be associated with severe difficulties with personal hygiene, cause chronic pain, difficulty sleeping, and be a source of symptoms of depression and anxiety [2, 5].
Most proximal humerus fractures can be treated non-operatively, but some, especially significantly displaced fractures, require surgery. It has been reported that up to 25% of all proximal humerus fractures are treated surgically [6]. Surgical treatment options include: repair with plate fixation, intramedullary nail fixation, or percutaneous pinning, and arthroplasty in the form of hemi-arthroplasty or reverse total shoulder replacement. Currently, plate fixation is considered the gold standard for surgical management of significantly displaced fractures in the young and active elderly [7, 8].
There are, however, complications associated with plate and screw fixation repair, including: nonunion, implant failure/migration (i.e., screw penetration), osteonecrosis, infection, posttraumatic osteoarthritis, and post-operative shoulder stiffness. Reoperation may be required to remove implants due to failure, impingement/stiffness, pain and discomfort, or infection. Complication rates of 38–44% have been reported in the elderly in some studies, with reoperation rates of 11–12% [9, 10]. Patients typically follow-up in the outpatient setting for one year after surgery to monitor for healing complications; however, some have suggested that further follow-up is warranted [10, 11].
The recent advent of the reverse total shoulder replacement (rTSA) for the treatment of select proximal humerus fractures has given rise to an increase treatment with that implant. Knowledge of how repaired proximal humerus fractures fare over time may provide evidence one way or another as to the viability of one treatment strategy over another. Given the increasing burden that proximal humerus fractures are expected to impose on the healthcare system and their impact on patients’ function and quality of life, it is important to determine whether current practices constitute optimal management. The purpose of this study was to assess for longer-term outcomes following proximal humerus fracture repair by comparing outcomes at one- and minimum 5-year follow-up following locking plate and screw fixation of proximal humerus fractures. The authors of this study hypothesized that outcomes following proximal humerus fracture repair at 5-year post-op would be similar to outcomes at 1-year follow-up.
Methods
Between 2003 and 2020, 262 patients who were treated by three trauma and two shoulder fellowship trained orthopedic surgeons for a displaced proximal humerus fractures with locking plates were enrolled into an IRB-approved database at time of initial treatment. These patients were all managed in a similar manner, with all treating surgeons using a similar protocol in their clinical decision making. Fracture repair was generally indicated based on the degree of fracture displacement in concert with a determination of patient functional level and expectations. While no absolutes existed surgery was performed in cases that were determined to be significantly displaced, unstable, or had patterns associated with a higher risk of osteonecrosis, all fractures were classified according to the Neer system. All surgery was performed open via a deltopectoral approach with direct reduction and application of an anterolateral proximal humerus locking plate (Synthes, Paoli, Pa, Exactech, Gainsville, Fla and Stryker, Mahwah, NJ).
Inclusion criteria for this study was any patient in this prospective database who were at least 18 years of age at time of injury and were at a minimum five years out from index surgical treatment. Patients were excluded from analysis if fewer than five years elapsed since initial operation or if they were deceased prior to five-year follow-up or at time of contact.
Data collected at time of enrollment included patient demographics, such as age, sex, race, BMI, age unadjusted Charlson comorbidity index (CCI), tobacco usage, alcohol consumption, illicit drug use, and worker’s compensation status. Injury and surgical information were also collected including accident type, Neer and OTA classifications, anesthesia type, plate manufacturer, number of screws, and intra-operative complications. Accident type was characterized as a high-energy or low-energy mechanism of injury. Low-energy mechanism are defined as mechanical falls or falls equal or less than the equivalent of two steps. High-energy mechanisms are defined as falls greater than two steps, pedestrians struck, or motor vehicle collisions.
Patient follow-up information and functional score data were collected at 3 months, 6 months, 12 months, and annually thereafter as needed. Outcome measures collected included the disabilities of arm, shoulder, and hand (DASH) scores, shoulder range of motion of the affected side, fracture healing, and any complications such as screw penetration, infection, malunion and nonunion, avascular necrosis (AVN) of the humeral head, and any additional orthopedic reoperation such as removal of implant or conversion to total shoulder.
When possible, the operating physician evaluated patients in person or via video telehealth, but in instances where this was not feasible, trained research personnel collected DASH scores via phone interview and obtained information related to any surgical intervention after last in person follow-up. Outcomes were compared between data collected at one year and at latest follow-up using paired t-tests. Chi-squared analysis and analysis of variance (ANOVA) were used for comparison of the 75 long-term follow-up patients and the 98 lost to follow-up patients. All analysis was conducted using IBM SPSS version 25.0 software.
Results
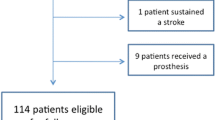
A total of 173 patients who underwent operative repair of a proximal humerus fracture with locking plate and screws who were a minimum of 5 years from index surgery and had been seen at one-year follow0up were eligible for analysis; however, ninety-eight patients (57%) did not have adequate follow-up data beyond 1-year post-operatively. Therefore, seventy-five patients (43%) with a mean 10.0 ± 3.2 years follow-up (range 5.0–16.8 years) met criteria for long-term data analysis. Radiographic data were available for all 75 patients to investigate new onset AVN, screw penetration, and radiographic evidence of reoperation after 5 years from index surgery. The demographic profile between the long-term and lost to follow-up cohorts was similar except that the longer-term follow-up group had a greater BMI. This comparison is detailed in Table 1.
Forty-five patients had surgery under regional anesthesia (60%) and the Neer classification of the long-term follow-up cohort, as classified by the operating surgeon, was: 2-part (22.7%), 3-part (61.3%), and 4-part (16.0%) (Table 2). Patient reported functional outcome scores between the one-year and long-term follow-up did not differ (DASH: 16.3 ± 17.4 vs. 15.1 ± 18.2, p = 0.555). Long-term shoulder range-of-motion data were only available for 31 patients (41.3%), who were seen in person (22 patients) or via video telehealth (9 patients). There was no difference in mean active shoulder forward flexion at 1 year compared to long-term follow-up (145.5 ± 32.4 degrees vs. 151.5 ± 39.1 degrees, p = 0.186). There was a trend toward improvement in mean active shoulder external rotation at long-term follow-up (57.9 ± 23.5) compared to 1 year (48.4 ± 16.6 degrees, p = 0.074). There was no further improvement in internal rotation between one-year and long-term follow-up (T10 vs. T9 vertebrae, p = 0.204) (Table 3).
Of the 173 patients, 18 patients (10.4%) experienced 26 complications within 1 year of initial fracture fixation. Of these, nine patients underwent 13 reoperations (5.2%). Complications included: eleven screw penetrations (6.4%), seven AVN (4.0%), three infections (1.7%), three malunions of the greater tuberosity (1.7%), and two fracture nonunions (1.2%). No patients experienced further complications related to the index surgery after 1 year. No patients reported developing AVN or infection that required any intervention following healing.
There were four patients (5.3%) underwent further shoulder surgery after 1 year, 2 of which were not related to the index injury. One patient underwent removal of implant and soft-tissue mass excision at 5 years following development of an unrelated benign neoplasm. One patient underwent removal of implant 2 years after initial fixation as part of a procedure that included a capsular release to improve motion. The same patient had an unrelated fall down stairs that resulted in a shoulder dislocation with a Bankart lesion and labral tear. She then required a Latarjet procedure 6 years after initial fracture fixation to correct recurrent shoulder instability that resulted from that event. A third patient underwent implant removal and rotator cuff repair 6 years post-operatively resulting from a second fall and dislocation. The fourth patient underwent implant removal 3 years post-operatively for painful hardware without further complication.
Discussion
Our study found that once healed, patients treated for a proximal humerus fracture with a locked plate construct have very good outcomes at one year with regard to function and these results do not decay with time. At a mean 10.0 years post-operative, these patients have a similar DASH scores and shoulder ROM as they did one year after fracture repair. When compared to the 98 patients without long-term follow-up, only BMI differed, indicating the long-term results are most likely generalizable to the entire cohort, as age has been shown to be the predominate contributing factor to differing outcomes [9, 10, 12].
The primary outcome measured in this study was patient reported functional outcomes as measured by DASH scores. The DASH is a questionnaire that comprises 30 questions with answer options ranging from 1 to 5. The total of these scores are calculated on a scale ranging from 0 to 100, with 0 being no impairment and 100 being the most severe impairment. Scores under 29 have been reported as no longer a major hindrance to everyday functioning, where a majority of patients report that they can return to work, can discontinue physical therapy, and are aware of their physical limitations but they are not a problem [13]. Further score delineation has shown that DASH scores < 15 = “no problem,” 16–40 = “problem, but working,” and > 40 = “unable to work” [14]. According to these parameters, the 15-point mean long-term DASH score in our cohort demonstrates all patients had positive long-term outcomes [15,16,17].
As the patient recovers from surgery, the DASH scores should decrease. These score changes can vary in clinical importance, with some studies showing a 10-point difference as a minimal important change in functioning, a 15-point difference as having their problem improved, and over 20-point difference as functionally improved [18, 19]. In our cohort, the 1-year DASH scores only differed by an average of 1-point comparative to their 5-year DASH scores, indicating no important change in functioning over the years. Thus, they were at their optimal functioning at one year and plateaued, without further functional decline over the years.
Overall, our long-term DASH scores are in concordance with pre-existing literature assessing long-term patient-reported outcomes for operatively treated proximal humerus fractures with compression locking plates. Hirschman et al. displayed an average DASH score of 15.3 ± 17.7 in a cohort with median 5-year post-injury follow-up [20]. Bahrs et al. demonstrated a mean DASH score of 12 points in their cohort of patients with a mean follow-up of 96 months [21]. Ockert et al. had a mean 10-year follow-up and demonstrated a higher, but still within functional limits, mean DASH score of 23.8 [22]. In addition to similar DASH scores, Hirschmen et al. also displayed similar physical examination outcomes and reoperation rates to our study, with a long-term average of 133 degrees forward flexion, and only two reoperations after 1 year from index surgery [20].
The low long-term complication rates in this study are similar to Robinson et al. who revealed a fixation failure and nonunion rate of 4.3% and 10-year reoperation rate of 10% [23]. However, Erasmo et al. and Greiner et al. state further than 1-year follow-up may be necessary due to complications that arise, particularly AVN and varus displacement, as found in those studies [11, 24]. In addition, after 1 year from initial fixation, Barlow et al. found 25 patients (19%) with failures; defined as screw backout/fracture, plate fracture, AVN, arthritis, nonunion, rotator cuff failure, and screw penetration [10]. Similarly, Ye et al. demonstrated a 20% complication rate (complications included subacromial impingements, screw cut-outs, malunions, tuberosity resorptions, AVN of the humeral head, and screw breakage) greater than 1-year following initial fixation [25]. Our long-term complication results are in contrast to these papers. While the 1-year complication rate was 10.4%, all of our patients healed by 1 year and thus would make it unlikely to see any healing complications following this point.
The current study had only four patients (5.3%) undergo further surgery after 1-year post-operatively each of which included removal of implants. Three of the four were related to other disease or injury processes and thus did not demonstrate any long-term complications related to index surgery for the entire cohort. Perhaps the discrepancy in the literature to our current study exists in the differing measures obtained for complication rates and lack of a detailed timeframes for when each complication took place. This study did not assess long-term arthritis, impingements, or rotator cuff failure as Ye et al. and Barlow et al.; therefore, a direct comparison of complication rates cannot be made. After 1 year post-operatively, Hirschmen et al. reported a 3.5% reoperation rate but did not detail other complication rates past 1 year [20]. Erasmo et al. displayed an AVN rate of 7.3% after 1 year but did not mention how many patients underwent reoperation after 1 year [11]. Similarly, Greiner et al. demonstrated an AVN rate of 10.4% after 1 year without detailing reoperation rates after 1 year post-operatively [24]. Higher-level studies on outcomes following proximal humerus fracture fixation are warranted to more clearly ascertain the long-term efficacy and safety of this operation.
This study is not without limitations. A majority of the patient reported outcome scores were collected via telephone interview, limiting physical examination and radiographic data, and created a reliance on some patients reporting reoperation and complication information. Additionally, less than half of the viable patient population for the study were included and although the lost to follow-up cohort was similar to the long-term follow-up cohort with respect to demographics, the possibility remains that the analyzed cohort has the potential to inaccurately represent the operative population as a whole.
Conclusion
Patient reported functional outcome scores and shoulder range of motion both plateau after one year following proximal humerus fracture fixation, and outcomes do not deteriorate at a minimum 5 years and mean 10 years. After one-year, long-term follow-up of fixed proximal humerus fractures may be unnecessary for those without symptoms. These results allow the treating physician to confidently provide patients with reasonable expectations for the longer term regarding their results following operative repair.
References
Passaretti D, Candela V, Sessa P, Gumina S (2017) Epidemiology of proximal humeral fractures: a detailed survey of 711 patients in a metropolitan area. J Shoulder Elbow Surg 26(12):2117–2124. https://doi.org/10.1016/j.jse.2017.05.029
Calvo E, Morcillo D, Foruria AM et al (2011) Nondisplaced proximal humeral fractures: high incidence among outpatient-treated osteoporotic fractures and severe impact on upper extremity function and patient subjective health perception. J Shoulder Elbow Surg. 20(5):795–801. https://doi.org/10.1016/j.jse.2010.09.008
Kim SH, Szabo RM, Marder RA (2012) Epidemiology of humerus fractures in the United States: nationwide emergency department sample, 2008. Arthritis Care Res (Hoboken). 64(3):407–414. https://doi.org/10.1002/acr.21563
Court-Brown CM, Caesar B (2006) Epidemiology of adult fractures: a review. Injury. 37(8):691–697. https://doi.org/10.1016/j.injury.2006.04.130
Sabharwal S, Archer S, Cadoux-Hudson D, Griffiths D, Gupte CM, Reilly P (2019) Exploring elderly patients’ experiences of recovery following complex proximal humerus fracture: a qualitative study. J Health Psychol. 26(6):880–889. https://doi.org/10.1177/1359105319850883
Jawa A, Burnikel D (2016) Treatment of proximal humeral fractures: a critical analysis review. JBJS Rev. https://doi.org/10.2106/JBJS.RVW.O.00003
Kancherla VK, Singh A, Anakwenze OA (2017) Management of acute proximal humeral fractures. J Am Acad Orthop Surg. 25(1):42–52. https://doi.org/10.5435/JAAOS-D-15-00240
Gonzalez-Hernandez E, Pietrzak WS, Jain S, Lapica HE (2020) Cross-elements to enhance fixation in osteoporotic bone with application to proximal humeral locking plates: a biomechanical study. J Shoulder Elbow Surg. 29(8):1606–1614. https://doi.org/10.1016/j.jse.2019.12.017
Klug A, Wincheringer D, Harth J, Schmidt-Horlohé K, Hoffmann R, Gramlich Y (2019) Complications after surgical treatment of proximal humerus fractures in the elderly-an analysis of complication patterns and risk factors for reverse shoulder arthroplasty and angular-stable plating. J Shoulder Elbow Surg. 28(9):1674–1684. https://doi.org/10.1016/j.jse.2019.02.017
Barlow JD, Logli AL, Steinmann SP et al (2020) Locking plate fixation of proximal humerus fractures in patients older than 60 years continues to be associated with a high complication rate. J Shoulder Elbow Surg. 29(8):1689–1694. https://doi.org/10.1016/j.jse.2019.11.026
Erasmo R, Guerra G, Guerra L (2014) Fractures and fracture-dislocations of the proximal humerus: a retrospective analysis of 82 cases treated with the Philos(®) locking plate. Injury. 45(Suppl 6):S43–S48. https://doi.org/10.1016/j.injury.2014.10.022
Goch AM, Christiano A, Konda SR, Leucht P, Egol KA (2017) Operative repair of proximal humerus fractures in septuagenarians and octogenarians: does chronologic age matter? J Clin Orthop Trauma. 8(1):50–53. https://doi.org/10.1016/j.jcot.2017.01.006
Disabilities of the Arm, Shoulder and Hand (DASH) Users Viewpoint Clarifies Interpretability of Scores. Dorcas E. Beaton, PhD; 2Carol A. Kennedy, BScPT, MSc
Kennedy CA, Beaton DE, Solway S, McConnell S, Bombardier C (2011) The DASH outcome measure user’s manual, 3rd edn. Institute for Work & Health, Toronto
Broder K, Christiano A, Zuckerman JD, Egol K (2013) Management of proximal humerus fractures with the equinoxe® locking plate system. Bull Hosp Jt Dis 2015(73 Suppl 1):S107–S110
Fisher ND, Barger JM, Driesman AS, Belayneh R, Konda SR, Egol KA (2017) Fracture severity based on classification does not predict outcome following proximal humerus fracture. Orthopedics. 40(6):368–374. https://doi.org/10.3928/01477447-20170925-04
Ong CC, Kwon YW, Walsh M, Davidovitch R, Zuckerman JD, Egol KA (2012) Outcomes of open reduction and internal fixation of proximal humerus fractures managed with locking plates. Am J Orthop (Belle Mead NJ) 41(9):407–412
Gummesson C, Atroshi I, Kkdahl C (2003) The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire – longitudinal construct validity and measuring self =-rated health change after surgery. BMC Musculoskel Dis 4:11. https://doi.org/10.1186/1471-2474-4-11
Beaton DE, Katz JN, Fossel AH, Wright JG, Tarasuk V, Bombardier C (2001) Measuring the whole or the parts? validity, reliability, and responsiveness of the disabilities of the arm, shoulder and hand outcome measure in different regions of the upper extremity. J Hand Ther 14:128–146
Hirschmann MT, Fallegger B, Amsler F, Regazzoni P, Gross T (2011) Clinical longer-term results after internal fixation of proximal humerus fractures with a locking compression plate (PHILOS). J Orthop Trauma. 25(5):286–293. https://doi.org/10.1097/BOT.0b013e3181f2b20e
Bahrs C, Kühle L, Blumenstock G, Stöckle U, Rolauffs B, Freude T (2015) Which parameters affect medium- to long-term results after angular stable plate fixation for proximal humeral fractures? J Shoulder Elbow Surg. 24(5):727–732. https://doi.org/10.1016/j.jse.2014.08.009
Ockert B, Siebenbürger G, Kettler M, Braunstein V, Mutschler W (2014) Long-term functional outcomes (median 10 years) after locked plating for displaced fractures of the proximal humerus. J Shoulder Elbow Surg. 23(8):1223–1231. https://doi.org/10.1016/j.jse.2013.11.009
Robinson CM, Stirling PHC, Goudie EB, MacDonald DJ, Strelzow JA (2019) Complications and long-term outcomes of open reduction and plate fixation of proximal humeral fractures. J Bone Joint Surg Am. 101(23):2129–2139. https://doi.org/10.2106/JBJS.19.00595
Greiner S, Ka¨a¨b MJ, Haas NP, Bail HJ (2009) Humeral head necrosis rate at mid-term follow-up after open reduction and angular stable plate fixation for proximal humeral fractures. Injury 40(2):186–91
Ye T, Wang L, Zhuang C, Wang Y, Zhang W, Qiu S (2013) Functional outcomes following locking plate fixation of complex proximal humeral fractures. Orthopedics. 36(6):e715–e722. https://doi.org/10.3928/01477447-20130523-14
Funding
No sources of funding have been granted for this study.
Author information
Authors and Affiliations
Contributions
Authorship has been granted only to those individuals who have contributed substantially to the research or manuscript. Material preparation, data collection, and analysis were performed by Rachel Ranson, Rachel Roller, Connor Littlefield, and Nicket Dedhia. The first draft of the manuscript was written by Rachel Ranson, Kenneth Egol, and Sanjit Konda and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest related to the contents of this manuscript.
Consent to participate
Informed written consent was obtained by all patients in this study.
Data availability
The data that support the findings of this study are available on request from the corresponding author, RR. The data are not publicly available due to their containing information that could compromise the privacy of research participants.
Code availability
The coding data that support the findings of this study are available on request from the corresponding author, RR. The data are not publicly available due to their containing information that could compromise the privacy of research participants.
Ethical approval
This study was approved by the NYU School of Medicine Institutional Review Board (Study Number: 05–201).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ranson, R., Roller, R., Dedhia, N. et al. No change in outcome ten years following locking plate repair of displaced proximal humerus fractures. Eur J Orthop Surg Traumatol 32, 1195–1200 (2022). https://doi.org/10.1007/s00590-021-03099-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-021-03099-6