Abstract
Cam-type femoroacetabular impingement is a recognized cause of intraarticular pathology and secondary osteoarthritis in young adults. Arthroscopy is reportedly useful to treat selected hip abnormalities and has been proposed as a method of correcting underlying impingement. We report the outcomes of arthroscopic management of cam-type femoroacetabular impingement. We prospectively assessed all 200 patients (207 hips) who underwent arthroscopic correction of cam impingement from December 2003 to October 2007, using a modified Harris hip score. The minimum followup was 12 months (mean, 16 months; range, 12–24 months); no patients were lost to followup. The average age was 33 years with 138 men and 62 women. One hundred and fifty-eight patients (163 hips) underwent correction of cam impingement (femoroplasty) alone while 42 patients (44 hips) underwent concomitant correction of pincer impingement. The average increase in Harris hip score was 20 points; 0.5% converted to THA. We had a 1.5% complication rate. The short-term outcomes of arthroscopic treatment of cam-type femoroacetabular impingement are comparable to published reports for open methods with the advantage of a less invasive approach.
Level of Evidence: Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Femoral head impingement is not a new concept. As early as 1913, Vulpius and Stöffel [24] described a bony resection procedure for the deformity created by a slipped capital femoral epiphysis. In 1936, Smith-Petersen [21] described excising the acetabular rim sometimes combined with a wedge resection of the femoral head-neck junction for patients with protrusio, slipped epiphysis, and coxa plana. Although primitive, with simple bone cuts, the technique bears a striking similarity to the recent descriptions of open surgical dislocation for pincer and cam impingement. This combined approach received no further mention in the literature, although osteoplasty for the femoral deformity associated with chronic slipped capital femoral epiphysis was popularized by Heyman and Herndon [15] and was similarly suggested for the misshapen femoral head of coxa plana as a sequela of Perthes’ disease [14]. In 1998, we described arthroscopic correction of impingement due to posttraumatic osteophytes and also reported an arthroscopic technique of cheilectomy of femoral protuberances associated with Perthes’ disease [8, 9].
In 1975, Stulberg et al. described the “pistol-grip” deformity of the femoral head and observed its association with early-age-onset osteoarthritis, especially in men [23]. However, it was Ganz and colleagues who formulated the concept of femoroacetabular impingement (FAI). This was first described as an iatrogenic process associated with overcorrection of periacetabular osteotomy performed for dysplasia [18]. Subsequently, they described FAI occurring in the native hip as a precursor to the development of osteoarthritis [13]. They subgrouped this into pincer, cam, and combined types and described an open surgical approach for correction [2, 16].
We believe FAI is not a cause of hip pain per se. Rather, it is simply a morphologic variant predisposing the joint to intraarticular pathology that then becomes symptomatic. Pincer impingement, caused by an overhanging of the anterolateral rim of the acetabulum, results primarily in breakdown of the acetabular labrum and secondarily, over time, a variable amount of associated articular damage to the acetabulum. Cam impingement, created by the prominent portion of a nonspherical femoral head engaging against the articular surface of the acetabulum, results in selective delamination and failure of the articular surface of the acetabulum with relative preservation of the labrum (Fig. 1A–B). These observations are important in the proposed arthroscopic management of FAI. Hips may possess the morphologic features of FAI without developing the cartilage failure associated with pathologic impingement. Thus, the arthroscopic findings are a determinant in the course of management for patients who possess radiographic features of FAI. Impingement is not the sole cause of intraarticular pathology and subsequent hip symptoms in active adults. In our experience in the arthroscopic management of FAI, there has been a preponderance of cam lesions. Cam impingement has a predilection for younger adult males and especially those who are physically active. It is possible to have a nonspherical femoral head (cam morphology) and not develop subsequent intraarticular damage. However, in the presence of hip joint symptoms, commonly characterized by groin pain, especially exacerbated with flexion and internal rotation, and a positive impingement sign, it may be better to take a proactive approach to the surgical management.
Diagrams illustrate (A) cam morphology created by bony prominence at the anterolateral head-neck junction, resulting in a nonspherical femoral head; and (B) dynamics of cam impingement that occur with hip flexion. Compared to normal, the cam lesion glides underneath the labrum engaging the edge of the articular cartilage and results in progressive delamination. Initially the labrum is relatively preserved, but secondary failure occurs over time. (Reprinted with permission from J. W. Thomas Byrd, MD.)
We hypothesized arthroscopic surgery would enhance function in patients with cam type FAI. The purpose of this study was to (1) ascertain whether arthroscopy improved the Harris hip score and (2) the frequency of complications.
Materials and Methods
We prospectively followed all 220 patients (227 hips) treated with arthroscopy for FAI from December 2003 to October 2007. From this group, cam impingement occurred in 200 patients (207 hips, of which 163 were cam only and 44 cam combined with pincer impingement). We excluded the other 20 hips with pincer impingement only leaving 207 hips. This cohort was identified from a database of all hip arthroscopy patients that have been prospectively assessed utilizing a modified Harris hip score [5, 6] preoperatively and then postoperatively at 3, 12, 24, 60, and 120 months. This modified score incorporates only the pain and function portion of the original Harris hip score. There were 138 men and 62 women with 120 right and 87 left hips. The cam patients tended to be slightly younger, with an average age of 33 years versus 35 years for combined lesions. A bimodal age distribution was identified with a peak at age 20 years and a second peak at age 43 years. Ninety-four (45%) were athletics-related. For those patients younger than 30 years (n = 88), 62 (70%) were associated with athletic activities, while after the third decade (n = 119), only 30 (25%) were associated with athletics. The younger-than-30-years group was also more male-dominated, with a male:female ratio of 3.1:1 compared to the older-than-30-years group with a ratio of 1.9:1. There was 100% followup of the 207 hips (163 cam; 44 combined) at a minimum of 12 months (average, 16 months; range, 12–24 months).The data obtained and presented in this manuscript have been granted exemption status by the Institutional Review Board.
The indication for hip arthroscopy was recalcitrant hip pain with imaging evidence of intraarticular pathology or clinical findings of persistent hip symptoms, as previously described, that were unresponsive to nonoperative measures including activity modification and time [7]. Offending activities were identified and efforts made to eliminate or reduce these below the threshold of creating symptoms. The duration of symptoms prior to surgical intervention averaged 32 months. Patients were excluded if (1) the disease state was too advanced to reasonably benefit from arthroscopic intervention, with bone on bone contact an absolute contraindication; or (2) the patient had unreasonable expectations that could not practically be accomplished by the procedure because the patient’s goal for activities exceeded the limitations imposed by the disease. Thus, while we attempted to establish objective criteria, the decision for surgery was partly influenced by how the disease process influenced each individual’s lifestyle.
For this cohort with cam impingement, the indications for addressing associated impingement were partly based on the radiographic findings and principally based on arthroscopic parameters. Cam impingement was suggested by the radiographic features of loss of sphericity of the femoral head. For cases in which this was suspected, a 3-D CT scan was helpful at more clearly detailing the bony architecture in anticipation of arthroscopic correction. We substantiated cam pathology associated with radiographic cam morphology by the arthroscopic finding of secondary abnormality characterized by articular surface failure with delamination of the anterolateral acetabulum.
The articular damage was classified according to the Outerbridge system [19]. Most patients had Outerbridge Grade IV (107) or Grade III (83) articular damage on at least one side of the joint. The most advanced changes were on the acetabular side with the femoral head appearing normal in 157 cases. Variable labral failure may begin to occur, but there remains a disproportionate amount of articular pathology with relative labral preservation. A variable amount of labral pathology was present in 189 cases.
The basic principles developed in the early 1990s have served as the foundation for the subsequent establishment of methods of addressing FAI [3, 10, 11]. While corrective surgery has been performed for impingement due to posttraumatic osteophytes since early in the development of the technique, FAI as a formal indication has been incorporated only since 2003 [4, 8, 9, 12].
Addressing cam impingement began with arthroscopy of the central compartment where the presence of cam pathology was documented (Figs. 2A–G, 3A–G). The characteristic feature was articular failure of the anterolateral acetabulum. There was often associated failure of the labrum at its base, but there was a disproportionate amount of articular abnormality relative to the labral pathology. The articular damage was addressed with chondroplasty and microfracture as dictated by its severity. The associated labral pathology was conservatively débrided, creating a stable edge. Débridement could be selectively limited to the articular side of the labrum, allowing preservation of its capsular surface and maintaining much of the labral substance. Fifty-eight underwent microfracture. Microfracture was indicated for Grade IV articular lesions with an intact subchondral plate and healthy surrounding articular edges.
Images illustrate the case of a 20-year-old hockey player with a 4-year history of right hip pain. (A) An anteroposterior radiograph is unremarkable. (B) A frog lateral radiograph demonstrates a morphologic variant with bony buildup at the anterior femoral head-neck junction (arrow) characteristic of cam impingement. (C) A 3-D CT scan further defines the extent of the bony lesion (arrows). (D) Viewing from the anterolateral portal, the probe introduced anteriorly displaces an area of articular delamination from the anterolateral acetabulum characteristic of the peel back phenomenon created by the bony lesion shearing the articular surface during hip flexion. (E) Viewing from the peripheral compartment, the bony lesion is identified (*) immediately below the free edge of the acetabular labrum (L). (F) The lesion has been excised, recreating the normal concave relationship of the femoral head-neck junction immediately adjacent to the articular surface (arrows). Posteriorly, resection is limited to the midportion of the lateral neck to avoid compromising blood supply to the femoral head from the lateral retinacular vessels. (G) A postoperative 3-D CT scan illustrates the extent of bony resection. (Reprinted with permission from J. W. Thomas Byrd, MD.)
Images illustrate the case of a 38-year-old woman with progressive pain and loss of motion of the right hip. (A) An anteroposterior radiograph demonstrates acquired bony buildup/osteophyte formation on the lateral femoral head (arrow). (B) A frog lateral radiograph further defines the bony buildup on the anterior femoral head (arrow). (C) A 3-D CT scan further defines the femoral head osteophyte (*) and the anterior acetabular lesion (arrows). (D) Arthroscopy of the central weightbearing surface of the joint demonstrates good articular preservation of both the acetabulum (A) and femoral head (FH) with some reactive synovitis within the fossa (S). (E) The anterior acetabular osteophyte is excised. (F) Viewing peripherally, the femoral head has been recontoured showing the edge of the femoral articular surface (white arrows) and the labrum (black arrows). (G) A postoperative 3-D CT scan demonstrates the extent of bony recontouring of both the acetabulum and femoral head. (Reprinted with permission from J. W. Thomas Byrd, MD.)
After completing arthroscopy of the central compartment, the cam lesion was addressed from the peripheral compartment. A capsulotomy was created by connecting the anterior and anterolateral portals. The posterolateral portal could be removed and the anterior and anterolateral cannulae were simply backed out of the central compartment. The traction was released, and the hip flexed approximately 35°. As the hip was flexed under arthroscopic visualization, the line of demarcation between healthy cartilage and abnormal fibrocartilage that covered the cam lesion could usually be identified.
A cephalad anterolateral portal was established approximately 5 cm above the anterolateral portal, entering through the capsulotomy already established. These proximal and distal anterolateral portals worked well for accessing and addressing the cam lesion. The anterior portal could be removed or maintained if it was needed for better access to the medial side of the femoral neck.
Most of the work for performing the recontouring of the cam lesion (femoroplasty) involved soft tissue preparation. This included capsular débridement as necessary to assure complete visualization of the lesion and then removal of the fibrocartilage and scar that covered the abnormal bone. With the hip flexed, the proximal portal provided better access for the lateral and posterior portion, while the distal portal was more anterior relative to the joint and provided best access for the anterior part of the lesion. The lateral synovial fold was identified as the arthroscopic landmark for the retinacular vessels and care was taken to preserve this structure during the recontouring. Switching between the portals was important to fully appreciate the 3-D anatomy of the recontouring.
Once the bone was fully exposed, recontouring was performed with a spherical burr. The goal was to remove the abnormal bone identified on the preoperative CT scan and recreate the normal concave relationship that should exist where the femoral neck meets the articular edge of the femoral head. We began the resection at the lateral/posterior limit of the cam lesion with the arthroscope in the more distal portal and instrumentation in the more proximal portal. The posterior extent of the resection was usually the most difficult; the resection was also the most critical to avoid notching the tensile surface of the femoral neck; and particular attention was given to avoiding and preserving the lateral retinacular vessels. Then, switching the arthroscope to the proximal portal, the burr was introduced distally and the reshaping was completed along the anterior head and neck junction. Lastly, attention was given to making sure all bone debris was removed as thoroughly as possible to lessen the likelihood of developing heterotopic ossification.
We initiated formal supervised physical therapy within 1 or 2 days after surgery. Emphasis was placed on optimizing range of motion, with early implementation of closed chain joint stabilization and core strengthening exercises. Patients were allowed to weight bear as tolerated, but crutches were used for 4 weeks as a precautionary measure to protect the femoroplasty site against any awkward twisting episodes. Once normal muscle tone and firing were regained, these adequately protected the joint for normal forces. We recommended avoiding impact loading for 3 months while the bone fully remodeled. The rehabilitation protocol was modified for microfracture by keeping patients on a strict protected weight bearing status for 2 months. Patients were allowed to place the weight of their leg on the ground in order to reduce the forces across the joint. A formal structured rehabilitation protocol was continued for 3 months. For athletes, functional progression was then advanced as tolerated. While some athletes resumed unrestricted activities quickly, usually it was anticipated that another 1 to 3 months were necessary for full participation.
Results
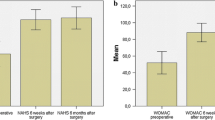
The mean improvement in the Harris hip score at last followup was 20 points with a range of −17 to 60 points. Overall, 83% were improved. We noted continued improvement throughout the first year, with scores maintained in those with 2-year followup (Fig. 4). The scores of patients with cam and combined lesions were comparable, with 20- (range −17 to 60) versus 19- point (range −15 to 49) improvement, respectively. Those with microfracture demonstrated an average 20-point improvement (preoperative score, 65; postoperative score, 85) with a range of −17 to 58.
One patient (0.5%) with extensive Grade IV articular loss of both the acetabular and femoral surfaces was converted to a THA at 8 months postarthroscopy for recalcitrant pain. Three patients underwent a second arthroscopic procedure due to mechanical symptoms. Three patients had complications, but all resolved clinically. There was one transient neuropraxia of the pudendal nerve that resolved within 2 weeks and one partial neuropraxia of the lateral femoral cutaneous nerve that resolved by 1 month. One patient developed heterotopic ossification within the capsule, which did not preclude a high Harris hip score.
Discussion
Femoroacetabular impingement is a well-recognized cause of joint damage and osteoarthritis among young adults. With this study, we have tried to reflect on the response to arthroscopic treatment for cam-type FAI.
There are two major limitations of this study. First is the absence of a control group from which to compare the results of arthroscopic intervention. With the recognition of impingement as a causative factor in joint pathology, we believe it difficult to justify neglecting its presence in symptomatic individuals or simply address the secondary joint pathology without correcting the underlying impingement, either of which would provide an otherwise interesting comparison group. The second limitation of this study is a lack of an adequate outcomes measurement tool for assessing hip function in active individuals. The pain and function portion of the Harris hip score, which constitutes the modified version, has been validated but still has a ceiling effect with difficulty separating those with a high level of function [25]. The Harris hip score has several shortcomings (eg, ceiling effects), but as a recognized and accepted instrument, we continue to use it until a clearly superior rating system can be developed.
While surgery can result in successful outcomes, the joint can never be truly restored to a disease-free state. Thus, with the recognized causal relationship of FAI with intraarticular pathology, emphasis on injury prevention will become more paramount. We observed a bimodal age distribution with the older cohort reflecting the traditionally recognized group of early onset adult osteoarthritis. The younger cohort tended to be much more active, with 70% participating in athletic activities. Often, athletes push their bodies beyond their physiologic limits, where breakdown occurs. With impingement, this threshold is lowered where failure of the hip can occur with seemingly physiologic activities. It is hoped, if impingement can be identified in those with an active lifestyle, then maybe modifications could be implemented to protect their joint before breakdown occurs. Simple examples such as squats as a form of training and conditioning may prove especially deleterious to hips at risk for impingement. Perhaps, with better recognition of impingement and offending activities, substantial strides could be made in nonoperative management. We did not address the etiology of the cam morphology but our observations support those in other reports that this type of proximal femoral deformity is male-dominated [23]. This is observed in the older cohort of mature adults developing early age onset osteoarthritis with a 1.86 male:female ratio and especially evident among the younger active adults with a 3.14 male:female ratio.
Arthroscopic management of impingement is not a new concept. Acetabular and femoral lesions have been addressed at our center for two decades. However, these were limited to posttraumatic osteophytes, avulsed fragments, and the occasional severely misshapen femoral head as a sequela of Perthes’ disease [8, 9]. With the initial development of the concept of FAI, we were slow to adopt a role for its arthroscopic management. As the credence of FAI became more evident, we began to explore the potential value of a less-invasive arthroscopic approach [4, 12]. Compared to the generous exposure provided with open surgical dislocation of the hip, arthroscopic visualization and orientation of the cam lesion is more challenging. Meticulous soft tissue preparation and a capsular window as necessary to fully visualize the lesion are important. The 3-D CT scan provides certainty on defining the margins of abnormal bone. With good visualization, recontouring can then be performed in a comparable fashion that approaches that of the open technique. We also believe there may be many individuals with abnormally shaped femoral heads who do not develop intraarticular failure due to cam impingement. Thus, it is possible to have cam morphology without cam pathology. The arthroscopic findings then become an important component in the decision to address the cam lesion. Frank or impending articular failure of the anterior acetabulum reflects the importance of performing an accompanying femoroplasty. The surgeon must weigh the risks of performing a potentially unnecessary procedure in an asymptomatic individual with cam morphology against the risks of allowing unchecked progression of the deleterious process. In our study, 94% already had Grade IV (107) or Grade III (83) articular damage. While some cases may remain stable for a protracted period of time, if the clinical presentation reflects progressive symptoms, we would advocate a proactive approach in the management of impingement. Femoroplasty is the term chosen for reshaping the femoral lesion, as this is consistent with other nomenclature for the hip (ie, acetabuloplasty) and the arthroscopic nomenclature used for other joints, such as acromioplasty in the shoulder or notchplasty in the knee. In the arthroscopic management of impingement, osteoplasty is too generic and nondescript and the term chondro-osteoplasty is easily confused with chondroplasty when describing arthroscopic procedures.
Our early experience in the arthroscopic management of cam impingement has resulted in generally high Harris hip scores, even in the presence of advanced pathology with 94% Grade IV and Grade III articular damage. Overall, 83% were improved with only one (0.5%) having conversion to a THA at 8 months postarthroscopy. We performed microfracture in 58 cases. In general, this was reserved for Grade IV lesions with healthy surrounding cartilage. Diffuse erosive lesions were deemed a contraindication. However, sometimes this was attempted even for more severe lesions in younger patients. While it is uncertain whether this resulted in more favorable outcomes than would have been encountered with chondroplasty alone, it did not seem to have any deleterious consequences. As supported for other joints, microfracture offers some opportunity for potentiating a fibrocartilaginous healing response with minimal added morbidity [22]. With regards to arthroscopic correction of cam impingement, we observed few complications and none that adversely affected a patient’s outcome. The problems encountered likely reflected the more extensive nature of this arthroscopic procedure in contrast to simpler arthroscopic cases in which the impingement is not addressed. Nonetheless, in contrast to open methods for addressing impingement, this less-invasive procedure has several advantages. It is performed on an outpatient basis with few complications and facilitates the postoperative rehabilitation. Also, imaging studies may underestimate the severity of articular loss, which may only become evident during arthroscopy and may be better suited for this less-invasive method in the presence of occult advanced disease.
These results compare favorably to outcomes reported with open surgical dislocation including Beck et al. [2], who described 68% successful outcomes with 26% conversion to THA and Murphy et al. [17], who described 65% successful outcomes with 30% conversion to THA. Peters and Erickson did not record the number of successful outcomes but cited only a 13% failure due to conversion or pending conversion to THA [20]. Most recently, Beaulé et al. reported comparable outcomes with their open technique with 82% improved, although they had a 30% reoperation rate related to the surgical approach (ie, screw removal and failure of fixation) [1]. For arthroscopic methods, it is hoped that improved techniques and better understanding of patient selection may lead to more favorable outcomes.
However, as the arthroscopic management is refined, this option may be offered to more marginal candidates in whom the alternatives are limited. Thus, it is difficult to forecast how these results will change with growing experience, but these current data justify its role with current applications.
While cam morphology may be present as an incidental finding, cam impingement is recognized as a causative factor in early age onset osteoarthritis and also a source of substantial disability among young adults with an active lifestyle. Arthroscopy is a useful tool in the assessment and intervention of this disorder. High functional scores can be expected in the majority of patients with low morbidity.
References
Beaulé PE, Le Duff MJ, Zaragoza E. Quality of life following femoral head-neck osteochondroplasty for femoroacetabular impingement. J Bone Joint Surg Am. 2007;89:773–779.
Beck M, Leunig M, Parvizi J, Boutier V, Wyss D, Ganz R. Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop Relat Res. 2004;418:67–73.
Byrd JW. Hip arthroscopy utilizing the supine position. Arthroscopy. 1994;10:275–280.
Byrd JW. Hip arthroscopy: evolving frontiers. Op Tech Orthop. 2004;14:58–67.
Byrd JW, Jones KS. Prospective analysis of hip arthroscopy with two year follow up. Arthroscopy. 2000;16:578–587.
Byrd JW, Jones KS. Prospective analysis of hip arthroscopy with five year follow up. Arthroscopy. 2003;19:88.
Byrd JW, Jones KS. Diagnostic accuracy of clinical assessment, MRI, gadolinium MRI, and intraarticular injection in hip arthroscopy patients. Am J Sports Med. 2004;32:1668–1674.
Byrd JWT. Indications and contraindications. In: Byrd JWT, ed. Operative Hip Arthroscopy. New York, NY: Thieme; 1998:7–24.
Byrd JWT. Arthroscopy of select hip lesions. In: Byrd JWT, ed. Operative Hip Arthroscopy. New York, NY: Thieme; 1998:153–170.
Byrd JWT. The supine approach. In: Byrd JWT, ed. Operative Hip Arthroscopy. 2nd ed. New York, NY: Springer; 2005:145–169.
Byrd JWT. Hip arthroscopy: the supine position. In: Ireland ML, ed. Instructional Course Lectures Sports Medicine. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2005:235–244.
Byrd JWT. Hip morphology and related pathology. In: Johnson DH, Pedowitz RA, ed. Practical Orthopaedic Sports Medicine and Arthroscopy. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:491–503.
Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120.
Garceau GJ. Surgical treatment of coxa plana. J Bone Joint Surg Br. 1964;46:779–780.
Heyman CH, Herndon CH. Slipped femoral epiphysis with severe displacement: a conservative operative treatment. J Bone Joint Surg Am. 1957;39:293–413.
Lavigne M, Parvizi J, Beck M, Siebenrock KA, Ganz R, Leunig M. Anterior femoroacetabular impingement: part I. Techniques of joint preserving surgery. Clin Orthop Relat Res. 2004;418:61–66.
Murphy S, Tannast M, Kim YJ, Buly R, Millis MD. Debridement of the adult hip for femoroacetabular impingement: indications and preliminary clinical results. Clin Orthop Relat Res. 2004;429:178–181.
Myers SR, Eijer H, Ganz R. Anterior femoroacetabular impingement after periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:81–92.
Outerbridge R. Etiology of chondromalacia patella. J Bone Joint Surg Br. 1961;43:752–754.
Peters CL, Erickson JA. Treatment of femoro-acetabular impingement with surgical dislocation and débridement in young adults. J Bone Joint Surg Am. 2006;88:1735–1741.
Smith-Petersen MN. Treatment of malum coxae senilis, old slipped upper femoral epiphysis, intrapelvic protrusion of the acetabulum, and coxa plana by means of acetabuloplasty. J Bone Joint Surg Am. 1936;18:869–880.
Steadman JR, Rodkey WG, Rodrigo JJ. Microfracture: surgical technique and rehabilitation to treat chondral defects. Clin Orthop Relat Res. 2001;391(Suppl):S362–S369.
Stulberg SD, Cordell LD, Harris WH, Ramsey PL, MacEwen GD. Unrecognized childhood hip disease: a major cause of idiopathic osteoarthritis of the hip. In: The Hip: Proceedings of the Third Open Scientific Meeting of the Hip Society. St. Louis, MO: CV Mosby; 1975:212–228.
Vulpius O, Stöffel A. Orthopäadische Operationslehre. Stuttgart, Germany: F. Enke; 1913.
Wright JG, Young NL. A comparison of different indices of responsiveness. J Clin Epidemiol. 1997;50:239–246.
Acknowledgments
We thank Sharon Simmons for her input and diligence in the preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
One of the authors (JWTB) is a consultant for Smith & Nephew Endoscopy, Andover, MA, and has received funding for this study from Smith & Nephew Endoscopy.
Each author certifies that his or her institution has approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
About this article
Cite this article
Byrd, J.W.T., Jones, K.S. Arthroscopic Femoroplasty in the Management of Cam-type Femoroacetabular Impingement. Clin Orthop Relat Res 467, 739–746 (2009). https://doi.org/10.1007/s11999-008-0659-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-008-0659-8