Abstract
Purpose of review
The goal of this review is to highlight the influence of therapeutic maneuvers on neuro-prognostication measures administered to comatose survivors of cardiac arrest. We focus on the effect of sedation regimens in the setting of targeted temperature management (TTM), one of the principle interventions known to improve neurological recovery after cardiac arrest. Further, we discuss the critical need for novel markers, as well as refinement of existing markers, among patients receiving extracorporeal membrane oxygenation (ECMO) in the setting of failed conventional resuscitation, known as extracorporeal cardiopulmonary resuscitation (ECPR).
Recent findings
Automated pupillometry may have some advantage over standard pupillary examination for prognostication following TTM, sedation, or the use of ECMO after cardiac arrest. New serum biomarkers such as Neurofilament light chain have shown good predictive abilities and need further validation in these populations. There is a high-level uncertainty in brain death declaration protocols particularly related to apnea testing and appropriate ancillary tests in patients receiving ECMO.
Summary
Both sedation and TTM alone and in combination have been shown to affect prognostic markers to varying degrees. The optimal approach to analog-sedation is unknown, and requires further study. Moreover, validation of known prognostic markers, as well as brain death declaration processes in patients receiving ECMO is warranted. Data on the effects of TTM, sedation, and ECMO on biomarkers (e.g., neuron-specific enolase) and electrophysiology measures (e.g., somatosensory-evoked potentials) is sparse. The best approach may be one customized to the individual patient, a precision-medicine approach.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
With the advent of targeted temperature management (TTM) and extracorporeal membrane oxygenation (ECMO), we entered a new era of therapeutics that fundamentally altered our ability to prognosticate and brought the well-accepted pre-TTM era guidelines into question. Further, it has become a common practice to prescribe analgesics and sedatives for at least the initial 24 h of TTM for the prevention and treatment of shivering and the duration of ECMO administration for safety and comfort. The effect of TTM, ECMO, and these pharmacologic agents on the prognostic accuracy of predictors of neurologic recovery has not been systematically evaluated. The 2006 American Academy of Neurology (AAN) guideline for outcome prediction in comatose survivors of cardiac arrest was published prior to the TTM era and recommended outcome prediction within 72 h of cardiopulmonary resuscitation and return of spontaneous circulation [1]. In 2014, the European Resuscitation Council’s advisory statement on outcome prediction recommended delaying neuro-prognostication beyond 72 h if residual effects of sedation or paralysis are suspected [2].
It is especially important to understand the accuracy of prognostic testing in patients receiving ECMO during cardiac arrest or for post-cardiac arrest cardiogenic shock, as recent research shows that profound and irreversible neurological deficits are often the primary reason that surrogate decision-makers cite for withdrawal of ECMO support from a critically ill patient [3], and neurological etiologies are among the most common cause of death in ECMO patients [4]. Limited data exists regarding the extent to which ECMO may affect the prognosticators of patient recovery from acute brain injury.
The impact of medical management on prognostication
Indications and implications of TTM
The 2015 American Heart Association (AHA) guideline recommends that comatose adult survivors of cardiac arrest undergo TTM between 32 °C and 36 °C (class I, level of evidence (LOE) B-R for shockable rhythms with out-of-hospital cardiac arrest; class I, LOE C-EO for non-shockable rhythms and in-hospital cardiac arrest) [5••]. The AHA suggests that TTM be maintained for at least 24 h after achieving target temperature (class IIa, LOE C-EO), but recommends against the routine prehospital cooling of patients with rapid infusion of cold fluids (class III, LOE A). Finally, the same AHA guideline states that it may be reasonable to actively prevent fever in comatose patients following TTM (class IIb, LOE C-LD) [5••]. TTM can be achieved using intravascular or surface cooling with limited data demonstrating no clear superiority of one method over another [6,7,8]. Shivering is the most common complication of TTM and most prominent during the induction phase when target temp is 32–34 °C and occurs regardless of target temperature chosen [9, 10]. Shivering attenuates the benefits of TTM by increasing metabolism and lowering brain oxygenation [11, 12]. Vigilant monitoring for shivering with aggressive treatment is indicated [13].
Understanding the pharmacokinetics and pharmacodynamics of sedatives and analgesics as well as the different factors that may lead to their accumulation and prolonged elimination plays a key role in prognostication in the setting of TTM. Predictors of late awakening in comatose cardiac arrest survivors treated with therapeutic hypothermia and sedation have been evaluated in a single-center observational cohort [14•]. While the use of midazolam alone [14•] or in combination with fentanyl [15•] has been shown to be associated with late awakening compared with propofol. This could be explained by the differences between midazolam and propofol pharmacokinetic properties (see supplementary Table 1). Physiologic alterations impacting pharmacokinetics have also been described during TTM. These include a decrease in the cytochrome P450 activity, reduction in both hepatic transformation and renal excretion, due to a decrease in hepatic and renal blood flow, respectively [16, 17]. An excess of serum drug concentrations used for sedation and neuromuscular blockade, a decrease in total body clearance, and persistence of elevated drug levels even hours after rewarming have been demonstrated in brain-injured patients receiving TTM to 32–34 °C [18,19,20].
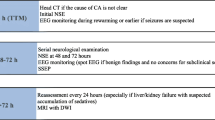
Neurological exam
In patients who receive TTM, the AHA guideline recommends [5••] waiting for 72 h after return to normothermia (class IIb, LOE C-EO) to help reduce the confounding risk of sedation and neuromuscular blockade, especially in the context of decreased drug clearance in the setting of TTM, liver injury, or acute kidney injury [21]. TTM either prolongs the time to awakening or allows those who otherwise would not regained consciousness to do so in a delayed fashion [22,23,24,25,26,27]. A post hoc analysis of the TTM trial evaluated the time until awakening after cardiac arrest and its association with the goal temperature of 33 versus 36 °C [28]. Despite receiving comparable cumulative doses of sedatives in both groups, and no difference in ultimate neurological outcome, daily awakening was delayed in patients in the 33 °C group. This might be due to decreased clearance of sedatives and analgesics at lower body temperature. In this trial, the false positive rate (FPR) of absent pupillary reflex was 2.1% (95% confidence intervals (CI) 0.3–11.2%), and the FPR of absent corneal reflex was 2.2% (95% CI 0.3–11.4%). Though not statistically significant, both false positives were in patients cooled to 33 °C as opposed to 36 °C, which raises the issue of patients cooled to 33 °C requiring more time prior to prognostication than those cooled to 36 °C [29].
The European Resuscitation Council reported an FPR of absent pupillary reflex of 8% (95% CI 1–25%) within the first day with an improvement of 0% at 72 h both in patients treated with TTM and those not treated with TTM [30]. The AHA guideline likewise suggests that absence of pupillary reflex in patients 72 h post-cardiac arrest was a reasonable basis for poor outcome prediction with a FPR of 1% (95% CI 0–3%) in patients who have undergone TTM (class I, LOE B-NR) [5••]. However, in a subsequent study of patients receiving TTM, 5 of 78 patients (FPR 6%) with absent pupillary light reflexes on day 3 had a favorable outcome [31••].
Overall, absence of the corneal reflex seems less specific for poor outcome than absence of the pupillary light reflex. In patients treated with TTM to 33 °C, absent corneal reflex at 72–120 h predicts poor outcome with a FPR of 2% (95% CI 0–7%) [32, 33]. The FPR for absence of either pupillary or corneal reflexes at 72 h has been reported as 4% (95% CI 1–15%) at 33 °C [34] with similar findings at 36 °C [35].
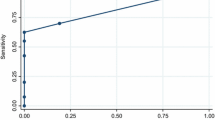
Recently, investigators have assessed automated pupillometry as an advance over standard pupillary examination for prognostication following cardiac arrest. Suys et al. reported that under conditions of TTM to 33 °C with concomitant sedation, quantitative pupillometry light response is lower than in normothermic conditions in the absence of sedation [36]. Nonetheless, quantitative pupillometry has shown promise as a prognostic tool during TTM with sedation with a quoted FPR of 0% for quantitative pupillary light reactivity measure (expressed as the % of pupillary response to a calibrated light stimulus) of < 7% in one and < 13% in two other studies [36,37,38]. The Neurological Pupil index (NPi) may be an even more accurate prognosticator than the quantitative pupillary light reflex during the first days of TTM, as it may be more sensitive and less influenced by opioids and ambient light [31••].
The AHA guideline recommends that motor responses alone should not be used for predicting a poor neurologic outcome (class III harm, LOE B-NR) [5••] due to high FPRs (10–20%) associated with it of 10% (95% CI 7–15%) [33, 34].
While the brainstem reflexes are seen to be more present upon discontinuation of sedation [39], a retrospective evaluation demonstrated that while sedation decreases the positive predictive value of the absence of corneal reflexes and poor motor exam, it does not affect the prognostic accuracy of the absence of pupillary responses [40].
While any myoclonus within 72 h predicts a poor outcome (5% FPR; 95% CI 3–8%) [33, 34, 41, 42], patients with myoclonus associated with epileptiform activity on electroencephalography (EEG) seem to have a worse prognosis than those without epileptiform activity [43]. Given the high FPRs, the AHA recommends that the presence of any myoclonus should not be used to predict poor neurological outcome (class III: harm, LOE B-NR). They do suggest, however, that the presence of status myoclonus may be used during the first 72 to 120 h after cardiac arrest in combination with other tests to predict poor outcome (class IIa, LOE B-NR) [5••]. In the TTM era, there has been a push towards increasingly sophisticated classifications of myoclonus, including consideration of the anatomical distribution, type, duration, associated EEG findings, and response to treatment [43, 44••, 45, 46, 47••].
Electrophysiology (EEG and SSEP)
Electroencephalography
EEG background is widely used for early prognostication and risk stratification, with several patterns correlating with poor outcome after CA. These patterns include malignant features [48, 49] such as burst-suppression pattern [50], low voltage [51, 52], status epilepticus [53,54,55], stimulus-induced rhythmic, and periodic or ictal discharges [56]. Conversely, presence of continuous background during the post-resuscitation phase, including the time from arrest to the development of such background is associated with good outcome [52, 57]. However, sedation is known to affect the EEG background in healthy individuals [58], and the influence of sedation on these patterns is not routinely reported. A single-center study showed that suppression ratio and amplitude-integrated EEG have been changed significantly after sedation lightening in cardiac arrest patients, with the degree of change correlating with outcome [59]. Given these factors, clinicians who attempt interpretation without taking sedation into account may make inappropriate conclusions. Another EEG-based feature, reactivity to external stimulus, has also been associated with outcome and has been reported in several evaluations of multimodal prognostication [2, 52, 60]. The effect of sedation on EEG reactivity has not been reported, although it is likely there would be changes similar to those seen with EEG background. This has resulted in the most recent international consensus for EEG reactivity reporting recommending that information on analgesics and sedatives be reported when testing EEG reactivity in cardiac arrest patients [61]. A recent study showed that a routinely used sedative, propofol, induces changes in the post-anoxic EEG, but does not affect its value for the prediction of outcome [62•].
Somatosensory-evoked potentials
In patients who have undergone TTM, absent N20 responses after rewarming may be slightly more accurate than during TTM in prediction of a poor outcome (FPR 1%, 95% CI 0–3% vs. FPR 2%, 95% CI 0–4%) [32,33,34, 42, 63, 64]. The AHA reports that it is reasonable to consider bilaterally absent N20 responses 24 to 72 h after cardiac arrest, regardless of TTM, as a predictor of poor outcome (class IIa, LOE B-NR). A caveat to that recommendation is that artifact frequently limits the interpretability of somatosensory-evoked potentials (SSEPs), even in paralyzed patients [65]. Analgesics and sedatives could increase the latency and decrease the amplitude of the SSEP response in a dose-dependent manner [21]. Despite evaluations reporting low FPR of 0.7% (95% CI 0–5%) for bilateral absent N20, when adjusted for early withdrawal of life supporting therapy, the FPR increased to 7.7% [66•]. Nonetheless, some researchers have suggested a more nuanced analysis of N20 amplitudes beyond the dichotomous presence versus absence distinction to increase the sensitivity of SSEPs to predict poor outcome [67, 68].
Serum biomarkers
Neuron-specific enolase and serum S-100 β protein
Serum neuron-specific enolase (NSE), a marker of neuronal injury, is the best-studied serum biomarker for prognostication following cardiac arrest. By attenuating secondary neuronal injury, TTM may lower serum NSE levels [69]. Serum S-100 β protein, a marker of glial injury as opposed to neuronal injury, may be less affected by TTM than serum NSE [69]. The depth and duration of TTM do not seem to have a significant effect on NSE or S-100 β protein levels [70,71,72]. It is uncertain if any definite threshold exists to predict poor outcome in patients treated with TTM, but certainly, a serum NSE threshold of 33 μg/L results in unacceptably high FPRs [32, 33, 70]. In one study, a cut-off of 151 μg/L was needed to obtain an FPR of 0% [73]. Some of the difficulty in establishing an acceptable threshold for biomarkers like NSE or Serum S-100 β protein may be attributable to sample hemolysis, variance in storage practices and diagnostic assays, or other laboratory-based variations [74]. The AHA guideline recommends that NSE or serum S-100 β protein should not be used alone to predict poor neurologic outcome (class III harm, LOE C-LD) [5••]. If obtaining a single serum NSE, day 3 values may be the most accurate for diagnosing poor outcome [75]. Serial sampling may also improve accuracy [76].
Serum neurofilament light chain
The development of an ultrasensitive assay has prompted interest in serum neurofilament light chain as a predictor of poor outcome following cardiac arrest. In the TTM trial, serum neurofilament light chain was a more sensitive predictor of poor outcome than the neurological exam or electrophysiological assessments with comparable specificity [77••]. Target temperature may affect levels depending on the time-point tested.
Neuroimaging
Computed tomography (CT)
Reduced gray-white ratio at the level of the basal ganglia predicts poor outcome with variably low FPRs based on measurement technique and threshold [78,79,80,81]. Insufficient data are available to suggest a significant effect of TTM on CT imaging following cardiac arrest. The AHA guideline suggests that it may be reasonable to use a marked reduction in gray-white ratio on brain CT obtained within 2 h after cardiac arrest to predict poor outcome in patients not treated with TTM (class IIb, LOE B-NR), but makes no recommendations for patients treated with TTM [5••].
Magnetic resonance imaging (MRI)
Neuronal injury on MRI is detected by diffusion-weighted imaging (DWI) and quantified by the apparent diffusion coefficient (ADC). Both qualitative measures of DWI abnormalities and quantified ADC thresholds have been reported as predictors of poor outcome following cardiac arrest, in either regional or global distributions [82, 83, 84•]. Methodological variance is partially responsible for the wide variation of reported FPRs for poor outcome. There are also concerns regarding interrater reliability when quantitative values are not obtained [85]. In addition, MRI changes following cardiac arrest are dynamic [86]. The preferred timing of MRI for prognostication is uncertain, but most experts advocate waiting 2–5 days following cardiac arrest. The influence of TTM on MRI-based prognostication is unknown, but some advocate for longer waiting periods prior to obtaining MRI in patients who undergo TTM [87•]. The AHA guidelines suggests that it may be reasonable to consider extensive restriction of diffusion 2–6 days following cardiac arrest in combination with other predictors to predict poor outcome (class IIB, LOE B-NR) [5••]. Whether hypothermia has any effect on resting state neural networks, fractional anisotropy on diffusion tensor imaging or any metabolites measured via magnetic resonance spectroscopy is unknown.
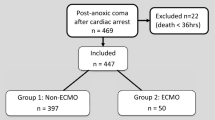
ECMO as a therapeutic agent after cardiac arrest
ECMO is an increasingly used technique providing cardiopulmonary support to patients with severe refractory cardiac and respiratory failure. Venoarterial ECMO in the setting of cardiac arrest is used either as extracorporeal cardiopulmonary resuscitation (ECPR) during cardiac arrest refractory to conventional cardiopulmonary resuscitation, or for post-cardiac arrest cardiogenic shock. There is a high incidence of neurological complications reported in patients requiring ECMO during or after cardiac arrest [88, 89••, 90]. Neuromonitoring would be appropriate pre-cannulation to identify the salvageable cases devoid of severe anoxic brain injury in cases where this is feasible, and post-cannulation to prognosticate comatose survivors and to potentially declare brain death when there is evidence for it (Table 1). Limited data exist regarding the predictive value of the different monitoring modalities in this setting.
Neurological exam
During ECMO support, patients may undergo physical examinations per the standard procedure, restricted only by sedation and neuromuscular blockade. Comatose ECMO patients are thus, often-limited to pupillary assessments, and data is conflicting at best. Maekawa et al. suggested that pupil diameter on hospital arrival may be a key predictor of neurologic outcome in patients who went on to receive ECMO [91]. However, another study showed no differences in pupil diameter on arrival to the emergency room between survivors and non-survivors of ECMO for out-of-hospital cardiac arrest [92]. The authors did observe a positive pupillary reflex more frequently in after initiation of ECMO, and this was seen in significantly more survivors than non-survivors.
New automatic computerized devices such as the NPi-200 Pupillometer, which measures pupillary size and reactivity, have eliminated inaccuracies caused by interpreter reliability. One small study (N = 28) has found the quantitative neurological pupillary index to be a useful early neuro-prognosticator in venoarterial ECMO patients [93•].
Electrophysiology (EEG and SSEP)
While there is very little data in adults, studies from critically ill neonates placed on ECMO post-hypoxic-ischemic encephalopathy provide some evidences that monitoring of electrical activity via EEG and SSEP may not be entirely accurate for patients during ECMO [94]. Data from neonates receiving ECMO have highlighted the fact that abnormalities in EEG background could be a result of ECMO and may resolve with time [95, 96]. The most abnormal EEG while receiving ECMO and EEG and SSEP readings after decannulation have been shown to have the strongest predictive value for neurological prognosis [95]. The data is sparse in adults; there has been a recent small study examining EEG background (N = 13) and SSEPs (N = 7) in patients on VA ECMO [97•]. Only poor variability and absence of reactivity were associated with unfavorable neurologic outcome. Of the seven patients who received the SSEPs as well, all had poor outcomes, despite the presence of N20 response (4 normal, 3 delayed). However, based on the small sample size and the fact that no patients had absent N20 responses and, even when they were present, they were due to peripheral delays; the researchers urge caution when using EEG and SSEPs to prognosticate in patients receiving ECMO until the results of their study are better understood and validated (5).
Neuroimaging
Choices for imaging techniques, as with physical examinations, are limited during ECMO support. Due to the ferrous properties of the ECMO pump and circuit, magnetic resonance imaging while receiving ECMO is contraindicated. In adults, cranial computed tomography (CT) is preferred but due to the difficulty of transporting patients receiving ECMO support [98], some ECMO patients only undergo CT after decannulation. Portable CT scanners have potential to make imaging more widely available. Studies looking at the predictive ability of CT in ECMO patients are sparse. One small study (N = 20) [92] showed that findings on brain CT just after ECMO and subsequent images may represent an important predictor for neurologic outcome. Further, all patients (N = 4) who had intracranial hemorrhage due to hypoxic brain damage on follow-up images died regardless of the initial CT findings. Growing clinical experience with ECMO has led to greater awareness about CT imaging pitfalls, including variable levels of flow assistance and cannulation strategies that all may potentially affect interpretation of imaging studies [99].
Serum biomarkers
Plasma biomarkers have the potential to emerge as a leading monitoring tool to predict the neurological outcome for patients during ECMO. An ideal biomarker would have high sensitivity for detection of both ischemic and hemorrhagic injury, provide real-time information, and allow detection of injury at the cellular level that precedes cellular death [100]. Several biomarkers related to glial injury (glial fibrillary acidic protein (GFAP) and serum S-100 β), neuronal injury (NSE), and other markers of neuroinflammation (ICAM-5 and monocyte chemoattractant protein 1/chemokine (C-C motif) ligand 2 (MCP-1/CCL-2)) have been associated with a higher risk of neurological injury and death [100,101,102]. Similarly, serum S-100 β may serve as an early indicator of cerebral complications, in particular, intracerebral hemorrhage [103]. In a more recent meta-analysis (17 papers containing 903 cases), high serum lactate level was associated with poor survival and poor neurological outcome in CA patients treated with ECMO [104•]. Lastly, elevated concentrations of GFAP and ICAM-5 predicted abnormal neuroimaging [101]. While validation in larger studies is still required, these preliminary findings have suggested biomarkers mentioned above as potential indicators for obtaining further investigations (i.e., neuroimaging and non-invasive neuromonitoring) and for initiation of neuroprotective therapies.
Brain death declaration
The American Academy of Neurology has outlined criteria for the determination of brain death [105]. Given the high reported mortality rates—and in particular, brain death—in patients treated with ECMO for cardiac arrest, a thorough understanding of the definition and determinations of brain death is critical. Despite the importance of the assessment of brain death, objective protocols for patients receiving ECMO are clearly lacking [106•]. Unfortunately, patients who require ECMO support often have physiologic conditions that might further challenge apnea testing. For patients being supported with venoarterial ECMO, pulsatile flow and blood pressures in the absence of significant doses of vasoactive agents might be too low as mandated by the AAN prior to attempting an apnea test. Various strategies have been proposed but have not reached universal consensus [107, 108]. Ancillary tests including continuous electroencephalographic (EEG) testing may be helpful when positive, but external electromagnetic energy sources like ECMO circuitry, may make conclusive interpretation of results difficult. Cerebral angiography or nuclear scanning may document the absence of cerebral blow flow, but such testing in patients receiving ECMO may be due to logistics [109•]. To compensate for the confounding influence of the inherent ability of the ECMO circuit not only to provide hemodynamic stability, but also more importantly, to maintain adequate oxygenation and normal blood carbon dioxide levels; some investigators have proposed modifications of ECMO flows and gas exchange during apnea testing. However, such experiences are limited to small series of patients [107, 108].
Conclusion
With advances in therapeutics such as TTM and ECMO and effective public health campaigns, survival rates after cardiac arrest have increased significantly in the last decade. Despite such optimistic developments, withdrawal of life-sustaining therapy because of perceived poor neurological prognosis remained the most common cause of hospital death after cardiac arrest. Sedation continues to be the most critical confounder adversely affecting the reliability and the validity of measures traditionally being validated in the pre-TTM era for neuro-prognostication after cardiac arrest. Future studies are needed to examine the value of a multimodal prognostication scheme that includes novel biomarkers, quantitative measures of brain stem reflexes, and point-of-care cerebral perfusion monitors that allow optimization of blood flow after achieving a return of spontaneous circulation after cardiac arrest. Outcomes to test predictive abilities should integrate neurocognitive, functional, and psychological deficits along with survival.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Wijdicks EF, Hijdra A, Young GB, Bassetti CL, Wiebe S. Practice parameter: prediction of outcome in comatose survivors after cardiopulmonary resuscitation (an evidence-based review): report of the quality standards Subcommittee of the American Academy of Neurology. Neurology. 2006;67:203–10.
Sandroni C, Cariou A, Cavallaro F, Cronberg T, Friberg H, Hoedemaekers C, et al. Prognostication in comatose survivors of cardiac arrest: an advisory statement from the European Resuscitation Council and the European Society of Intensive Care Medicine. Intensive Care Med. 2014;40(12):1816–31.
Lan, Chinchun, Pi-Ru Tsai, Yih-Sharng Chen, and Wen-Je Ko. "Prognostic factors for adult patients receiving extracorporeal membrane oxygenation as mechanical circulatory support-a 14-year experience at a medical center." Artif Organs 34, no. 2 (2010).
Bridwell A, Tymkew H. Physical therapy for patients with a centralized insertion of extracorporeal membrane oxygenation: a case series. Cardiopulm Phys Ther J. 2014;25(4):132–3.
•• Callaway CW, Donnino MW, Fink EL, et al. Part 8: post-cardiac arrest care: 2015: American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18 Suppl 2):S465–82. This 2015 systematic review examined numerous studies of the diagnostic accuracy of clinical findings, electrophysiological modalities, imaging modalities, and blood markers for predicting neurologic outcome in comatose post–cardiac arrest patients who receive TTM, as well as who do not receive TTM.
Tømte Ø, Drægni T, Mangschau A, Jacobsen D, Auestad B, Sunde K. A comparison of intravascular and surface cooling techniques in comatose cardiac arrest survivors. Crit Care Med. 2011;39(3):443–9.
Deye N, Cariou A, Girardie P, Pichon N, Megarbane B, Midez P, et al. Endovascular versus external targeted temperature management for patients with out-of-hospital cardiac arrest: a randomized , controlled study. Circulation. 2015;132(3):182–93.
Glover GW, Thomas RM, Vamvakas G, al-Subaie N, Cranshaw J, Walden A, et al. Intravascular versus surface cooling for targeted temperature management after out-of-hospital cardiac arrest - an analysis of the TTM trial data. Crit Care. 2016;20(1):381.
Polderman KH, Herold I. Therapeutic hypothermia and controlled normothermia in the intensive care unit: practical considerations, side effects, and cooling methods. Crit Care Med. 2009;37(3):1101–20.
Nielsen N, Wetterslev J, Cronberg T, et al. Targeted temperature management at 33°C versus 36°C after cardiac arrest. N Engl J Med. 2013;369(23):2197–206.
Badjatia N, Strongilis E, Gordon E, Prescutti M, Fernandez L, Fernandez A, et al. Metabolic impact of shivering during therapeutic temperature modulation: the bedside shivering assessment scale. Stroke. 2008;39(12):3242–7.
Oddo M, Frangos S, Maloney-Wilensky E, Andrew Kofke W, Le Roux PD, Levine JM. Effect of shivering on brain tissue oxygenation during induced normothermia in patients with severe brain injury. Neurocrit Care. 2010;12(1):10–6.
Choi HA, Ko SB, Presciutti M, Fernandez L, Carpenter AM, Lesch C, et al. Prevention of shivering during therapeutic temperature modulation: the Columbia anti-shivering protocol. Neurocrit Care. 2011;14(3):389–94.
• Rey A, Rossetti AO, Miroz JP, et al. Late awakening in survivors of post-anoxic coma: early neurophysiologic predictors and association with ICU and long-term neurologic recovery. Crit Care Med. 2019;47:85–92 A single-center, observational cohort study examining the neurophysiologic predictors and outcomes of patients with late awakening following cardiac arrest. The study showed delaying prognostication will permit late awakening with favorable outcomes.
• Paul M, Bougouin W, Dumas F, et al. Comparison of two sedation regimens during targeted temperature management after cardiac arrest. Resuscitation. 2018;128:204–10. The potential advantages of short-acting agents for sedation use during TTM has not been studied well. This multi-center study showed that sedation with propofol-remifentanil was associated with significantly earlier awakening and more ventilator-free days as compared with midazolam-fentanyl.
Sunjic KM, Webb AC, Šunjić I, et al. Pharmacokinetic and other considerations for drug therapy during targeted temperature management. Crit Care Med. 2015;43:2228–38.
Tortorici MA, Kochanek PM, Poloyac SM, et al. Effects of hypothermia on drug disposition, metabolism, and response: a focus of hypothermia-mediated alterations on the cytochrome P450 enzyme system. Crit Care Med. 2007;35:2196–204.
Fritz HG, Holzmayr M, Walter B, Moeritz KU, Lupp A, Bauer R. The effect of mild hypothermia on plasma fentanyl concentration and biotransformation in juvenile pigs. Anesth Analg. 2005;100:996–1002.
Fukuoka N, Aibiki M, Tsukamoto T, Seki K, Morita S. Biphasic concentration change during continuous midazolam administration in brain-injured patients undergoing therapeutic moderate hypothermia. Resuscitation. 2004;60:225–30.
Leslie K, Sessler DI, Bjorksten AR, et al. Mild hypothermia alters propofol pharmacokinetics and increases the duration of action of atracurium. Anesth Analg. 1995;80:1007–14.
Polderman KH. Mechanisms of action, physiological effects, and complications of hypothermia. Crit Care Med. 2009;37(7 Suppl):S186–202.
Gold B, Puertas L, Davis SP, et al. Awakening after cardiac arrest and post resuscitation hypothermia: are we pulling the plug too early? Resuscitation. 2014;85(2):211–4.
Grossestreuer AV, Abella BS, Leary M, Perman SM, Fuchs BD, Kolansky DM, et al. Time to awakening and neurologic outcome in therapeutic hypothermia-treated cardiac arrest patients. Resuscitation. 2013;84(12):1741–6.
Eid SM, Albaeni A, Vaidya D, Nazarian SM, Llinas R, Chandra-Strobos N. Awakening following cardiac arrest: determined by the definitions used or the therapies delivered? Resuscitation. 2016;100:38–44.
Mulder M, Gibbs HG, Smith SW, Dhaliwal R, Scott NL, Sprenkle MD, et al. Awakening and withdrawal of life-sustaining treatment in cardiac arrest survivors treated with therapeutic hypothermia. Crit Care Med. 2014;42(12):2493–9.
Irisawa T, Vadeboncoeur TF, Karamooz M, Mullins M, Chikani V, Spaite DW, et al. Duration of coma in out-of-hospital cardiac arrest survivors treated with targeted temperature management. Ann Emerg Med. 2017;69(1):36–43.
Zanyk-McLean K, Sawyer KN, Paternoster R, Shievitz R, Devlin W, Swor R. Time to awakening is often delayed in patients who receive targeted temperature management after cardiac arrest. Ther Hypothermia Temp Manag. 2017;7(2):95–100.
Lybeck A, Friberg H, Aneman A, Hassager C, Horn J, Kjærgaard J, et al. Prognostic significance of clinical seizures after cardiac arrest and target temperature management. Resuscitation. 2017;114:146–51.
Dragancea I, Horn J, Kuiper M, et al. Neurological prognostication after cardiac arrest and targeted temperature management 33°C versus 36°C: results from a randomised controlled clinical trial. Resuscitation. 2015;93:164–70.
Sandroni C, Cariou A, Cavallaro F, Cronberg T, Friberg H, Hoedemaekers C, et al. Prognostication in comatose survivors of cardiac arrest: an advisory statement from the European Resuscitation Council and the European Society of Intensive Care Medicine. Intensive Care Med. 2014;40(12):1816–31.
•• Oddo M, Sandroni C, Citerio G, et al. Quantitative versus standard pupillary light reflex for early prognostication in comatose cardiac arrest patients: an international prospective multicenter double-blinded study. Intensive Care Med. 2018;44(12):2102–11. In this prospective international multicenter study (10 centers), quantitative NPi was shown to have excellent ability to predict an unfavorable outcome from day 1 after cardiac arrest, with no false positives, and significantly higher specificity than standard manual pupillary examination.
Fugate JE, Wijdicks EF, Mandrekar J, Claassen DO, Manno EM, White RD, et al. Predictors of neurologic outcome in hypothermia after cardiac arrest. Ann Neurol. 2010;68(6):907–14.
Bouwes A, Binnekade JM, Kuiper MA, et al. Prognosis of coma after therapeutic hypothermia: a prospective cohort study. Ann Neurol. 2012;71(2):206–12.
Rossetti AO, Oddo M, Logroscino G, Kaplan PW. Prognostication after cardiac arrest and hypothermia: a prospective study. Ann Neurol. 2010;67(3):301–7.
Tsetsou S, Novy J, Pfeiffer C, Oddo M, Rossetti AO. Multimodal outcome prognostication after cardiac arrest and targeted temperature management: analysis at 36 °C. Neurocrit Care. 2018;28(1):104–9.
Suys T, Bouzat P, Marques-Vidal P, Sala N, Payen JF, Rossetti AO, et al. Automated quantitative pupillometry for the prognostication of coma after cardiac arrest. Neurocrit Care. 2014;21(2):300–8.
Heimburger D, Durand M, Gaide-Chevronnay L, Dessertaine G, Moury PH, Bouzat P, et al. Quantitative pupillometry and transcranial Doppler measurements in patients treated with hypothermia after cardiac arrest. Resuscitation. 2016;103:88–93.
Solari D, Rossetti AO, Carteron L, Miroz JP, Novy J, Eckert P, et al. Early prediction of coma recovery after cardiac arrest with blinded pupillometry. Ann Neurol. 2017;81(6):804–10.
Rohaut B, Porcher R, Hissem T, et al. Brainstem response patterns in deeply-sedated critically-ill patients predict 28-day mortality. PLoS One. 2017;12:e0176012.
Samaniego EA, Mlynash M, Caulfield AF, Eyngorn I, Wijman CA. Sedation confounds outcome prediction in cardiac arrest survivors treated with hypothermia. Neurocrit Care. 2011;15(1):113–9.
Crepeau AZ, Rabinstein AA, Fugate JE, Mandrekar J, Wijdicks EF, White RD, et al. Continuous EEG in therapeutic hypothermia after cardiac arrest: prognostic and clinical value. Neurology. 2013;80(4):339–44.
Oddo M, Rossetti AO. Early multimodal outcome prediction after cardiac arrest in patients treated with hypothermia. Crit Care Med. 2014;42(6):1340–7.
Seder DB, Sunde K, Rubertsson S, Mooney M, Stammet P, Riker RR, et al. Neurologic outcomes and postresuscitation care of patients with myoclonus following cardiac arrest. Crit Care Med. 2015;43(5):965–72.
•• Rossetti AO, Rabinstein AA, Oddo M. Neurological prognostication of outcome in patients in coma after cardiac arrest. Lancet Neurol. 2016;15(6):597–609. This review emphasized the important of utilizing multimodal neuroprognostication paradigm and the fact that multimodal assessment could provide reassurance about the reliability of a prognostic estimate by offering concordant evidence.
Reynolds AS, Rohaut B, Holmes MG, Robinson D, Roth W, Velazquez A, et al. Early myoclonus following anoxic brain injury. Neurol Clin Pract. 2018;8(3):249–56.
Dhakar MB, Sivaraju A, Maciel CB, Youn TS, Gaspard N, Greer DM, et al. Electro-clinical characteristics and prognostic significance of post anoxic myoclonus. Resuscitation. 2018;131:114–20.
•• Geocadin RG, Callaway CW, Fink EL, et al. Standards for studies of neurological prognostication in comatose survivors of cardiac arrest: a scientific statement from the American Heart Association. Circulation. 2019:CIR0000000000000702. https://doi.org/10.1161/CIR.0000000000000702. This a scientific statement from The American Heart Association Emergency Cardiovascular Care Science Subcommittee comprising of adult and pediatric experts from neurology, cardiology, emergency medicine, intensive care medicine, and nursing to review existing neurological prognostication studies, the practice of neurological prognostication, and withdrawal of life-sustaining treatment.
Amorim E, Rittenberger JC, Baldwin ME, Callaway CW, Popescu A; Post Cardiac Arrest Service. Malignant EEG patterns in cardiac arrest patients treated with targeted temperature management who survive to hospital discharge. Resuscitation 2015;90:127–132.
Mettenburg JM, Agarwal V, Baldwin M, Rittenberger JC. Discordant observation of brain injury by MRI and malignant electroencephalography patterns in comatose survivors of cardiac arrest following therapeutic hypothermia. AJNR Am J Neuroradiol. 2016;37:1787–93.
Andresen JM, Girard TD, Pandharipande PP, Davidson MA, Ely EW, Watson PL. Burst suppression on processed electroencephalography as a predictor of post-coma delirium in mechanically ventilated ICU patients. Crit Care Med. 2014;42:2244–51.
Hofmeijer J, Beernink TM, Bosch FH, Beishuizen A, Tjepkema-Cloostermans MC, van Putten MJ. Early EEG contributes to multimodal outcome prediction of postanoxic coma. Neurology. 2015;85:137–43.
Sivaraju A, Gilmore EJ, Wira CR, Stevens A, Rampal N, Moeller JJ, et al. Prognostication of post-cardiac arrest coma: early clinical and electroencephalographic predictors of outcome. Intensive Care Med. 2015;41:1264–72.
Dragancea I, Backman S, Westhall E, Rundgren M, Friberg H, Cronberg T. Outcome following postanoxic status epilepticus in patients with targeted temperature management after cardiac arrest. Epilepsy Behav. 2015;49:173–7.
Geocadin RG, Ritzl EK. Seizures and status epilepticus in post cardiac arrest syndrome: therapeutic opportunities to improve outcome or basis to withhold life sustaining therapies? Resuscitation. 2012;83:791–2.
Mikhaeil-Demo Y, Gavvala JR, Bellinski II, Macken MP, Narechania A, Templer JW, et al. Clinical classification of post anoxic myoclonic status. Resuscitation. 2017;119:76–80.
Alvarez V, Oddo M, Rossetti AO. Stimulus-induced rhythmic, periodic or ictal discharges (SIRPIDs) in comatose survivors of cardiac arrest: characteristics and prognostic value. Clin Neurophysiol. 2013;124:204–8.
Westhall E, Rosén I, Rundgren M, Bro-Jeppesen J, Kjaergaard J, Hassager C, et al. Time to epileptiform activity and EEG background recovery are independent predictors after cardiac arrest. Clin Neurophysiol. 2018 Aug;129(8):1660–8.
Sleigh JW, Vacas S, Flexman AM, Talke PO. Electroencephalographic arousal patterns under dexmedetomidine sedation. Anesth Analg. 2018 Oct;127(4):951–9.
Drohan CM, Cardi AI, Rittenberger JC, Popescu A, Callaway CW, Baldwin ME, et al. Effect of sedation on quantitative electroencephalography after cardiac arrest. Resuscitation. 2018 Mar;124:132–7.
Noirhomme Q, Lehembre R, Lugo ZDR, Lesenfants D, Luxen A, Laureys S, et al. Automated analysis of background EEG and reactivity during therapeutic hypothermia in comatose patients after cardiac arrest. Clin EEG Neurosci. 2014;45:6–13.
Admiraal MM, van Rootselaar AF, Horn J. International consensus on EEG reactivity testing after cardiac arrest: towards standardization. Resuscitation. 2018 Oct;131:36–41.
• Ruijter BJ, van Putten MJAM, van de Bergh WM, et al. Propofol does not affect the reliability of early EEG for outcome prediction of comatose patients after cardiac arrest. Clin Neurophysiol. 2019;130:1263–70 In a prospective multicenter cohort study, Propofol induces changes of the postanoxic EEG were described and showed that those changes does not affect the value of EEG for the prediction of outcome.
Tiainen M, Kovala TT, Takkunen OS, Roine RO. Somatosensory and brainstem auditory evoked potentials in cardiac arrest patients treated with hypothermia. Crit Care Med. 2005;33(8):1736–40.
Leithner C, Ploner CJ, Hasper D, Storm C. Does hypothermia influence the predictive value of bilateral absent N20 after cardiac arrest? Neurology. 2010;74(12):965–9.
Maciel CB, Morawo AO, Tsao CY, Youn TS, Labar DR, Rubens EO, et al. SSEP in therapeutic hypothermia era. J Clin Neurophysiol. 2017;34(5):469–75.
• Amorim E, Ghassemi MM, Lee JW, et al. Estimating the false positive rate of absent somatosensory evoked potentials in cardiac arrest prognostication. Crit Care Med. 2018;46(12):e1213–21 In a systematic review based on 35 studies in cardiac arrest, prognostication that reported somatosensory evoked potentials, a statistical model was created to estimate the false positive rate for poor outcome after cardiac arrest.
Endisch C, Storm C, Ploner CJ, Leithner C. Amplitudes of SSEP and outcome in cardiac arrest survivors: a prospective cohort study. Neurology. 2015;85(20):1752–60.
Oh SH, Park KN, Choi SP, Oh JS, Kim HJ, Youn CS, et al. Beyond dichotomy: patterns and amplitudes of SSEPs and neurological outcomes after cardiac arrest. Crit Care. 2019;23(1):224.
Tiainen M, Roine RO, Pettilä V, Takkunen O. Serum neuron-specific enolase and S-100B protein in cardiac arrest patients treated with hypothermia. Stroke. 2003;34(12):2881–6.
Stammet P, Collignon O, Hassager C, Wise MP, Hovdenes J, Åneman A, et al. Neuron-specific enolase as a predictor of death or poor neurological outcome after out-of-hospital cardiac arrest and targeted temperature management at 33°C and 36°C. J Am Coll Cardiol. 2015;65(19):2104–14.
Duez CHV, Grejs AM, Jeppesen AN, Schrøder AD, Søreide E, Nielsen JF, et al. Neuron-specific enolase and S-100b in prolonged targeted temperature management after cardiac arrest: a randomised study. Resuscitation. 2018;122:79–86.
Stammet P, Dankiewicz J, Nielsen N, Fays F, Collignon O, Hassager C, et al. Protein S100 as outcome predictor after out-of-hospital cardiac arrest and targeted temperature management at 33 C and 36 C. Crit Care. 2017;21(1):153.
Zellner T, Gärtner R, Schopohl J, Angstwurm M. NSE and S-100B are not sufficiently predictive of neurologic outcome after therapeutic hypothermia for cardiac arrest. Resuscitation. 2013;84(10):1382–6.
Mlynash M, Buckwalter MS, Okada A, Caulfield AF, Venkatasubramanian C, Eyngorn I, et al. Serum neuron-specific enolase levels from the same patients differ between laboratories: assessment of a prospective post-cardiac arrest cohort. Neurocrit Care. 2013;19(2):161–6.
Luescher T, Mueller J, Isenschmid C, et al. Neuron-specific enolase (NSE) improves clinical risk scores for prediction of neurological outcome and death in cardiac arrest patients: results from a prospective trial. Resuscitation. 2019.
Gillick K, Rooney K. Serial NSE measurement identifies non-survivors following out of hospital cardiac arrest. Resuscitation. 2018;128:24–30.
•• Moseby-Knappe M, Mattsson N, Nielsen N, Zetterberg H, Blennow K, Dankiewicz J, et al. Serum neurofilament light chain for prognosis of outcome after cardiac arrest. JAMA Neurol. 2019;76(1):64–71. In a prospective clinical biobank study of data from the randomized Target Temperature Management after Cardiac Arrest trial, an international, multicenter study with 29 participating sites, at comparable specificities, serum NFL levels had greater sensitivity for poor outcome compared with routine electroencephalogram, somatosensory-evoked potentials, head computed tomography, and both pupillary and corneal reflexes.
Kim SH, Choi SP, Park KN, Youn CS, Oh SH, Choi SM. Early brain computed tomography findings are associated with outcome in patients treated with therapeutic hypothermia after out-of-hospital cardiac arrest. Scand J Trauma Resusc Emerg Med. 2013;21:57.
Metter RB, Rittenberger JC, Guyette FX, Callaway CW. Association between a quantitative CT scan measure of brain edema and outcome after cardiac arrest. Resuscitation. 2011;82(9):1180–5.
Wu O, Batista LM, Lima FO, Vangel MG, Furie KL, Greer DM. Predicting clinical outcome in comatose cardiac arrest patients using early noncontrast computed tomography. Stroke. 2011;42(4):985–92.
Hong JY, Lee DH, Oh JH. Grey-white matter ratio measured using early unenhanced brain computed tomography shows no correlation with neurological outcomes in patients undergoing targeted temperature management after cardiac arrest. Resuscitation. 2019;140:161–9.
Hirsch KG, Mlynash M, Eyngorn I, Pirsaheli R, Okada A, Komshian S, et al. Multi-center study of diffusion-weighted imaging in coma after cardiac arrest. Neurocrit Care. 2016;24(1):82–9.
Ryoo SM, Jeon SB, Sohn CH, Ahn S, Han C, Lee BK, et al. Predicting outcome with diffusion-weighted imaging in cardiac arrest patients receiving hypothermia therapy: multicenter retrospective cohort study. Crit Care Med. 2015;43(11):2370–7.
• Reynolds AS, Guo X, Matthews E, et al. Post-anoxic quantitative MRI changes may predict emergence from coma and functional outcomes at discharge. Resuscitation. 2017;117:87–90. Using a semi-automated algorithm to perform quantitative volumetric analysis of apparent diffusion coefficient (ADC) sequences at various thresholds, this single-center study showed MRI parameters to be superior in predicting failure to wake up from coma compared to bilateral absence of pupillary reflexes.
Greer D, Scripko P, Bartscher J, Sims J, Camargo E, Singhal A, et al. Clinical MRI interpretation for outcome prediction in cardiac arrest. Neurocrit Care. 2012;17(2):240–4.
Mlynash M, Campbell DM, Leproust EM, Fischbein NJ, Bammer R, Eyngorn I, et al. Temporal and spatial profile of brain diffusion-weighted MRI after cardiac arrest. Stroke. 2010;41(8):1665–72.
• Greer DM, Rosenthal ES, Wu O. Neuroprognostication of hypoxic-ischaemic coma in the therapeutic hypothermia era. Nat Rev Neurol. 2014;10(4):190–203. In this review, was discussed the data and its limitations for neuroimaging to date. Promising results from advanced neuroimaging techniques, and practical advice for the clinician caring for these patients in the real world were presented.
Extracorporeal Life Support Organization. ECLS registry report, international summary. Ann Arbor: Extracorporeal Life Support Organization; 2019.
•• Brodie D, Slutsky AS, Combes A. Extracorporeal life support for adults with respiratory failure and related indications: a review. JAMA. 2019;322(6):557–68. This review highlights the physiology and biology of extracorporeal support, and increased knowledge of how it might benefit the treatment of a variety of clinical conditions.
Nasr DM, Rabinstein AA. Neurologic complications of extracorporeal membrane oxygenation. J Clin Neurol. 2015;11(4):383–9.
Maekawa K, Tanno K, Hase M, Mori K, Asai Y. Extracorporeal cardiopulmonary resuscitation for patients with out-of-hospital cardiac arrest of cardiac origin: a propensity-matched study and predictor analysis. Crit Care Med. 2013;41:1186–96.
Lee JJ, Han SJ, Jin S, et al. Out-of-hospital cardiac arrest patients treated with cardiopulmonary resuscitation using extracorporeal membrane oxygenation: focus on survival rate and neurologic outcome. Scand J Trauma, Resusc Emerg Med. 2016;24:74.
• Miroz, JP, Solari D, Eckert, P, Oddo, M, Ben-Hamouda, N. Neurological Pupil Index for early neuroprognostication in ECMO patients. Conference: Proceedings of Réanimation 2018, The French Intensive Care Society international congress, at Paris (France), volume: annals of intensive care 2018, 8(Suppl 1): F-35. This conference paper for the first time showed pilot data on the feasibility and effectiveness of using quantitative pupillometry in cardiac arrest patients with ECMO.
Schumacher RE, Spak C, Kileny PR. Asymmetric brain stem auditory evoked responses in infants treated with extracorporeal membrane oxygenation. Ear Hear. 1990;11(5):359–62.
Amigoni A, Pettenazzo A, Biban P, Suppiej A, Freato F, Zaramella P, et al. Neurologic outcome in children after extracorporeal membrane oxygenation: prognostic value of diagnostic tests. Pediatr Neurol. 2005;32(3):173–9.
Streletz LJ, Bej MD, Graziani LJ, Desai HJ, Beacham SG, Cullen J, et al. Utility of serial EEGs in neonates during extracorporeal membrane oxygenation. Pediatr Neurol. 1992;8(3):190–6.
• Cho, Sung-Min, Wendy Ziai, Yunis Mayasi, Aaron M. Gusdon, Jennifer Creed, Matthew Sharrock, et. al. Noninvasive neurological monitoring in extracorporeal membrane oxygenation. ASAIO J, 2019. Through a small, single-center study optimal neurologic monitoring methods for cardiac arrest patients on ECMO were characterized.
Lidegram M, Palmer K, Joruf H, et al. CT in the evaluation of patients on ECMO due to acute respiratory failure. Pediatr Radiol. 2002;32:567–74.
Liu KL, et al. Multislice CT scans in patients on extracorporeal membrane oxygenation: emphasis on hemodynamic changes and imaging pitfalls. Korean J Radiol. 2014;15(3):322–9. https://doi.org/10.3348/kjr.2014.15.3.322.
Susana M. Bowling, Joao Gomes and Michael S. Firstenberg (September 14th 2016). Neurologic issues in patients receiving extracorporeal membrane oxygenation support, extracorporeal membrane oxygenation - advances in therapy, Michael S. Firstenberg, IntechOpen: https://doi.org/10.5772/64269.
Bembea MM, Rizkall N, Freedy J, et al. Plasma biomarkers of brain injury as diagnostic tools and outcome predictors after extracorporeal membrane oxygenation. Crit Care Med. 2015;43(10):2202–11.
Bembea MM, Savage W, Strouse JJ, Schwartz JM, Graham E, Thompson CB, et al. Glial fibrillary acidic protein as a brain injury biomarker in children undergoing extracorporeal membrane oxygenation. Pediatr Crit Care Med. 2011;12(5):572–9.
Gazzolo D, Masetti P, Meli M, Grutzfeld D, Michetti F. Elevated S100B protein as an early indicator of intracranial haemorrhage in infants subjected to extracorporeal membrane oxygenation. Acta Paediatr. 2002;91:218–21.
• Zhang Y, Li CS, Yuan XL, Ling JY, Zhang Q, Liang Y. Association of serum biomarkers with outcomes of cardiac arrest patients undergoing ECMO. Am J Emerg Med. 2018;36(11):2020–8 A systematic review and meta-analysis with 17 papers containing 903 cases of CA patients treated with ECMO, high serum lactate level was associated with poor survival and poor neurological outcome.
Wijdicks EF, Varelas PN, Gronseth GS, Greer DM, American Academy of Neurology. American academy of neurology: Evidence-based guideline update: determining brain death in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2010;74:1911–8.
• Bein T, Müller T, Citerio G. Determination of brain death under extracorporeal life support. Intensive Care Med. 2019;45(3):364–6. This review highlights the technical challenges associated with brain death declaration in ECMO patients, as brain death sometimes marks the end of strenuous therapeutic efforts.
Giani M, Scaravilli V, Colombo SM, Confalonieri A, Leo R, Maggioni E, et al. Apnea test during brain death assessment in mechanically ventilated and ECMO patients. Intensive Care Med. 2016;42(1):72–81.
Van der Jagt M, Lin MS, Briegel J. Optimizing apnea testing to determine brain death. Intensive Care Med. 2016 Jan;42(1):117–8.
• Sutter R, Tisljar K, Marsch S. Acute neurologic complications during extracorporeal membrane oxygenation: a systematic review. Crit Care Med. 2018;46(9):1506–13. In this systematic review, high occurrence rates of neurologic complications were reported, especially with venoarterial extracorporeal membrane oxygenation. Further highlighted was the low quality of evidence indicating the need for more high-quality studies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Sachin Agarwal, Nicholas Morris, Caroline Der-Nigoghossian, and Teresa May each declare no potential conflicts of interest.
Daniel Brodie reports a grant from ALung Technologies, personal fees from Baxter, and serves and/or served as a member of the Medical Advisory Boards for ALung Technologies, Hemovent, BREETHE, and Xenios.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Critical Care Neurology
Electronic supplementary material
Supplementary Table 1
(DOCX 14 kb)
Rights and permissions
About this article
Cite this article
Agarwal, S., Morris, N., Der-Nigoghossian, C. et al. The Influence of Therapeutics on Prognostication After Cardiac Arrest. Curr Treat Options Neurol 21, 60 (2019). https://doi.org/10.1007/s11940-019-0602-1
Published:
DOI: https://doi.org/10.1007/s11940-019-0602-1