Abstract
Combined segmental and cavitary deficiencies of the acetabulum (American Academy of Orthopaedic Surgeons Type III) are a difficult problem that revision arthroplasty surgeons must tackle with increasing frequency. Porous-coated bilobed acetabular components are a reconstruction option that allows for increased host bone-prosthesis contact with restoration of the anatomic hip center without the use of a structural bone graft. Eleven consecutive Type III acetabular defects in 11 patients were revised with a porous-coated bilobed cup without a structural bone graft between January 1999 and January 2001 and prospectively followed. Average Harris hip scores improved from 36 preoperatively to 85 postoperatively. Radiographic analysis showed improvement in the average vertical displacement of the hip center. Average leg length discrepancies decreased from 34 mm preoperatively to 7 mm postoperatively. There have been no revisions performed or planned. Porous-coated bilobed acetabular components can provide good clinical and radiographic results at intermediate followup for treatment of Type III acetabular deficiencies. Bilobed components offer a viable option for reconstruction of Type III defects without the use of a structural bone graft or cement while maximizing the host bone-implant contact and restoring the native hip center.
Level of Evidence: Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Massive deficiencies in acetabular bone stock often are encountered in revision total hip surgery [1, 10, 12]. Options to deal with this bone loss include impaction grafting [3], structural bone grafting [12, 15, 19], and the use of cement with or without acetabular cages and rings [1]. These methods run the risk of early failure because a considerable portion of the acetabular component is not fixed onto host bone [15, 20]. More recently, some surgeons have started to use modular tantalum shells and augments to address bone loss; however, the durability of these implants remains to be validated [22, 30]. In the senior author’s (JTM) experience, the loosening rate for combined cavitary and segmental pelvic defects, American Academy of Orthopaedic Surgeons Type III, reconstructed by hemispheric cups and structural bone grafts have been high (33%) [20]. This is similar to reported rates of 24% to 47% [10, 12, 15, 17, 24, 25, 27].
Acetabular reconstruction without cement and bone graft in cases with extensive bone loss often requires use of a jumbo cup [7, 31] or placement of a smaller cup higher in the pelvis [25, 27]. Although avoiding the use of a structural bone graft and cement, both methods fail to restore the hip center to a more anatomic position [2] and jumbo cups risk additional bone loss from the anterior and/or posterior column.
Bilobed acetabular components maximize host bone-implant contact while restoring the native hip center without a structural bone graft or cement. The design attempts to allow support of the prosthesis entirely on host bone while restoring the anatomic hip center.
Studies on the use of bilobed components are limited and results are mixed [2, 5, 8]. Although recommended for segmental (Type II) defects and on rare occasions useful for large cavitary (Type I) defects, they are not routinely recommended for combined segmental and cavitary (Type III) defects [2, 5, 7]. The purpose of this study was to prospectively follow patients who had the exclusive use of bilobed cups in revision hip arthroplasties with Type III defects without the use of structural bone graft or cement.
In a previous study, the early (2-year) outcomes of this cohort of patients were encouraging with considerable improvement in function and pain relief without the need for revision [21]. This longer-term investigation is directed at establishing if bilobed acetabular components remain a viable treatment option for Type III acetabular defects based on intermediate followup. Specifically, did the clinical improvement in pain and function persist or deteriorate? Were the radiographic improvements in leg length, component position, and ingrowth maintained?
Materials and Methods
From January 1999 to January 2001, the senior author (JTM) performed 68 revision hip arthroplasties (THAs) in 64 patients. All acetabular deficiencies were classified based on plain radiographs (anteroposterior pelvis and Judet views) according to the American Academy of Orthopaedic Surgeons system [6]. In this period, all patients with combined segmental and cavitary (Type III) acetabular defects in which restoration of the anatomic hip center could not be achieved with a hemispheric cup without the use of a structural bone graft, cement, and/or an acetabular reconstruction cage were revised using a bilobed component, the S-ROM Oblong Cup (Depuy, Johnson and Johnson, Warsaw, IN) without a structural bone graft. There were 11 hips in 11 patients that met the inclusion criteria for this study. We prospectively followed patients clinically and radiographically for a minimum of 60 months (mean, 72 months; range, 60–84 months) after the index surgery. No patients were lost to followup. One patient died of causes unrelated to the revision hip arthroplasty before 5 years followup. This patient had a good result clinically and radiographically at the latest followup before death and was not included in this study.
The average age of the patients at the time of index revision surgery was 66.3 years (range, 46–80 years). There were seven men and four women. The average height and weight were 99 kg (range, 56–116 kg) and 168 cm (range, 163–178 kg), respectively.
Seven patients had their original THA secondary to degenerative osteoarthritis. The remaining four patients’ indications were osteonecrosis, slipped capital femoral epiphysis, hip dysplasia, and seronegative inflammatory arthropathy. Revision surgery was indicated for aseptic loosening in 10 of these patients and a late dislocation with infection in one.
Two of the 11 patients had procedures before their primary THAs. The patients with slipped capital femoral epiphysis and osteonecrosis underwent pinning of the epiphysis with cannulated screws and core decompression, respectively.
Five of the 11 patients had previous acetabular revision surgery before index revision with a bilobed component. Three had acetabular component revision with a structural bone graft and a cementless cup. One patient had a structural bone graft, an acetabular cage, and a cemented cup. The fifth patient presented from an outside institution with a late dislocation and workup revealed an infection. This patient had a resection arthroplasty with placement of an antibiotic spacer.
We performed revision arthroplasty for aseptic loosening of a primary THA in the remaining four patients. Three of these patients had cementless acetabular components that showed clinical and radiographic evidence of loosening with superior and rotational migration and massive osteolysis resulting in a Type III acetabular deficiency. The fourth patient, at an outside institution, had a cemented all-polyethylene cup placed in a high hip center secondary to hip dysplasia. Fragmentation of the cement mantle and cup eventually resulted in failure with massive bone stock loss.
Ten of the femoral components were well fixed and retained during the acetabular revision. We performed the index revision using a trochanteric slide surgical approach [14]. The acetabulum was underreamed 1 to 3 mm before implant insertion. We removed fibrous tissue from cavitary defects and filled them with particulate graft when appropriate. Reaming in each case was performed freehand in a sequential fashion using hemispheric acetabular reamers for the inferior and superior hemispheres independently without the use of the bilobed reaming guide. Each bilobed implant was an E25, which has built-in anteversion of the inferior hemisphere maximizing bony contact while avoiding posterior instability. Component size was selected after reaming to maximize host bone-implant contact and minimize anterior and posterior bone removal. We used screws in all cases.
We performed routine anteroposterior pelvis and true lateral radiographs of the hip immediately postoperatively, at 3 and 6 months, and at yearly intervals thereafter. All radiographic measurements were performed by one observer (JTM). The angle of the cup and the distance from the acetabular component to Kohler’s line and the teardrop were measured and compared on serial radiographs. We defined linear migration of the acetabular component as a change greater than 2 mm in either the medial or superior direction, or both [11]. Rotational migration was defined as a change greater than 3° in the theta angle, which is the angle formed by the horizontal line drawn through the teardrop and the plane of the opening of the lower lobe of the cup [4]. We also recorded the radiographic distance from the hip center to the interteardrop line before and after surgery.
We evaluated the acetabular bone-prosthesis interface using a modification of the method of DeLee and Charnley [9] as described by Berry et al. [2]. In this system, the superior lobe is considered Zone 1 and the superior and inferior halves of the lower lobe are considered Zones 2 and 3, respectively.
We assessed clinical status before and after arthroplasty with Harris hip scores and measurement of leg length differences at each visit. All clinical observations were made by two individuals (JTM, LLF).
Results
As reported previously [21], the average bilobed component size was 60-E25 (range, 54-E25-63-E25) and fixed with an average of five screws (range, 4–7 screws). The equivalent jumbo hemispheric cup average diameter was 85 mm (range, 80–88 mm) in the superoinferior direction. The average volume of the bilobed component was 42% smaller than the equivalent jumbo hemispheric cup (range, 40%–45%).
Clinical improvements in pain and functional status were maintained at intermediate followup. At a minimum of 60 months followup (mean, 6.2 years; range, 60–84 months), the mean Harris hip scores improved from 36 preoperatively (range, 25–45) to 85 postoperatively (range, 81–90). The average pain scores improved from 8 (range, 0–10) preoperatively to 42 (range, 40–44) postoperatively. There have been no postoperative dislocations, clinical deep venous thrombosis, pulmonary embolism, infections, or intraoperative fractures.
Radiographic analysis shows improvements in component position and leg length differences have been maintained at intermediate followup. The average leg length difference improved from 34 mm preoperatively (range, 16 mm short to 53 mm short) to 7 mm postoperatively (range, 2 mm long to 14 mm short). The distance from the interteardrop line to the hip center decreased from 42 mm preoperatively (range, 31–74 mm) to 29 mm postoperatively (range, 18–38 mm). The average theta angle of the inferior lobe was 43° (range, 32°–58°). Despite an average postoperative limb lengthening greater than 2 cm, no postoperative nerve palsies were observed.
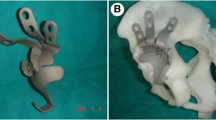
At a minimum of 60 months followup, there were no findings of focal osteolysis or lucencies. Nine of the acetabular components appeared osteointegrated with evidence of spot wielding of the pelvis to the prosthesis. At the 3-year postoperative visit, the acetabular component in one patient had two broken screws. Five years after surgery, the patient is without component migration and remains clinically asymptomatic (Fig. 1). We currently consider this component to have a stable fibrous ingrowth and have no immediate plans to revise this component but will continue to monitor with annual clinical and radiographic evaluations.
(A) A preoperative photograph shows catastrophic failure of the acetabular implant and protrusio. A radiograph obtained at the 2-year followup shows good apparent stability. (B) The patient had a broken screw in this hip at the 3-year followup but otherwise was asymptomatic. (C) At the 5-year followup, the patient had a broken screw without additional signs of loosening. The patient remains asymptom- atic.
Discussion
Orthopaedic surgeons are performing an increasing number of revision hip arthroplasties each year as life expectancy and the number of primary THAs performed increase. Revision acetabuloplasties with considerable pelvic bone stock deficiencies requiring complex reconstructive techniques are becoming more common [2, 10, 12]. Bilobed acetabular components can be an attractive alternative for American Academy of Orthopaedic Surgeons Type III defects compared with hemispheric implants of the same superoinferior diameter because the bilobed cups are smaller in the anteroposterior and mediolateral dimensions. This should allow for preservation of anterior and posterior column bone stock and a decreased risk of disrupting Kohler’s line with subsequent protrusio. They allow the defect to be filled without structural allograft bone and promote restoration of an anatomic hip center.
The importance of returning the hip center to as near an anatomic position as possible has been reported in clinical studies [18, 23, 29]. Restoration of the hip center potentially will improve leg length differences, decrease limp, and help reestablish and maintain hip stability, mechanics, and range of motion [2, 27]. Superolateral placement of the acetabular component theoretically can increase joint contact forces and subsequent wear rates causing early loosening and higher failure rates [8].
Attempting to restore the anatomic hip center using a structural bone graft with or without reconstruction rings or cages can place the acetabular component on predominantly nonviable bone and at risk for loosening and early failure [15, 20]. Impaction grafting places the reconstruction on nonhost bone; however, the results for this type of reconstruction have been very good [3, 13, 26, 28].
Long-term results of Type III acetabular deficiencies with structural bone grafts and cementless or cemented components have not been as good as the results for Types I and II deficiencies [2, 5, 12, 15, 16, 23]. Reported revision rates range from 20% to 30% with overall failure rates as much as 50% when Type III deficiencies are revised with a structural bone graft and cementless cups [15, 24].
The current series has good intermediate results in a subset of patients with challenging Type III acetabular defects. The study is limited by the low number of cases, but this is a relatively rare clinical scenario and these intermediate results therefore are pertinent. An additional limitation is that intraobserver variation was not measured for radiographic measurements performed.
Reported results of bilobed implants have been variable. As a result of technical difficulty and a 24% rate of loosening at an average of 41 months, Chen et al. did not recommend the use of bilobed acetabular components [5]. They also believe its use is specifically contraindicated in Type III deficiencies with greater than 2 cm superior migration of the acetabular component with a medial wall defect [5].
Conversely, a multicenter trial using bilobed acetabular components found few complications. There was one acetabular failure in 38 hips [2]; this failure was in a revision in which the component sat on greater than 50% structural allograft from a previous revision. In another study including 15 revision acetabuloplasties, there were no revisions and no loose components at an average followup of 4.5 years [8]. Both of these studies included a wide range of acetabular deficiencies, including Types I and II in addition to Type III defects. To our knowledge, there is only one other study examining results for Type III deficiencies without structural bone graft. In this study, less than  of the patients had reconstruction surgery with bilobed components; most patients were treated with hemispheric components [23].
of the patients had reconstruction surgery with bilobed components; most patients were treated with hemispheric components [23].
The majority of revision acetabuloplasties can be performed using a standard hemispheric component. In a small but increasing subset of patients with considerable acetabular deficiencies, use of a standard cup requires use of a structural allograft, defect-bridging devices with bone graft and/or cement or placement of the component above the anatomic hip center. Modular tantulum or custom-made implants also can be used. In the 3-year period this study was conducted, 84% of the revision acetabuloplasties at our institution were performed using a standard porous-coated hemispheric cup. There was a subgroup of 11 patients (16%) in which use of a hemispheric cup would have required extensive structural allograft or the use of defect-bridging devices (antiprotrusio or reconstruction cages) with bone graft and/or cement or placing the component high in the pelvis. In these cases with Type III acetabular deficiencies, porous-coated bilobed acetabular components without structural bone graft were used. This continues to be the implant used in these situations by the senior author (JTM). Our review of this series of patients has shown good clinical and radiographic results at an average followup of 6.2 years. It is our conclusion that porous-coated bilobed acetabular components without structural allograft are a viable alternative for reconstructing Type III acetabular deficiencies in revision hip surgery.
References
Berry DJ, Müller ME. Revision arthroplasty using an anti-protrusio cage for massive acetabular deficiency. J Bone Joint Surg Br. 1992;74:711–715.
Berry DJ, Sutherland CJ, Trousdale RT, Colwell CW Jr, Chandler HP, Ayres D, Yashar AA. Bilobed oblong porous coated acetabular components in revision total hip arthroplasty. Clin Orthop Relat Res. 2000;371:154–160.
Bolder SB, Melenhorst J, Gardeniers JWM, Slooff TJ, Veth RPH, Schreurs BW. Cemented total hip arthroplasty with impacted morcellized bone-grafts to restore acetabular bone defects in congenital hip dysplasia. J Arthroplasty. 2001;16(8 suppl 1):164–169.
Callaghan JJ, Salvati EA, Pellicci PM, Wilson PD Jr, Ranawat CS. Results of revision for mechanical failure after cemented total hip replacement, 1972–1982: a two to five-year follow-up. J Bone Joint Surg Am. 1985;67:1074–1085.
Chen WM, Engh CA Jr, Hopper RH Jr, McAuley JP, Engh CA. Acetabular revision with use of a bilobed component inserted without cement in patients who have acetabular bone stock deficiency. J Bone Joint Surg Am. 2000;82:197–206.
D’Antonio JA, Capello WN, Borden LS, Bargar WL, Bierbaum BF, Boettcher WG, Steinberg ME, Stulberg SD, Wedge JH. Classification and management of acetabular abnormalities in total hip arthroplasty. Clin Orthop Relat Res. 1989;243:126–137.
Dearborn JT, Harris WH. Acetabular revision arthroplasty using so-called jumbo cementless components: an average 7-year follow-up study. J Arthroplasty. 2000;15:8–15.
DeBoer DK, Christie MJ. Reconstruction of the deficient acetabulum with an oblong prosthesis: three to seven-year results. J Arthroplasty. 1998;13:674–680.
DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20–32.
Dorr LD, Wan Z. Ten years of experience with porous acetabular components for revision surgery. Clin Orthop Relat Res. 1995;319:191–200.
Garbuz D, Morsi E, Gross AE. Revision of the acetabular component of a total hip arthroplasty with a structural allograft: study with a minimum five-year follow-up. J Bone Joint Surg Am. 1996;78:693–697.
Gerber SD, Harris WH. Femoral head autografting to augment acetabular deficiency in patients requiring hip replacement: a minimum five-year and an average seven-year follow-up study. J Bone Joint Surg Am. 1986;68:1241–1248.
Gie GA, Linder L, Ling LS, Simon JP, Slooff TJ, Timperley AJ. Impacted cancellous allografts and cement for revision total hip arthroplasty. J Bone Joint Surg Br. 1993;75:14–21.
Glassman AH, Engh CA, Bobyn JD. A technique of extensile exposure for total hip arthroplasty. J Arthroplasty. 1987;2:11–21.
Hooten JP Jr, Engh CA Jr, Engh CA. Failure of structural acetabular allografts in cementless revision hip arthroplasty. J Bone Joint Surg Br. 1994;76:419–422.
Jasty M, Harris WH. Salvage total hip reconstruction in patients with major acetabular bone deficiency using structural femoral head allografts. J Bone Joint Surg Br. 1990;72:63–67.
Kwong LM, Jasty M, Harris WH. High failure rate of bulk femoral head allografts in total hip acetabular reconstructions at 10 years. J Arthroplasty. 1993;8:341–346.
Linde F, Jensen J. Socket loosening in arthroplasty for congenital dislocation of the hip. Acta Orthop Scand. 1988;59:254–257.
Moskal JT, Danisa OA, Shaffrey CI. Isolated revision acetabuloplasty using a porous-coated cementless acetabular component without removal of a well-fixed femoral component: a 3- to 9-year follow-up study. J Arthroplasty. 1997;12:719–727.
Moskal JT, Shen FH. The use of bilobed-porous coated acetabular components without structural bone graft for type III acetabular defects in revision total hip arthroplasty: a prospective study with a minimum 2-year follow-up. J Arthroplasty. 2004;19:867–873.
Moskal JT, Shen FH, Brown TE. The fate of stable femoral components retained during isolated acetabular revision: a six- to twelve-year follow-up study. J Bone Joint Surg Am. 2002;84:250–255.
Nehme A, Lewallen DG, Hanssen AD. Modular porous metal augments for treatment of severe acetabular bone loss during revision total hip arthroplasty. Clin Orthop Relat Res. 2004;429:201–208.
Paprosky WG, Magnus RE. Principals of bone grafting in revision total hip arthroplasty: acetabular technique. Clin Orthop Relat Res. 1994;298:147–155.
Pollock FH, Whiteside LA. The fate of massive allografts in total hip revision acetabular surgery. J Arthroplasty. 1992;7:271–276.
Russotti GM, Harris WH. Proximal placement of the acetabular component in total hip arthroplasty: a long term follow-up study. J Bone Joint Surg Am. 1991;73:587–592.
Schreurs BW, Thien TM, de Waal Malefijt MC, Buma P, Veth RP, Slooff TJ. Acetabular revision with impacted morselized cancellous bone graft and a cemented cup in patients with rheumatoid arthritis: three to fourteen-year follow-up. J Bone Joint Surg Am. 2003;85:647–652.
Schutzer SF, Harris WH. High placement of porous-coated acetabular components in complex total hip arthroplasty. J Arthroplasty. 1994;9:359–367.
Stulberg SD. Impaction grafting: doing it right. J Arthroplasty. 2002;17(4 suppl 1):147–152.
Sutherland CJ. Treatment of type III acetabular deficiencies in revision total hip arthroplasty without structural bone graft. J Arthroplasty. 1996;11:91–98.
Unger AS, Lewis RJ, Greun T. Evaluation of a porous tantalum uncemented acetabular cup in revision total hip arthroplasty: clinical and radiological results of 60 hips. J Arthroplasty. 2005;20:1002–1009.
Whaley AL, Berry DJ, Harmsen WS. Extra-large uncemented hemispherical acetabular components for revision total hip arthroplasty. J Bone Joint Surg Am. 2001;83:1352–1357.
Acknowledgments
We thank Linda L. Franklin, RN, ONC, for help in collecting Harris hip scores.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has either waived or does not require approval for the human study protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
An erratum to this article can be found at http://dx.doi.org/10.1007/s11999-008-0215-6.
About this article
Cite this article
Moskal, J.T., Higgins, M.E. & Shen, J. Type III Acetabular Defect Revision With Bilobed Components. Clin Orthop Relat Res 466, 691–695 (2008). https://doi.org/10.1007/s11999-007-0079-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-007-0079-1