Opinion statement
Sleep has a strong influence on interictal epileptiform discharges and on epileptic seizures. Interictal epileptiform discharges are activated by sleep deprivation and sleep, and some epilepsies occur almost exclusively during sleep. Treatment of sleep-related epilepsy should take in account the type of epileptic syndrome, the type of seizures, the patient characteristics, and also the pharmacokinetics of the drug. Proper characterization of the epilepsy is essential to choose appropriate antiepileptic drugs. Drugs effective in focal epilepsy may be used to treat benign genetic focal epilepsies such as rolandic epilepsy and other focal (frontal or not) sleep epilepsies. These include both classical (such as carbamazepine) and new (such as levetiracetam and lacosamide) antiepileptic drugs. Drug-resistant cases should be evaluated for epilepsy surgery, which may be efficacious in this setting. Valproate, lamotrigine, topiramate, levetiracetam, and perampanel are effective against generalized tonic-clonic seizures in genetic generalized epilepsies, which frequently happen on awakening. Risks of valproate should be considered before prescribing it to women of childbearing age. Specific syndromes such as ESES require specific treatment such as a combination of high dose steroids, benzodiazepines, levetiracetam, and even surgery when an epileptogenic lesion is present. Sleep disorders that may worsen epilepsy such as obstructive sleep apnea or insomnia should be adequately treated to improve seizure frequency. Adequate control of seizures during sleep (especially generalized tonic-clonic seizures) decreases risk of sudden unexpected death in epilepsy (SUDEP).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The fact that sleep has effects on epilepsy has been observed since the nineteenth century (1). Early studies observed that a significant number of seizures occur during sleep or during awakening, and this observation has been confirmed to the present day. Thus, there are some epilepsies in which seizures appear mainly or exclusively in this state (pure sleep epilepsy). Epilepsies whose seizures occur during awakening have been called “awake epilepsy”. Sleep has also a strong influence on seizure frequency and types and electroencephalogram abnormalities.
In this article, we will review the effects of sleep on epilepsy in general and on specific epileptic syndromes. We will also discuss the most appropriate treatment strategies for sleep-related seizures.
Effect of sleep on epilepsy
Effects of sleep on seizures and interictal epileptiform discharges (IEDs)
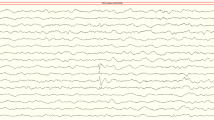
Sleep has an influence on seizures. It is accepted that non-REM sleep (NREM) is a facilitator of seizure activity, while REM sleep is a suppressor (2, 3). In NREM stage, epileptiform discharges increase in frequency and spreading. This phenomenon occurs as we move towards a deeper state of sleep, and presents in both generalized and focal epilepsies (4, 5), but seizures usually appears in stage 2 sleep (2, 3). One possible explanation of the increase of interictal discharges during NREM sleep is the progressive neuronal synchronizations that occur in deep sleep stages.
In REM sleep, both the frequency and the spread of interictal epileptiform discharges (IEDs) decrease. The extent and lateralization of IEDS is useful to localize the epileptogenic foci in refractory temporal lobe epilepsy (4, 6). In a recent study in children with generalized discharges in scalp EEG and normal/subtle changes in the MRI evaluated for epilepsy surgery, IEDs during REM helped to lateralize the epileptogenic hemisphere and proceed to surgery (7•). There is also a very low rate of seizures arising from REM sleep (3).
Sleep deprivation has long been recognized as a seizure precipitant, especially in patients with awakening epilepsies. This influence is not understood, but there is some evidence that sleep deprivation increases neuronal excitability (8). In a recent prospective study of a cohort of 104 patients, this was the second most frequent (71 % of cases) triggering factor for seizures, with the patients with generalized epilepsy being specially sensitive (9). Many other studies have also reported that sleep deprivation can precipitate EEG epileptiform discharges (10, 11), even in the absence of sleep during recordings (12). Comparative studies show that it activates epileptiform discharges in 23 to 93 % of patients with definite or suspected seizures (13).
Sleep deprivation has been used as a procedure for EEG activation. There is only one prospective study to show a specific effect on EEG. The authors reported 85 patients with suspected epilepsy to routine EEG, sleep-deprived EEG, and EEG during drug-induced sleep in a random order, and reported that sleep-deprived EEG was significantly more likely to show IEDs (14). In another recent study (15•), sleep-deprived EEG was more able to induce IEDs than routine EEG both in focal and generalized epilepsies. Using a sleep-deprived EEG as the first protocol in young patients with suspected epilepsy could reduce the number of EEGs requested in this population. Most authors advocate that the activating effect of IEDs of sleep-deprived EEG is a specific effect of deprivation, and not only sleep (16•, 17••).
Effect of sleep on epilepsy syndromes
There are a variety of epilepsies that are clearly related with sleep. These epilepsies are mainly the following:
West syndrome
This syndrome is characterized by infantile spasms and hypsarrhythmia on EEG, and usually starts between 3 and 12 months of age. The spasms are brief and usually occur in clusters. Seizures most commonly occur shortly after awakening. The characteristic high amplitude hypsarrhythmic EEG pattern is seen prominently in early NREM sleep (18) and, even more, can appear only in sleep (19). Recently, it has been shown that hypsarrhythmia impairs the physiological overnight decrease of slow waves in NREM sleep (20).
Lennox-Gastaut syndrome
This syndrome is characterized by the presence of tonic seizures, atypical absences, and tonic-clonic seizures. Typically, tonic seizures predominate during NREM sleep.
Benign epilepsy with centrotemporal spikes (BECTS)
This is the most frequent epilepsy in children (21). The onset is between 3 and 13 years, with remission before the age of 16 years (22). Seizures are characterized by hemifacial clonic and lateral clonic deviation of mouth and tongue with salivary flow. Approximately 70 % of seizures occur during sleep, early after falling asleep, or shortly before awakening. The syndrome, also known as benign rolandic epilepsy, is generally self-remitting, and prognosis is excellent. Interictal EEG is characterized by high-voltage centrotemporal spikes. Amplitude and frequency of IEDs increases during sleep.
Panayiotopoulos syndrome
It is another benign age-related genetic focal epilepsy. Almost two thirds of seizures occur while the patient is asleep. Seizures are characterized by nausea, emesis, other autonomic features, loss of consciousness, and eye and head deviation. Half of the seizures end up as a hemiconvulsion or generalized convulsion. Interictal EEG shows focal or multifocal spikes that appear or increase in frequency during sleep. Most frequent spikes are recorded from the occipital regions but also from other locations such as the centrotemporal area or the midline. Even irregular generalized spike and wave discharges may be seen. A few cases display no interictal epileptiform activity (23).
Prognosis is excellent and more than 75 % of patients achieve complete remission without treatment, within 1–2 years from onset (24).
Electrical status epilepticus during slow sleep (ESES)
It is an epileptic encephalopathy defined by the following features: (a) a continuous EEG activity consistent in spike-wave discharges during slow sleep; (b) frequent seizures; and (c) global cognitive regression (25••). The association with seizures and cognitive impairment has been made since early reports (26). Another term that has been used is “continuous spike-wave discharges during sleep” (CSWS). ESES results from the association of various seizures types, partial or generalized, occurring during sleep, and atypical absences during the awake state. The EEG pattern consists of continuous or almost continuous diffuse spike waves during non-REM sleep. It is an age-related syndrome with seizure onset between 2 months and 12 years, and a peak at 2–4 years (27). This could be due to the fact that childhood is the period in which slow waves are most prominent and synaptic density higher (28, 29). The absence of tonic seizures differentiates it from Lennox-Gastaut Syndrome. ESES is associated with cognitive and behavioral impairment, producing regression that can be acute or subacute (30).
About half of patients with ESES have malformations or cortical lesions (31). Pre or perinatal thalamic lesions have been associated with the ESES. Mutations have also been described in gene GRIN2A (32•, 33•). The pathophysiologic mechanism that triggers ESES is unknown. Cognitive impairment has attributed to the influence of continuous epileptiform activity during sleep, which does not allow adequate consolidation of memory during sleep (34). Processing of cortical information is disrupted by epileptiform activity (35). Similarly, some studies have established a correlation between neurocognitive deficits and the brain regions where EEG abnormalities are more frequent and dense (30, 36, 37). Two similar syndromes to ESES are also characterized by a specific increase in spike-wave during sleep: Landau-Kleffner syndrome, also known as acquired epileptic aphasia. Aphasia is due to hearing agnosia. Age of onset is between 3 and 9 years. Typically, there is an acute or gradual language regression, often with seizures. Sleep EEG may show continuous spikes and waves in NREM sleep (38). Spike and waves can be unilateral, lateralized, or diffuse (39, 40). There are no associated lesions on MRI and aphasia improves if the EEG normalizes, but language and cognitive deficits can persist.
The second variant is atypical benign partial epilepsy. These patients meet the criteria for benign partial epilepsy, but they have the continuous spike and wave EEG pattern during sleep. Besides focal motor seizures, atypical absences, myoclonic, and tonic seizures may occur (41). Cognition is preserved, but if mental retardation is present, the term “pseudo-Lennox-Gastaut” is used. EEG patterns and outcomes are similar to ESES.
Some authors consider these genetic or idiopathic focal epilepsies as a continuum, in which the rolandic epilepsy represents the mildest form, and ESES with this variants the most serious form (17••). To emphasize this hypothesis, mutations of the GRIN2A gene in BECTS, ESES, and Landau-Kleffner syndrome have been described (32•, 42, 43•). GRIN2A encodes the GLuN2A subunit of the NMDA receptor, that has important roles in synaptogenesis and synaptic plasticity (43•). According to some studies, these epilepsies may be associated with these mutations up to 10–20 % of cases (44, 45).
Genetic generalized epilepsies
Juvenile myoclonus epilepsy (JME)
It is also an age-related epilepsy and is clearly associated to sleep. Seizures occur after awakening from sleep or in the evening relaxation period and are facilitated by sleep deprivation and sudden arousal. JME is characterized by the presence of short myoclonic jerks, generally in the morning after awakening, without altered level of consciousness. The upper extremities are especially affected. The myoclonus may evolve to a generalized tonic-clonic seizure. Recently it was established that the presence of myoclonus is a requisite for the diagnosis of JME (46•). Absences and praxis-induced seizures can occur (47). The EEG shows spikes and widespread polyspikes and diffuse spike and wave at 2.5–3.5 Hz, increased at sleep onset and on awakening, but less frequent in NREM and REM sleep and during the awake state (48). Because sometimes the routine EEG is normal, it is recommended to perform a prolonged EEG with sleep deprivation. Epileptiform discharges on awakening are considered a marker of JME and other genetic or idiopathic generalized epilepsies (49).
Epilepsy with tonic-clonic seizures on awakening
This syndrome may occur independently or as a part of other idiopathic generalized epilepsy syndromes, as JME. Seizures occur after awakening or during evening relaxation (50).
Nocturnal frontal lobe epilepsy (NFLE)
This is a frontal lobe epilepsy in which more than 90 % of attacks occur during sleep (51). NFLE is an heterogeneous disease as idiopathic, sporadic, familial, or symptomatic forms exist (51–53).
The genetic form of NFLE is heterogeneous with autosomal dominant inheritance (ADNFLE). Most frequent mutations involve genes coding for subunits of the heteromeric neuronal nicotinic receptors (nAChRs). However, these mutations account for around 12 % of cases (54•). ADNLFE is very similar to sporadic NFLE, but some mutations are frequently associated with specific psychiatric symptoms. ADNLFE was the first epilepsy in which genetic basis was detected (52). Recently, a recessive form due to mutation in PRIMA1 gene has been described. PRIMA1 is a transmembrane protein which anchors acetylcholinesterase to neuron membranes, and the mutation causes increase in cholinergic responses (55•).
The most frequent etiology of symptomatic forms is type II focal cortical dysplasia (56).
NFLE usually begins before 20 years of age, with different types of seizures: (1) short-lasting stereotyped movements involving the limbs, axial musculature, or head (57, 58); (2) paroxysmal arousals that are sudden and brief (5–10 s), sometimes accompanied by stereotyped movements, vocalizations, frightened expression, or fear (51); and (3) major attacks, (20–30 s in duration), with tonic or dystonic posturing, or complex movements such as pelvic thrusting, pedaling, or more violent movements of limbs (51, 52, 57). Almost all seizures occur during NREM sleep. NFLE has been studied with special interest for its resemblance to NREM parasomnias (sleepwalking and night terrors). Nocturnal PSG with synchronized audiovisual recording is often normal in NFLE. If the diagnosis is unclear, the use of sphenoidal electrodes to record epileptiform activity can be helpful (59).
Other focal nocturnal epilepsies
Sleep-related complex motor seizures are not necessarily frontal in all occasions. They may also originate from the temporal lobe (60, 61), the insula (62), and the posterior regions (63). In these cases, auras can help to differentiate them from NFLE (64).
A nocturnal temporal lobe epilepsy has been described, but is uncommon (65).
Primary sleep disturbances and epilepsy
Excessive daytime sleepiness is the most common sleep complaint in patients with epilepsy (66•). The origin is multifactorial, the most common being an adverse effect of antiepileptic drugs (AED) and sleep disorders that frequently coexist with epilepsy, such as insufficient nighttime sleep and obstructive sleep apnea (OSA) (67). Excessive daytime sleepiness affects negatively the quality of life of patients with epilepsy.
Obstructive sleep apnea is a primary sleep disorder, and is one of the most frequent in patients with epilepsy. The prevalence of OSA in patients with epilepsy exceeds that of the general population and is even more frequent in patients with drug-resistant epilepsy (68). Risk factors are the same than in general population: older age, male sex, and increased body mass index (69). A recent study found that, in a regression model, only age, dental problems, and standardized AED dose are predictors of OSA (66•). The pathophysiology of OSA in patients with epilepsy however still remains unknown. Total load of AEDs (especially of some such as benzodiazepines) may decrease upper airway tone; in addition, the epileptic discharges and/or seizures could alter upper airway control during sleep. However, this hypothesis remains untested (66•). The Sleep Apnea Scale of the Sleep Disorders Questionnaire has shown validity as a screening instrument for the diagnosis of OSA in adults with epilepsy (70). OSA causes sleep deprivation because it results in fragmented sleep. OSA has been associated with poor control of seizures (69, 71).
Association between NREM sleep parasomnias (sleepwalking and night terrors) and NFLE is unclear, because both conditions are often difficult to distinguish on clinical grounds and PSG findings may be unclear.
REM sleep behavior disorder (RBD) is a parasomnia characterized by abnormal and often violent motor behaviors and complex vocalizations in which patients seem to enact their dreams while in REM sleep (72••). RBD can be misdiagnosed as sleep-related epilepsy. In addition, elderly patients with epilepsy may have RBD (73).
Sudden unexpected death in epilepsy (SUDEP)
Premature death among patients with epilepsy is higher than in the general population, and SUDEP is the most common cause of this mortality. This is defined as the sudden, unexpected, witnessed or unwitnessed, non-traumatic, and non-drowning death in an individual with epilepsy, with or without evidence of a seizure, and excluding documented status epilepticus, in which the autopsy does not reveal a toxicological or anatomic cause of death (74). Recent studies estimate 7000 deaths per year in Europe and USA (75) due to SUDEP. The risk of sudden unexpected death is considered to be 24–40 times higher than general population (76, 77). The cause of SUDEP is unknown, but several risk factors have been reported: poor seizure control, frequent tonic-clonic seizures, and long-standing epilepsy (78, 79). Deaths are typically unwitnessed, and associated with prone position (80), especially in individuals 40 or younger (81). Nocturnal seizures seem to be an independent risk factor for SUDEP: in a study of 154 patients who died of SUDEP, it was primarily a sleep-related (in 58 % of patients) and unwitnessed (86 %) event (82•). Several studies point out that SUDEP usually happens during sleep (83–87). Postmortem, half of the patients are found to have subtherapeutic levels of AEDs and most display evidence of a recent seizure (tongue injury, petechial hemorrhages in the skin, superior vena cava distribution, or conjunctiva) (74).
One study aimed to assess if NFLE could be a risk factor for SUDEP that included 103 patients showed that the incidence of SUDEP was not higher than the rates previously reported in prevalent epilepsy populations (88•), perhaps because of the low incidence of GTC seizures in this type of epilepsy. Some hypotheses that could explain the relationship between SUDEP and sleep are the autonomic changes that occur during sleep, both physiologically and those produced by seizures and the presence of other sleep disorders such as OSA (89).
SUDEPs reported in epilepsy monitoring units show combined cardiac and respiratory failure after a generalized tonic-clonic seizure (90••). Prolonged postictal generalized EEG suppression has been described in all observed cases of SUDEP in monitoring units (90••). This pattern correlates with respiratory depression and autonomic dysfunction (91, 92). To improve the knowledge about SUDEP in order to establish preventing strategies and diminish SUDEP incidence, a new multicenter collaborative research consortium is ongoing (75).
Night supervision, use of monitoring devices, treatment of sleep comorbidities (89, 90••), or avoiding prone position (81) could reduce the occurrence of this dreadful complication of epilepsy.
Treatment of sleep-related epilepsies and sleep-related seizures (Table 1)
Specific literature on treatment of sleep-related epilepsy is scarce. Possible reasons include the fact that pure sleep epilepsies are relatively uncommon and for the rest, which combine diurnal and nocturnal seizures in variable proportions, differential responses of diurnal and nocturnal seizures are often not studied or reported. Efficacy of antiepileptic drugs is assumed to be similar in sleep or a wake seizures, when that may not be necessarily the case.
In addition, objective measurement of nocturnal seizures is difficult due to the need to perform PSG to exclude subtle seizures which may not be noticed by the patient or the caregiver. This fact limits the possibility to perform randomized controlled studies. We will review the current treatment strategies in the types of epilepsies presenting mainly during sleep.
Genetic focal epilepsies
In general, no antiepileptic treatment is recommended in patients with benign epilepsy with centrotemporal spikes (rolandic epilepsy) and infrequent nocturnal seizures without secondary generalization, and the same may be applied to Panayotopoulos syndrome or idiopathic occipital lobe epilepsy. The extent of EEG abnormalities does not correlate with seizure frequency or prognosis, and so it should not be used to take treatment decisions. Antiepileptic drugs may be considered in case of frequent seizures, occasional generalization, or extreme family anxiety. During many years, carbamazepine has been the drug of choice in rolandic epilepsy. Another option is oxcarbazepine (93). Valproate may be used in the minority of patients (around 10–20 %) who fail carbamazepine (94). There have been some reports associating carbamazepine to atypical negative evolutions, increasing the frequency of epileptiform discharges and producing temporary cognitive symptoms, although evidence is inconclusive (95–97). Sulthiame has been reported to be effective (98), even more than carbamazepine (99), decreasing epileptiform activity and improving cognition (100).
Levetiracetam monotherapy is also effective and well tolerated in patients with rolandic epilepsy who need treatment, (101). It seems to be as efficacious as valproic acid to control seizures (102•).
Continuous spike and wave during sleep (ESES)
In this pediatric syndrome with epileptic discharges highly activated by sleep, treatment is directed to reduce epileptiform discharges during sleep, as this may translate into cognitive improvement. However, there is no standard regimen and different combinations are used in different centers, as no controlled clinical trials have been conducted to establish the efficacy of various AEDs. For this reason, evidence to guide therapeutic decisions is only class III (open-label uncontrolled trials) or class IV (case reports or expert opinion).
High dose benzodiazepines (usually clobazam) and corticosteroids have been used to diminish EEG abnormalities and improve cognition and behavior, which has been shown to be associated with the duration of ESES (103). Drowsiness associated to benzodiazepines may limit their usefulness in this particular syndrome. Corticosteroids are reserved for drug-resistant cases associated to cognitive regression because of the side effect profile. In a series of 44 patients with ESES treated with oral hydrocortisone (initial dose 5 mg/kg/day in the first month) with a progressive weaning and a total duration of corticosteroid treatment of 21 months, 75 % of patients responded in the first 3 months but only 45 % were long-term responders (104). High dose valproate (associated to ethosuximide in those patients initially not responding) has been reported to improve EEG pattern in more than 50 % of patients (105). Other possible alternative treatments are sulthiame and lamotrigine.
Of the new drugs, add on therapy with levetiracetam has been shown to improve EEG or cognition in more than 50 % of the patients, although some of the initial responders may later relapse. A better response has been described in those patients with ESES and underlying structural lesions (106, 107). Another options for patients who are resistant to conventional AEDs and corticosteroids is the ketogenic diet, which may cause some improvement in the EEG in a minority of patients (108).
Multiple subpial transections, a surgical procedure which is sometimes performed to treat language regression in Landau-Kleffner syndrome, may have some positive effect over cognition and behavior in patients with ESES. (109••). If the patient displays a clear-cut lesion in the MRI and the presurgical evaluation is concordant, other surgical procedures such as hemispherectomy or focal resections may be considered.
A recent study performed a pooled analysis of 112 articles including 950 treatments in 575 patients (110). Antiepileptic drugs were associated with improvement (i.e., cognition or decrease of EEG discharges) in 49 % of patients, benzodiazepines in 68 %, and steroids (n = 166) in 81 %. Surgery resulted in improvement in 90 % of patients. In a subgroup analysis of patients who were consecutively reported, the authors found improvement in a smaller proportion treated with AEDs (34 %), benzodiazepines (59 %), and steroids (75 %), whereas the improvement percentage after surgery was preserved (93 %). Possible predictors of improved outcome were treatment category, normal development before ESES onset, and the absence of structural abnormalities (110).
Lennox-Gastaut syndrome
Tonic seizures during sleep which are a hallmark of Lennox-Gastaut syndrome and occur in over 90 % of patients. Tonic status during sleep is a very difficult to treat severe complication of this syndrome, and sometimes it is the result of treating other seizure types with high doses of intravenous benzodiazepines (111, 112).
Genetic generalized epilepsies
In general, seizures in idiopathic or genetic generalized epilepsies occur on awakening. In particular, the syndromes of juvenile myoclonic epilepsy and epilepsy with generalized tonic-clonic seizures (GTC) on awakening. Seizures occur more frequently after nights of sleep deprivation and alcohol intake. As these types of syndromes are seen preferentially in young patients, it is mandatory to stress the importance of therapeutic compliance, to recommend lifestyle with regular wake-sleep rhythm and to avoid sudden awakenings.
Valproic acid is still the most effective drug against the different types of seizures seen in idiopathic generalized epilepsies. However, careful assessment of risk-benefit ratio is required when valproate is prescribed to women of childbearing age, given its teratogenic potential and the negative impact on the psychosocial development of children exposed in utero to this drug (113••).
Other drugs that may be used in this population are lamotrigine (may exacerbate myoclonus in some patients) (114), topiramate (effective in GTC seizures) (115), levetiracetam (effective in myoclonic and GTC seizures) (116, 117), zonisamide (evidence in absences, myoclonus, and GTC shown in small open series only) (118), and perampanel (efficacy in GTC) (119, 120•).
Some antiepileptic drugs should not be used in these types of epilepsy because they either do not work or exacerbate seizure types other than GTC seizures, that is, absence and myoclonic seizures. These include carbamazepine, oxcarbazepine, phenytoin, gabapentin, and tiagabine (119).
Pharmacokinetics of the drug may be used to adjust the time of maximum expected concentration to the habitual time of seizure occurrence. Extended-release formulations may be used to delay time of maximum serum concentration of the drug. An occasional extra dose of a benzodiazepine can be used at bedtime if the patient has been sleep-deprived.
Only a minority of patients with idiopathic or genetic generalized epilepsy will present with generalized tonic-clonic seizures restricted exclusively to sleep. In these cases a frontal origin of the seizures should be ruled out.
Frontal and other focal sleep epilepsies
Antiepileptic drugs
The majority of pure sleep epilepsies are focal epilepsies (121), frequently non-lesional and often with a relatively benign outcome and good response to antiepileptic drugs. Focal seizures occurring mainly during sleep are usually frontal in origin, although other seizure onset zones may be possible. Nocturnal temporal lobe epilepsy is uncommon.
Treatment should be done with drugs which are effective in focal epilepsies.
Carbamazepine, oxcarbazepine, and topiramate are useful drugs in patients with frontal and other focal sleep epilepsies (51, 122–125).
Specific treatments such as acetazolamide can be used in the 30 % of patients with the genetic autosomal dominant frontal lobe epilepsy who do not respond to carbamazepine (52).
Some studies have shown potential usefulness of nicotine patches in some patients (126). Among new antiepileptic drugs, lacosamide seems to be also efficacious in patients with focal epilepsy and nocturnal seizures, with up to 65 % of patients with nocturnal drug-resistant seizures experiencing more than 50 % of seizure reduction in a retrospective study (127).
Surgical treatment of focal sleep-related epilepsy
Focal sleep epilepsy may be drug resistant. When the patient has failed two trials of appropriately given AEDs, he is considered to have drug-resistant epilepsy and surgical options should be considered taking into account the individual features of the epilepsy and the patient.
In a recent study (128•), the outcome of 95 patients with refractory sleep epilepsy who underwent presurgical evaluation and focal resection was analyzed. Most patients (61 %) had frontal lobe epilepsy, as expected, but up to 39 % underwent extrafrontal resection because of presumed seizure onset outside the frontal lobes. Most patients (almost 80 %) had a lesion in the MRI and the majority required invasive studies. 76 % of the patients, after a mean follow up of 82 months, were seizure free. Positive MRI findings, no need for invasive monitoring, complete removal of the epileptogenic zone, and cortical dysplasia type II in the pathology were associated with a good outcome. Cortical dysplasia type I was associated with seizure recurrence. The authors concluded that drug-resistant focal sleep epilepsy is cured with surgery in up to two thirds of cases including those not arising from the frontal lobe (128•).
Chronopharmacology in sleep epilepsies
Basic principles of chronopharmacology can be applied to treatment of sleep-related epilepsy. In a pilot trial (129), 18 patients with nocturnal or early-morning seizures refractory to conventional AED therapy were prospectively enrolled in a differential dosing trial. Patients were treated with a schedule in which the evening dose was twice the morning dose, keeping the total dose of medication constant. Of the 18 patients treated by this dosing strategy, 11 patients became seizure free following a mean follow up time of 5.3 months, and 4 patients had a 75–90 % reduction of seizures. This study suggested that chronotherapy can provide improved seizure control compared with conventional therapy in selected patients.
If seizures tend to occur during the transition from wakefulness to sleep, immediate release formulations can be more effective than extended-release ones, who would be more efficacious in seizures happening later at night or during sleep-wakefulness transition.
Treatment of factors that may worsen sleep-related epilepsy
Several studies have shown that OSA treatment with CPAP decreases interictal epileptiform activity and improves seizure control (130–132). Surgical treatment of OSA in children is also associated with decrease in seizure frequency, especially in those with elevated body mass index scores and younger age at time of surgery (133•). Based on these findings, some authors propose the implementation of OSA screening in adult epilepsy clinics, especially in patients with poor seizure control (66•, 134).
Insomnia is frequent in adults with epilepsy, being present in up to 40–55 % of patients (135, 136). It is correlated with number of AEDs and higher scores on depression scales. In patients with epilepsy and insomnia, melatonin can be used. However, its effect on seizure frequency is unclear. One study reported improvement in seizure frequency (137•), while other randomized placebo-controlled studies reported better sleep but no change in interictal epileptiform discharges or seizure frequency (138•). More research will be needed to evaluate the efficacy of melatonin for epilepsy.
Effect of epilepsy treatments on sleep
A different range of effects of antiepileptic drugs on sleep architecture have been described, including reduced sleep onset latency (phenobarbital, phenytoin, gabapentin), reduced arousals from sleep (phenobarbital, gabapentin), increase in slow-wave sleep (pregabalin, carbamazepine, and gabapentin), decrease in slow-wave sleep (levetiracetam, ethosuximide), and increase (ethosuximide, gabapentin) or decrease (phenobarbital, phenytoin) in REM sleep (139, 140). Several non-pharmacological epilepsy treatments for drug-resistant epilepsy (ketogenic diet, successful epilepsy surgery, and vagal nerve stimulator) have been reported to improve sleep quality. However it is unclear how much of this effect is due to improvement in seizure frequency.
Some epilepsy treatments, however, may have a negative impact on sleep disorders. In some patients, vagal nerve stimulator may worsen OSA (141). This complication can be treated with changes in the operational parameters of the device or with the use of CPAP.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Gowers W. Epilepsy and other chronic convulsive disorders. London: William Wood; 1885.
Minecan D, Natarajan A, Marzec M, Malow B. Relationship of epileptic seizures to sleep stage and sleep depth. Sleep. 2002;25:899–904.
Herman ST, Walczak TS, Bazil CW. Distribution of partial seizures during the sleep–wake cycle: differences by seizure onset site. Neurology. 2001;56:1453–9.
Sammaritano M, Gigli GL, Gotman J. Interictal spiking during wakefulness and sleep and the localization of foci in temporal lobe epilepsy. Neurology. 1991;41:290–7.
Malow BA, Lin X, Kushwaha R, Aldrich MS. Interictal spiking increases with sleep depth in temporal lobe epilepsy. Epilepsia. 1998;39:1309–16.
Malow BA, Bowes RJ, Lin X. Predictors of sleepiness in epilepsy patients. Sleep. 1997;20:1105–10.
Okanari K, Baba S, Otsubo H, et al. Rapid eye movement sleep reveals epileptogenic spikes for resective surgery in children with generalized interictal discharges. Epilepsia. 2015;56:1445–53. This article highlights the importance of sleep recording to lateralize the irritative zone in patients with generalized discharges, who can then become surgical candidates.
Badawy RA, Curatolo JM, Newton M, Berkovic SF, Macdonell RA. Sleep deprivation increases cortical excitability in epilepsy: syndrome-specific effects. Neurology. 2006;67:1018–22.
Ferlisi M, Shorvon S. Seizure precipitants (triggering factors) in patients with epilepsy. Epilepsy Behav. 2014;33:101–5.
Rajna P, Veres J. Correlations between night sleep duration and seizure frequency in temporal lobe epilepsy. Epilepsia. 1993;34:574–9.
Fountain NB, Kim JS, Lee SI. Sleep deprivation activates epileptiform discharges independent of the activating effects of sleep. J Clin Neurophysiol. 1998;15:69–75.
Ellingson RJ, Wilken K, Bennett DR. Efficacy of sleep deprivation as an activation procedure in epilepsy patients. J Clin Neurophysiol. 1984;1:83–101.
Foldvary-Schaefer N, Grigg-Damberger M. Sleep and epilepsy: what we know, don’t know, and need to know. J Clin Neurophysiol. 2006;23:4–20.
Leach JP, Stephen LJ, Salveta C, Brodie MJ. Which electroencephalography (EEG) for epilepsy? The relative usefulness of different EEG protocols in patients with possible epilepsy. J Neurol Neurosurg Psychiatry. 2006;77:1040–2.
Giorgi FS, Perini D, Maestri M, et al. Usefulness of a simple sleep-deprived EEG protocol for epilepsy diagnosis in de novo subjects. Clin Neurophysiol. 2013;124:2101–7. This study analyzes the yield of sleep deprived EEG in patients with suspected seizures (focal or generalized) and normal baseline EEG.
Giorgi FS, Guida M, Caciagli L, et al. What is the role for EEG after sleep deprivation in the diagnosis of epilepsy? Issues, controversies, and future directions. Neurosci Biobehav Rev. 2014;47:533–48. This article review the usefulness of sleep-deprived EEG in the diagnosis of epilepsy, discussing critically the availabe literature on the subject.
Schmitt B. Sleep and epilepsy syndromes. Neuropediatrics. 2015;46:171–80. This is a well structured and complete review on the influence of sleep on epilepsy syndromes.
Guerrini R, Pellock JM. Age-related epileptic encephalopathies. Handb Clin Neurol. 2012;107:179–93.
Watanabe K, Negoro T, Aso K, Matsumoto A. Reappraisal of interictal electroencephalograms in infantile spasms. Epilepsia. 1993;34:679–85.
Fattinger S, Schmitt B, Bolsterli Heinzle BK, Critelli H, Jenni OG, Huber R. Impaired slow wave sleep downscaling in patients with infantile spasms. Eur J Paediatr Neurol. 2015;19:134–42.
Lerman P. Benign partial epilepsies with centro-temporal spikes. In: Roger J, Dravet C, Bureau M, Dreifuss F, Wolf P, editors. Epileptic syndromes in infancy, childhood and adolescence. London: John Libbey Eurotext; 1985. p. 150–8.
Proposal for classification of epilepsies and epileptic syndromes. Commission on classification and terminology of the international league against epilepsy. Epilepsia. 1985;26:268–78.
Koutroumanidis M. Panayiotopoulos syndrome: an important electroclinical example of benign childhood system epilepsy. Epilepsia. 2007;48:1044–53.
Panayiotopoulos CP, Michael M, Sanders S, Valeta T, Koutroumanidis M. Benign childhood focal epilepsies: assessment of established and newly recognized syndromes. Brain. 2008;131:2264–86.
Sanchez FI, Chapman K, Peters JM, et al. Treatment for continuous spikes and waves during sleep (CSWS): survey on treatment choices in North America. Epilepsia. 2014;55:1099–108. This study reports the results of a survey about the different drugs and doses used to treat CSWS (valproate, corticosteroids, benzodiazepines, etc) and the goals of the treatment in North America.
Patry G, Lyagoubi S, Tassinari CA. Subclinical “electrical status epilepticus” induced by sleep in children. A clinical and electroencephalographic study of six cases. Arch Neurol. 1971;24:242–52.
Tassinari C. Electrical status epilepticus during sleep (ESE or CSWS) including acquired epileptic aphasia (Landau-Kleffner syndrome). In: Roger J, Bureau M, Dravet C, Genton P, Tassinari C, Wolf P, editors. Epileptic syndromes in infancy, childhood and adolescence. London: John Libbey Eurotext LTd; 2005. p. 295–314.
Kurth S, Jenni OG, Riedner BA, Tononi G, Carskadon MA, Huber R. Characteristics of sleep slow waves in children and adolescents. Sleep. 2010;33:475–80.
Huttenlocher PR, Dabholkar AS. Regional differences in synaptogenesis in human cerebral cortex. J Comp Neurol. 1997;387:167–78.
Roulet PE, Davidoff V, Despland PA, Deonna T. Mental and behavioural deterioration of children with epilepsy and CSWS: acquired epileptic frontal syndrome. Dev Med Child Neurol. 1993;35:661–74.
Galanopoulou AS, Bojko A, Lado F, Moshe SL. The spectrum of neuropsychiatric abnormalities associated with electrical status epilepticus in sleep. Brain Dev. 2000;22:279–95.
Lemke JR, Lal D, Reinthaler EM, et al. Mutations in GRIN2A cause idiopathic focal epilepsy with rolandic spikes. Nat Genet. 2013;45:1067–72. This study reports the finding of alterations of the gene encoding the NMDA receptor subunit NR2A as an important risk factor for idopathic focal epilepsies, especially in patients with more severe phenotypes.
Carvill GL, Regan BM, Yendle SC, et al. GRIN2A mutations cause epilepsy-aphasia spectrum disorders. Nat Genet. 2013;45:1073–6. This study reports the finding of GRIN2A mutations in families with aphasia epilepsy syndromes, establishing the genetic basis for some of these patients.
Diekelmann S, Born J. The memory function of sleep. Nat Rev Neurosci. 2010;11:114–26.
Kleen JK, Scott RC, Holmes GL, et al. Hippocampal interictal epileptiform activity disrupts cognition in humans. Neurology. 2013;81:18–24.
LANDAU WM, KLEFFNER FR. Syndrome of acquired aphasia with convulsive disorder in children. Neurology. 1957;7:523–30.
Veggiotti P, Beccaria F, Guerrini R, Capovilla G, Lanzi G. Continuous spike-and-wave activity during slow-wave sleep: syndrome or EEG pattern? Epilepsia. 1999;40:1593–601.
Van BP, King MD, Paquier P, et al. Acquired auditory agnosia in childhood and normal sleep electroencephalography subsequently diagnosed as Landau-Kleffner syndrome: a report of three cases. Dev Med Child Neurol. 2013;55:575–9.
Caraballo RH, Cejas N, Chamorro N, Kaltenmeier MC, Fortini S, Soprano AM. Landau-Kleffner syndrome: a study of 29 patients. Seizure. 2014;23:98–104.
Deonna TW. Acquired epileptiform aphasia in children (Landau-Kleffner syndrome). J Clin Neurophysiol. 1991;8:288–98.
Aicardi J, Chevrie JJ. Atypical benign partial epilepsy of childhood. Dev Med Child Neurol. 1982;24:281–92.
Conroy J, McGettigan PA, McCreary D, et al. Towards the identification of a genetic basis for Landau-Kleffner syndrome. Epilepsia. 2014;55:858–65.
Marwick K, Skehel P, Hardingham G, Wyllie D. Effect of a GRIN2A de novo mutation associated with epilepsy and intellectual disability on NMDA receptor currents and Mg(2+) block in cultured primary cortical neurons. Lancet. 2015;385 Suppl 1:S65. This study reports the effects of the disease associated mutation GluN2A(N615K) on the function of the NMDA receptor and NMDA current density, with possible pathogenic effect.
Lesca G, Rudolf G, Bruneau N, et al. GRIN2A mutations in acquired epileptic aphasia and related childhood focal epilepsies and encephalopathies with speech and language dysfunction. Nat Genet. 2013;45:1061–6.
Lal D, Steinbrucker S, Schubert J, et al. Investigation of GRIN2A in common epilepsy phenotypes. Epilepsy Res. 2015;115:95–9.
Kasteleijn-Nolst Trenite DG, Schmitz B, Janz D, et al. Consensus on diagnosis and management of JME: from founder’s observations to current trends. Epilepsy Behav. 2013;28 Suppl 1:S87–90. This is an interesting expert consensus on diagnostic criteria for JME and updated guidelines on treatment, published after an international workshop.
Mayer TA, Schroeder F, May TW, Wolf PT. Perioral reflex myoclonias: a controlled study in patients with JME and focal epilepsies. Epilepsia. 2006;47:1059–67.
Zambrelli E, Canevini MP. Pre- and post-dormitum epilepsies: idiopathic generalized epilepsies. Sleep Med. 2011;12 Suppl 2:S17–21.
Fittipaldi F, Curra A, Fusco L, Ruggieri S, Manfredi M. EEG discharges on awakening: a marker of idiopathic generalized epilepsy. Neurology. 2001;56:123–6.
Janz D. Epilepsy with grand mal on awakening and sleep-waking cycle. Clin Neurophysiol. 2000;111 Suppl 2:S103–10.
Provini F, Plazzi G, Tinuper P, Vandi S, Lugaresi E, Montagna P. Nocturnal frontal lobe epilepsy. A clinical and polygraphic overview of 100 consecutive cases. Brain. 1999;122(Pt 6):1017–31.
Combi R, Dalpra L, Tenchini ML, Ferini-Strambi L. Autosomal dominant nocturnal frontal lobe epilepsy—a critical overview. J Neurol. 2004;251:923–34.
Scheffer IE, Bhatia KP, Lopes-Cendes I, et al. Autosomal dominant nocturnal frontal lobe epilepsy. A distinctive clinical disorder. Brain. 1995;118(Pt 1):61–73.
Becchetti A, Aracri P, Meneghini S, Brusco S, Amadeo A. The role of nicotinic acetylcholine receptors in autosomal dominant nocturnal frontal lobe epilepsy. Front Physiol. 2015;6:22. The article discusses some possible pathogenetic mechanisms of ADFLE in the light of recent advances about the nAChR role in different cerebral regions.
Hildebrand MS, Tankard R, Gazina EV, et al. PRIMA1 mutation: a new cause of nocturnal frontal lobe epilepsy. Ann Clin Transl Neurol. 2015;2:821–30. The article reports a newly discovered mutation in a family with nocturnal frontal lobe epilepsy and recessive inheritance.
Blumcke I, Thom M, Aronica E, et al. The clinicopathologic spectrum of focal cortical dysplasias: a consensus classification proposed by an ad hoc Task Force of the ILAE Diagnostic Methods Commission. Epilepsia. 2011;52:158–74.
Oldani A, Zucconi M, Asselta R, et al. Autosomal dominant nocturnal frontal lobe epilepsy. A video-polysomnographic and genetic appraisal of 40 patients and delineation of the epileptic syndrome. Brain. 1998;121(Pt 2):205–23.
Halasz P, Kelemen A, Szucs A. The role of NREM sleep micro-arousals in absence epilepsy and in nocturnal frontal lobe epilepsy. Epilepsy Res. 2013;107:9–19.
Tinuper P, Cerullo A, Cirignotta F, Cortelli P, Lugaresi E, Montagna P. Nocturnal paroxysmal dystonia with short-lasting attacks: three cases with evidence for an epileptic frontal lobe origin of seizures. Epilepsia. 1990;31:549–56.
Mai R, Sartori I, Francione S, et al. Sleep-related hyperkinetic seizures: always a frontal onset? Neurol Sci. 2005;26 Suppl 3:s220–4.
Nobili L, Cossu M, Mai R, et al. Sleep-related hyperkinetic seizures of temporal lobe origin. Neurology. 2004;62:482–5.
Proserpio P, Cossu M, Francione S, et al. Insular-opercular seizures manifesting with sleep-related paroxysmal motor behaviors: a stereo-EEG study. Epilepsia. 2011;52:1781–91.
Proserpio P, Cossu M, Francione S, et al. Epileptic motor behaviors during sleep: anatomo-electro-clinical features. Sleep Med. 2011;12 Suppl 2:S33–8.
Nobili L, Francione S, Cardinale F, Lo RG. Epileptic nocturnal wanderings with a temporal lobe origin: a stereo-electroencephalographic study. Sleep. 2002;25:669–71.
Bernasconi A, Andermann F, Cendes F, Dubeau F, Andermann E, Olivier A. Nocturnal temporal lobe epilepsy. Neurology. 1998;50:1772–7.
Foldvary-Schaefer N, Andrews ND, Pornsriniyom D, Moul DE, Sun Z, Bena J. Sleep apnea and epilepsy: who’s at risk? Epilepsy Behav. 2012;25:363–7. This study reports the OSA predictors in patients unselected for epilepsy severity and sleep disorder symptoms. Its results support the routine OSA screening in adult epilepsy clinics.
Malow BA. The interaction between sleep and epilepsy. Epilepsia. 2007;48 Suppl 9:36–8.
Malow BA, Levy K, Maturen K, Bowes R. Obstructive sleep apnea is common in medically refractory epilepsy patients. Neurology. 2000;55:1002–7.
Manni R, Terzaghi M, Arbasino C, Sartori I, Galimberti CA, Tartara A. Obstructive sleep apnea in a clinical series of adult epilepsy patients: frequency and features of the comorbidity. Epilepsia. 2003;44:836–40.
Economou NT, Dikeos D, Andrews N, Foldvary-Schaefer N. Use of the sleep apnea scale of the sleep disorders questionnaire (SA-SDQ) in adults with epilepsy. Epilepsy Behav. 2014;31:123–6.
Chihorek AM, Bou-Khalil B, Malow BA. Obstructive sleep apnea is associated with seizure occurrence in older adults with epilepsy. Neurology. 2007;69:1823–7.
Iranzo A, Santamaria J, Tolosa E. Idiopathic rem sleep behaviour disorder: diagnosis, management and research implications. Lancet Neurol. 2016. A very recent and thorough review of RBD by well known experts in the field.
Manni R, Terzaghi M, Zambrelli E. REM sleep behaviour disorder in elderly subjects with epilepsy: frequency and clinical aspects of the comorbidity. Epilepsy Res. 2007;77:128–33.
Clark D, Riney K. A population-based post mortem study of sudden unexpected death in epilepsy. J Clin Neurosci. 2016;23:58–62.
Lhatoo S, Noebels J, Whittemore V. Sudden unexpected death in epilepsy: identifying risk and preventing mortality. Epilepsia. 2015;56:1700–6.
Ficker DM. Sudden unexplained death and injury in epilepsy. Epilepsia. 2000;41 Suppl 2:S7–12.
Ficker DM, So EL, Shen WK, et al. Population-based study of the incidence of sudden unexplained death in epilepsy. Neurology. 1998;51:1270–4.
Scorza CA, Cavalheiro EA, Scorza FA. SUDEP research: challenges for the future. Epilepsy Behav. 2013;28:134–5.
Surges R, Thijs RD, Tan HL, Sander JW. Sudden unexpected death in epilepsy: risk factors and potential pathomechanisms. Nat Rev Neurol. 2009;5:492–504.
Hesdorffer DC, Tomson T, Benn E, et al. Combined analysis of risk factors for SUDEP. Epilepsia. 2011;52:1150–9.
Harden CL. SUDEP prevention “position statement”. Epilepsy Curr. 2015;15:321–2.
Lamberts RJ, Thijs RD, Laffan A, Langan Y, Sander JW. Sudden unexpected death in epilepsy: people with nocturnal seizures may be at highest risk. Epilepsia. 2012;53:253–7. This study compares living controls with patients who died of SUDEP (confirmed autopsy) to find out predictive factors regarding seizure frequency and presentation. Nocturnal seizures were an indepenent predictor for SUDEP.
Khiari HM, Franceschetti S, Jovic N, Mrabet A, Genton P. Death in Unverricht-Lundborg disease. Neurol Sci. 2009;30:315–8.
Weber P, Bubl R, Blauenstein U, Tillmann BU, Lutschg J. Sudden unexplained death in children with epilepsy: a cohort study with an eighteen-year follow-up. Acta Paediatr. 2005;94:564–7.
Aurlien D, Leren TP, Tauboll E, Gjerstad L. New SCN5A mutation in a SUDEP victim with idiopathic epilepsy. Seizure. 2009;18:158–60.
Kloster R, Borresen HC, Hoff-Olsen P. Sudden death in two patients with epilepsy and the syndrome of inappropriate antidiuretic hormone secretion (SIADH). Seizure. 1998;7:419–20.
McLean BN, Wimalaratna S. Sudden death in epilepsy recorded in ambulatory EEG. J Neurol Neurosurg Psychiatry. 2007;78:1395–7.
Mostacci B, Bisulli F, Vignatelli L, et al. Incidence of sudden unexpected death in nocturnal frontal lobe epilepsy: a cohort study. Sleep Med. 2015;16:232–6. This study analyzes the incidence of SUDEP in a cohort of patients with frontal lobe epilepsy and almost exclusively nocturnal seizures. The incidence was not different from the rates reported for prevalent epilepsy populations.
Nobili L, Proserpio P, Rubboli G, Montano N, Didato G, Tassinari CA. Sudden unexpected death in epilepsy (SUDEP) and sleep. Sleep Med Rev. 2011;15:237–46.
Ryvlin P, Nashef L, Lhatoo SD, et al. Incidence and mechanisms of cardiorespiratory arrests in epilepsy monitoring units (MORTEMUS): a retrospective study. Lancet Neurol. 2013;12:966–77. This study reports the results of a worldwide survey to describe the features of cardiorespiratory arrests occurring during video EEG monitoring. The authors recommend improve supervision in the monitoring units to avoid the cardiorespiratory depression after generalized tonic clonic seizures, especially during sleep.
Hesdorffer DC, Tomson T. Adjunctive antiepileptic drug therapy and prevention of SUDEP. Lancet Neurol. 2011;10:948–9.
Poh MZ, Loddenkemper T, Reinsberger C, et al. Autonomic changes with seizures correlate with postictal EEG suppression. Neurology. 2012;78:1868–76.
Coppola G, Franzoni E, Verrotti A, et al. Levetiracetam or oxcarbazepine as monotherapy in newly diagnosed benign epilepsy of childhood with centrotemporal spikes (BECTS): an open-label, parallel group trial. Brain Dev. 2007;29:281–4.
Eeg-Olofsson O. Rolandic epilepsy. In: Bazil CW, Malow B, Sammaritano M, editors. Sleep and epilepsy: the clinical sprectrum. 1st ed. Amsterdam: Elservier Science B.V.; 2002. p. 257–63.
Genton P. When antiepileptic drugs aggravate epilepsy. Brain Dev. 2000;22:75–80.
Oguni H. Treatment of benign focal epilepsies in children: when and how should be treated? Brain Dev. 2011;33:207–12.
Prats JM, Garaizar C, Garcia-Nieto ML, Madoz P. Antiepileptic drugs and atypical evolution of idiopathic partial epilepsy. Pediatr Neurol. 1998;18:402–6.
Rating D, Wolf C, Bast T. Sulthiame as monotherapy in children with benign childhood epilepsy with centrotemporal spikes: a 6-month randomized, double-blind, placebo-controlled study. Sulthiame Study Group. Epilepsia. 2000;41:1284–8.
Gross-Selbeck G. Treatment of “benign” partial epilepsies of childhood, including atypical forms. Neuropediatrics. 1995;26:45–50.
Deonna T. Rolandic epilepsy: neuropsychology of the active epilepsy phase. Epileptic Disord. 2000;2 Suppl 1:S59–61.
Verrotti A, Coppola G, Manco R, et al. Levetiracetam monotherapy for children and adolescents with benign rolandic seizures. Seizure. 2007;16:271–5.
Xiao F, An D, Deng H, Chen S, Ren J, Zhou D. Evaluation of levetiracetam and valproic acid as low-dose monotherapies for children with typical benign childhood epilepsy with centrotemporal spikes (BECTS). Seizure. 2014;23:756–61. This study compares the efficacy of low doses of valproic acid and levetiracetam in children with newly diagnosed BECTS. Both drugs were equally effective to control seizures although valproic acid in this study improved EEG abnormalities to a greater extent.
Seegmuller C, Deonna T, Dubois CM, et al. Long-term outcome after cognitive and behavioral regression in nonlesional epilepsy with continuous spike-waves during slow-wave sleep. Epilepsia. 2012;53:1067–76.
Buzatu M, Bulteau C, Altuzarra C, Dulac O, Van BP. Corticosteroids as treatment of epileptic syndromes with continuous spike-waves during slow-wave sleep. Epilepsia. 2009;50 Suppl 7:68–72.
Inutsuka M, Kobayashi K, Oka M, Hattori J, Ohtsuka Y. Treatment of epilepsy with electrical status epilepticus during slow sleep and its related disorders. Brain Dev. 2006;28:281–6.
Atkins M, Nikanorova M. A prospective study of levetiracetam efficacy in epileptic syndromes with continuous spikes-waves during slow sleep. Seizure. 2011;20:635–9.
Chhun S, Troude P, Villeneuve N, et al. A prospective open-labeled trial with levetiracetam in pediatric epilepsy syndromes: continuous spikes and waves during sleep is definitely a target. Seizure. 2011;20:320–5.
Nikanorova M, Miranda MJ, Atkins M, Sahlholdt L. Ketogenic diet in the treatment of refractory continuous spikes and waves during slow sleep. Epilepsia. 2009;50:1127–31.
Veggiotti P, Pera MC, Teutonico F, Brazzo D, Balottin U, Tassinari CA. Therapy of encephalopathy with status epilepticus during sleep (ESES/CSWS syndrome): an update. Epileptic Disord. 2012;14:1–11. This is an updated review about therapeutic options for ESES, including a personal approach by the authors who are experts in the field.
van den Munckhof B, van Dee V, Sagi L, et al. Treatment of electrical status epilepticus in sleep: a pooled analysis of 575 cases. Epilepsia. 2015;56:1738–46.
Arzimanoglou A, French J, Blume WT, et al. Lennox-Gastaut syndrome: a consensus approach on diagnosis, assessment, management, and trial methodology. Lancet Neurol. 2009;8:82–93.
Perucca E, Gram L, Avanzini G, Dulac O. Antiepileptic drugs as a cause of worsening seizures. Epilepsia. 1998;39:5–17.
Tomson T, Battino D, Perucca E. Valproic acid after five decades of use in epilepsy: time to reconsider the indications of a time-honoured drug. Lancet Neurol. 2015. This is a position statement about indications of valproic acid in view of its risks when taken during pregnancy. It should not be prescribed to women of childbearing age when equally effective treatments are available.
Crespel A, Genton P, Berramdane M, et al. Lamotrigine associated with exacerbation or de novo myoclonus in idiopathic generalized epilepsies. Neurology. 2005;65:762–4.
Biton V, Montouris GD, Ritter F, et al. A randomized, placebo-controlled study of topiramate in primary generalized tonic-clonic seizures. Topiramate YTC study group. Neurology. 1999;52:1330–7.
Noachtar S, Andermann E, Meyvisch P, Andermann F, Gough WB, Schiemann-Delgado J. Levetiracetam for the treatment of idiopathic generalized epilepsy with myoclonic seizures. Neurology. 2008;70:607–16.
Berkovic SF, Knowlton RC, Leroy RF, Schiemann J, Falter U. Placebo-controlled study of levetiracetam in idiopathic generalized epilepsy. Neurology. 2007;69:1751–60.
Velizarova R, Crespel A, Genton P, Serafini A, Gelisse P. Zonisamide for refractory juvenile absence epilepsy. Epilepsy Res. 2014;108:1263–6.
Benbadis SR. Practical management issues for idiopathic generalized epilepsies. Epilepsia. 2005;46 Suppl 9:125–32.
French JA, Krauss GL, Wechsler RT, et al. Perampanel for tonic-clonic seizures in idiopathic generalized epilepsy: A randomized trial. Neurology. 2015. This is the pivotal study which showed that perampanel is more efficacious than placebo as add on treatment to reduce frequency of generalized tonic clonic seizures in patients with idiopathic generalized epilepsy.
Yaqub BA, Waheed G, Kabiraj MM. Nocturnal epilepsies in adults. Seizure. 1997;6:145–9.
Romigi A, Marciani MG, Placidi F, et al. Oxcarbazepine in nocturnal frontal-lobe epilepsy: a further interesting report. Pediatr Neurol. 2008;39:298.
Raju GP, Sarco DP, Poduri A, Riviello JJ, Bergin AM, Takeoka M. Oxcarbazepine in children with nocturnal frontal-lobe epilepsy. Pediatr Neurol. 2007;37:345–9.
Picard F, Bertrand S, Steinlein OK, Bertrand D. Mutated nicotinic receptors responsible for autosomal dominant nocturnal frontal lobe epilepsy are more sensitive to carbamazepine. Epilepsia. 1999;40:1198–209.
Oldani A, Manconi M, Zucconi M, Martinelli C, Ferini-Strambi L. Topiramate treatment for nocturnal frontal lobe epilepsy. Seizure. 2006;15:649–52.
Willoughby JO, Pope KJ, Eaton V. Nicotine as an antiepileptic agent in ADNFLE: an N-of-one study. Epilepsia. 2003;44:1238–40.
Garcia-Morales I, Delgado RT, Falip M, Campos D, Garcia ME, Gil-Nagel A. Early clinical experience with lacosamide as adjunctive therapy in patients with refractory focal epilepsy and nocturnal seizures. Seizure. 2011;20:801–4.
Losurdo A, Proserpio P, Cardinale F, et al. Drug-resistant focal sleep related epilepsy: results and predictors of surgical outcome. Epilepsy Res. 2014;108:953–62. This is a retrospective study about outome of drug resistant focal sleep related epilepsy in 95 patients treated with surgery. At the end of the follow up almost 70% of the patients were free of seizures.
Guilhoto LM, Loddenkemper T, Vendrame M, Bergin A, Bourgeois BF, Kothare SV. Higher evening antiepileptic drug dose for nocturnal and early-morning seizures. Epilepsy Behav. 2011;20:334–7.
Eriksson SH. Epilepsy and sleep. Curr Opin Neurol. 2011;24:171–6.
Pornsriniyom D, Shinlapawittayatorn K, Fong J, Andrews ND, Foldvary-Schaefer N. Continuous positive airway pressure therapy for obstructive sleep apnea reduces interictal epileptiform discharges in adults with epilepsy. Epilepsy Behav. 2014;37:171–4.
Vendrame M, Auerbach S, Loddenkemper T, Kothare S, Montouris G. Effect of continuous positive airway pressure treatment on seizure control in patients with obstructive sleep apnea and epilepsy. Epilepsia. 2011;52:e168–71.
Segal E, Vendrame M, Gregas M, Loddenkemper T, Kothare SV. Effect of treatment of obstructive sleep apnea on seizure outcomes in children with epilepsy. Pediatr Neurol. 2012;46:359–62. This study reports the positive effect of surgical treatment of OSA on seizure frequency in children with epilepsy, especially in those with younger age and higher body mass index.
Hollinger P, Khatami R, Gugger M, Hess CW, Bassetti CL. Epilepsy and obstructive sleep apnea. Eur Neurol. 2006;55:74–9.
Byars AW, Byars KC, Johnson CS, et al. The relationship between sleep problems and neuropsychological functioning in children with first recognized seizures. Epilepsy Behav. 2008;13:607–13.
Lopez MR, Cheng JY, Kanner AM, Carvalho DZ, Diamond JA, Wallace DM. Insomnia symptoms in South Florida military veterans with epilepsy. Epilepsy Behav. 2013;27:159–64.
Goldberg-Stern H, Oren H, Peled N, Garty BZ. Effect of melatonin on seizure frequency in intractable epilepsy: a pilot study. J Child Neurol. 2012;27:1524–8. In this study, treatment with melatonin decreased frequency of diurnal seizures in children with drug resistant epilepsy. However, maximal number of seizures, sleep parameters and behavior remained unchanged.
Jain SV, Horn PS, Simakajornboon N, et al. Melatonin improves sleep in children with epilepsy: a randomized, double-blind, crossover study. Sleep Med. 2015;16:637–44. In this study, melatonin showed efficacy to decrease sleep latency in 9 children with epilepsy. No significant effects on seizure frequency were seen.
Jain SV, Glauser TA. Effects of epilepsy treatments on sleep architecture and daytime sleepiness: an evidence-based review of objective sleep metrics. Epilepsia. 2014;55:26–37.
Jain SV, Kothare SV. Sleep and epilepsy. Semin Pediatr Neurol. 2015;22:86–92.
Parhizgar F, Nugent K, Raj R. Obstructive sleep apnea and respiratory complications associated with vagus nerve stimulators. J Clin Sleep Med. 2011;7:401–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Santiago Fernández declares no conflict of interest.
Mar Carreño reports grants and personal fees from UCB Pharma and Eisai and personal fees from Esteve and Bial Pharmaceutical.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Sleep Disorders