Abstract
The use of bioabsorbable pins with prolonged degradation periods for fracture fixation has raised concerns about adverse soft tissue reactions, including seromas, discharging sinuses, or osteolytic changes. We asked whether bioabsorbable pins of self-reinforced polylactic acid polymer used in radial head fractures resulted in such reactions. We retrospectively reviewed 21 patients followed a minimum of 36 months (mean, 81 months; range, 36–136 months). There were nine Mason II, 10 Mason III, and two Mason IV fractures, which were evaluated clinically and radiographically. All fractures healed well with no radiographic signs of osteolysis. The mean Mayo Elbow Performance score was 93.8 (range, 20–100), which is comparable to the outcome of historical groups with radial head arthroplasty. The mean range of flexion of the elbow was 9° to 132°, with 79° pronation and 77° supination. The grip strength of the operated arm was not affected in comparison to the contralateral arm (mean range, 38.6 versus 40.9 kg). No material-related adverse effects were observed during and beyond the degradation period. Our data suggest concerns about soft tissue or bony reactions from these materials in radial head fractures are not justified.
Level of Evidence: Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The best method for treating displaced radial head fractures in adults remains controversial [6, 7, 12]. The decision regarding whether the fractured head is salvageable by means of internal fixation is largely based on subjective criteria, including the surgeon’s experience and preference and the equipment available. Whereas radial head replacement is gaining popularity, there is little doubt a salvageable and properly fixed radial head provides the best option for a long-term functional outcome [2, 7, 15].
Various metallic implants are being used for operative fixation of radial head fractures, including minifragment screws, Kirschner wires, Herbert screws, and miniplates [10, 13, 19]. However, during the last two decades, bioabsorbable pins have been introduced to treat radial head fractures [9, 21, 26]. Their widespread acceptance has been hampered partly by reports regarding soft tissue reactions during the fast degradation process and suboptimal mechanical properties of these implants [4, 24]. Second-generation implants composed of self-reinforced (SR) poly-L-lactic acid (PLLA) with improved strength and a slower degradation rate were intended to eliminate these drawbacks and apparently did so [22, 24, 25].
Nevertheless, the prolonged degradation period of the new implants has raised continuing concerns regarding whether the adverse soft tissue reactions of these materials are in fact not diminished but rather take longer to appear [3]. The strength of SR-PLLA rods decreases to the level of cancellous bone in 36 weeks, but total loss of implant mass takes much longer [11, 30]. Remnants of SR-PLLA plates have been detected as long as 5 years after fixation of mandibular osteotomies in sheep [28]. This necessitates clinical studies with a long followup [4, 23].
Furthermore, such studies need to focus on the clinical outcome of comminuted radial head fractures in particular. Recently published series underline the substantial controversy regarding the role of open reduction internal fixation (ORIF) versus arthroplasty for Mason Type III and Type IV fractures [15, 27]. Although some authors consider severe comminution an absolute indication for replacement of the radial head, advocates of the ORIF claim favorable clinical outcomes regardless of the fracture’s complexity [6, 29].
We asked whether adverse reactions, such as seroma formation, discharging sinuses, or osteolytic reactions, would occur during and beyond the material’s degradation period. We then asked whether patients would achieve reasonable functional scores and whether function scores related to fracture type (Mason classification [16]), age, or length of followup.
Materials and Methods
From a group of 68 patients admitted with closed radial head fractures, we retrospectively reviewed 25 selected patients treated with ORIF with absorbable pins from September 1995 until February 2004. We included only Grades II to IV fractures according to the McKee and Jupiter modification [17] of the Mason classification [16] and surgery in the first 48 hours after the traumatic event. We excluded 23 patients for whom we judged salvage of the radial head by internal fixation was impractical. Another 20 patients were treated by other means of ORIF (screws, Kirschner wires, miniplates) and also were excluded from the study. Two of the 25 patients were lost to followup, leaving 23 for evaluation. There were 12 men and nine women with an average age at the time of surgery of 37.8 years (range, 18–78 years; Table 1). All fractures were secured with the use of SR-PLLA pins (SmartPin®; formerly Bionx Implants Oy, now ConMed Livantec Biomaterials Ltd, Tampere, Finland). The clinical outcome was assessed and compared with two historical groups using radial head arthroplasty [2, 18]. The minimum followup was 36 months (median, 97 months; range, 36–136 months).
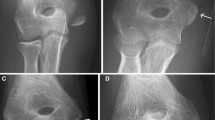
All operations were performed by the senior author (PKG). With the patient supine, under axillary block or general anesthesia, and the use of a pneumatic tourniquet, a straight lateral 5- to 6-cm incision was made over the radial head and through a modified Kocher approach and the fracture was identified. We reduced the major fragments with the aid of the convex surface of a McDonald instrument and temporarily secured them with miniclamps. Smaller fragments were reduced and compressed in position manually. We used pronation/supination maneuvers during the reduction process. The fractures were fixed by two to five predrilled pins (Fig. 1). When the fracture included the head only, we inserted the pins parallel to the joint line. When the fracture included the subcapital region, additional pins were inserted obliquely to the axis of the joint line. In one case, we removed the comminuted head from the surgical site, fixed it ex situ with bioabsorbable pins, and reinserted and attached it to the radial neck with long (40-mm length) pins in an oblique direction. Any protruding part of the pins was cut flat at the bone level with a Number 15 blade. We fixed the major fragments with 1.5- to 2.0-mm pins of 20- to 30-mm length. Smaller fragments were either fixed with 1.1-mm pins or packed manually. Stability and range of motion were tested intraoperatively. When present, concomitant lateral ligament injuries were repaired primarily with bone anchors. The wound was closed in layers over a drain and we obtained a postoperative radiograph.
Postoperatively, an above-elbow posterior splint was applied for up to 2 weeks followed by early mobilization. A strengthening program was initiated 4 weeks postoperatively, including active-assisted and active free weights and wall pulley exercises.
We performed complete clinical and radiographic evaluations in 21 of the 23 patients; two patients were interviewed over the telephone. Patients were interviewed and examined by one of two independent observers (PDS, PSD) who did not participate in any of the operations. All possible adverse effects and complications were recorded. We evaluated the functional outcome according to the Mayo Elbow Performance score [20]. This continuous score combines four criteria: pain, motion, stability, and function of the affected elbow. The ranges of motion of the affected and contralateral elbow also were recorded separately. Grip strengths of the affected and the contralateral arm were measured with a hydraulic hand dynamometer (Jamar®; Nex Gen Ergonomics Inc, Quebec, Canada).
We (PKG, AGC) retrospectively reclassified the injuries; in case of discrepancy, final assessment was based on concurrence. In four of the 25 cases, some of the radiographs were of poor quality or missing from the patients’ files. The radiographic evaluation included plain radiographs in anteroposterior and lateral views in all patients (Fig. 2).
(A) An anteroposterior radiograph shows a Mason Type III fracture of the radial head. (B) The lateral radiograph of the same patient shows the fracture’s comminution. (C) A postoperative radiograph obtained at the final followup shows successful reconstruction of the radial head. (D) A postoperative lateral radiograph shows fracture union and satisfactory alignment of the radiohumeral joint.
Categorical variables were presented with frequencies and percentages. Continuous variables were summarized with means and 95% confidence intervals and with median and interquartile ranges whenever the data were not normally distributed. The grip strengths of the affected and the normal elbow were compared with the Wilcoxon signed-rank test for paired samples. Data of two published series of patients with radial head fractures treated with arthroplasty (titanium prosthesis and metal radial heads) were extracted and compared with data from our sample of patients [2, 18].
We evaluated the association of categorical variables (gender distribution and Mason type between groups) with the chi square test or Fisher’s exact test when the expected marginal cell count was less than five. Differences in clinical scores and in variables on range of motion between groups (Mason II and Mason III to IV fracture types) were assessed with either Student’s t test for unpaired samples or the Mann-Whitney U test whenever the variables deviated from normality; tests were two-tailed. The age and followup times of the two groups were similar. Analyses were conducted using SPSS 14 (SPSS Inc, Chicago, IL).
Results
We observed no early or late occurrences of clinically evident seroma formation, discharging sinus over the fracture site, or osteolytic changes of the radial head in any patient. For 15 of the 21 patients, the followup exceeded 5 years, which is the maximum degradation period of the specific implant.
The median Mayo Elbow Performance score was 93.8 (range, 20–100; Table 1). Three patients with a score of 85 had mild pain on activity. The mean range of flexion of the elbow was 9° to 132°, with 79° pronation and 77° supination. The grip strength of the surgically treated arm was not affected in comparison to the contralateral arm (mean range, 38.6 versus 40.9 kg). One patient with a poor result had a fixed flexion deformity resulting from a complete bony bridge of heterotopic ossification at the medial side of the elbow despite the full pronation/supination range of motion. He was offered and accepted soft tissue release and removal of the heterotopic ossification with improvement of the range of motion from 30° to 120°. No other patient underwent a second operation. The two patients interviewed over the telephone reported no pain or alteration of their activities resulting from the fracture.
Fracture severity did not correlate with clinical outcome (Table 1). The median Mayo score was 100 for Mason II and Mason III to IV fracture type groups. Range of motion was similar for the Mason II and Mason III-IV groups (mean flexion 130° versus 134°, respectively). Pronation and supination were also similar (Table 2).
We identified no major complications. One patient had a superficial postoperative infection resulting from Staphylococcus epidermidis, which was treated successfully with oral antibiotics. One patient had residual moderate instability. Two cases of radiographically apparent heterotopic ossification were seen, one over the annular ligament without any functional impairment and another over the medial aspect of the elbow with a fixed flexion contracture (mentioned above). The latter patient had not adhered to the routine rehabilitation protocol, having prolonged the immobilization period arbitrarily followed by aggressive physiotherapy. On the postoperative films of four patients, we observed a step-off between the fragments of as much as 1.5 mm although the patients appeared to have no clinical sequelae.
Discussion
Qualities of an ideal fixation material include adequate strength and rigidity, lack of adverse reactions, lack of interference with bone healing, lack of visibility and palpability, and avoidance of an implant removal operation. Early reports of adverse effects in fracture fixation from the use of bioabsorbable materials mainly composed of polyglycolide acid (PGA) have led to the development of new implants with a longer degradation period, such as the SR-PLLA. However, this has raised additional concerns regarding the possible late occurrence of such reactions. We therefore asked whether adverse reactions, such as seroma formation, discharging sinuses, or osteolytic reactions, would occur during and beyond the material’s degradation period.
We did not have a control group with which we could compare functional outcomes of alternative approaches in the long term. Rather, we compared our results with published results of historical groups in which the same type of fractures was treated and the same score was used for assessment of elbow function. Another limitation is the inclusion of Mason Type II fractures in our study group. According to some studies, these injuries may yield a good clinical outcome by nonoperative treatment [1, 31] or delayed head excision in selected patients [5]. However, we agree with Morrey [19] that because today’s patients demand a greater degree of function, internal fixation of radial head fractures is being widely used for Type II fractures. Moreover, a mismatch between radiographic and intraoperative evaluations of these fractures, the latter always being more severe, was noted in some of our cases. Regardless, we found fracture severity did not correlate with outcome in our series and this agrees with the study by Koslowsky et al. [15].
Previous studies suggest, among the various clinical applications of bioabsorbable implant for fracture fixation, their use in radial head fractures seems to have the most benign clinical course. Böstman and Pihlajamäki [4] reviewed 2528 patients in whom such implants were used in more than 20 applications. They report patients with radial head fractures had the lowest adverse reaction in their series (0.3%), which is in conformity with our series. This has been partly attributed to an inverse association between vascularity of the local tissues and the implant’s reaction rate. Recently, a prospective, randomized study was published [8] in which bioabsorbable polylactide implants were compared with standard metal fixation for treatment of displaced radial head fractures. The authors report equally satisfactory results for both methods; however, their followup is limited to 2 years, whereas material-related foreign body reactions can emerge as late as 4 or 5 years after the original surgery for fracture fixation [3, 4]. Our data confirm these favorable results until and beyond the complete absorption of this implant. Another bioabsorbable material that has been used is PGA [9, 21]. This material lacks a methyl group, which makes it hydrophilic and thus more susceptible to hydrolysis and faster degradation than polylactide, usually within 6 months after insertion [24]. It has been reported to have a high incidence of soft tissue reactions varying from 2.0% to 46.7%, which created skepticism regarding its clinical application [4].
We are unaware of reports of delayed adverse effects from using SR-PLLA pins. Polylactic acid is a derivative of cyclic diesters of lactic acid from which it has been produced by ring-opening polymerization resulting in a poly-alpha-hydroxy derivative of the original acid. The methyl group makes polylactic acid hydrophobic and is thus resistant to hydrolysis [22]. Its mechanical in vitro degradation time is 9 months, and animal studies show complete resorption of SR-PLLA implants within 5 years [8, 14]. The SR technique strengthens the polymer and gives it metal-like mechanical properties without influencing the degradation process.
Our data using an absorbable pin fixation group suggest favorable outcomes compared with use of a titanium prosthesis in Mason Type III radial head fractures (Tables 3, 4) [2, 18]. The followup was longer in our absorbable pin fixation group than in the reported arthroplasty groups. Compared with the study by Ashwood et al. [2], flexion and Mayo score were greater in the absorbable pin fixation group than in the titanium prosthesis group. Compared with the study by Moro et al. [18], there were no differences between the two groups with respect to flexion, loss of extension, supination, or pronation. However, the Mayo score was greater in our absorbable pin fixation group than in the titanium prosthesis group.
We consider the midterm outcome of internal fixation of displaced radial head and neck fractures with PLLA pins satisfactory in our series. This was documented by a combination of subjective and objective clinical criteria, such as pain, range of motion, alignment, stability, and grip strength of the affected arm.
Our results were superior to those of published series in which the comminuted fractures were treated with metallic replacement [2, 18]. Although a recent comparative study favors the bipolar radial head prosthesis versus ORIF for treatment of Mason Type III fractures, the followup is rather short for definite conclusions [27]. The preferential use of either ORIF or replacement for comminuted radial head fractures continues to cause debate and controversy. Whereas the exact clinical and radiographic criteria that dictate the decision for a head sacrifice have not yet been established [29], some authors believe, even in comminuted fractures, an initial attempt for internal fixation should be made; we agree with this concept [6, 12, 15]. In any case, the surgeon should be prepared for any operation, including radial head sacrifice or replacement, and the final decision should be made intraoperatively.
The use of bioabsorbable pins in the treatment of radial head fractures has yielded satisfactory midterm clinical and radiographic outcomes. Concerns about soft tissue reactions from the use of these materials in radial head fractures are not justified according to our results, having overcome the maximum degradation period.
References
Akesson T, Herbertsson P, Josefsson PO, Hasserius R, Besjakov J, Karlsson MK. Primary nonoperative treatment of moderately displaced two-part fractures of the radial head. J Bone Joint Surg Am. 2006;88:1909–1914.
Ashwood N, Bain GI, Unni R. Management of Mason type-III radial head fractures with a titanium prosthesis, ligament repair, and early mobilization. J Bone Joint Surg Am. 2004;86:274–280.
Böstman O, Pihlajamäki H. Clinical biocompatibility of biodegradable orthopaedic implants for internal fixation: a review. Biomaterials. 2000;21:2615–2621.
Böstman OM, Pihlajamäki HK. Adverse tissue reactions to bioabsorbable fixation devices. Clin Orthop Relat Res. 2000;371:216–227.
Broberg MA, Morrey BF. Results of delayed excision of the radial head after fracture. J Bone Joint Surg Am. 1986;68:669–674.
Esser RD, Davis S, Taavao T. Fractures of the radial head treated by internal fixation: late results in 26 cases. J Orthop Trauma. 1995;9:318–323.
Furry KL, Clinkscales CM. Comminuted fractures of the radial head: arthroplasty versus internal fixation. Clin Orthop Relat Res. 1998;353:40–52.
Helling HJ, Prokop A, Schmid HU, Nagel M, Lilienthal J, Rehm KE. Biodegradable implants versus standard metal fixation for displaced radial head fractures: a prospective, randomized, multicenter study. J Shoulder Elbow Surg. 2006;15:479–485.
Hirvensalo E, Böstman O, Rokkanen P. Absorbable polyglycolide pins in fixation of displaced fractures of the radial head. Arch Orthop Trauma Surg. 1990;109:258–261.
Hotchkiss RN. Displaced fractures of the radial head: internal fixation or excision? J Am Acad Orthop Surg. 1997;5:1–10.
Hughes TB. Bioabsorbable implants in the treatment of hand fractures: an update. Clin Orthop Relat Res. 2006;445:169–174.
Ikeda M, Sugiyama K, Kang C, Takagaki T, Oka Y. Comminuted fractures of the radial head: comparison of resection and internal fixation. Surgical technique. J Bone Joint Surg Am. 2006;88(suppl 1 pt 1):11–23.
Josten C, Korner J, Lill H. Radiusköpfchenfrakturen In: Josten C, Lill H, eds. Ellenbogen Verletzungen: Biomechanik, Diagnose, Therapie. Heidelberg, Germany: Steinkopf Verlag; 1997:137–149.
Jukkala-Partio K, Pohjonen T, Laitinen O, Partio EK, Vasenius J, Toivonen T, Kinnunen J, Törmälä P, Rokkanen P. Biodegradation and strength retention of poly-L-lactide screws in vivo: an experimental long-term study in sheep. Ann Chir Gynaecol. 2001;90:219–224.
Koslowsky TC, Mader K, Gausepohl T, Pennig D. Reconstruction of Mason type-III and type-IV radial head fractures with a new fixation device: 23 patients followed 1–4 years. Acta Orthop. 2007;78:151–156.
Mason ML. Some observations on fractures of the head of the radius with a review of one hundred cases. Br J Surg. 1954;42:123–132.
McKee MD, Jupiter JB. A contemporary approach to the management of complex fractures of the distal humerus and their sequelae. Hand Clin. 1994;10:479–494.
Moro JK, Werier J, MacDermid JC, Patterson SD, King GJ. Arthroplasty with a metal radial head for unreconstructible fractures of the radial head. J Bone Joint Surg Am. 2001;83:1201–1211.
Morrey BF. Radial head fracture. In: Morrey BF, ed. The Elbow and its Disorders. 3rd ed. Philadelphia, PA: Saunders; 2000:341–364.
Morrey BF, Adams RA. Semiconstrained arthroplasty for the treatment of rheumatoid arthritis of the elbow. J Bone Joint Surg Am. 1992;74:479–490.
Pelto K, Hirvensalo E, Böstman O, Rokkanen P. Treatment of radial head fractures with absorbable polyglycolide pins: a study on the security of the fixation in 38 cases. J Orthop Trauma. 1994;8:94–98.
Peltoniemi HH, Hallikainen D, Toivonen T, Helevirta P, Waris T. SR-PLLA and SR-PGA miniscrews: biodegradation and tissue reactions in the calvarium and dura mater. J Craniomaxillofac Surg. 1999;27:42–50.
Prokop A, Jubel A, Hahn U, Dietershagen M, Bleidistel M, Peters C, Höfl A, Rehm KE. A comparative radiological assessment of polylactide pins over 3 years in vivo. Biomaterials. 2005;26:4129–4138.
Prokop A, Jubel A, Helling HJ, Eibach T, Peters C, Baldus SE, Rehm KE. Soft tissue reactions of different biodegradable polylactide implants. Biomaterials. 2004;25:259–267.
Prokop A, Jubel A, Helling HJ, Udomkaewkanjana C, Brochhagen HG, Rehm KE. [New biodegradable polylactide implants (Polypin-C) in therapy for radial head fractures] [in German]. Chirurg. 2002;73:997–1004.
Rehm KE, Helling HJ, Gatzka C. [New developments in the application of resorbable implants] [in German]. Orthopade. 1997;26:489–497.
Ruan HJ, Fan CY, Liu JJ, Zeng BF. A comparative study of internal fixation and prosthesis replacement for radial head fractures of Mason type III. Int Orthop. 2007 Oct 16 [Epub ahead of print].
Suuronen R, Pohjonen T, Hietanen J, Lindqvist C. A 5-year in vitro and in vivo study of the biodegradation of polylactide plates. J Oral Maxillofac Surg. 1998;56:604–614; discussion 614–605.
Tejwani NC, Mehta H. Fractures of the radial head and neck: current concepts in management. J Am Acad Orthop Surg. 2007;15:380–387.
Waris E, Ashammakhi N, Kaarela O, Raatikainen T, Vasenius J. Use of bioabsorbable osteofixation devices in the hand. J Hand Surg Br. 2004;29:590–598.
Weseley MS, Barenfeld PA, Eisenstein AL. Closed treatment of isolated radial head fractures. J Trauma. 1983;23:36–39.
Acknowledgments
We thank Bettina Haidich for assistance with statistical analysis of the data.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution either has waived or does not require approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
About this article
Cite this article
Givissis, P.K., Symeonidis, P.D., Ditsios, K.T. et al. Late Results of Absorbable Pin Fixation in the Treatment of Radial Head Fractures. Clin Orthop Relat Res 466, 1217–1224 (2008). https://doi.org/10.1007/s11999-008-0134-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-008-0134-6