Abstract
Introduction
The concept of femoroacetabular impingement (FAI) and the indication for surgical intervention have been established in the last decade. Despite promising short-term results and emerging arthroscopic techniques, it remains unclear whether patients benefit from surgical correction in the mid- to long-term and whether progressive joint degeneration can be prevented.
Materials and methods
A retrospective study of our first 50 consecutive patients who underwent arthroscopic correction for FAI was conducted. The modified Harris hip score (mHHS) was assessed preoperatively and at final follow-up. In addition, the Western Ontario and McMaster Universities osteoarthritis index (WOMAC) and a subjective hip value (SHV) were added at final follow-up. Degenerative changes according to Kellgren and Lawrence scale and the α angle were analyzed preoperatively and on the most recent radiograph.
Results
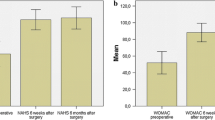
Of a total of 50 patients, 44 (24 male, 20 female) with a mean age of 34.3 years (17–65) were available with complete follow-up. Of these 44 patients, 39 were treated with correction of the femoral offset for isolated cam deformity, 5 with additional focal pincer correction and partial labral resection. After a mean follow-up of 66.3 ± 14.5 months the mHHS had improved significantly from 67.2 ± 6.4 preoperatively to 86.4 ± 13.5 (p < 0.001). The WOMAC score (converted to 0 = best/100 = worst) resulted in mean indices for the subcategories pain, stiffness and function of 11.8 ± 16.5, 12.2 ± 17.8 and 9.1 ± 16.1. The SHV was reported with a mean of 77.7 ± 21.8 % at final follow-up. The α angle was reduced significantly from 57.2° ± 10.1° to 46.3° ± 7.4° (p < 0.001). The Kellgren and Lawrence score showed a non-significant trend from 2.0 ± 0.8 preoperatively to 2.2 ± 0.9 in the most recent radiograph (p = 0.46). 5 patients had been converted to a total hip arthroplasty a mean of 28 ± 7.1 months postoperatively. These patients were significantly (p < 0.01) older with a mean age of 49.8 ± 7.8 years and showed significantly higher present osteoarthritic changes with an average Kellgren and Lawrence score of 2.6 ± 2.5 before FAI correction (p < 0.01).
Conclusions
Arthroscopic correction of femoroacetabular impingement results in a persistent clinical improvement without significant progression of degenerative changes in the majority of patients. The indication for surgery should be established cautiously when degenerative changes are present.
Level of evidence
Level IV, Case series with no comparison group.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The concept of femoroacetabular impingement (FAI) has been increasingly recognized as a cause of hip pain in younger adults, with an estimated overall prevalence of 10–15 % [12, 18, 22, 23]. Damage to the joint occurs due to an aspherity of the femoral neck (cam-type) or a prominent acetabular rim (pincer-type). This impingement conflict can lead to progressive damage to the chondrolabral complex, with subsequent damage to the adjacent articular cartilage, and is therefore considered a risk factor for the development of early hip osteoarthritis (OA) [12, 13, 17, 24]. Radiographic signs of femoroacetabular impingement can be seen in up to 40 % of patients <60 years of age scheduled for total hip replacement due to OA not related to dysplasia, femoral head necrosis, tumor or trauma [24].
Temporary relief of FAI symptoms can be achieved with activity modification and avoidance of end-range of motion, but non-operative treatment cannot eliminate the underlying mechanical problem caused by osseous alterations [9].
Surgical dislocation of the hip as described by Ganz et al. allows treatment of all manifestations of FAI with full access to the joint [2, 11, 32]. However, the dislocation requires an extensive approach, bearing a significantly higher risk for complications, while hip arthroscopy offers a minimally invasive approach with a notably lower complication rate and faster rehabilitation [3, 10, 25, 30].
Initial mid- to long-term studies evaluating surgical dislocation show ongoing improvement for up to 10 years, which is longer follow-up than current arthroscopic studies have obtained [27, 37].
Arthroscopic techniques were first introduced for treatment of cam lesions, but technical improvements have enabled treatment for more complex pathologies, including pincer lesions and labral tears, with favorable short-term results [5, 26, 34, 36].
Despite the favorable short-term results for arthroscopic treatment of FAI in the recent literature, little is known about the mid- to long-term clinical and radiological outcomes. We therefore conducted a retrospective analysis of our first 50 consecutive patients treated by arthroscopic FAI correction with the first hypothesis, that an ongoing improvement of the clinical outcome can be achieved in the mid term. The second hypothesis was that a progression of joint degeneration can be prevented.
Materials and methods
A retrospective study that included all consecutive patients who underwent arthroscopic surgery by the senior author for symptomatic FAI between March 2004 and December 2007 at our institution was conducted. The ethics committee of the medical faculty granted ethical approval for this trial. Written informed consents were obtained from all subjects.
Indications for arthroscopic correction were based on the physical examination in correlation with radiographic findings. Clinical symptoms indicating FAI were activity related pain in the groin unresponsive to non-operative measures (NSAIDs, activity modification and physiotherapy) and associated with a positive anterior impingement test recreating the specific pain when positioning the hip in flexion, adduction and internal rotation [33].
A cam deformity was defined as a loss of sphericity of the femoral head with a reduced head-neck offset and an elevated α angle >50°, as defined by Nötzli [29]. If clinical and radiological findings where ambiguous, an intraarticular anesthetic injection was conducted under fluoroscopic guidance.
Outcomes were measured preoperatively and at final follow-up using the modified Harris hip score (mHHS) [15]. The Western Ontario and McMaster Universities osteoarthritis index (WOMAC, transformed to 0 = best; 100 = worst) was assessed at final follow-up to further evaluate the clinical outcomes [38].
In addition, based on the subjective shoulder value by Gilbart and Gerber, we asked the patients for a similar subjective hip value (SHV) at final follow-up [14]. Similar to the subjective shoulder value, the SHV was defined as a patient’s subjective hip assessment expressed as a percentage of an entirely normal hip, which would score 100 %. All patients routinely received standing AP pelvic and frog-leg lateral views of the affected hip prior to surgery and for follow-up examinations. In addition, conventional magnetic resonance imaging (MRI) or magnetic resonance arthrography (MRA) was performed for further evaluation of the joint configuration and the chondrolabral complex. For evaluation of the osteoarthritic changes, the preoperative and most recent radiograph were compared and graded according to the classification by Kellgren and Lawrence [19]. For analysis of the cam deformity, the α angle according to Nötzli et al. was measured in the frog leg lateral radiograph as described by Clohisy et al. [7, 29]. All radiographs were blinded and analyzed by an independent radiologist at final follow-up.
Surgical technique
Arthroscopy was performed with the patient placed on the traction table in the supine position [8]. In the peripheral compartment and without traction, correction of the cam morphology was performed with reshaping of the head-neck junction by osteochondroplasty. The central compartment was inspected under traction. A capsulotomy was not performed. When the intraoperative findings with focal labral degeneration and a prominent acetabular rim indicated an additional pincer focal conflict, resection of the degenerated labrum and focal rim trimming was conducted.
Rehabilitation
Partial weight bearing of 20 kg on the operated leg using crutches was prescribed for 3 weeks. Physiotherapy with continuous passive motion, core strengthening and manual therapy was started on the first day after surgery. NSAIDs (Indomethacin 25 mg) were administered thrice daily for 21 days to prevent heterotopic ossification.
Patients and physiotherapists were advised to omit strengthening of the hip flexors for 6 weeks postoperatively in order to prevent iliopsoas tendinitis. Furthermore, internal rotation as well as hip flexion over 90° was to be avoided for the first 3 weeks. Cautious sports-specific training was allowed after 3 months.
Statistical analysis
SPSS Statistic v.20 (IBM, Armonk, NY, USA) was used for statistical analysis. The amount of improvement was assessed for statistical significance using the Wilcoxon signed rank test. The significance level was defined at p < 0.05 for all tests. The Mann–Whitney U test was performed for inter-group comparison. Unless otherwise stated, the results are reported as the mean ± standard deviation.
Results
44 of 50 patients were included (88 %), 6 patients went well when contacted by telephone but were not interested in the follow-up study due to private reasons or a long distance to hospital. Apart from complaints while participating in sports, deep hip flexion, ascending stairs and prolonged sitting provoked symptoms most frequently. None of the patients had undergone previous hip surgery. The mean age was 34.3 ± 13.2 years (range 17–65) with 24 male and 20 female patients. In our population the male patients were significantly (p = 0.04) older (38.6 ± 12.3 versus 30.3 ± 14.8 years) and had a significantly higher preoperative α angle of 60.9° ± 9.3° when compared to the female patients with 53.1° ± 9.6° (p = 0.04).
Of these 44 patients, 39 (89 %) were treated with correction of the femoral offset for isolated cam deformity, 5 with additional focal pincer correction and partial labral resection. With regard to complications, there was no incidence of persistent pudendal or perineal nerve injury, avascular necrosis, fracture, venous thromboembolism, infection or intra-abdominal fluid extravasation. 3 patients had documented transient traction-related sensory disorders as minor complications.
At final follow-up after a mean of 66.3 ± 14.5 months (range 43–87, median 67.0 months), the modified Harris hip score (mHHS) had improved significantly (p < 0.001) from 67.2 ± 6.4 (range 58–76) preoperatively to 86.4 ± 13.5 (range 69–100). The evaluation of the WOMAC score (converted to 0 = best/100 = worst) at final follow-up resulted in mean indices for the subcategories pain 11.8 ± 16.5 (range 0–68), stiffness 12.2 ± 17.8 (range 0–60) and function 9.1 ± 16.1 (range 0–61). The SHV was estimated by the patients at final follow-up with a mean of 77.7 ± 21.8 % (range 30–100 %) when compared to 100 % in an unimpaired hip joint (Table 1).
Radiographs after surgery were available from 38 patients (Table 1) with a mean follow-up of 36.6 ± 24.6 months (range 12–70 months). The α angle was reduced significantly (p < 0.001) from 57.2° ± 10.1° (range 52°–85°) to 46.3 ± 7.4 (range 38°–63°). The mean Kellgren and Lawrence score for OA showed a non-significant increase (p = 0.46) from 2.0 ± 0.8 (range 0–3) preoperatively to 2.2 ± 0.9 (range 0–3) in last available radiograph. In one patient (2.3 %), follow-up radiographs revealed asymptomatic heterotopic ossifications type II according to Brooker [4].
5 patients underwent secondary surgery for total hip arthroplasty a mean of 28 months ± 7.1 (range 12–56) after the arthroscopic surgery for FAI. These patients were significantly older (p < 0.01) with a mean age of 49.8 ± 7.8 years (range 42–62) when compared to the other patients with 33.0 ± 13.2 years (range 17–65) who did not undergo further surgery. The level of already present osteoarthritic changes preoperatively was significantly (p < 0.01) higher with a mean Kellgren and Lawrence score of 2.6 ± 2.5 (range 2–3) preoperatively in comparison to 2.0 ± 0.7 (range 0–3) in the patients who completed follow-up (Table 1).
Discussion
Despite published promising early results of arthroscopic surgery for femoroacetabular impingement, the benefit in the mid- to long-term and the possibilities for prevention of progressive joint degeneration remain unclear [1, 5, 20, 28, 31, 34, 35]. We were able to demonstrate that encouraging short-term results are maintained in the mid-term, with a clinical improvement 5.5 years after arthroscopic correction of cam- and mixed-type FAI.
Persistent clinical improvement implies that the patients have continued to improve over the entire postoperative period, rather than maintain their level of improvement compared to before surgery.
The HHS is a long-established outcome instrument for hip associated disorders. Nevertheless, concerns have been expressed that this score, initially having been developed for the evaluation of OA, contains a ceiling effect when it comes to a young, active and demanding patient population due to its limited number of challenging items [6, 39]. Therefore, we also asked for the SHV, which can reflect the patients’ satisfaction with their hip function and depends only on their preferences and expectations.
Our results are comparable to the studies with a considerably shorter follow-up on arthroscopic surgery for FAI. Byrd et al. evaluated patients with a minimum follow-up of 24 months, showing a mean improvement of 21 points in the mHHS [5], Philippon et al. showed an improvement of 24 points in the average after 28 months, and Larsson et al. demonstrated an average increase of 21 points after 31 months [20, 34].
Our results show a 10.8 % conversion rate to THA an average of 28 months after FAI correction. Those 5 patients were significantly older and had significantly more advanced degenerative changes preoperatively compared to the 39 patients who completed follow-up.
Horisberger et al. published a retrospective study on 20 patients with an average age of 47 years who underwent arthroscopic FAI correction with advanced degenerative changes. Similarly to our results, the presence of degenerative changes increased the risk of subsequent THA significantly, with a mean of 1.4 years between FAI correction and THA [16].
Larson et al. compared 154 patients (169 hips) without radiographic joint space narrowing to 56 patients (58 hips) with preoperative radiographic joint space narrowing after a mean follow-up of 27 months. The failure rate, defined as an mHHS < 70 or conversion to THA, was 52 % in the cohort with degenerative changes compared to 12 % in the cohort without signs of OA preoperatively [21].
Our results are in line with the literature and indicate that patients with existing degenerative changes do not benefit in the mid- to long-term from arthroscopic FAI correction. The comparably long follow-up period and the comprehensive clinical and radiological follow-up using well-established scores are the strong points of this study. The retrospective study design and a possible bias in the selection of the patient population due to the limited arthroscopic surgical techniques at this time are limitations that have to be considered. The new subjective hip value is an additional tool for outcome evaluation but has not been validated yet. Recently published tailored outcome tools for the specific evaluation of younger and active FAI patients are now available but can limit comparison to results of earlier studies.
In conclusion, we were able to show that arthroscopic correction of femoroacetabular impingement results in a persistent favorable clinical and radiological outcome in the majority of patients a mean of 5.5 years after surgery. One must bear in mind that patients with existing degenerative changes do not benefit in the mid- to long-term and that, despite FAI correction, progression of OA with an indication for THA may then be inevitable.
References
Bardakos NV, Vasconcelos JC, Villar RN (2008) Early outcome of hip arthroscopy for femoroacetabular impingement: the role of femoral osteoplasty in symptomatic improvement. J Bone Joint Surg Br 90:1570–1575
Beck M, Siebenrock KA, Affolter B, Notzli H, Parvizi J, Ganz R (2004) Increased intraarticular pressure reduces blood flow to the femoral head. Clin Orthop Relat Res 424:149–152
Botser IB, Jackson TJ, Smith TW, Leonard JP, Stake CE, Domb BG (2014) Open surgical dislocation versus arthroscopic treatment of femoroacetabular impingement. Am J Orthop 43:209–214
Brooker AF, Bowerman JW, Robinson RA, Riley LH (1973) Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am 55:1629–1632
Byrd JW, Jones KS (2011) Arthroscopic management of femoroacetabular impingement: minimum 2-year follow-up. Arthroscopy 27:1379–1388
Chahal J, Van Thiel GS, Mather RC, Lee S, Song SH, Davis AM, Salata M, Nho SJ (2015) The patient acceptable symptomatic state for the modified Harris Hip Score and hip outcome score among patients undergoing surgical treatment for femoroacetabular impingement. Am J Sports Med 43:1844–1849
Clohisy JC, Nunley RM, Otto RJ, Schoenecker PL (2007) The frog-leg lateral radiograph accurately visualized hip cam impingement abnormalities. Clin Orthop Relat Res 462:115–121
Dienst M, Gödde S, Seil R, Hammer D, Kohn D (2001) Hip arthroscopy without traction: in vivo anatomy of the peripheral hip joint cavity. Arthroscopy 17:924–931
Emara K, Samir W, el Motasem H, Ghafar KA (2011) Conservative treatment for mild femoroacetabular impingement. J Orthop Surg 19:41–45
Fink B, Sebena P (2010) Treatment of femoroacetabular impingement using a minimally invasive anterior approach. Oper Orthop Traumatol 22:17–27
Ganz R, Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U (2001) Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br 83:1119–1124
Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA (2003) Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res 417:112–120
Ganz R, Leunig M, Leunig-Ganz K, Harris WH (2008) The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res 466:264–272
Gilbart MK, Gerber C (2007) Comparison of the subjective shoulder value and the Constant score. J Shoulder Elbow Surg 16:717–721
Harris WH (1969) Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 51:737–755
Horisberger M, Brunner A, Valderrabano V, Herzog RF (2010) Femoroacetabular impingement of the hip in sports—a review for sports physicians. Sportverletz Sportschaden Germany 24:133–139
Ipach I, Mittag F, Syha R, Kunze B, Wolf P, Kluba T (2012) Indications for total hip arthroplasty in young adults—idiopathic osteoarthritis seems to be overestimated. Rofo 184:239–247
Ito K, Minka MA, Leunig M, Werlen S, Ganz R (2001) Femoroacetabular impingement and the cam-effect. A MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br 83:171–176
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16:494–502
Larson CM, Giveans MR (2008) Arthroscopic management of femoroacetabular impingement: early outcomes measures. Arthroscopy 24:540–546
Larson CM, Kelly BT, Stone RM (2011) Making a case for anterior inferior iliac spine/subspine hip impingement: three representative case reports and proposed concept. Arthroscopy 27:1732–1737
Leunig M, Beck M, Dora C, Ganz R (2005) Femoroacetabular impingement: etiology and surgical concept. Oper Tech Orthop 15:247–255
Leunig M, Beck M, Dora C, Ganz R (2006) Femoroacetabular impingement: trigger for the development of coxarthrosis. Orthopade 35:77–84
Lung R, O’Brien J, Grebenyuk J, Forster BB, De Vera M, Kopec J, Ratzlaff C, Garbuz D, Prlic H, Esdaile JM (2012) The prevalence of radiographic femoroacetabular impingement in younger individuals undergoing total hip replacement for osteoarthritis. Clin Rheumatol 31:1239–1242
Matsuda DK, Carlisle JC, Arthurs SC, Wierks CH, Philippon MJ (2011) Comparative systematic review of the open dislocation, mini-open, and arthroscopic surgeries for femoroacetabular impingement. Arthroscopy 27:252–269
Matsuda DK, Gupta N, Hanami D (2014) Hip arthroscopy for challenging deformities: global pincer femoroacetabular impingement. Arthrosc Tech 3:e197–e204
Naal FD, Miozzari HH, Schär M, Hesper T, Nötzli HP (2012) Midterm results of surgical hip dislocation for the treatment of femoroacetabular impingement. Am J Sports Med 40:1501–1510
Nielsen TG, Miller LL, Lund B, Christiansen SE, Lind M (2014) Outcome of arthroscopic treatment for symptomatic femoroacetabular impingement. BMC Musculoskelet Disord 15:394
Nötzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J (2002) The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br 84:556–560
Nwachukwu BU, Rebolledo BJ, McCormick F, Rosas S, Harris JD, Kelly BT (2015) Arthroscopic versus open treatment of femoroacetabular impingement: a systematic review of medium- to long-term outcomes. Am J Sports Med [Epub ahead of print]
Palmer DH, Ganesh V, Comfort T, Tatman P (2012) Midterm outcomes in patients with cam femoroacetabular impingement treated arthroscopically. Arthroscopy 28:1671–1681
Peters CL, Erickson JA (2006) Treatment of femoro-acetabular impingement with surgical dislocation and débridement in young adults. J Bone Joint Surg Am 88:1735–1741
Philippon MJ, Stubbs AJ, Schenker ML, Maxwell RB, Ganz R, Leunig M (2007) Arthroscopic management of femoroacetabular impingement: osteoplasty technique and literature review. Am J Sports Med 35:1571–1580
Philippon MJ, Briggs KK, Yen YM, Kuppersmith DA (2009) Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction: minimum two-year follow-up. J Bone Joint Surg Br 91:16–23
Philippon MJ, Schroder E, Souza BG, Briggs KK (2012) Hip arthroscopy for femoroacetabular impingement in patients aged 50 years or older. Arthroscopy 28:59–65
Redmond JM, El Bitar YF, Gupta A, Stake CE, Domb BG (2014) Arthroscopic acetabuloplasty and labral refixation without labral detachment. Am J Sports Med 43:105–112
Steppacher SD, Anwander H, Zurmühle CA, Tannast M, Siebenrock KA (2015) Eighty percent of patients with surgical hip dislocation for femoroacetabular impingement have a good clinical result without osteoarthritis progression at 10 years. Clin Orthop Relat Res 473:1333–1341
Stucki G, Meier D, Stucki S, Michel BA, Tyndall AG, Dick W, Theiler R (1996) Evaluation of a German version of WOMAC (Western Ontario and McMaster Universities) Arthrosis Index. Z Rheumatol 55:40–49
Wamper KE, Sierevelt IN, Poolman RW, Bhandari M, Haverkamp D (2010) The Harris hip score: do ceiling effects limit its usefulness in orthopedics? Acta Orthop 81:703–707
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Hufeland, M., Krüger, D., Haas, N.P. et al. Arthroscopic treatment of femoroacetabular impingement shows persistent clinical improvement in the mid-term. Arch Orthop Trauma Surg 136, 687–691 (2016). https://doi.org/10.1007/s00402-016-2427-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-016-2427-7