Abstract
Purpose
Revision total hip arthroplasty (THA) is challenging if severe periacetabular bone loss is present. Here we describe a method that uses a customised cage to reconstruct an acetabulum with a massive bone defect.
Methods
Designed with the aid of the rapid prototyping technique, a customised cage with a hook, crest and flange or braids was made, and then utilized to reconstruct severe compromised acetabulum in revision THA since 2001. Twenty-two patients (23 hips) were included in this study. The mean patient age at the time of surgery was 60.9 years (range, 38–80 years). Three hips had massive acetabular bone defects of Paprosky type IIIA and 20 of type IIIB. The Harris hip score was used to evaluate hip function. Radiographs were taken to evaluate loosening of the cage and resorption of allograft bone.
Results
The average follow up was 81.6 ± 24.9 months. The mean Harris hip score improved from 39.6 pre-operatively to 80.9 at the final follow-up. There were no instances of deep infection, severe venous thrombosis, and nerve palsy. One patient who had an intra-operative rupture of the superior acetabular artery was successfully treated using the haemostatic suturing technique. Two patients experienced dislocation at post-operative days four and six, respectively, and both were treated with closed reduction and skin traction for three weeks.
Conclusions
The present study demonstrates that a customised cage may be a promising option for THA revision of severely compromised acetabula. Extended follow-up is necessary to evaluate the long-term performance of this approach.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acetabular revision in the presence of massive bone defects remains one of the most difficult challenges in hip arthroplasty. Although many approaches have been developed, such as revision with jumbo acetabular components, oblong cups, structural grafts, reinforcement rings, antiprotrusio cages, and cementless modular revision system, there are few reliable options [1–4]. Furthermore, despite greatly enhancing the surgeon’s ability to reconstruct severely compromised acetabula, the recently developed porous-coated or ultraporous metal cups, shells, and augments do not fully recapitulate the lost bone [5, 6]. In addition, some total hip arthroplasty (THA) revisions are beyond the scope of these techniques.
The periacetabular anatomy is complex, and each patient tends to be unique in terms of the anatomy of the acetabular deficiency. With the development of the rapid prototyping (RP) technique for medical applications, a customized cage in combination with an allograft may be an attractive option for acetabular revision in cases with severe bone loss. The customized cage is designed based on a thin-cut pre-operative computed tomography (CT) scan of the whole pelvis, which is used to create three-dimensional digital models. The RP technique provides surgeons with key information regarding the bone defects, which may be difficult to obtain through imaging data alone. Based on the RP model and using computer-aided design (CAD) software and specialised programs, the customized cage is manufactured and utilised in the THA reconstruction of the acetabulum with massive bone defects. Potential advantages of this technique include the ability to provide an individualised fit for each patient; place the cage in the correct anatomic position; fine-tune the number, position, and direction of screws; and support the overall mechanical stability of the bone-cage system.
We have employed the RP technique to design customized cages for the reconstruction of severe acetabulum defects in revision THA since 2001. The purpose of this study was to retrospectively analyse the clinical and radiographic outcomes and to present our experience with the use of customized cages for revision of the acetabula with massive defects.
Patients and methods
Between September 2001 and July 2011, we used customized cages in revision hip arthroplasty for 23 patients (24 hips) with massive acetabular bone defects of Paprosky type III. One patient was lost to follow-up, leaving 22 patients (23 hips) for study. The indications for the use of customized cages were severe bone defects with pelvic discontinuity that could not be reconstructed using commercially available cages based on a prototyping model.
The mean age of the patients at the time of surgery was 60.9 years (range, 38–80 years). One male patient underwent staged bilateral hip revision surgery with customized cages, and both hips were included in the study. The indications for the primary THA included developmental dysplasia (n = 11), femoral head necrosis (n = 4), osteoarthritis (n = 3), and femoral neck fracture (n = 5). The reasons for revision were aseptic loosening in 21 hips and sepsis in two hips. The Paprosky classification system was used to evaluate the degree of bone defect [7]. There were three hips of type IIIA and 20 hips of type IIIB. Eighteen femoral component revisions were performed concomitantly at the time of acetabular revision for aseptic loosening (16 hips) or infection (two hips). The remaining five femoral components were stable in pre-operative evaluation and reconfirmed during operation. Twenty-three hips received follow-up care for an average of 81.6 ± 24.9 months.
Design of cages
The RP technique was used to convert standard pre-operative CT information into an isometric physical object model as we described previously [8]. In short, using a CAD software and a specialised program (MIMICS-Materialise Interactive Medical Image Control System Software, Materialise, Belgium), CT scans of the whole pelvis obtained with intervals of 1 mm were converted into three-dimensional digital models. These digital models were then used to produce life-size three-dimensional pelvis models using a laminated object manufacturing system called Dimension Elite (Stratasys Inc., MN, USA).
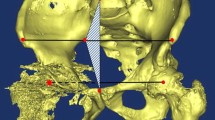
A series of trials were conducted using the RP model to determine whether a commercially available cage could be well supported by the host bone. Customized cages were utilised in cases where the bone abnormality presented additional challenges. The customized cage was designed with the MIMICS software. The cage comprised three parts: the dome, hook, and flange or three braids (Fig. 1a). The dome was designed to accommodate a polyethylene liner, and the flange or braids had holes for screw fixation to the ilium. The hook is extended from the inferior margin of the dome to be positioned just below the inferior side of the acetabulum. Three principles were taken into account during the design and manufacturing of the customized cage:
First, for the purpose of anatomical reconstruction, the centre of the cage’s dome should be placed symmetrically to the rotation centre of the contralateral hip to restore the height, lateral distance, and abduction angle.
Second, the cage should be reliably supported by the host supra-acetabular bone. If a severe bone defect precludes achieving a solid support, an M-shaped crest can be used to connect the cage’s dome to the host bone (Fig. 2).
Third, the flange or braids of the cage should be firmly fixed to the iliac bone with screws to assure rigid primary mechanical stabilisation. The site of attachment and size of the flange or braids should be planned meticulously to match the geometry of the ilium and bone defect. The hook must be placed well in the obturator just under the acetabulum to control the rotation stability as well as bear a part of the load.
After the digital cage was optimised based on the above three principles, a model of the customized cage was made. This cage model and the prototype pelvis were sent to the surgeons for review (Fig. 1b). The surgeons discussed with the engineers for further adjustments on the basis of the three principles. Once the design was finalised, the prototype was digitised and the final cage was manufactured of titanium (ShengShi Company, Shanghai, China). Porous and hydroxyapatite coatings were applied to the bone-implant interfaces to facilitate osteointegration.
Surgical procedures
All operations were performed by the senior author (Zhu). The posterolateral approach was used in all patients. Granulated tissues, cement, particles, and interface membranes were thoroughly removed from the acetabular defect region after the exposure and removal of the failed implant. The severity of the bone defect and the periacetabular bone quality were re-evaluated under direct observation. The soft tissue was then dissected along the ilium to achieve exposure of the wing of the ilium, sufficient for the proper placement of the flange or braids of the customized cage. The inferior margin of the acetabulum was exposed, allowing for the placement of the hook for fixation. The manufactured customized cage was then inserted and positioned according to the preoperative design. After confirming that the hook was placed in the obturator just below the inferior margin of the acetabulum and the flange or braids fitted the geometry of the iliac wing well, screws were inserted through the holes in the flange or braids. Morselised allograft was used to densely fill the remaining bone defect between the cage’s dome and host bone (Fig. 2). A polyethylene liner was cemented into the cage with proper anteversion and abduction angles.
Post-operative recovery and assessment
Standard antibiotics were administered for three days postoperatively (for patients with previous infection, this treatment was extended to ten to 14 days). Partial weight-bearing with a walker was advised for the first six weeks after the surgery. Progressive weight-bearing with crutches was then started, and free ambulation was allowed after three months.
Follow-ups were conducted three, six, and 12 months after the surgery, and then annually. The Harris hip score was used to evaluate hip function [9]. Clinical failure was defined as any need for revision of the acetabular component and was showing as endpoint. Radiographs were taken pre-operatively, immediately after the operation, and at the final follow-up in a manner similar to that described by Peters et al. [10]. Significant migration was defined as a change in the acetabular inclination of ≥5° or linear migration of the hip centre of ≥5 mm. The thickness of bone-implant radiolucent lines around the cage and screws was measured according to the zonal analysis of DeLee and Charnley [11]. The stability of the cage was assessed according to the criteria of Gill et al. [12], using the following grades: definitely loose (screw breakage or acetabular migration >5 mm or progressive radiolucent lines), probably loose (progressive radiolucent lines), and possibly loose (nonprogressive radiolucent lines not involving the screws). Following the criteria of Russotti [13], a revision was considered a failure if one or more of the following occurred: (a) re-revision of the acetabular component for any reason; (b) migration or loosening of the cage; and (c) severe resorption of the allograft. Resorption of allograft bone was assessed on anteroposterior pelvic radiographs and graded as minor (<1/3 of the graft resorbed), moderate (1/3 to 1/2 of the graft resorbed), and severe (>1/2 of the graft resorbed) [14].
Statistical methods
Statistical analysis was conducted with SPSS for Windows, version 11.5 (SPSS Inc., Chicago, IL, USA). To evaluate the significance of the findings, the Student t-test was used to compare paired variables. A P value <0.05 was considered to indicate statistical significance. Kaplan–Meier survival curves with 95 % confidence intervals (CI) were calculated using aseptic loosening and revision for any reason as the endpoints.
Results
The mean Harris hip score improved from 39.6 (range, 12–60) pre-operatively to 80.9 (range, 53–93) at the final follow-up (P < 0.01). There were no instances of deep infection, severe venous thrombosis, and nerve palsy. One patient (case 6) who had an intra-operative rupture of the superior acetabular artery (a branch of the superior gluteal artery) was successfully treated using the haemostatic suturing technique. Two patients (cases 8 and 18) experienced dislocation at post-operative days four and six, respectively, and both were treated with closed reduction and skin traction for three weeks. No redislocation occurred within the follow-up periods of 76 and 55 months, respectively, and the Harris scores were 81 and 78, respectively. Using the Kaplan-Meier survival analysis at 72 months (Fig. 3), the survival of the cage with revision for any reason was 91.30 % (95 % CI 58.10–73.95) and with aseptic loosening as the endpoint was 95.66 % (95 % CI 63.10–74.81).
Representative pre-operative and post-operative radiographs are shown in Figs. 4 and 5. There were two cases of early cage failure because of mechanical loosening (cases 4 and 5). Case 4 is represented in Fig. 6. The patient complained of groin pain when walking six months after the revision surgery. Radiography showed grafted bone absorption around the cage’s dome. This patient refused to undergo a re-revision intervention and used crutches in daily life. At 40 months, the graft bone absorption was severe according to the Gross grade.
A 56-year-old woman developed prosthetic cup loosening seven years after the operation. a A pre-operative radiograph shows a massive acetabular bone defect. b A customised cage with morselised allografts was used to reconstruct the acetabulum. c A radiograph taken at the nine-year follow-up showed that the cages are stable and the bone grafts are well remodeled
A 69-year-old man developed bilateral acetabular cup loosening 23 years after the operation. a A pre-operative radiograph shows massive acetabular bone defects on both sides. b An immediate post-operative radiograph shows the reconstitution with a cage and a morselised allograft on the right side. c Five months after the right revision, a revision was performed on the left side with a reconstruction cage and a morselised allograft. d A radiograph taken at the 76 months follow-up examination indicated that the cages are stable and the bone grafts are incorporated
A 47-year-old woman with acetabular cup loosening reconstructed with a customised cage. a An immediate post-operative radiograph. b and c Severe absorption of the grafted bone was observed 29 and 40 months after the revision operation, respectively. d Coronal and crosscut computed tomography scans showed that there was no bony connection between the cage and the host bone
The other failure (case 5) was due to a change in the cage position that occurred at post-operative day 12 when the patient was performing partial weight-bearing exercises. The reason for the loosening was failure to place the hook into the obturator. This patient underwent re-revision surgery four weeks later using another customized cage, which was stable (Harris hip score of 75) at the final follow-up four years after the surgery (Fig. 7).
A 64-year-old woman with acetabular cup loosening. a A pre-operative radiograph. b The customised cage loosened at post-operative day 12. c The patient underwent re-revision surgery four weeks later using another customised cage. d A radiograph taken at the four-year follow-up showed that the cages are stable
Twenty-two of the 23 cages (including the re-revision case) were considered stable and without migration based on the radiographic data. The overall incidence of radiolucent lines was 13 % (three hips). In all cases, the radiolucency was partial and nonprogressive, and the lines were <2 mm in width (DeLee and Charnley zone II in two cases and III in one case). Incorporation of the graft, defined as the presence of clearly delineated trabecula crossing the graft-host junction, was complete in 19 hips. No screw fractures were observed.
Discussion
Acetabular bone defects are common in THA revision. For Paprosky type I and II defects, a conventional acetabular component with or without an allograft can produce good results as there is sufficient support from the host bone to provide initial stability. In contrast, there are few reliable options for Paprosky type III defects because the remaining acetabular rim cannot provide adequate initial component stability [15]. A customized cage with a RP model can be used in especially challenging situations. First, an RP model is employed to determine whether such a cage is necessary. The cage can then be designed using a computer based on thin-cut CT images capable of precisely reproducing the whole pelvic region. The contralateral hip should be used as a reference to achieve the proper position of the rotation centre, offset, and leg length.
The mid-long term success of the cage relies on the incorporation of graft bone for achieving biologic fixation. On the other hand, the incorporation of graft bone is dependent on the initial stability of the cage to provide mechanical load protection. The following conditions should be met to maximize the initial stability of the cage: (1) the cage’s dome should be reliably supported by the host supra-acetabular bone, (2) the flange or braids must fit the shape of the ilium and be fixed firmly by screws, and (3) the hook must be set just below the acetabulum and placed in the obturator as far as possible. It is vital that the cage seats well on the host supra-acetabular bone to achieve a solid support. The loss of contact between the cage’s dome and the host bone is the main reason for failure by loosening [16, 17]. In a retrospective study reported by Friedrich et al. [18], 18 acetabula with Paprosky type 3B defects were reconstructed with custom-made acetabular components. The initial stability of the implant was obtained by screw fixation. Two of 18 custom-made implants were considered radiographically loose at an average follow up of 30 months. Case 4 of the present study failed without valid protection by the cage that lacked initial stability without solid support by the host bone. After this case, when the RP models indicate that the superior acetabulum as well as the posterior and anterior columns of the acetabulum cannot provide the necessary support for the cage’s dome, an M-shaped crest should be designed. The bottom of the “M” is fixed firmly on the cage’s dome, and its tips is designed to just entrap on the host supra-acetabular bone, achieving an initial mechanical support for the cage (Fig. 2). Morselised allograft was used to fill the remaining bone defect between cage and host bone. All of the grafts bone was incorporated after the crest was designed.
Solid fixation of the flange or braids is critically important for the initial stability of the cage. Therefore, their shapes should be designed to fit the geometry of the wing of the ilium precisely. The flange or braids should be designed and placed as far anteriorly as possible to prevent vessel rupture. In one of our early cases, the superior acetabular artery was ruptured intraoperatively in the process of detaching the soft tissue from the ilium at the posterosuperior side of the acetabulum. This main branch of the superior gluteal artery extending from the greater sciatic notch to the superior side of the acetabulum is prone to rupture when the soft tissue is being detached posteriorly.
The triflange cage is the most widely used custom-made component for massive bone defects repair [19–25]. This cage has three flanges designed to rest on the ilium, ischium, and pubis. Fixation by multiple screws through the holes in the flanges allows for a reliable contact between the cage and the host bone. The main difference between our customized cage and the triflange cage is that a hook instead of a flange extends from the inferior side of the dome. As a result, less extensive tissue dissection is sufficient for placing the hook into the obturator, and this procedure is less technically demanding than fixation of the flange on the ischium with screws. Another difference is the use of the crest designed for connecting the cage to the host bone in cases with insufficient support.
Kerboull described a hooked reinforcement device for acetabular revision and reported a 92.1 % survival rate at 13 years follow-ups [26]. This noncustomized device was partly or totally supported by femoral head allografts at the superior acetabular roof. Although the allograft bone was all incorporated by radiographical identification reported in Kerboull’s cases, we didn’t use bulk structure allografts due to difficult availability, cost, and worrying about collapse, immunogenicity and viral contamination [7, 27–31].
Impaction bone grafting is another method to restore acetabular bone stock. It is suitable for simple cavitary bone defects and can be used for segmental or combined structural defects. In the type of pelvic discontinuity defect, a plate must be used prior to impaction grafting, for a metal mesh alone is not adequate to bridge the discontinuous parts [31]. Long-term results reported by Schreurs et al. [32] and Busch et al. [33] demonstrated impaction bone grafting is an effective method for bone stock restoration in the setting of bone loss. Loading allografts with bone marrow derived mesenchymal stem cells could enhance incorporation of allografts with the host bone and decrease the failure rate for acetabular defect reconstruction. For Paprosky type 3A or 3B acetabular defects, Hernigou et al. [34] reported that the rate of mechanical failure was 30 % (9/30) with allograft without stem cells, while there were no failures (0/30) for patients with allograft loaded with stem cells.
The common complications of THA revision with a triflange cage include component failure, dislocation, deep infection, and nerve palsy. The dislocation rate ranges from 0 to 30 %. In the study of Christie et al. [19], the dislocation rate was 15.6 %, and 8 % (6/78) of the cases were revised for recurrent dislocation. Taunton et al. [20] reported a dislocation rate of 21 % in 57 hips followed up for 76 months. There were no cases with dislocation in the studies of Wind et al. [21] and Berasi et al. [22]. In the present study, the dislocation rate was 9 % (2/23), and dislocation was corrected by closed reduction in both cases. In line with the reports by Christie et al. [19], Joshi et al. [23], and Holt and Dennis [24], the present cage failure rate was 9 % (2/23). Importantly, there were no instances of deep infection in the present study. In this regard, two out of 57 cases (3.6 %) reported by Tauntonet al. [20] and two out of 22 (8 %) cases by Berasi et al. [22] required intervention for deep infection. In comparison, Christie et al. [19] and De Boer et al. [25] reported no infection cases in 67 and 30 hip revisions, respectively. Accurate placement of the custom triflange component requires substantial exposure of the ilium and ischium, increasing the risk of nerve and vascular injury [27]. Thus, six out of the seven studies reported nerve injury, with the sciatic and superior gluteal nerves being most commonly involved. In comparison, vascular injury occurred in one of the 23 (4 %) cases in the present study, and no instances of nerve palsy were observed. We believe that the utilisation of a hook in the design of the cage and placing the braids more anteriorly may reduce the rates of vascular and nerve complications.
This study is limited by its retrospective design and the lack of a control group. Bone defects of Paprosky type III are uncommon, and it is difficult to conduct a prospective study unless a multicentre observational study is arranged. Another limitation is the relatively short-term follow-up; the duration of the follow-up should be extended in the future.
In conclusion, reconstruction of the acetabula with massive defects has been a major surgical challenge in the past ten years. The findings of the present study show that a customized cage utilising a hook and crest and designed with the aid of the RP technique may be a promising option when reconstructing severely compromised acetabula.
References
Regis D, Magnan B, Sandri A, Bartolozzi P (2008) Long-term results of anti-protrusion cage and massive allografts for the management of periprosthetic acetabular bone loss. J Arthroplast 23:826–832. doi:10.1016/j.arth.2007.06.017
Sporer SM, O’Rourke M, Chong P, Paprosky WG (2005) The use of structural distal femoral allografts for acetabular reconstruction. Average ten-year follow-up. J Bone Joint Surg Am 87:760–765. doi:10.2106/JBJS.D.02099
Chen AF, Hozack WJ (2014) Component selection in revision total hip arthroplasty. Orthop Clin N Am 45:275–286. doi:10.1016/j.ocl.2014.03.001
Schmolders J, Friedrich MJ, Michel RD, Randau TM, Wimmer MD, Strauss AC, Kohlhof H, Wirtz DC, Gravius S (2015) Acetabular defect reconstruction in revision hip arthroplasty with a modular revision system and biological defect augmentation. Int Orthop 39:1–8
Abolghasemian M, Tangsataporn S, Sternheim A, Backstein D, Safir O, Gross AE (2013) Combined trabecular metal acetabular shell and augment for acetabular revision with substantial bone loss: a mid-term review. Bone Joint J 95-B:166–172. doi:10.1302/0301-620X.95B2.30608
Steno B, Kokavec M, Necas L (2015) Acetabular revision arthroplasty using trabecular titanium implants. Int Orthop 39:389–395
Paprosky WG, Perona PG, Lawrence JM (1994) Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J Arthroplasty 9:33–44
Li H, Wang L, Mao Y, Wang Y, Dai K, Zhu Z (2013) Revision of complex acetabular defects using cages with the aid of rapid prototyping. J Arthroplast 28:1770–1775. doi:10.1016/j.arth.2012.12.019
Harris WH (1969) Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 51:737–755
Peters CL, Curtain M, Samuelson KM (1995) Acetabular revision with the Burch-Schnieder antiprotrusio cage and cancellous allograft bone. J Arthroplast 10:307–312
DeLee JG, Charnley J (1976) Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res 121:20–32
Gill TJ, Sledge JB, Muller ME (2000) The management of severe acetabular bone loss using structural allograft and acetabular reinforcement devices. J Arthroplast 15:1–7
Pazzaglia UE (1990) Pathology of the bone-cement interface in loosening of total hip replacement. Arch Orthop Trauma Surg 109:83–88
Gross AE (1999) Revision arthroplasty of the acetabulum with restoration of bone stock. Clin Orthop Relat Res 369:198–207
Zagorodniy N, Nikolaev I, Nuzhdin V, Kagramanov S (2014) Prospective cohort study of six hundred and sixty four revisions of loose failed acetabular implants. Int Orthop 38:2021–2025
Gross AE (2006) Restoration of acetabular bone loss 2005. J Arthroplast 21:117–120
Sembrano JN, Cheng EY (2008) Acetabular cage survival and analysis of factors related to failure. Clin Orthop Relat Res 466:1657–1665. doi:10.1007/s11999-008-0183-x
Friedrich MJ, Schmolders J, Michel RD, Randau TM, Wimmer MD, Kohlhof H, Wirtz DC, Gravius S (2014) Management of severe periacetabular bone loss combined with pelvic discontinuity in revision hip arthroplasty. Int Orthop 38:2455–2461
Christie MJ, Barrington SA, Brinson MF, Ruhling ME, DeBoer DK (2001) Bridging massive acetabular defects with the triflange cup: 2- to 9-year results. Clin Orthop Relat Res 216–227
Taunton MJ, Fehring TK, Edwards P, Bernasek T, Holt GE, Christie MJ (2012) Pelvic discontinuity treated with custom triflange component: a reliable option. Clin Orthop Relat Res 470:428–434. doi:10.1007/s11999-011-2126-1
Wind MA Jr, Swank ML, Sorger JI (2013) Short-term results of a custom triflange acetabular component for massive acetabular bone loss in revision THA. Orthopedics 36:e260–e265. doi:10.3928/01477447-20130222-11
Berasi CC, Berend KR, Adams JB, Ruh EL, Lombardi AV Jr (2015) Are custom triflange acetabular components effective for reconstruction of catastrophic bone loss? Clin Orthop Relat Res 473:528–535. doi:10.1007/s11999-014-3969-z
Joshi AB, Lee J, Christensen C (2002) Results for a custom acetabular component for acetabular deficiency. J Arthroplast 17:643–648
Holt GE, Dennis DA (2004) Use of custom triflanged acetabular components in revision total hip arthroplasty. Clin Orthop Relat Res 429:209–214
DeBoer DK, Christie MJ, Brinson MF, Morrison JC (2007) Revision total hip arthroplasty for pelvic discontinuity. J Bone Joint Surg Am 89:835–840. doi:10.2106/JBJS.F.00313
Kerboull M, Hamadouche M, Kerboull L (2000) The Kerboull acetabular reinforcement device in major acetabular reconstructions. Clin Orthop Relat Res 378:155–168
Nieminen J, Pakarinen TK, Laitinen M (2013) Orthopaedic reconstruction of complex pelvic bone defects. Evaluation of various treatment methods. Scand J Surg SJS Off Organ Finnish Surg Soc Scand Surg Soc 102:36–41
Lee PT, Raz G, Safir OA, Backstein DJ, Gross AE (2010) Long-term results for minor column allografts in revision hip arthroplasty. Clin Orthop Relat Res 468:3295–3303. doi:10.1007/s11999-010-1591-2
Delloye C, Banse X, Brichard B, Docquier PL, Cornu O (2007) Pelvic reconstruction with a structural pelvic allograft after resection of a malignant bone tumor. J Bone Joint Surg Am 89:579–587. doi:10.2106/JBJS.E.00943
Dewal H, Chen F, Su E, Di Cesare PE (2003) Use of structural bone graft with cementless acetabular cups in total hip arthroplasty. J Arthroplast 18:23–28. doi:10.1054/arth.2003.50013
Sheth NP, Nelson CL, Springer BD, Fehring TK, Paprosky WG (2013) Acetabular bone loss in revision total hip arthroplasty: evaluation and management. J Am Acad Orthop Surg 21:128–139. doi:10.5435/JAAOS-21-03-128
Schreurs BW, Keurentjes JC, Gardeniers JW, Verdonschot N, Slooff TJ, Veth RP (2009) Acetabular revision with impacted morsellised cancellous bone grafting and a cemented acetabular component: a 20- to 25-year follow-up. J Bone Joint Surg (Br) 91:1148–1153. doi:10.1302/0301-620X.91B9.21750
Busch VJ, Gardeniers JW, Verdonschot N, Slooff TJ, Schreurs BW (2011) Acetabular reconstruction with impaction bone-grafting and a cemented cup in patients younger than fifty years old: a concise follow-up, at twenty to twenty-eight years, of a previous report. J Bone Joint Surg Am 93:367–371. doi:10.2106/JBJS.I.01532
Hernigou P, Pariat J, Queinnec S, Homma Y, Lachaniette CHF, Chevallier N, Rouard H (2014) Supercharging irradiated allografts with mesenchymal stem cells improves acetabular bone grafting in revision arthroplasty. Int Orthop 38:1913–1921
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Mao, Y., Xu, C., Xu, J. et al. The use of customized cages in revision total hip arthroplasty for Paprosky type III acetabular bone defects. International Orthopaedics (SICOT) 39, 2023–2030 (2015). https://doi.org/10.1007/s00264-015-2965-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-2965-6