Abstract
Fragility fractures are generally associated with substantial loss in trabecular bone mass and alterations in structural anisotropy. Despite the high correlations between measures of trabecular mass and mechanical properties, significant overlap in density measures exists between individuals with osteoporosis and those who do not fracture. The purpose of this paper is to provide an analysis of trabecular properties associated with fragility fractures. While accurate measures of bone mass and 3-D orientation have been demonstrated to explain 80% to 90% of the variance in mechanical behavior, clinical and experimental experience suggests the unexplained proportion of variance may be a key determinant in separating high- and low-risk patients. Using a hierarchical perspective, we demonstrate the potential contributions of structural and tissue morphology, material properties, and chemical composition to the apparent mechanical properties of trabecular bone. The results suggest that the propensity for an individual to remodel or adapt to habitual damaging or nondamaging loads may distinguish them in terms of risk for failure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is characterized by compromised bone integrity [46], increased vulnerability to fractures that impair a person’s quality of life [48, 64], and increased mortality [6, 30] and, as such, constitutes an enormous physical and economic burden in the aging population. The primary objective of osteoporosis treatment, to prevent fractures, is dependent on accurate and effective methods for characterizing bone integrity and the associated fracture risk in an individual. Early detection of a loss in bone integrity would enable the implementation of treatment regimens that may substantially improve outcomes and prevent the morbidity and costs that follow the advent of a fracture. Early diagnosis may also be important since the effectiveness of treatment diminishes with disease progression. Currently, patients are rarely symptomatic before considerable bone loss has occurred and in some cases not until after they have suffered their first fracture [13, 27]. It has been generally believed that the bone loss leading to osteoporosis begins at menopause in women (caused primarily by sex steroid deficiency) and later in life in men (caused by age-related factors) [53, 56, 61]. According to a more recent study, however, trabecular bone loss begins in young adulthood in both sexes and continues unabated throughout life [57]. Therefore, assessment of bone strength in individual patients of all ages is key to successful determination of fracture risk.
The most current view of osteoporosis, as emphasized at a recent consensus meeting sponsored by the National Institutes of Health and the American Society of Bone and Mineral Research, defines bone strength as an integration of both quantity and quality [46]. While bone quantity (mass) strongly correlates with strength [32], substantial variability remains unexplained [23] and growing evidence continues to demonstrate that measures or surrogates of bone quality are important for the evaluation of bone status [21, 52]. Although somewhat controversial and poorly defined, quality has been referred to as a combination of apparent modulus and strength as well as some quantified measures of the geometry, morphology, microdamage, material (tissue), and chemical properties of the bone [29]. From an engineering perspective, bone strength depends on a combination of its structural and material properties, both of which can be modulated by bone turnover [62]. Structural properties depend on the size and shape of the bone (ie, cortical thickness, cross sectional area, moments of inertia), the microarchitecture of the bone (ie, cortical porosity, trabecular morphology, degree of anisotropy), and the amount of accumulated damage (microcracks). Material properties depend on the degree of mineralization, the crystal size of minerals, the amount and type of collagen crosslinks, the interactions of mineral with the matrix, other proteins, and fat [29].
The purpose of this paper is to provide an analysis of trabecular properties associated with aging and fragility fractures using a hierarchical perspective in which we demonstrate the potential contributions of both bone quantity and quality to the apparent mechanical properties of trabecular bone. While accurate measures of bone quantity and quality have been demonstrated to explain nearly 90% of the variance in mechanical behavior, clinical and experimental experience suggests that the unexplained proportion of variance may be a key determinant in separating high- and low-risk patients. The information in this paper will consist of a review of prior studies on bone hierarchical properties in the literature combined with data from our laboratory in an effort to identify those factors that may be most influential in discriminating between low and high risk for fracture.
Current Assessment of Bone Quantity
Current conventional wisdom suggests that the most dominant factor related to skeletal fragility due to aging or osteoporosis is reduced bone mass. Measures of bone mineral density (BMD) have been demonstrated to explain a substantial portion of the risk of osteoporotic fractures [16, 39, 40]. Despite its limitations, areal bone mineral density (aBMD) by dual-energy xray absorptiometry (DXA) is widely used in clinical practice for the diagnosis and management of osteoporosis. aBMD can predict subsequent vertebral fractures with an increase in relative risk by 50% to 150% with each standard deviation decrease in bone mass, which is at least as good as the ability of blood pressure measurements to predict stroke and better than the predictive ability of serum cholesterol for cardiovascular disease [36]. BMD alone, however, does not determine if an individual will sustain a fracture [4, 36]. It is only one of many factors that contribute to bone strength [8]. In fact, there is substantial overlap in density measures between fracture and nonfracture patients [9, 11]. DXA does not provide information on volumetric density distribution, bone geometry, architecture, microstructure, or strength, parameters that have been found to be strong predictors of fracture [42]. Density, structure, and strength variables were highly correlated with spine aBMD, measured by DXA, but each was a stronger predictor of fracture in an age-adjusted logistic regression [42]. Furthermore, an analysis of bone structure and density interactions under different loading conditions revealed that the combination of bone loading estimates with skeletal strength parameters was more strongly associated with vertebral fracture risk than densitometry measure alone [42].
While BMD (a quantity measure) has traditionally been used for early detection of fracture risk, alternative structural imaging parameters (components of quality) are proposed to better predict the mechanical integrity of bone [43]. The inclusion of structural parameters follows a clear logic based on engineering principles. Following this logic, it is also assumed that accounting for the biomechanical material properties of the bone tissue would also contribute to improved risk prediction. As bone strength or other material properties cannot be directly assessed in vivo, indirect parameters may provide surrogates for fracture risk assessment [43]. In general, the evaluation of bone status is difficult because the bone changes are initially quite small, may not be highly related to apparent density, and are effectively localized to region (ie, one femoral head and not the other) and type of bone (ie, trabecular but not cortical) [43]. However, it has been shown that noninvasive assessment of structural parameters can provide a considerable predictive ability beyond the measurement of apparent density [43]. Importantly, many biologic and metabolic processes can have a great influence on the amount of bone, the local material properties, mechanisms of failure (such as crack propagation) and the ability to blunt or prevent failure. These processes include regulation of remodeling, the accumulation or repair of microdamage, and others. Taken together, the structural and material properties as well as the biologic activities that regulate these properties locally comprise what has been characterized as bone quality.
As noted earlier, the remainder of this paper is focused on describing the contribution of many of these quality factors to the resistance of bone to fracture.
Macrostructural Architecture
The geometry of the bones and the distribution of bone mass play an important role in determining bone strength and appear to differ in ways that parallel the risk of osteoporotic fracture [18, 73]. A recent study found that women with vertebral fractures had a slightly larger cross-sectional area accompanied by greater endocortical area and lower apparent cortical thickness, as well as reduced compressive strength in the outer 2 mm of vertebral cortical bone [42]. By estimating overall vertebral strength before and after virtually removing the peripheral 2-mm layer of bone in a finite element model, it has been shown that the cortical compartment carried about one half of the compressive load in both fracture cases and controls [42]. Therefore, although this paper focuses primarily on trabecular bone contributions in determining fracture risk, it is important to remember that the macrostructural architecture of cortical bone plays a crucial role in contributing to bone integrity.
Microstructural Architecture
Since macroscopic measures of bone density have not proven sufficient to explain clinical fracture, many studies have investigated the relationship between the architecture of trabecular bone and its mechanical properties. Work from our laboratory has clearly demonstrated the critical contribution of microarchitecture to the mechanical behavior of extracted volumes of trabecular bone[19, 20] and, as expected, trabecular bone microarchitecture, separate from density measures, has been shown to be an important determinant of bone strength [14]. Importantly, it appears to differ between osteoporotic and normal individuals and with age [9, 18]. Bone from nonfractured subjects has been shown to have substantially higher measures of bone volume fraction, trabecular number, and connectivity than fracture cases with a concomitant increase in apparent moduli and ultimate stress [9].
Detailed studies of both microarchitecture and density have provided strong correlations with trabecular bone stiffness and strength [19, 20]. Trabecular number, spacing, and connectivity highly correlate with ultimate strength and performed better than BMD derived from DXA in human calcaneal bone [43]. Given that the calcanei were of advanced age, it shows that bone loss, which ultimately leads to fragility fractures, occurs primarily through the loss of trabeculae (with concomitant loss of connectivity and increasing intertrabecular space), but not as a result of trabecular thinning [43]. In a study implementing a mechanical stimulation in ovine femora, the ultimate strength correlated most highly with structure model index (SMI), a purely architectural index, followed by bone volume fraction [44]. This important result implies that architecture may be considered an adjuvant to density for the evaluation of bone status and perhaps a viable alternative to densitometry. SMI and bone volume fraction also correlated with trabecular thickness and trabecular spacing, and less with trabecular number and connectivity. From a mechanistic perspective, this suggests that an increase in bone volume results in an increase in trabecular thickness, but does not cause an increase in trabecular number or connectivity [44]. Extrapolation of these results might support a strategy for a therapeutic intervention, such as mechanical stimuli, resulting in thickening of existing trabeculae, and not an increase in the number of trabeculae. However, ultimate strength is better correlated with trabecular number than with trabecular thickness. As a result, the maintenance of trabeculae is likely more important for the strength of the bone than is a subsequent increase in the thickness of remaining trabeculae. This supports the idea that prevention of bone loss may be more important and effective than strategies to add bone mass.
In addition to but separate from trabecular morphology, the degree of anisotropy of the trabecular bone (spatial orientation) has been shown to be important [9, 28]. In normal bone, between 80% and 90% of the variance in its mechanical behavior can be explained by the combined measures of density and orientation [19, 20]. Trabecular bone is highly anisotropic in nature and tends to form or reorganize itself toward the principal loading axis in order to increase its ability to withstand greater forces in the direction of maximal or habitual loading, regardless of bone density [27, 44]. The importance of trabecular anisotropy was remarkably demonstrated in a recent study we performed on bone sampled from hip fracture patients. Trabecular bone specimens retrieved from hip fracture patients were compared to site-matched specimens from a comparable sample extracted from unfractured cadaveric donors. When a group of specimens matched by density (using high-resolution micro-CT) were compared across the two groups, there was a substantial difference in anisotropy [9]. The osteoporotic hip fracture patients demonstrated an increase in anisotropy compared to controls (Fig. 1). Although the volume of bone tissue was equivalent between the groups, the hip fracture patients organized a greater amount of the bone tissue in the direction of habitual loading [9]. Consequently, during a fall in a direction orthogonal to the axis of habitual loading, the highly oriented bone (fracture group) had reduced ability to withstand the “off-axis” impact. In fact, in osteoporotic patients, trabecular bone reorganization may overcompensate for the low mass status by increasing the degree of anisotropy so that the strength of the bone is only maximized in the frequently loaded direction. Paralleling the findings in the hip, osteoporotic vertebral trabeculae were also shown to be more anisotropic than normal controls [28], although this adaptation may be advantageous in the spine, given that the mechanism of fracture is likely less related to loads from no habitual directions.
Bone specimens extracted from hip fracture patients and controls were evaluated for anisotropy. The specimens were matched by age, gender (female) and bone density (BV/TV by MicroCT). Fracture patients demonstrated a higher degree of anisotropy in the direction of habitual loading. (Adapted from J Bone Miner Res 2000;15:32–40 with permission of the American Society for Bone and Mineral Research.)
Tissue Material Properties
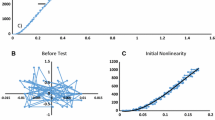
The mineral content of bone plays a crucial role in determining the stiffness and brittleness of bone tissue [12] and therefore may be associated with osteoporosis-related bone fragility. Although it is widely reported that mineral content increases with age [4, 22, 33], there have been no statistical differences reported in tissue modulus with age [26] or between patients with and without fractures [27]. However, unpublished data from our lab suggest there may be greater variability in local mineral content (even without differences in average mineral content) in hip fracture patients compared with controls (Fig. 2A–C). Therefore, it is conceivable that an increase in the variability of the bone mineral content of the bone tissue will lead to an increase in the number of initiated cracks and their spread, due to the increase in both the highly mineralized and less mineralized tissue.
Mean bone mineral content and standard deviation of bone mineral content were examined by scanning electron microscopy (SEM) in bone specimens extracted from osteoporotic hip fracture patients and normal non-fracture patients. The bone specimens were matched by age, gender (female) and bone density (BV/TV by MicroCT). (A) There was no difference in the means of pixel values between osteoporotic and normal individuals, (B) although there was a significantly higher standard deviation in pixel values in the osteoporotic patients (p = 0.004). (C) A representative SEM image shows the high variability in the degree of mineralization in a bone specimen extracted from a fracture patient.
Extracellular Matrix Properties
Quantifying the properties of bone extracellular matrix (ECM) is essential to defining the etiology and pathogenesis of osteoporosis and age-related increases in bone fragility. In fact, lamellar-level elastic modulus and hardness of bone depend on the microstructure of the ECM [26]. Nanoindentation studies demonstrate that the elastic moduli values for interstitial tissue exceed those for osteonal tissue and the values for trabecular tissue are lower than both [26]. This result is consistent with the fact that interstitial tissue is “older” (deposited at an earlier time point) and more mineralized than osteonal tissue. Trabecular tissue would be expected to have the lowest values since it is remodeled much more frequently.
Recent advances in the study of collagen maturation have revealed that collagen cross-links, constituents of the ECM, play an important role in bone strength [49, 50, 68, 71, 74] and proper biological function of bone [60, 67]. Cross-links derived from advanced glycation end products (AGE) have recently been reported to have detrimental effects on the mechanical behavior of bone. The level of serum and urine pentosidine, a well-characterized AGE in collagen, increases substantially with age [65, 72]. Accumulation of pentosidine decreases the mechanical property of bone and is associated with brittleness of collagen fibers [17, 69–71]. Urinary excretion of pentosidine was found to be associated with future vertebral fracture risk, independent of other traditional fracture risk factors, such as preexisting fractures, BMD, or age [63].
Cellular Biomechanics
Osteocytes have been hypothesized to play a central role in the mechanoregulatory system in bone. They are thought to contribute to the local maintenance of bone tissue by virtue of their ability to perceive the character of the mechanical demand on the bone and subsequently participate in signaling that regulates resorption or formation. Clearly, this hypothesized role is critical to maintain mechanical integrity of the tissue. As a result, it is logical to hypothesize that degradation in the ability of the osteocytes to sense the local mechanical demand could be responsible for the loss of bone associated with osteoporosis. This change in the ability of the cell to sense mechanical conditions could be caused by changes in the geometry of the osteocyte and its lacuna, changes in the fluid flow surrounding the cell, alterations in the material properties with the pericellular matrix, alterations in the cellular structural properties (such as cytoskeletal elements), changes in the cellular signaling mechanisms, and others. Recent data from our laboratory suggest, however, that neither the size nor shape of the lacunae, which influences the strain in osteocytes, play a role in osteoporotic fracture [37]. On the other hand, unpublished data in our lab suggest the relative properties of the osteocyte cytosol and unmineralized pericellular matrix are critical in influencing the strain in the osteocyte. In addition, the geometry of the lacuna, pericellular space, and osteocyte also act to modify the cell strain relative to the average matrix strain. Taken together, these data provide evidence that subtle changes in the pericellular matrix and possible age-related reduction in intracellular signaling mechanisms may contribute to a decrease in maintenance of ECM integrity and, therefore, bone integrity.
Chemical Properties
Beyond a relativity simple measure of mineral content, variations in the chemical composition of the organic and inorganic constituents of bone may be important in understanding fragility fractures. Mineral composition changes may involve crystallite size and size distribution, structural rearrangement and/or substitution (eg, Mg, CO3) [5]. Analogously, changes in collagen crosslinks or in collagen/mineral interactions may also result in alterations in the mechanical properties of the bone. Based on work in our group in collaboration with Prof. Michael Morris, the carbonate/phosphate ratio, measured by Raman spectroscopy, appears to be a key variable in osteoporotic fractures [38]. The differences in the carbonate/phosphate ratio may indicate a difference in the size of the mineral crystals in the bone tissue and/or may be an indirect measure of recent remodeling activity [38]. Recent data obtained by examining regions of visible damage in femoral bone tissue extracted from subjects who had hip fractures demonstrated a trend towards decreased mineral/matrix ratio. These results suggest the possibility that fractures in those patients were a result of chemical changes in the bone tissue, perhaps as a result of increased remodeling prior to fracture. Therefore, bone tissue quality, as described by chemical composition, may prove to be an additional factor to consider in characterizing the risk for osteoporotic fracture.
Discussion
Osteoporosis and bone fragility have principally been studied with regard to their association with low bone mass [58]. However, it is becoming increasingly evident that additional factors are likely critical to fully characterize the risk of osteoporotic fracture. A variety of factors that coalesce under the rubric of “quality” include measures of morphology, architecture, damage, remodeling dynamics, ECM and cellular mechanical properties, chemical constituency, and likely many others. Accounting for some or most of these factors may substantially improve our ability to assess fracture risk. Importantly, it also critical to recognize that many of these factors are influenced by genetic and hormonal regulation, as well as other conditions such as fall dynamics.
As noted above, most of these quantity and quality factors leading to osteoporotic bone fragility appear to be under strong genetic influence. For example, it has been reported that 80% to 85% of BMD is determined by genetics [45, 54]. A recent quantitative trait loci (QTL) study in our laboratories on mice vertebrae utilizing a genetically heterogeneous mouse population demonstrated the complexity of genetic control over vertebral form, function, and aging [55]. The QTL data found genetic markers were associated with traits on at least 13 different chromosomes influencing the size, shape, and/or mechanical properties of the vertebrae [55]. It is also generally recognized that estrogen deficiency plays an important role in the pathogenesis of postmenopausal bone loss and the subsequent development of osteoporosis and fractures [41]. Estrogen deficiency at menopause induces a phase of rapid bone loss over 5 to 10 years that is prevented by exogenous estrogen therapy [34]. Postmenopausal bone loss is associated with an increased bone turnover, reflected by an increase in biochemical markers of bone turnover [24, 59]. In a large cohort of healthy and ambulatory elderly women, the levels of serum estradiol (E2) and sex hormone-binding globulin (SHBG) were predictors of hip fracture, but this association was dependent on body weight [7]. However, women with high bone resorption were at higher risk of hip fracture, independently of other predictors, including hormonal levels [7]. The increased bone resorption, however, was not related to the degree of estrogen deficiency or to the level of serum SHGB [7].
Recent data suggest falls are a stronger predictor of hip fractures than BMD [31]. Falls increase in frequency with advancing age and account for at least 95% of hip fractures in the elderly [47]. More than a third of community-dwelling elderly people will fall each year and approximately 10% will sustain a major injury [66]. Elderly individuals tend to fall sideways or backward in a manner that applies a load in a direction very different from the usual load-bearing axis of the involved bone. Bone has been shown to be very anisotropic, with a microarchitecture that places more of the trabecular bone in an orientation to maximally withstand loads that are similarly aligned with the loads associated with habitual use (such as walking). Consequently, the proximal femur is more susceptible to fracture when the impact occurs in a direction that is nonhabitual. Thus, the risk of hip fracture is high in response to loads from a sideways fall [8].
Fractures are likely to occur when the load applied to a bone exceeds its strength, the ability to resist that load. The loads encountered in daily life are a function of body weight, height, and bending moments [15]. The ability to resist them is a function of the cross sectional area and vBMD of the bone [1]. In principle, the ratio of applied load to whole bone strength should predict fracture risk more efficiently than BMD measurements alone [25]. In order to asses this load-to-strength ratio, the activity or event associated with a fracture must be identified, and the applied load and bone strength for that event estimated. The ability of a bone to resist fracture at a given loading configuration depends not only on its mass but also on the spatial distribution of bone tissue and the intrinsic properties of bone material [2, 10, 35, 51]. A recent study showed that the ratio of skeletal loading to bone strength indices, as assessed by QCT, explains the age- and sex-specific patterns of wrist and hip fractures better than does BMD [57]. In addition, a similar study found that age- and sex-specific ratios for vertebral loading, relative to bone strength indices at the lumbar spine, resembled the incidence pattern of vertebral fractures over life more closely than did changes in spine vBMD [3]. Thus, to better understand the mechanisms contributing to fractures, both the forces applied to the bone and the strength of the bone need to be considered.
Given the hierarchical properties described in this paper and the fracture data summarized from the literature, several interesting observations and interpretations can be made concerning the factors associated with fracture risk.
Clearly, bone mass is an important factor. However, as noted in our studies evaluating trabecular architecture in a population of fracture and nonfracture subjects, high risk of hip fracture was most associated with the degree of trabecular anisotropy. When matched for bone mass, those individuals with more trabecular bone oriented in the direction of habitual loading were actually at higher risk for fracture.
In the vertebral bodies, the distribution of bone (bone mass organization) was associated with vertebral strength.
A variety of studies have found strong associations between genetic markers and bone structure and strength in both animals and humans.
We have described important relationships between measures of bone chemical constituency (using Raman microspectroscopy), functional properties and fractures. For example, carbonate/phosphate ratios were different between normal and hip fracture subjects.
Taken together, these observations demonstrate a consistently important role of trabecular bone macroscopic architecture, especially its anisotropy or 3-D spatial orientation. Perhaps, more importantly, they may relate to the propensity for an individual to optimally organize the existing trabecular bone in an orientation that tries to maximize load bearing in response to habitual usage patterns. In the hip, this was disadvantageous and placed the subjects at high risk of fractures from falls to the side. In the vertebral bodies, it likely maximizes strength for a given bone mass. Furthermore, the ability of an individual to maintain or perhaps create the structural anisotropy appears to be under strong genetic control. We would propose that the genetic regulation is manifest in the ability of the individual to remodel their trabecular bone in response to local mechanical conditions. Additional support for this premise may come from the Raman analyses. Properties such as carbonate/phosphate ratios may be characteristic of bone that is easier to resorb by osteoclasts and provide the ability for effective remodeling to occur.
In summary, the risk of fracture is far more complex than just assessing bone density. It likely depends on the combination and interaction of geometry, architecture (at all levels of hierarchy), material properties and the distribution of material properties, extracellular and cellular contributions, chemical properties as well as the character of the imposed loads (magnitude, rate, and direction) [4]. Genetics can influence the quantity or quality of bone or the propensity for an individual to alter these features in response to environmental cues or underlying physiological conditions. In fact, our studies could be interpreted to suggest that one of the most important factors associated with an individual’s risk of fracture may be their sensitivity or ability and propensity to remodel their trabecular bone to local mechanical factors.
References
Biggemann M, Hilweg D, Brinckmann P. Prediction of the compressive strength of vertebral bodies of the lumbar spine by quantitative computed tomography Skeletal Radiol. 1998;17:264–269.
Bouxsein ML. Application of biomechanics to the aging human skeleton. In: Glowacki J, Rosen CJ, Bilezikian JP, eds. The Aging Skeleton. San Diego, CA: Academic Press; 1999:315–330.
Bouxsein ML, Melton LJ, III, Riggs BL, Muller J, Atkinson EJ, Oberg AL, Robb RA, Camp JJ, Rouleau PA, McCollough CH, Khosla S. Age- and sex-specific differences in the factor of risk for vertebral fracture: A population-based study using QCT. J Bone Miner Res. 2006;21:1475–1482.
Boyce TM, Bloebaum RD. Cortical aging differences and fracture implications for the human femoral neck. Bone. 1993;14:769–778.
Carden A, Morris MD. Application of vibrational spectroscopy to the study of mineralized tissues. J Biomed Opt. 2000;5:259–268.
Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA. Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet. 1999;353:878–882.
Chapurlat RD, Garnero P, Breart G, Meunier PJ, Delmas PD. Serum estradiol and sex hormone-binding globulin and the risk of hip fracture in elderly women: The EPIDOS study. J Bone Miner Res. 2000;15:1835–1841.
Cheung AM, Detsky AS. Osteoporosis and fractures: missing the bridge? JAMA. 2008;299:1468–1470.
Ciarelli TE, Fyhrie DP, Schaffler MB, Goldstein SA. Variations in three dimensional cancellous bone architecture of the proximal femur in female hip fractures and in controls. J Bone Miner Res. 2000;15(1):32–40.
Crawford RP, Cann CE, Keaveny TM. Finite element models predict in vitro vertebral body compressive strength better than quantitative computed tomography. Bone. 2003;33:744–750.
Cummings SR. Are patients with hip fractures more osteoporotic? Review of the evidence. Am J Med. 1985;78:487–494.
Currey JD. The effect of porosity and mineral content on the Young’s modulus of elasticity of compact bone. J Biomech. 1988;21:131–139.
Davidson MR. Pharmacotherapeutics for osteoporosis prevention and treatment. J Midwifery Womens Health. 2003;48:39–52.
Dempster DW. The contribution of trabecular architecture to cancellous bone quality. J Bone Miner Res. 2000;15:20–23.
Duan Y, Seeman E, Turner CH. The biomechanical basis of vertebral body fragility in men and women. J Bone Miner Res. 2001;16:2276–2283.
Faulkner DG, Cummings SR, Black D, Palermo L, Glüer C-C, Genant HK. Simple measurement of femoral geometry predicts hip fracture: The study of osteoportic fractures. J Bone Miner Res. 1993;8:1211–1217.
Garnero P BO, Gineyts E, Duboeuf F, Solberg H, Bouxsein ML, Christiansen C, Delmas PD. Extracellular post-translational modifications of collagen are major determinants of biomechanical properties of fetal bovine cortical bone. Bone. 2006;38:300–309.
Gluer C-C CS, Pressman A, Li J, Gluer K, Faulkner KG, Grampp S, Genant HK, The Study of Osteoporotic Fractures Research Group. Prediction of hip fractures from pelvic radiographs: The study of osteoporotic fractures. J Bone Miner Res. 1994;9:671–677.
Goldstein SA, Goulet R, McCubbrey D. Measurement and significance of three-dimensional architecture to the mechanical integrity of trabecular bone. Calcif Tissue Int. 1993;53(Suppl 1):S127–S133.
Goulet RW, Goldstein SA, Ciarelli MJ, Kuhn JL, Brown MB, Feldkamp LA. The relationship between the structural and mechanical properties of trabecular bone. J Biomech. 1994;27(4):375–389.
Grimm MJ, Williams JL. Assessment of bone quantity and “quality” by ultrasound attenuation and velocity in the heel. Clin Biomech. 1997;5:281–285.
Grynpas M. Age and disease-related changes in the mineral of bone. Calcif Tissue Int. 1993;53(Suppl 1):S57–S64.
Hans D, Fuerst T, Lang T, Majumdar S, Lu Y, Genant HK, Glüer C. How can we measure bone quality? Baillieres Clin Rheumatol. 1997;11:495–515.
Hansen MA, Kirsten O, Riis BJ, Christiansen C. Role of peak bone mass and bone loss in postmenopausal osteoporosis: 12 years study. BMJ. 1991;303:961–964.
Hayes WC, Piazza SJ, Zysset PK. Biomechanics of fracture risk prediction of the hip and spine by quantitative computed tomography. Radiol Clin North Am. 1991;29:1–8.
Hoffler CE, Moore KE, Kozloff K, Zysset PK, Goldstein SA. Age, gender, and bone lamellae elastic moduli. J Orthop Res. 2000;18:432–437.
Homminga J, McCreadie BR, Ciarelli TE, Weinans H, Goldstein SA, Huiskes R. Cancellous bone mechanical properties from normals and patients with hip fractures differ on the structure level, not on the bone hard tissue level. Bone. 2002;30:759–764.
Homminga J, Rietbergen Bv, Lochmuller E-M, Weinans H, Eckstein F, Huiskes R. The osteoporotic vertebral structure is well adapted to the loads of daily life, but not to infrequent”error” loads. Bone. 2004;34:510–516.
Judex S, Boyd S, Quin Y-X, Miller L, Muller R, Rubin C. Combining high-resolution micro-computed tomography with material composition to define the quality of bone tissue. Curr Osteoporos Rep. 2003;1:11–19.
Kado DM, Browner WS, Palermo L, Nevitt MC, Genant HK, Cummings SR. Vertebral fractures and mortality in older women: a prospective study. Study of Osteoporotic Fractures Research Group. Arch Intern Med. 1999;159:1215–1220.
Kaptoge S, Benevolenskaya LI, Bhalla AK, Cannata JB, Boonen S, Falch JA, Felsenberg D, Finn JD, Nuti R, Hoszowski K, Lorenc R, Miazgowski T, Jajic I, Lyritis G, Masaryk P, Naves-Diaz M, Poor G, Reid DM, Scheidt-Nave C, Stepan JJ, Todd CJ, Weber K, Woolf AD, Roy DK, Lunt M, Pye SR, O’Neill TW, Silman AJ, Reeve J. Low BMD is less predictive than reported falls for future limb fractures in women across Europe: results from the European Prospective Osteoporosis Study. Bone. 2005;36(3):387–398.
Keaveny TM, Morgan EF, Niebur GL, Yeh OC. Biomechanics of trabecular bone. Annu Rev Biomed Eng. 2001;3:307–333.
Kingsmill VJ, Boyde A. Mineralization density of human mandibular bone: quantitative backscattered electron image analysis. J Anat. 1998;192:245–256.
Lindsay R, Hart DM, Forrest C, Baird C. Prevention of spinal osteoporosis in oophorectomized women. Lancet. 1980;2:1151–1153.
Lochmuller E-M, Lill CA, Kuhn V, Schneider E, Eckstein F. Radius bone strength in bending, compression, and falling and its correlation with clinical densitometry at multiple sites. J Bone Miner Res. 2002;17:1629–1638.
Marshall D, Johnell O, Wedel H. Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ. 1996;312:1254–1259.
McCreadie BR, Hollister SJ, Schaffler MB, Goldstein SA. Osteocyte lacuna size and shape in women with and without osteoporotic fracture. J Biomech. 2004;37(4):563–572.
McCreadie BR, Morris MD, Chen T, Rao Ds, Finney WF, Widjaja E, Goldstein SA. Bone tissue compositional differences in women with and without osteoporotic fracture. Bone. 2006;39:1190–1195.
Melton LJ III, Atkinson EJ, O’Connor MK, O’Fallon WM, Riggs BL. Determinants of bone loss from the femoral neck in women of different ages. J Bone Miner Res. 2000;15:24–31.
Melton LJ III, Atkinson EJ, O’Fallon WM, Wahner HW, Riggs BL. Long-term fracture prediction by bone mineral assessed at different skeletal sites. J Bone Miner Res. 1993;8:1227–1233.
Melton LJ III, Khosla S, Riggs BL. A unitary model for involution osteoporosis: Estrogen deficiency causes both type I and type II osteoporosis in postmenopausal women and contributes to bone loss in aging men. J Bone Miner Res. 1998;13:763–773.
Melton LJ III, Riggs BL, Keaveny TM, Achenbach SJ, Hoffmann PF, Camp JJ, Rouleau PA, Bouxsein ML, Amin S, Atkinson EJ, Robb RA, Khosla S. Structural determinants of vertebral fracture risk. J Bone Miner Res. 2007;22:1885–1892.
Mittra E, Rubin C, Gruber B, Qin Y-X. Evaluation of trabecular mechanical and microstructural properties in human calcaneal bone of advanced age using mechanical testing μCT, and DXA. J Biomech. 2008;41:368–375.
Mittra E, Rubin C, Qin Y-X. Interrelationship of trabecular mechanical and microstructural properties in sheep trabecular bone. J Biomech. 2005;38:1229–1237.
Nguyen TV, Eisman JA. Genetics of fracture: challenges and opportunities. J Bone Miner Res. 2000;15:1253–1256.
NIH Consensus Development Panel on Osteoporosis Prevention, Diagnosis, Therapy. Osteoporosis prevention, diagnosis, and therapy. JAMA. 2001;285:785–795.
Nyberg L, Gustafson Y, Berggren D, Brannstrom B, Bucht G. Falls leading to femoral neck fractures in lucid older people. J Am Geriatr Soc. 1996;44:156–160.
Oleksik A, Lips P, Dawson A, Minshall ME, Shen W, Cooper C, Kanis J. Health-related quality of life in postmenopausal women with low BMD with or without prevalent vertebral fractures. J Bone Miner Res. 2000;15:1384–1392.
Oxlund H, Barchman M, Ortoft G, Andreassen TT. Reduced concentration of collagen cross-links are associated with reduced strength of bone. Bone. 1995;17(Suppl 4):S365–S371.
Oxlund H, Mosekilde L, Ortoft G. Reduced concentration of collagen reducible crosslinks in human trabecular bone with respect to age and osteoporosis. Bone. 1996;19:479–484.
Pistoia W, Rietbergen BV, Lochmuller E-M, Lill CA, Eckstein F, Ruegsegger P. Estimation of distal radius failure load with micro-finite element analysis models based on three-dimensional peripheral quantitative computed tomography images. Bone. 2002;30:842–848.
Pothuaud L, Rietbergen Bv, Mosekilde L, Beuf O, Levitz P, Benhamou CL, Majumdar S. Combination of topological parameters and bone volume fraction better predicts the mechanical properties of trabecular bone. J Biomech. 2002;35:1091–1099.
Raisz LG. Local and systemic factors in the pathogenesis of osteoporosis. N Engl J Med. 1998;318:818–828.
Ralston SH. The genetics of osteoporosis. Bone. 1999;25:85–86.
Reeves GM, McCreadie BR, Chen S, Galecki AT, Burke DT, Miller RA, Goldstein SA. Quantitative trait loci modulate vertebral morphology and mechanical properties in a population of 18-month-old genetically heterogeneous mice. Bone. 2007;40:433–443.
Riggs BL, Khosla S, Melton LJ. Sex steroids and the construction and conservation of the adult skeleton. Endocr Rev. 2002;23:279–302.
Riggs BL, LJ Melton I, Robb RA, Camp JJ, Atkinson EJ, McDaniel L, Amin S, Rouleau PA, Khosla S. A population-based assessment of rates of bone loss at multiple skeltal sites: evidence for substantial trabecular bone loss in young adult women and men. J Bone Miner Res. 2008;23:205–214.
Riggs BL, Melton LJ. Involutional osteoporosis. N Engl J Med. 1986;314:1676–1686.
Riis BJ, Hansen AM, Jensen K, Overgaard K, Christiansen C. Low bone mass and fast rate of bone loss at menopause-equal risk factors for future fracture. A 15 years follow-up study. Bone. 1996;19:9–12.
Saito M, Soshi S, Fujii K. Effect of hyper- and micro-gravity on collagen post-translational controls of MC3T3-E1 osteoblast. J Bone Miner Res. 2003;18:1695–1705.
Seeman E. Pathogenesis of bone fragility in women and men. Lancet. 2002;359:1841–1850.
Seeman E, Delmas PD. Bone quality: the material and structural basis of bone strength and fragility. N Engl J Med. 2006;354:2250–2261.
Shiraki M, Kuroda T, Tanaka S, Saito M, Fukunaga M, Nakamura T. Nonenzymatic collagen cross-links induced by glycoxidation (pentosidine) predicts vertebral fractures. J Bone Miner Res. 2008;26:93–100.
Silverman SL, Minshall ME, Shen W, Harper KD, Xie S. Health-related quality of life subgroup of the Multiple Outcomes of Raloxifene Evaluation Study. The relationship of health-related quality of life to prevalent and incident vertebral fractures in postmenopausal women with osteoporosis: results from Multiple Outcomes of Raloxifene Evaluation Study. Arthritis Rheum. 2001;44:2611–2619.
Takahashi M, Oikawa M, Nagano A. Effect of age and menopause on serum concentrations of pentosidine, an advanced glycation end product. J Gerontol A Biol Sci Med Sci. 2000;55:137–140.
Tinetti ME. Preventing falls in elderly persons. N Engl J Med. 2003;348:42–49.
Uzawa K, Grezesik WJ, Nishimura T, Kuznetsov SA, Robey PG, Brenner DA, Yamauchi M. Differential expression of human lysyl hydroxylase genes,lysyl hydroxylation, and cross-linking of type I collagen during osteoblastic differentiation in vitro. J Bone Miner Res. 1999;14:1270–1280.
Vashishth D, Gibson GJ, Khoury JI, Schaffler MB, Kimura J, Fyhrie DP. Influence of nonenzymatic glycation on biochemical properties of cortical bone. Bone. 2001;28:195–201.
Viguet-Carrin S, Garnero P, Delmas PD. The role of collagen in bone strength. Osteoporos Int. 2006;17:319–336.
Viguet-Carrin S, Roux JP, Arlot ME, Merabet Z, Leeming DJ, Byrjalsen I, Delmas PD, Bouxsein ML. Contribution of the advanced glycation end product pentosidine and of maturation of type I collagen to compressive biomechanical properties of human lumbar vertebrae. Bone. 2006;39:1073–1079.
Wang X, Shen X, Li X, Agrawal CM. Age-related changes in the collagen network and toughness of bone. Bone. 2002;31:1–7.
Yoshihara K, Nakamura K, Kanai M, Nagayama Y, Takahashi S, Saito N, Nagata M. Determination of urinary and serum pentosidine and its application to elder patients. Biol Pharm Bull. 1998;21:1005–1008.
Yoshikawa T, Turner CH, Peacock M, Slemenda CW, Weaver CM, Teegarden D, Markwardt P, Burr DB. Geometric structure of the femoral neck measured using dual-engergy x-ray absorptiometry. J Bone Miner Res. 1994;9:1053–1064.
Zioupos P, Currey JD, Hamer AJ. The role of collagen in the declining mechanical properties of aging human cortical bone. J Biomed Mater Res. 1999;45:108–116.
Acknowledgments
We thank Peggy Piech for her contributions to this manuscript. We acknowledge the scientific contributions of Dr. Barbara McCreadie and Dr. Traci Ciarelli from discussions and reviews of their research.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article. Funding from the wide variety of studies summarized in this paper was provided from grants from the National Institutes of Health, the National Science Foundation, and the Whitaker Foundation.
About this article
Cite this article
Kreider, J.M., Goldstein, S.A. Trabecular Bone Mechanical Properties in Patients with Fragility Fractures. Clin Orthop Relat Res 467, 1955–1963 (2009). https://doi.org/10.1007/s11999-009-0751-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-009-0751-8