Abstract
In this chapter, we discuss sleep-related epilepsy, co-morbidity, differential diagnosis and the association with sleep disorders. The impairment of cognitive capabilities and the role of sleep-epileptic network are also additionally discussed. Some epilepsy syndromes occur primarily during sleep and others primarily upon awakening. The American Academy of Sleep Medicine uses the term sleep-related epilepsy (SRE) for the following epilepsies: sleep-related hypermotor epilepsy (SHE), benign focal epilepsy of childhood with centrotemporal spikes, Panayiotopoulos syndrome, tonic seizures of Lennox-Gastaut syndrome; electrical status epilepticus/continuous spike-waves during sleep and Landau-Kleffner syndrome. The majority of them have their onset during childhood and have a genetic component and a benign course. We describe the distinctive features of each epilepsy syndrome. Moreover, subjects with epilepsy may suffer from sleep disorder co-morbidities, from chronic insomnia to obstructive sleep apnoea syndrome, with significant impact on quality of life. In particular, the occurrence of sleep apnoea may be a challenge, as a sleep seizure may be misdiagnosed as sleep apnoea. Another significant co-morbidity, and differential diagnosis, includes sleep parasomnias. Over the last years, several new aspects have contributed to the understanding of sleep as a contributor to activation of interictal and ictal epileptic phenomena: the interrelationship between the sleep-wake circuitry and the different epileptic networks and the microstructure of sleep associated with epileptic activation, identified within the system of cyclic alternating pattern, and its implication on cognitive consequences of sleep epilepsy. All these new aspects may have strong implications for treatment and prognosis.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Sleep epilepsy
- Sleep seizures
- Children
- Sleep hypermotor epilepsy
- Cyclic alternating pattern analysis
- Benign epilepsy with centrotemporal spikes
- Insomnia
- Sleep apnoea
Introduction
The importance of sleep in epilepsy is well known since ancient times. Aristotele wrote that sleep is similar to epilepsy and epilepsy to sleep, and sleep deprivation was a known trigger for seizures [1]. At the end of the nineteenth century, Gower described patients with seizures exclusively during sleep [2], while the effects of sleep on epileptiform discharges (IEDs) were described for the first time by Gibbs and Gibbs in 1947 [3, 4]. Nowadays, it is well known that IEDs are activated by non-rapid eye movement (NREM) but decrease significantly and are more localized during REM sleep [5]. Mirroring the behaviour of IEDs, nocturnal seizures occur mostly during stages N1 and N2 NREM and very rarely during REM sleep [6]. The majority of generalized seizures occur during sleep-wake transitional states, while the majority of frontal lobe seizures occur during sleep. Only 20% of temporal lobe seizures occur during sleep. Although the atonia during REM sleep may inhibit the motor activation of a seizure, it is not clear how REM sleep really inhibits the ictal event or, in the case of temporal lobe seizures, increases the rate of secondary generalization [5]. In addition, the occurrence of partial seizures induces a suppression of REM sleep, lasting for one night, while status epilepticus induces a stronger suppression, lasting for days [5]. Sleep may help to discriminate real seizures from psychogenic ones, since the latter do not occur in sleep [6].
When correlated with dim light melatonin onset (DLMO), temporal lobe seizures occurred most frequently 6 hours before DLMO and frontal lobe seizures mainly in the 6–12-hour window after the DLMO, suggesting that seizures are synchronized to the circadian rhythm [7]. Information on the circadian nature of seizures can help physicians to choose the right therapies (administered at bedtime), including a future possibility of light therapy [6].
In this chapter, a description of sleep-related epilepsy, along with co-morbidity and differential diagnosis with sleep disorders, is presented. The impairment of cognitive capabilities and the role of sleep-epileptic network are also additionally discussed.
Sleep-Related Epilepsy
Specific epilepsies occur primarily during sleep and others primarily upon awakening. The American Academy of Sleep Medicine created the term sleep-related epilepsy (SRE) to define those epilepsies in which more than 70% of seizures occur during sleep [8]. Epilepsies with seizures occurring upon awakening from sleep are primary generalized seizures upon awakening and juvenile myoclonic epilepsy (JME), while SRE are sleep-related hypermotor epilepsy, benign focal epilepsy of childhood with centrotemporal spikes, Panayiotopoulos syndrome, tonic seizures of Lennox-Gastaut syndrome, electrical status epilepticus/continuous spike-waves during sleep and Landau-Kleffner syndrome.
Sleep-Related Hypermotor Epilepsy
Nocturnal frontal lobe epilepsy (NFLE) involves the attractive world of sleep [9]. It was discovered in Bologna in 1981 when Lugaresi and Cirignotta described five patients with frequent and clustering sleep episodes, characterized by bizarre movements and/or dystonic-tonic posturing of the limbs, strongly suspected to be epileptic, considering the optimal response to carbamazepine [10].
NFLE have been recently renamed as sleep-related hypermotor epilepsy (SHE) , in accordance with a consensus conference of sleep and epileptology experts, who defined the diagnostic criteria [11]. The term “nocturnal” was considered misleading because it implies a circadian rather than a state specificity of the occurrence of seizures during sleep. The typical seizures may arise from other cerebral regions such as temporal or parietal regions. Finally, the original name did not specify the typical clinical hypermotor pattern of seizures [11]. According to the consensus conference, SHE is a rare disease, with an estimated prevalence of 1.8/100,000 individuals, without a gender predominance, and with a peak onset during childhood and adolescence. Seizures are abrupt in onset and offset, typically brief (2 minutes), and have a highly stereotyped hypermotor pattern, usually accompanied to vegetative signs, vocalization, emotional facial expression and asymmetric tonic/dystonic seizures with or without head/eye deviation. Awareness of seizure is common. More rarely, protracted ambulatory behaviour known as epileptic nocturnal wandering (ENW) has been described (lasting more than 2 minutes).
Patients have usually several episodes per night, but this is not regular. Patients may also complain of non-restorative sleep and excessive daytime sleepiness.
The majority of patients are of normal intelligence. However, intellectual disability and behavioural disorders have been reported. Carbamazepine is effective at low doses in two-thirds of patients. Identified aetiologies are heterogeneous and include structural anomalies, acquired injuries and genetic causes. When genetic, sporadic is the most frequent form. In some patients with drug-resistant SHE , the aetiology may involve a surgically treatable lesion, in particular type II focal cortical dysplasia (TFCD), which does not exclude a genetic origin. Nobili et al. found a strong association between nocturnal epilepsy and TFCD in drug-resistant epileptic patients, ascribed to the particular firing pattern of TFCD during NREM sleep [12]. During NREM sleep, the interictal activity is mainly organized in pseudoperiodically recurrent short bursts of fast discharges, often spreading to surrounding non-lesion-related regions and subsequently developing into a seizure [13].
A minority of familial cases has a known genetic mutation. Scheffer et al. described a large Australian family with autosomal dominant NFLE (named ADNFLE, now renamed ADSHE). CHRNA4 was the first epilepsy gene discovered, coding the alpha4 subunit of the neuronal nicotinic acetylcholine receptor (nAChR) [14]. Until now, other mutations in genes (CHRNA2 and CHRNB2) coding for other subunits (alpha2 and beta2) of the nAChR have been identified [15]. The dysfunction of nAChRs is probably at the origin of the additional major neurological or psychiatric symptoms observed in many patients, such as intellectual disability, regression, depression, psychosis, aggression and personality disorder [16, 17]. Furthermore, severe ADSHE has been associated with mutations of the sodium-activated potassium channel encoded by KCNT1, which is also mutated in a severe epileptic encephalopathy with migrating focal seizures of infancy (MFSI). Similarly, in some families with ADSHE, mutations have been found in DEPDC5, another gene implicated in MFSI, encoding a repressor of the mammalian target of rapamycin (mTOR) pathway, a key regulator of cell growth.
Seizures may be preceded by a sudden arousal or a distinct aura. A warning sensation (consisting of fear, especially associated with epigastric discomfort or déjà vu) and auditory aura seem to be more suggestive of a temporal onset [18, 19]. Patients with nocturnal insulo-opercular epilepsy often reported viscero-sensitive (laryngeal and throat sensations, breathing discomfort, unpleasant or rising epigastric sensations) and somatosensory (unpleasant or electrical paresthesiae, diffused or restricted to a small cutaneous area) manifestations and auditory hallucinations. Visual hallucinations are indicative of occipital involvement [20]. Infrequent feeling of levitation has been described in a patient with cortical dysplasia in the right praecuneus region [21].
Considering that epileptic foci are located in deeper areas of the brain like the orbitofrontal or mesial structures, difficult to detect with scalp EEG, stereo-EEG studies on patients who underwent surgery have provided much more information on the anatomo-electro-clinical correlations of SHE. Patients with an asymmetric tonic or dystonic posturing showed an early activation of the supplementary motor area and involvement of the posterior mesial and cingulated frontal cortex. Patients with hyperkinetic ictal behaviour showed the involvement of mesial-dorsolateral, orbitopolar, opercular or larger lobar cortical regions. The epileptic manifestations characterized by fear and prolonged organized motor behaviours, i.e., ENW, involve the activation of anterior cingulate, orbitopolar and temporal regions. In other words, a network including frontal, and possibly extrafrontal, limbic structures is responsible for these complex epileptic manifestations [15, 19]. The increasing complexity of ictal motor behaviours reflects a different duration and propagation of the discharge within the frontal lobe [15]. Apart from the ictal semiology, a long delay (10–20 s) between the electrical and the clinical onset of motor seizure suggests an extrafrontal origin of SHE [19]. Recently a stereo-EEG study revealed that the mean electrographic seizure duration was shorter (38.5 sec vs. 61.8 sec), the mean elapsed time from EEG onset to the first video detectable movement was lower (4.3 sec vs. 9.5 sec), the delay between the first movement and the onset of hypermotor manifestation was shorter (2.2 sec vs. 11.4 sec) and the duration of clinical manifestation was shorter (32.3 sec vs. 52 sec) in frontal than in extrafrontal SHE [22]. Once the hypermotor manifestation began, no differences in seizure phenotype were observed, supporting the hypothesis of a seizure induced-frontal release of central pattern generators (CPGs) [19, 22].
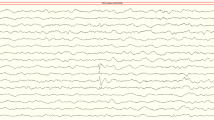
Even though many of SHE’s core features have been clarified, some critical issues remain: the semiological overlap between SHE and sleep disorders is challenging even for sleep and epilepsy experts (see Fig. 11.1). The behavioural patterns of NREM arousal parasomnias, REM behaviour disorders and SHE have some similarities. Ictal motor sequences in SHE contain either epileptic features like dystonic posturing and choreic or ballistic movements, either more parasomnic behaviours like repetitive rocking or rolling, deambulation and even pseudoperiodic patterns [15], reflecting the release of the abovementioned CPGs [23]. CPGs are innate motor patterns present in all organisms and localized in the spinal cord and mesencephalon pons and bulb, essential for survival [24]. In adults, these motor sequences are normally under the control of the mature neopallium but may re-emerge during transient loss of neocortical control, such as during an epileptic seizure, cerebral anoxia or parasomnia [23]. Many of these behaviours should be automatically present when the neomammalian cortex is still “in progress”. Indeed alimentary, locomotory and grasping behaviours occur “spontaneously” in foetuses and newborns [25]. This hypothesis is supported by the widely acknowledged existence of different frontal-subcortical circuits reciprocally connecting frontal lobe, striatum, globus pallidus/substantia nigra and thalamus in humans [8, 26]. Another critical topic challenging the differential diagnosis is the high prevalence of arousal disorders in the personal and family histories of patients with SHE , suggesting a common impairment of the pathway controlling physiologic arousal for both conditions [15]. Stereo-EEG case studies revealed a specific dissociative pattern during a NREM sleep parasomnia, with increased sleep-like delta waves over fronto-parietal associative networks, spindles in the hippocampus and wake-like patterns over motor cortex and limbic structures. A GABAergic and nociceptive dysfunction has been hypothesized, similar to SHE, and a similar increase of sleep instability during slow wave sleep responsible for triggering the episodes was found [27]. Other findings showed a significant overlap between NFLE and parasomnias; muscle and movement artefact, rhythmic non-epileptiform θ or δ activity (arousal patterns) over the frontal regions and diffuse attenuation in EEG amplitude (a manifestation of seizure onset or state change) are common findings in both conditions, and did not have a real discriminatory value [28] (Fig. 11.1).
Two instruments have been developed to help clinicians to discriminate parasomnia from SHE: the Frontal Lobe Epilepsy and Parasomnias (FLEP) scale [29] and the Structured Interview for NFLE [30]. The FLEP scale was found to be associated with a real risk of misdiagnosis in some patients, especially subjects presenting ENWs, which were misinterpreted as arousal parasomnias, lowering sensitivity; meanwhile, in patients with REM behaviour disorder, the scale gave misleading epileptic diagnosis, lowering its specificity [31].
The Clinical Spectrum of Benign Epilepsy During Sleep
Based on the current knowledge, some authors postulated the concept of “system epilepsies”, responsible of the clinical spectrum of benign epilepsy during sleep [32].
Panayiotopoulos syndrome (PS) is a common idiopathic childhood-specific epilepsy, characterized by seizures, often prolonged, with predominantly autonomic symptoms and shifting and/or multiple foci, often with occipital predominance on EEG [32]. Onset is from age 2 to 11 years. The hallmark of PS is ictal autonomic emesis, associated to other autonomic manifestations, such as pallor, sphincteric incontinence, hypersalivation, cyanosis, mydriasis or miosis, coughing, abnormalities of intestinal motility, breathing, cardiac irregularities and syncopal-like manifestations [32]. PS is a model of childhood autonomic epilepsy [33] (Fig. 11.2).
Benign epilepsy with centrotemporal spikes (BECTS), also called self-limited epilepsy with centrotemporal spikes or childhood epilepsy with centrotemporal spikes (CECTS), is the most common type of focal epilepsy in children, presumably genetic. Age of onset ranges from 1 to 14 years, and the prevalence is about 15–20% of epilepsy in children younger than 15 years of age [34]. BECTS is characterized by infrequent hemifacial sensorimotor seizures during sleep, which may secondarily generalize in half of the cases or rarely induce a status epilepticus, usually reflecting non-lesion cortical excitability from Rolandic regions. These seizures are often associated with oro-pharyngo-laryngeal symptoms, such as making strange noises, speech arrest and salivation. The seizures predominantly occur during sleep, often in the early morning hours; their frequency is low, typically 2–5 total seizures, but also quite variable, ranging from a single lifetime episode to multiple seizures per day [35]. Interestingly, children with BECTS may present with autonomic seizures referable to PS, while others may alternately have autonomic and Rolandic seizures [32]. Drowsiness and sleep increase the rate of discharges, and an extreme discrepancy between rarity of seizures and the abundant activity of the EEG foci is common [35]. The onset of focal seizures is frequently preceded in early childhood by various developmental deficits, including speech dyspraxia and impairments in language, literacy, attention and behaviour. These neuropsychological deficits cluster in families of BECTS patients, who do not have epilepsy themselves [35].
The prognosis is usually excellent, notwithstanding the abovementioned neuropsychological deficits. Neuroimaging studies have shown subtle cortical abnormalities in the frontal-temporal, perisylvian and parietal region [36]. It seems that neuroimaging abnormalities precede BECTS onset and evolve over time as a marker of a more complex cerebral maturation problem, responsible for both seizures and learning disabilities [35]. These data suggest an association between BECTS and systemic brain disorganization with functional defects in Rolandic areas leading to neurocognitive impairments [37].
The atypical evolution of BECTS can result in:
-
1.
Atypical benign childhood focal epilepsy (ABCFE)
-
2.
Status epilepticus of BECTS (SEBECTS)
-
3.
Landau-Kleffner syndrome (LKS)
-
4.
Epileptic encephalopathy with continuous spikes and waves during sleep (CSWS)
All of the above are considered part of a single spectrum of disorders [34]. Notwithstanding epileptic encephalopathies being within the spectrum of CSWS syndromes, ABFEC and SEBECTS have a favourable outcome when right therapeutic measures are taken. Prognosis of LKS and CSWSS syndrome instead is not so good in terms of full recovery [32].
Atypical features in BECTS comprise many clinical and electrophysiological findings: seizures only occur in the daytime, are associated to Todd’s paralysis or even present as status epilepticus. Besides hemifacial contraction, the seizures may present with dysfunctions of the lip, tongue and pharynx, including speech arrest, dysarthria, excessive drooling, oromotor dyspraxia and swallowing difficulties (pseudo-opercular syndrome), further including generalized tonic-clonic seizures, atypical absence, myoclonic seizures, atonic seizures and negative myoclonus at a later stage (pseudo Lennox-Gastaut). The associated seizures tend to be resistant to many antiepileptic drugs; however, they disappear before adolescence, along with the neuropsychological deficits. SEBECTS refers to status epilepticus that can be convulsive or non-convulsive and either generalized or focal. Although some patients remain mentally retarded even after the remission of the seizures, ultimate neurocognitive outcome appears good when the disorder is treated [34] (Fig. 11.3). The EEG usually shows a marked increase and a bilateral synchronization of epileptiform discharges in the Rolandic area or otherwise ripples (80–250 Hz), superimposed on Rolandic spikes [38], which may become continuous during NREM sleep or may evolve in CSWS. Recently, two types of HFO have been distinguished: (a) ripples with slower frequency (80–160 Hz) as physiological activity and (b) fast ripples with higher frequency (200–500 Hz) as a pathological activity, associated with epilepsy [39]. Spike dipole was directed anteriorly in patients with good outcome (seizure control), whereas dipole orientation headed posteriorly was observed in patients with poor seizure control or neurocognitive deficits [40].
LKS , known as acquired epileptic aphasia, is an epileptic encephalopathy characterized by various types of seizures and insidious or sudden-onset acquired aphasia with verbal auditory agnosia. More than half of these children have problems with receptive language, auditory processing, auditory working memory and verbal memory, as well as learning difficulties and attentional and behavioural problems. Benign EEG patterns, like focal epileptiform discharges, may evolve into CSWS sleep in about half of children with LKS. Adequate and early medical intervention may avoid language and cognitive impairments. Acquired opercular epilepsy with oromotor dysfunction is a condition that is difficult to categorize because the clinical features look similar to SEBECTS and LKS [34].
Epileptic encephalopathy with CSWS is a rare childhood epilepsy syndrome and may represent between 0.2% and 2% of the epilepsies. Tassinari et al. first introduced these terms in 1977 [41]. CSWS is the extreme end of atypical BECTS. The onset of seizures varies, but the seizures tend to peak at about 5 years of age, before evolving into epileptic encephalopathy within 1–2 years. Seizure types are not specific. Linguistic, neurocognitive decline and neuropsychiatric features are commonly associated with this condition. It appears that the longer the duration of CSWS, the poorer the outcome is [34]. The EEG pattern at time of diagnosis shows almost continuous slow (typically 1.5–3 Hz) spikes and waves, seen in slow sleep. Some authors provide percentages of slow wave sleep that must be occupied by continuous spikes and waves, e.g., >50% or >85%. The Commission on Classification and Terminology of the International League Against Epilepsy (1989) does not require these criteria [42]. A recent review found that approximately 68% of the cases were diagnosed with CSWS epilepsy-aphasia spectrum when they had spike-wave index >50% clearly activated during sleep [43]. The abnormal EEG activity interferes with sleep-related physiological functions and possibly neuroplasticity processes mediating higher cortical functions, such as learning and memory consolidation [44]. CSWS can concur with other syndromes like Rett syndrome, tuberous sclerosis complex and autism spectrum disorder [43]. The underlying aetiology is unknown although brain malformations, immune disorders and genetic factors have been reported. Immunity disorders with evidence of onconeuronal antibodies have been reported [43]. The SCN2A gene encodes subunits of voltage-gated sodium channel, whereas KCNB1, KCNQ2 and KCNA2 genes encode for subunits of the potassium channel which is highly expressed in brain neurons. The GRIN2A gene encodes N-methyl-D-aspartate (NMDA) glutamate receptor α2 subunit. The NMDA receptor is a glutamate-activated ion channel permeable to sodium, potassium and calcium and found at excitatory synapses throughout the brain. CNKSR2 gene encodes connector enhancer of KSR2 which is a synaptic protein involved in Ras signalling-mediated neuronal proliferation, migration and differentiation. The SLC6A1 gene encodes voltage-dependent gamma-aminobutyric acid (GABA) transporter 1 (GAT-1), one of the main GABA transporters in the central nervous system. Several mutations (in terms of copy number variations) of these transporters have been found in CSWS epilepsy-aphasia spectrum. Therefore, channelopathy may play a major role in pathogenesis of CSWS/epilepsy-aphasia spectrum [43, 45]. The recommendation is to avoid the classic AEDs (phenobarbital, phenytoin and carbamazepine) and some of the new AEDs, such as oxcarbazepine, lamotrigine, topiramate and levetiracetam and to start treatment with ethosuximide, benzodiazepines or sulthiame. In refractory cases, a ketogenic diet, corticosteroids such as methylprednisolone pulse therapy or dexamethasone, intravenous immunoglobulin and even surgical interventions are suggested [32, 34].
Sleep Macrostructure
Epilepsy per se and/or the seizures themselves may promote sleep disruption and significantly affect the quality, quantity and the architecture of sleep [46]. Increased sleep fragmentation and higher percentage of wakefulness and light sleep, with a decrease in SWS and REM sleep, are common polysomnographic findings in individuals with epilepsy [47, 48]. When seizures occur during the nocturnal period, in addition to a decrease in the duration of REM sleep and increase in REM sleep latency, sleep efficiency and total sleep time drop, causing sleep fragmentation [49]. Generally, a good outcome and response to treatment is accompanied with a significant amelioration of sleep quality, as it has been demonstrated in children with childhood absence epilepsy [50].
Few data are available on sleep macrostructure alterations related to specific epileptic syndromes.
In a group of patients with SHE, a significant increase in wake after sleep onset, SWS duration and REM latency were found, whereas REM sleep duration was significantly lower [51].
A systematic review and meta-analysis of the polysomnographic aspect of sleep in children with epilepsy with centrotemporal spikes showed a longer sleep latency as the strongest outcome associated to the epilepsy [52]. Some studies report that children affected by symptomatic partial epilepsy show permanent modifications in sleep architecture, including a significant decrease of slow wave sleep [53, 54, 55].
Sleep Microstructure
During NREM sleep, phasic EEG events, such as K-complexes, vertex waves, delta wave bursts, and short-lasting arousals, show a peculiar time arrangement, indicated as ”cyclic alternating pattern” or CAP. CAP has been described as consisting of transient complexes (phase A) that periodically interrupt the tonic theta/delta activities of NREM sleep (phase B). Functionally, CAP is thought to translate a condition of sustained arousal instability oscillating between a greater arousal level (phase A) and a lesser arousal level (phase B). CAP oscillations are maximally expressed over the frontal areas [56] and may imply that epileptogenic foci could be more prone to be activated by these oscillatory mechanisms. CAP has been analysed in several forms of epilepsy. In genetic generalized epilepsy, a higher CAP rate is reported, along with spikes occurring during phase A1, and similar findings have been reported in lesional temporal lobe epilepsy. In patients with SHE, a significant increase of CAP time, CAP rate, CAP cycles and mean duration of a CAP sequence has been reported, with a significant increase in the number of all CAP phase A subtypes and, in particular, of A1 subtype. The majority of the motor epileptic events are associated with the occurrence of phase A [51, 57], although the minor motor events, coupled to arousal and CAP A phases, have not been considered true epileptic manifestations [58].
In children with BECTS, CAP analysis showed reduced CAP instability due to the presence of spikes which replaced phase A1 and suggested that the centrotemporal spikes may disrupt the physiological synchronization mechanism [59], in contrast with children with drug-resistant epilepsy, in whom an increase of CAP rate was found [55, 60].
Sleep Disorders, Co-morbidity, Differential Diagnosis and Consequences
Approximately one-third to one-half of patients with epilepsy will have a sleep-related complaint. Co-morbid sleep disorders may aggravate the epileptic state, facilitating spikes as well as nocturnal seizures, increasing daytime sleepiness and reducing quality of life [61]. Studies regarding epilepsy and sleep disturbances frequently lack descriptive and statistical analysis for specific sleep disorders (such as insomnia, parasomnia and sleep apnoea) and rather focus on sleep complaints and sleep quality more generally [62]. The most common sleep-wake complaint among adults with epilepsy is sleep maintenance insomnia, occurring with a prevalence of up to 79%, whereas the second sleep-wake complaint is excessive sleepiness [62]. Complaint of insomnia or sleepiness in adults with epilepsy warrants consideration of co-morbid depression, anxiety and suicidal ideation [61, 63]. Insomnia severity and poor sleep quality may be significantly related to the number of antiepileptic medications, and amelioration of insomnia is accompanied by remission of [61]. Specific evidence for the usefulness of cognitive behavioural therapy for insomnia (CBTi) in epilepsy is currently lacking. CBTi can be recommended as an initial treatment strategy although sleep restriction should be considered cautionary in epileptic population [61].
Despite the increase in studies regarding sleep disorders in children with epilepsy over the last decade, none evaluated insomnia as the primary endpoint, and few assessed risk factors and treatment outcomes related to sleep disturbances [62]. Insomnia symptoms were more common in children with epilepsy and developmental delay [62], mostly related to bedtime resistance and co-sleeping. Higher frequency of co-sleeping and room sharing in epileptic children could be explained by parental concern, especially relating to nocturnal seizures [62]. Lower melatonin levels have been found in patients with refractory epilepsy compared with healthy controls [64], and melatonin has been demonstrated to be an optional treatment for insomnia [65]. In a randomized placebo-controlled study, melatonin improved sleep with non-significant improvement in IEDs and seizure frequency [66]. However, negative effects have also been noted, including EEG abnormalities in patients with temporal lobe epilepsy and increased seizure activity in neurologically disabled children.
After the discussion of 26 papers reporting an association between melatonin and epilepsy or seizures, a recent review suggests that in view of conflicting results from earlier work, more large-scale, double-blind, randomized, placebo-controlled clinical trials were needed [67].
Recently, an anecdotal report demonstrated the efficacy of pitolisant, a drug used to treat refractory diurnal sleepiness, to suppress generalized IEDs for 4 hours, in 6 patients out of 14 photosensitive adults [68].
Sleep-related breathing disorders may trigger paroxysmal events during sleep and may exacerbate pre-existing seizures. Sleepiness, a common complaint of patients with epilepsy that is frequently attributed to antiepileptic drugs, may be linked to undiagnosed sleep disorders such as restless legs syndrome or OSA [69]. Patients with epilepsy should be questioned about the presence of other sleep disorders, such as OSA, restless legs syndrome (RLS), insomnia and disorders of hypersomnia, such as narcolepsy. Although it has not been validated in epilepsy patients, the Epworth Sleepiness Scale (ESS) can be used in the evaluation of EDS in epilepsy patients for the presence of these sleep disorders [4].
Co-morbid Sleep-Disordered Breathing in Epilepsy
Both obstructive sleep apnoea (OSA) and central sleep apnoea (CSA) have been reported in epilepsy patients, but CSA has received less attention [61]. At least mild severity OSA (AHI ≥5) was found in nearly 30% of patients, while moderate-to-severe OSA (AHI ≥15) was seen in 10% of patients. Men were three times more likely to have OSA [70]. The prevalence of OSA did not significantly differ according to seizure type (focal versus generalized seizures), epilepsy control (refractory versus controlled epilepsy) or number of antiepileptic drugs [70]. The sleepiness and cognitive dysfunction caused by OSA are usually ignored in epilepsy [65]. Patients with epilepsy and co-morbid OSA were more likely to experience seizures during sleep than patients without OSA; the onset of OSA symptoms may temporally coincide with a change in seizure control – either an increase in seizure frequency or a new onset of seizures or status epilepticus [61]. PSG should be considered when a patient exhibits refractory sleep-related epilepsy [65]. According to a recent meta-analysis, epilepsy patients treated with continuous-positive airway pressure (C-PAP) were >5 times more likely to have a significant reduction in seizure frequency and daytime sleepiness compared to untreated patients [70]. It has been recently described that a 50-year-old man with focal epilepsy controlled by AEDs during daytime underwent PSG for suspected OSA and daytime somnolence. The video PSG revealed many breathing events appearing immediately after falling asleep, suggesting a pattern of so-called sleep-onset central apnoea hypopneas (SOCA). Most of the breathing events ended with brief (2–8 s), stereotyped paroxysmal motor episodes characterized by a ventral flexion of the head, eyes opening, dystonic upper limb extension and mild abduction. Bilateral frontal synchronous bursts of spikes or 2-Hz spike-wave complexes started around 1 s before the onset of each event. Normalization of the respiratory pattern was obtained on adaptive servo-ventilation. The motor events also disappeared, and a striking improvement of sleep was achieved [71]. Interestingly, successful epilepsy surgeries improve OSA symptoms, apnoea hypopnea index and related sleep parameters [65]. Treatment with a compound containing carbonic anhydrase inhibitor properties such as topiramate, zonisamide and acetazolamide may improve both CSA and OSA and should be taken into consideration when a sleep respiratory disorder is co-morbid to epilepsy [65]. Treatment of excessive daytime sleepiness with modafinil is warranted in adults with epilepsy and OSA, which may have benefit also in seizure control, reducing the deleterious effect of drowsiness [65].
The relation between OSA and epilepsy is complex, especially in developmental age: OSA and epilepsy may be in co-morbidity, or recurrent hypoxia and sleep fragmentations may increase the risk to develop epilepsy, and finally OSA may be a misleading diagnosis for epilepsy, and finally OSA as a misleading diagnosis for epilepsy. The prevalence of OSA is nearly 40% in children with refractory epilepsy [72, 73]. Children with neurodevelopmental disability and epilepsy, with or without specific syndromes (such as Angelman syndrome), have higher prevalence of co-morbid OSA (more than 30% of cases) and numerous periodic limb movements during sleep (more than 40% of cases) [74, 75]. As for adults, the precocious diagnosis and treatment of OSA (mostly adenotonsillectomy) may reduce seizure frequency [76].
Few reports showed activation of epilepsy by OSA in children without a previous history of epilepsy. A preliminary study showed IEDs during sleep in 18 of 127 (14.2%) children with OSA. IEDs during sleep are mostly represented by CTS, occipital in the younger and frontal on the older. Children with IEDs and OSA were older and had a longer OSAS duration of disease [77]. Considering that PSG recordings revealed an epileptiform activity during sleep in 1.45% of otherwise healthy children [78], OSA may represent an additional risk factor to develop epilepsy. Subjects with IEDs had a high occurrence of perinatal injuries, suggesting the possibility that a primary brain insult may predispose to both OSAS and the paroxysmal EEG activity [77]. Furthermore CAP analysis showed findings similar to BECTS: a lower CAP rate and A1 index during SWS and a lower A2 index during total NREM sleep, similar to CAP [77]. The same results were replicated in a population of 298 children with OSA or snoring: 48 (16.1%) children were found to have IEDs, whereas 3 were also found to have nocturnal seizures (2 females diagnosed with Rolandic epilepsy and a male diagnosed with SHE). After 6 months, the IEDs had disappeared in those subjects who reported improvement of OSA, while it appeared or persisted in those without changes in OSA parameters [69]. These findings suggest that the risk of developing IEDs, which may or may not be associated with nocturnal seizures, increases if sleep-disordered breathing persists. A similar finding was found in a cohort of Spanish children who underwent nap or standard PSG for suspected OSA: 6 of 25 met the criteria for sleep-disordered breathing and also had PA/IEDs and/or seizure [60]. Four of them (16% of all the samples) met the criteria for OSAS and epilepsy, with IEDs and seizures during sleep. In one patient, the video PSG showed many IEDs with minor motor events, mostly during SWS, and a diagnosis of SHE was established. The magnetic resonance imaging (MRI) showed signs of focal cortical dysplasia involving the right Sylvian fissure. A further two cases met the criteria for BECTS, with partial motor seizures during sleep. The last case received a diagnosis of focal symptomatic epilepsy, and the MRI performed after the PSG study revealed the presence of a malacic area on the left subcortical white matter. These results suggest that children with SBD and neurological conditions may have an additional risk of developing IEDs and/or epilepsy [60]. Another study found higher apnoea hypopnea index in children with BECTS compared to normal control, as well as a trend towards lower oxygen saturation and longer duration of apnoea [79].
A case report of an obese child with severe OSA in whom nocturnal frontal lobe seizures started within a week after he began nasal C-PAP therapy corroborated the hypothesis about a complex relationship between OSA and epilepsy. In this case, treatment caused a rebound of SWS, in particular, of slow wave activity, in terms of significant increase of A1 component of CAP, triggering motor seizure, which was masked by the sleep fragmentation caused by respiratory events. MRI disclosed signs of focal cortical dysplasia involving the right inferior frontal circumvolution . The diagnosis was NFLE, and antiepileptic treatment was started with topiramate (3 mg/kg per day). Topiramate induced a decrease of CAP rate and of arousal index (already decreased by ventilation therapy), suggesting that the control of the seizures was mediated by decreasing SWS-CAP sleep instability [80].
Some symptoms of seizures (e.g., snoring and/or apnoea; vocalizations; coughing; tachypnea; tachycardia; bruxism; salivation; and head, body or limb movements during sleep) can mimic OSA, thus leading clinicians to mistake symptoms of epileptic seizures for obstructive sleep respiratory events [60, 81], especially in patients with SHE from frontal, temporal or insular origin [65]. PSG with extended EEG and video is the gold standard tool to evaluate patients with apnoea due to suspected seizures [69]. Epilepsy in children can be difficult to diagnose, when the only manifestation is central apnoea: in a case report, seizure was documented as the cause of apnoea and desaturation in an otherwise healthy 24-month-old child. The aetiology of the spells was partial seizures originating in the right anterior mid-temporal region. In this case, the absence of associated bradycardia to central apnoea is a red flag for seizure [81]. Choking, air hunger and agitation, from SWS associated to desaturation, were the only symptoms of nocturnal seizure of SHE in a 4-year-old girl with a long history for episodes of choking, four to five times per night [82]. A similar case diagnosis was described in a 3-year-old girl referred for snoring and apnoea, who underwent a cardiorespiratory PSG revealing the presence of atypical obstructive sleep apnoea with stereotyped artefact. A following sleep EEG revealed a motor seizure with ictal discharge from frontal regions. For this reason, she performed a full PSG recording which showed several ictal obstructive apnoea before the onset of motor component of the seizures [83]. Parrino et al. demonstrated that an unattended cardiorespiratory PSG showing repeated ictal polygraphic patterns may indicate the presence of seizures during the night [84]. A video polysomnography should be performed to confirm the ictal nature of such patterns. After being referred for OSA and parasomnias at night, a paediatric Spanish cohort of 24 out of 190 children were diagnosed with SHE, because of repeated recorded motor seizures demonstrated by the attended PSG recording [85].
Co-morbid Restless Legs Syndrome (RLS) in Epilepsy
RLS co-morbidity appears to be frequent, yet highly variable, in different epileptic patient cohorts, and diagnosis was based on symptoms, ranging from 10% to 30% of population investigated [61]. Very rarely, aura symptoms of focal seizures may mimic RLS symptoms, as reported in a single case of right posterior frontal focal cortical dysplasia that presented with nocturnal unilateral left leg paresthesias and cramps that preceded generalized tonic clonic seizures [86].
Co-morbid Parasomnia in Epilepsy
The NREM parasomnia has been discussed in the differential diagnosis and common features of SHE. Co-morbidity with REM behaviour disorder (RBD) has been poorly described in epilepsy [61]. In one large Turkish outpatient epilepsy-clinic cohort [87], 12% of epilepsy patients had probable RBD in response to a survey-based instrument, compared to only 6% of controls. RBD was relatively frequently seen (12.5%), especially in elderly epilepsy patients when systematically investigated for concurrent parasomnias, with RBD prevailing in cryptogenic epilepsy [88]. Conversely, 26.6% of patients with idiopathic RBD had interictal epileptiform activity on EEG [89]. Rarely, autoimmune encephalitis, especially when paraneoplastic, may concomitantly give rise to RBD and focal epilepsy, accompanied by other syndromic cognitive, motor or autonomic features typical of limbic encephalitis. RBD may be treated with clonazepam or melatonin [61].
Association of Sleep with Sudden Unexpected Death in Epilepsy (SUDEP)
SUDEP is a rare but tragic phenomenon, defined as death in people with epilepsy occurring in the absence of a known structural cause of death. The frequency of SUDEP is 1.2 per 1000 patient-years in people with epilepsy overall [90].
SUDEP risk factors have been identified, including a major association with uncontrolled tonic-clonic seizures, as well as medication non-compliance, male sex, epilepsy onset before 16 years and duration of epilepsy >15 years [90]. Patients at particularly high risk are those with developmental and epileptic encephalopathies due to sodium channel (SCN) gene mutations, such as Dravet syndrome. A recent systematic review and meta-analysis found that 69.3% of all reported SUDEP cases occurred during sleep and 30.7% of them occurred during wakefulness [91]. Patients were 6.3 times more likely to die in the prone position during sleep than during wakefulness. These circumstances of SUDEP are remarkably similar to those of sudden infant death syndrome (SIDS) and suggest that sleep might be an important risk factor for SUDEP [91]. Nocturnal seizures are associated with more prominent autonomic dysfunction than are diurnal seizures. Generalized tonic-clonic seizures (GTCS) are the most important risk factor for SUDEP, as they have been observed in a vast majority of witnessed and monitored SUDEP cases. The low incidence of SUDEP in people with NFLE might reflect the low occurrence of GTCS [91]. In the MORTEMUS study, GTCS preceded all SUDEP cases. An expert panel discovered a consistent pattern of tachypnea (18–50 breaths per min) immediately after seizure termination, which was followed by a transient or terminal cardiorespiratory arrest within 3 min [92]. Postictal generalized EEG suppression (PGES) is associated commonly with GTCS, with impaired postictal arousal and with immobility, which may compromise the brainstem autoresuscitation mechanism [91].
The Effect of Antiepileptic Drugs (AEDs) on Sleep
The effect of treatment is summarized on Table 11.1 [4]. The effect on sleep architecture may be mediated by the remission of epilepsy [6]. Ketogenic diet, successful epilepsy surgery and vagus nerve stimulator improved nocturnal sleep. The latter also improved daytime sleepiness, and it may increase the rise of OSA and central apnoeic patterns during sleep [93].
Medication selection can be tailored towards sleep complaints. Patients with difficulties sleeping at night may benefit from a higher dose of a sedating agent, and individuals with hypersomnia may benefit from alerting AEDs during the day [4]. If seizures tend to occur during the transition from wakefulness to sleep, immediate-release formulations can be more effective than extended-release ones, which would be more efficacious in seizures happening later at night or during sleep-wakefulness transition [94].
Sleep and System Epilepsy: The Cognitive Impact
ADHD is the most prevalent neuropsychiatric co-morbidity in epileptic patients, especially in the refractory cases, presented in up to 60–70% of patients, worsening the psychosocial prognosis [95]. It is less difficult to explain cognitive deficits associated with symptomatic epilepsies when they are the result of recognizable cerebral lesions rather than of epilepsy per se or inducing encephalopathic epilepsy. More difficult to explain is why the so-called idiopathic benign epilepsies are associated with cognitive impairment starting at the onset of or during the natural course of epilepsy [96].
Over the last years, several new aspects have been elaborated contributing to understand better the activation of interictal and ictal epileptic phenomena by sleep: the interrelationship between the sleep-wake circuitry and the different epileptic networks, and the microstructure of sleep associated with epileptic activation, identified within the system of CAP [39].
In summary, IED seems to follow either sigma or delta power, depending on the type of epilepsy. IED rate (ISR) was correlated with sigma power in childhood epilepsy syndromes such as BECTS or CSWS whereas followed delta power in adults with structural temporal or frontal epilepsy (inducing decreasing or increasing of CAP instability, respectively). Recently, the classical dichotomy of partial and generalized epilepsy has been replaced by the unifying network concept. The so-called “generalized” epilepsies involve a bilaterally represented large cerebral system, namely, the thalamocortical system. “Focal” epilepsies involve more or less wide, sometimes bilateral regional circuitries [39]. Activation during sleep is related to the network properties of the particular epileptic syndromes, with interference with cognitive process: (1) via the thalamocortical system as main route and (2) other ways like (a) frontal epilepsy by epileptic transformation of the cholinergic arousal system in NREM sleep and (b) activation of temporal-limbic epilepsy by NREM and REM sleep via hippocampal changes during sleep [39].
In the idiopathic generalized epilepsy (IGE), several studies proved that during interictal spike-wave discharges, a transient cognitive impairment is detectable [97]. The working mode of the system by which the spike pattern develops is proved to be the same that works during NREM sleep opposed to waking and REM state [39]. There is a close relationship between vigilance level and expression of spike-wave paroxysms. Spontaneous paroxysms are promoted by transitory decreases of vigilance level during awake state, after awakening, after lunch, in evening sleepiness, during a boring task and after sleep deprivation [39]. Both in deep NREM sleep and in absences the cortical activity is reduced in certain (mainly frontal) areas. The functional neuroimaging, neurophysiologic and clinical data point to the thalamocortical network as a common substrate of NREM sleep and IGE. Spike-wave discharges and sleep spindles can also be interpreted by the different degrees of GABAergic inhibition in the thalamus. According to the slogan of Steriade – “sleep and epilepsy are bedfellows” – spike-wave discharges of IGE represent the epileptic exaggeration of the bursting mode of the thalamocortical system [39]. Association of generalized spike-wave pattern in IGE with sleep instability in NREM sleep can be measured by CAP rate, usually increased, proportional with sleep instability [98].
Heterogeneous cognitive deficits have been described since the 1990s in typical BECTS, affecting both non-verbal cognitive functions (visual, executive, fine motor execution, attention, memory and speed processing) and verbal functions, during the active phase of the epilepsy. BECTS is associated with a high frequency of learning disorders (10–40%) and academic underachievement [32]. In a prospective study of 44 children with BECTS, the atypical group had significant lower full-scale IQ and verbal IQ [99]. Some patients, especially those in whom the epileptic process is localized around the perisylvian cortex, present with features of autistic spectrum disorder, but unlike primary autism, there is no loss of social interaction [100]. Functional magnetic resonance imaging (fMRI) data support a functional deficit of the default mode network (DMN). This dysfunction is most apparent in the precuneus, a key region of the DMN. In particular, children with BECTS show reduced activation of the DMN during the rest condition and a deactivation during cognitive effort. In addition, reduced functional connectivity was demonstrated between the sensorimotor network and the left inferior frontal gyrus (Broca’s area) [32]. This functional decoupling might be a clue to understand language impairment in typical RE and is in line with the identified neuropsychological profile of anterior language dysfunction [101]. The nature and severity of interictal cognitive symptoms are closely related to localization within the network and amount of epileptic interictal discharges during sleep [39]. The brain tissue responsible for the disorder is localized around the Sylvian fissure and strongly correlated with speech function and cognition. Several authors have reported a higher incidence of nocturnal epileptiform EEG discharges in children with specific language impairment, without epilepsy. The benefit of antiepileptic drug treatment remains questionable in this case [32].
In PS, a slightly different network is implicated. Autonomic symptoms are usually generated by activation or inhibition of parts of the central autonomic network that involves the insular cortex, medial prefrontal cortex, amygdala, hypothalamus and ventrolateral medulla. Thus, irrespective of the localization of their onset, ictal discharges may activate the lower threshold autonomic centres [32].
In benign epilepsy during sleep, the amount and persistence time of interictal discharges seem to correlate with the degree of cognitive deficits, and there is a correlation between the degree of spiking during sleep and the degree of cognitive deficits across syndromes. The epileptic discharges are accompanied with a slow wave component, associated with cognitive deficits rather than frequent seizures. This characteristic situation has been called “cognitive epilepsy”. The slow wave components of the discharges may protect against conventional sustained, depolarization-based seizures but on the other hand interfere with normal cortical functioning. This assumption is strongly supported by several new results showing that sleep has a use-dependent homeostatic function, connected with sleep slow wave activity, needed for the plastic functions, impaired when abundant IEDs interfere. CSWS affects auditory discrimination and may have a long-lasting impact on cognitive function, whereas in typical children with BECTS with a lower degree of IEDs, plastic brain reorganization or the preservation of networks may prevent such difficulty [102] or reduce the impact of cognitive deficits. Slow wave downscaling measuring according to amount of slow wave activity, amplitude of slow waves, slope of waves and amount of multipeak waves during night sleep are impaired in CSWS patients [102, 103]. After remission of CSWS, the slope decreased significantly overnight. Analysis of slow waves might serve as a prognostic factor regarding cognitive outcome [104].
Recently, the characteristic feature of NREM sleep in Lennox-Gastaut syndrome (LGS), namely, the runs of generalized paroxysmal fast activity (GPFA), has been demonstrated to be a distortion of physiological leading to giant pathological spindles [39]. In Doose syndrome, where GPFA is not present, mental deterioration is less frequent and not as severe as in LGS. GPFA may have a special worsening effect on memory consolidation and can be considered a malignization marker of primary and secondary generalized epilepsies (also induced by benzodiazepine drugs and barbiturates) [39].
Temporo-limbic network epilepsy (TLNE) is the most frequent epilepsy type in adulthood. The main substrate of TLNE is held to be the hippocampus; however, more widespread temporal structural damage plays a role. Within NREM sleep, the activation of temporal spiking was found to be the highest during SWS. The characteristic cognitive deficit conjoining TLNE is disturbance in declarative memory, due to hippocampal dysfunction which is in a certain extent side specific related to verbal memory in the dominant side and to visuospatial memory in subdominant side. There are only some lines of evidence for the role of IEDS during NREM sleep in the memory deficit interfering with hippocampal-cortical dialog during NREM sleep [39].
The role of the frontal lobe during memory process has gained attention in the last years: several studies showed that specific areas within the frontal cortex are involved in long-term memory, contrary to the traditional view that the frontal lobe role is limited to working memory [105]. A systematic neuropsychological study on a representative sample of patients affected by SHE showed neuropsychological deficits in more than half of cases (53.33%), associated with mental disability in 11.7% or a concomitant cognitive decline in 15% of them. A discrepancy strongly emerged between verbal and non-verbal IQ, irrespective of lateralization of seizure foci. A significant worse total IQ mean score was found in patients carrying mutations in the known genes for SHE compared to patients without mutations, independently of the specific gene involved [105]. Even among patients with normal intelligence, deficits involving memory, visuospatial abilities and selected executive functions (phonemic fluency, inhibitory control and working memory), with preserved shifting abilities and planning [105], were found. The finding of memory deficits can be readily explained by both the possible origin of hypermotor seizures from extrafrontal (temporal) networks and the main involvement of frontal areas [105]. In the SHE, similar to parasomnia, the ACh mutation within the frontal system is mainly affected. The number of microarousal during NREM sleep is increased [51], but with opposite function compared to the IGE networks, since the cholinergic arousal system inhibits the thalamic reticular activity [39], inducing a frontal-temporal altered networking. One study reveals a different network structure and inter-area connectivity characterized by a higher connectivity in the occipitoparietal regions and lower values in the frontal areas [106]. Furthermore, an alteration of homeostatic process has been hypothesized in patients with SHE. It has been found that ictal events occur almost exclusively in SWS (72%), with a predominance in the first sleep cycle and decreasing in frequency together with the exponential decay of SWS across the night. In the first sleep period, the repetitive interruptions due to epileptic facilitation produce a sleep fragmentation with a significant increase of REM latency and a homeostatic rebound of deep sleep in the second part of the night, resulting in an unexpected enhancement of SWS. No other untreated sleep disorders, including insomnia, share such a long REM latency with high amount of SWS [51].
Finally, in humans, only 1% of seizures occurred in REM sleep, and the rate of seizures, focal and generalized IEDs and focal high-frequency oscillations (HFOs) was all lowest in REM sleep. Cortical desynchronization in REM sleep suppresses seizure, IEDs and HFO distribution. Cortical desynchronization makes it harder for spontaneously occurring aberrant activity to organize into an IED and then harder still for IEDs to organize into seizures [107]. REM sleep has also been shown to selectively and persistently rebound after successful surgery of epilepsy. The absence of orexinergic activity in REM sleep, which is characterized by diffuse cortical desynchronization, may be overall protective against IEDs and seizures [107]. On the contrary, the presence of orexinergic activity in wakefulness, SWS and state transitions, which are characterized by a relatively greater degree of cortical synchronization, is overall less protective against IEDs and seizures [107].
In Table 11.2, the different states of vigilance implicated in sleep-related epilepsy, the NREM sleep instability related and the suggested appropriate treatment are summarized.
References
Degen R, Degen HE. Sleep and sleep deprivation in epileptology. Epilepsy Res Suppl. 1991;2:235–60.
Gowers W. Epilepsy and other chronic convulsive diseases. London: William Wood; 1885.
Bazil CW, Malow BA, Sammaritano MR. Sleep and epilepsy: the clinical spectrum. 1st ed. Amsterdam/New York: Elsevier; 2002.
Kataria L, Vaughn BV. Sleep and epilepsy. Sleep Med Clin. 2016 Mar;11(1):25–38.
Bazil CW. Seizure modulation by sleep and sleep state. Brain Res. 2018. https://doi.org/10.1016/j.brainres.2018.05.003. Epub ahead of print.
Jain SV, Kothare SV. Sleep and epilepsy. Semin Pediatr Neurol. 2015;22(2):86–92.
Hofstra WA, Gordijn MC, van der Palen J, et al. Timing of temporal and frontal seizures in relation to the circadian phase: a prospective pilot study. Epilepsy Res. 2011;94:158–62.
Iber C, Ancoli-Israel S, Chesson A, Quan SF, editors. The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. 1st ed. Westchester: American Academy of Sleep Medicine; 2007.
Tinuper P, Bisulli F, Provini F, Montagna P, Lugaresi E. Nocturnal frontal lobe epilepsy: new pathophysiological interpretations. Sleep Med. 2011;12(Suppl 2):S39–42.
Lugaresi E, Cirignotta F. Hypnogenic paroxysmal dystonia: epileptic seizures or a new syndrome? Sleep. 1981;4:129–38.
Tinuper P, et al. Definition and diagnostic criteria of sleep-related hypermotor epilepsy. Neurology. 2016;86(19):1834–42.
Nobili L, Cardinale F, Magliola U, Cicolin A, Didato G, Bramerio M, et al. Taylor’s focal cortical dysplasia increases the risk of sleep-related epilepsy. Epilepsia. 2009;50(12):2599–604.
Francione S, Nobili L, Cardinale F, Citterio A, Galli C, Tassi L. Intralesional stereo-EEG activity in Taylor’s focal cortical dysplasia. Epileptic Disord. 2003;5(Suppl 2):S105–14.
Scheffer IE, Bhatia KP, Lopes-Cendes I, Fish DR, Marsden CD, Andermann F, et al. Autosomal dominant frontal epilepsy misdiagnosed as sleep disorder. Lancet. 1994;343(8896):515–7.
Tinuper P, Bisulli F. From nocturnal frontal lobe epilepsy to sleep-related hypermotor epilepsy: a 35-year diagnostic challenge. Seizure. 2017;44:87–92.
Derry CP, Heron SE, Phillips F, Howell S, MacMahon J, Phillips HA, Duncan JS, Mulley JC, Berkovic SF, Scheffer IE. Severe autosomal dominant nocturnal frontal lobe epilepsy associated with psychiatric disorders and intellectual disability. Epilepsia. 2008;49(12):2125–9.
Steinlein OK. Genetics of idiopathic epilepsies. Handb Clin Neurol. 2012;107:145–51.
Ferri L, et al. Auditory aura in nocturnal frontal lobe epilepsy: a red flag to suspect an extra-frontal epileptogenic zone. Sleep Med. 2014;15(11):1417–23.
Proserpio P, Cossu M, Francione S, Gozzo F, Lo Russo G, Mai R, Moscato A, Schiariti M, Sartori I, Tassi L, Nobili L. Epileptic motor behaviors during sleep: anatomo-electro-clinical features. Sleep Med. 2011a;12(Suppl 2):S33–8.
Proserpio P, et al. Insular-opercular seizures manifesting with sleep-related paroxysmal motor behaviors: a stereo-EEG study. Epilepsia. 2011b;52(10):1781–91.
Gibbs SA, Figorilli M, Casaceli G, Proserpio P, Nobili L. Sleep related hypermotor seizures with a right parietal onset. J Clin Sleep Med. 2015;11(8):953–5.
Gibbs SA, Proserpio P, Francione S, Mai R, Cossu M, Tassi L, Nobili L. Seizure duration and latency of hypermotor manifestations distinguish frontal from extrafrontal onset in sleep-related hypermotor epilepsy. Epilepsia. 2018;59:e130–4.
Tassinari CA, Cantalupo G, Högl B, Cortelli P, Tassi L, Francione S, Nobili L, Meletti S, Rubboli G, Gardella E. Neuroethological approach to frontolimbic epileptic seizures and parasomnias: the same central pattern generators for the same behaviors. Rev Neurol (Paris). 2009;165(10):762–8.
Grillner S, Wallen P. Central pattern generators for locomotion, with special reference to vertebrates. Ann Rev Neurosci. 1985;8:233–61.
Tassinari CA, et al. Central pattern generators for a common semiology in fronto-limbic seizures and in parasomnias. A neuroethologic approach. Neurol Sci. 2005;26(Suppl 3):s225–32.
Gardella E, Rubboli G, Francione S, Tassi L, Lo Russo G, Grillner S, Tassinari CA. Seizure-related automatic locomotion triggered by intracerebral electrical stimulation. Epileptic Disord. 2008;10(4):247–52.
Castelnovo A, Lopez R, Proserpio P, Nobili L, Dauvilliers Y. NREM sleep parasomnias as disorders of sleep-state dissociation. Nat Rev Neurol. 2018;14(8):470–81.
Derry CP, Harvey AS, Walker MC, Duncan JS, Berkovic SF. NREM arousal parasomnias and their distinction from nocturnal frontal lobe epilepsy: a video EEG analysis. Sleep. 2009;32(12):1637–44.
Derry CP, Davey M, Johns M, Kron K, Glencross D, Marini C, et al. Distinguishing sleep disorders from seizures: diagnosing bumps in the night. Arch Neurol. 2006;63:705–9.
Bisulli F, Vignatelli L, Naldi I, Pittau F, Provini F, Plazzi G, et al. Diagnostic accuracy of a structured interview for nocturnal frontal lobe epilepsy (SINFLE): a proposal for developing diagnostic criteria. Sleep Med. 2012;13:81–7.
Manni R, Terzaghi M, Repetto A. The FLEP scale in diagnosing nocturnal frontal lobe epilepsy, NREM and REM parasomnias: data from a tertiary sleep and epilepsy unit. Epilepsia. 2008;49:1581–5.
Pal DK, et al. Idiopathic focal epilepsies: the “lost tribe”. Epileptic Disord. 2016;18(3):252–88.
Panayiotopoulos CP, Michael M, Sanders S, Valeta T, Koutroumanidis M. Benign childhood focal epilepsies: assessment of established and newly recognized syndromes. Brain. 2008;131(9):2264–86.
Lee YJ, Hwang SK, Kwon S. The clinical spectrum of benign epilepsy with centro-temporal spikes: a challenge in categorization and predictability. J Epilepsy Res. 2017;7(1):1–6.
Parisi P, Paolino MC, Raucci U, Ferretti A, Villa MP, Trenite DK. “Atypical forms” of benign epilepsy with centrotemporal spikes (BECTS): how to diagnose and guide these children. A practical/scientific approach. Epilepsy Behav. 2017;75:165–9.
Overvliet GM, Besseling RM, Jansen JF, van der Kruijs SJ, Vles JS, Hofman PA, et al. Early onset of cortical thinning in children with rolandic epilepsy. Neuroimage Clin. 2013;2:434–9.
Xiao F, Lei D, An D, Li L, Chen S, Chen F, et al. Functional brain connectome and sensorimotor networks in rolandic epilepsy. Epilepsy Res. 2015;113:113–25.
van Klink NE, van’t Klooster MA, Leijten FS, Jacobs J, Braun KP, Zijlmans M. Ripples on rolandic spikes: a marker of epilepsy severity. Epilepsia. 2016;57(7):1179–89.
Halász P. How sleep activates epileptic networks? Epilepsy Res Treat. 2013;2013:425697. https://doi.org/10.1155/2013/425697. Epub 2013 Sep 12.
Kim H, Yoo IH, Lim BC, Hwang H, Chae JH, Choi J, et al. Averaged EEG spike dipole analysis may predict atypical outcome in benign childhood epilepsy with centro-temporal spikes (BCECTS). Brain Dev Jpn Soc Child Neurol. 2016;38(10):903e8.
Tassinari CA, Dravet CR. Encephalopathy related to electrical status epilepticus during slow sleep. Electroencephalogr Clin Neurophysiol. 1977;43:529e30.
Commission on Classification and Terminology of the International League Against Epilepsy. Proposal for revised classification of epilepsies and epileptic syndromes. Epilepsia. 1989;30(4):389e99.
Kessi M, Peng J, Yang L, Xiong J, Duan H, Pang N, Yin F. Genetic etiologies of the electrical status epilepticus during slow wave sleep: systematic review. BMC Genet. 2018;19(1):40.
Striano P, Capovilla G. Epileptic encephalopathy with continuous spikes and waves during sleep. Curr Neurol Neurosci Rep. 2013;13(7):360.
de Kovel CGF, Syrbe S, Brilstra EH, Verbeek N, Kerr B, Dubbs H, Bayat A, Desai S, Naidu S, Srivastava S, et al. Neurodevelopmental disorders caused by De novo variants in KCNB1 genotypes and phenotypes. JAMA Neurol. 2017;74(10):1228–36.
Kothare SV, Kaleyias J. Sleep and epilepsy in children and adolescents. Sleep Med. 2010;11:674–85.
Touchon J, Baldy-Moulinier M, Billiard M, Besset A, Cadilhac J. Sleep organization and epilepsy. Epilepsy Res Suppl. 1991;2:73–81.
Nunes ML, Ferri R, Arzimanoglou A, Curzi L, Appel CC, Costa da Costa J. Sleep organization in children with partial refractory epilepsy. J Child Neurol. 2003;18:763–6.
Wang YQ, Zhang MQ, Li R, Qu WM, Huang ZL. The mutual interaction between sleep and epilepsy on the neurobiological basis and therapy. Curr Neuropharmacol. 2018;16(1):5–16.
Dinopoulos A, Tsirouda MA, Bonakis A, Pons R, Pavlopoulou ID, Tsoumakas K. Sleep architecture and epileptic characteristics of drug naïve patients in childhood absence epilepsy spectrum. A prospective study. Seizure. 2018;59:99–107.
Parrino L, De Paolis F, Milioli G, Gioi G, Grassi A, Riccardi S, Colizzi E, Terzano MG. Distinctive polysomnographic traits in nocturnal frontal lobe epilepsy. Epilepsia. 2012;53(7):1178–84.
Halal CDS, Horta BL, Nunes ML. Polysomnographic aspects of sleep architecture on self-limited epilepsy with centrotemporal spikes: a systematic review and meta-analysis. Sleep Sci. 2017;10(4):161–7.
Deray MJ, Epstein MA. Sleep abnormalities in children with intractable epilepsy. Sleep Res. 1991;20:98.
Bruni O, Cortesi F, Giannotti F, Curatolo P. Sleep disorders in tuberous sclerosis: a polysomnographic study. Brain and Development. 1995;17:52–6.
Pereira AM, Bruni O, Ferri R, Palmini A, Nunes ML. The impact of epilepsy on sleep architecture during childhood. Epilepsia. 2012;53(9):1519–25.
Ferri R, Bruni O, Miano S, Terzano MG. Topographic mapping of the spectral components of the cyclic alternating pattern (CAP). Sleep Med. 2005;6:29–36.
Terzano MG, et al. Cyclic alternating pattern as a provocative factor in nocturnal paroxysmal dystonia. Epilepsia. 1997;38(9):1015–25.
Terzaghi M, Sartori I, Mai R, Tassi L, Francione S, Cardinale F, Castana L, Cossu M, LoRusso G, Manni R, Nobili L. Coupling of minor motor events and epileptiform discharges with arousal fluctuations in NFLE. Epilepsia. 2008;49(4):670–6.
Bruni O, Novelli L, Luchetti A, Zarowski M, Meloni M, Cecili M, Villa M, Ferri R. Reduced NREM sleep instability in benign childhood epilepsy with centro-temporal spikes. Clin Neurophysiol. 2010;121(5):665–71.
Miano S, Bachiller C, Gutiérrez M, Salcedo A, Villa MP, Peraita-Adrados R. Paroxysmal activity and seizures associated with sleep breathing disorder in children: a possible overlap between diurnal and nocturnal symptoms. Seizure. 2010;19(9):547–52.
Latreille V, St Louis EK, Pavlova M. Co-morbid sleep disorders and epilepsy: a narrative review and case examples. Epilepsy Res. 2018;145:185–97.
Macêdo PJOM, Oliveira PS, Foldvary-Schaefer N, Gomes MDM. Insomnia in people with epilepsy: a review of insomnia prevalence, risk factors and associations with epilepsy-related factors. Epilepsy Res. 2017;135:158–67.
Grigg-Damberger MM, Ralls F. Sleep disorders in adults with epilepsy: past, present, and future directions. Curr Opin Pulm Med. 2014;20(6):542–9.
Paprocka J, Dec R, Jamroz E, et al. Melatonin and childhood refractory epilepsy—a pilot study. Med Sci Monit. 2010;16:CR389–96.
Liu F, Wang X. Diagnosis and treatment of epilepsy and sleep apnea comorbidity. Expert Rev Neurother. 2017;17(5):475–85.
Jain SV, Horn PS, Simakajornboon N, et al. Melatonin improves sleep in children with epilepsy: randomized, double-blind cross-over study. Sleep Med. 2015;16:637.
Jain S, Besag FM. Does melatonin affect epileptic seizures? Drug Saf. 2013;36(4):207–15.
Kasteleijn-Nolst Trenité D, Parain D, Genton P, Masnou P, Schwartz JC, Hirsch E. Efficacy of the histamine 3 receptor (H3R) antagonist pitolisant (formerly known as tiprolisant; BF2.649) in epilepsy: dose-dependent effects in the human photosensitivity model. Epilepsy Behav. 2013;28(1):66–70.
Miano S, Tabarrini A, Vitelli O, Mazzotta A, Del Pozzo M, Rabasco J, Barreto M, Parisi P, Ferretti A, Villa MP. The cooccurrence of interictal discharges and seizures in pediatric sleep-disordered breathing. Epilepsy Behav. 2013;29(3):508–12.
Lin Z, Si Q, Xiaoyi Z. Obstructive sleep apnoea in patients with epilepsy: a metanalysis. Sleep Breath. 2017;21:263–70.
Khachatryan SG, Prosperetti C, Rossinelli A, Pedrazzi P, Agazzi P, Ratti PL, Manconi M. Sleep-onset central apneas as triggers of severe nocturnal seizures. Sleep Med. 2015;16(8):1017–9.
Jain SV, Simakajornboon S, Shapiro SM, Morton LD, Leszczyszyn DJ, Simakajornboon N. Obstructive sleep apnea in children with epilepsy: prospective pilot trial. Acta Neurol Scand. 2012;125(1):e3–6.
Kaleyias J, Cruz M, Goraya JS, Valencia I, Khurana DS, Legido A, Kothare SV. Spectrum of polysomnographic abnormalities in children with epilepsy. Pediatr Neurol. 2008;39(3):170–6.
Miano S, Bruni O, Elia M, Musumeci SA, Verrillo E, Ferri R. Sleep breathing and periodic leg movement pattern in Angelman syndrome: a polysomnographic study. Clin Neurophysiol. 2005;116(11):2685–92.
Miano S, Bruni O, Aricò D, Elia M, Ferri R. Polysomnographic assessment of sleep disturbances in children with developmental disabilities and seizures. Neurol Sci. 2010b;31(5):575–83.
Segal E, Vendrame M, Gregas M, Loddenkemper T, Kothare SV. Effect of treatment of obstructive sleep apnea on seizure outcomes in children with epilepsy. Pediatr Neurol. 2012;46:359–62.
Miano S, Paolino MC, Peraita-Adrados R, Montesano M, Barberi S, Villa MP. Prevalence of EEG paroxysmal activity in a population of children with obstructive sleep apnea syndrome. Sleep. 2009;32(4):522–9.
Sans Capdevila O, Dayyat E, Kheirandish-Gozal L, Gozal D. Prevalence of epileptiform activity in healthy children during sleep. Sleep Med. 2008;9:303–9.
Gogou M, Haidopoulou K, Eboriadou M, Pavlou E. Sleep disturbances in children with rolandic epilepsy. Neuropediatrics. 2017;48(1):30–5.
Miano S, Pelliccia A, Evangelisti M, Pagani J, Villa MP. Role of continuous positive airway pressure therapy on the pathogenesis of sleep-related frontal lobe epilepsy in a child with obstructive sleep apnea syndrome. J Child Neurol. 2008;23(1):124–8.
Andrade EO, Arain A, Malow BA. Partial epilepsy presenting as apneic seizures without posturing. Pediatr Neurol. 2006;35:359–62.
Seo WH, Park M, Eun SH, Rhie S, Song DJ, Chae KY. My child cannot breathe while sleeping: a report of three cases and review. BMC Pediatr. 2017;17(1):169.
Vitelli O, Miano S, Tabarrini A, Mazzotta AR, Supino MC, Forlani M, Villa MP. Epilepsy and sleep-disordered breathing as false friends: a case report. J Child Neurol. 2014;29(10):NP114–7.
Parrino L, Milioli G, Grassi A, et al. Atypical patterns in portable monitoring for sleep apnoea: features of nocturnal epilepsy? Eur Respir J. 2013;41:368–75.
Miano S, Peraita-Adrados R. Nocturnal frontal lobe epilepsy is often misdiagnosed as sleep disorders in children: a case series. Rev Neurol. 2013;56(5):257–67.
Arico I, Condurso R, Granata F, Nobili L, Bruni O, Silvestri R. Nocturnal frontal lobe epilepsy presenting with restless leg syndrome-like symptoms. Neurol Sci. 2011;32:313–5.
Ismayilova V, Demir AU, Tezer FI. Subjective sleep disturbance in epilepsy patients at an outpatient clinic: a questionnaire-based study on prevalence. Epilepsy Res. 2015;115:119–25.
Manni R, Terzaghi M, Zambrelli E. REM sleep behavior disorder in elderly subjects with epilepsy: frequency and clinical aspects of the comorbidity. Epilepsy Res. 2007;77:128–33.
Manni R, Terzaghi M, Zambrelli E, Pacchetti C. Interictal, potentially misleading, epileptiform EEG abnormalities in REM sleep behavior disorder. Sleep. 2006;29:934–7.
Myers KA, Bello-Espinosa LE, Symonds JD, Zuberi SM, Clegg R, Sadleir LG, Buchhalter J, Scheffer IE. Heart rate variability in epilepsy: a potential biomarker of sudden unexpected death in epilepsy risk. Epilepsia. 2018;59(7):1372–80. https://doi.org/10.1111/epi.14438.
Ali A, Wu S, Issa NP, Rose S, Towle VL, Warnke P, Tao JX. Association of sleep with sudden unexpected death in epilepsy. Epilepsy Behav. 2017;76:1–6.
Ryvlin P, Nashef L, Lhatoo SD, Bateman LM, Bird J, Bleasel A, et al. Incidence and mechanisms of cardiorespiratory arrests in epilepsy monitoring units (MORTEMUS): a retrospective study. Lancet Neurol. 2013;12:966–77.
Parhizgar F, Nugent K, Raj R. Obstructive sleep apnea and respiratory complications associated with vagus nerve stimulators. J Clin Sleep Med. 2011;7:401–7.
Carreño M, Fernández S. Sleep-related epilepsy. Curr Treat Options Neurol. 2016;18(5):23.
Ott D, R C, Guthrie D, et al. Measures of psychopathology in children with complex partial seizures and primary generalized epilepsy with absence. J Am Acad Child Adolesc Psychiatry. 2001;40:907–14.
Parisi P, Bruni O, Pia Villa M, Verrotti A, Miano S, Luchetti A, Curatolo P. The relationship between sleep and epilepsy: the effect on cognitive functioning in children. Dev Med Child Neurol. 2010;52(9):805–10.
Aldenkamp AP, Arends J, Verspeek S, Berting M. The cognitive impact of epileptiform EEG-discharges; relationship with type of cognitive task. Child Neuropsychol. 2004;10(4):297–305.
Terzano MG, Parrino L, Anelli S, Halasz P. Modulation of generalized spike-and-wave discharges during sleep by cyclic alternating pattern. Epilepsia. 1989;30(6):772–81.
Metz-Lutz MN, Filippini M. Neuropsychological findings in rolandic epilepsy and Landau-Kleffner syndrome. Epilepsia. 2006;47(2):71–5.
Deonna T, Roulet-Perez E. Early-onset acquired epileptic aphasia (Landau-Kleffner syndrome, LKS) and regressive autistic disorders with epileptic EEG abnormalities: the continuing debate. Brain and Development. 2010;32(9):746–52.
Besseling RM, Jansen JF, Overvliet GM, et al. Reduced functional integration of the sensorimotor and language network in rolandic epilepsy. Neuroimage Clin. 2013;2:239–46.
Melissa F, Antonella B, Melania G, Antonella P, Angelo R, Assunta MM, et al. Comparing cortical auditory processing in children with typical and atypical benign epilepsy with centrotemporal spikes: electrophysiologic evidence of the role of non-rapid eye movement sleep abnormalities. Epilepsia. 2015;56:726–34.
Tassinari CA, Rubboli G, Volpi L, et al. Encephalopathy with electrical status epilepticus during slow sleep or ESES syndrome including the acquired aphasia. Clin Neurophysiol. 2000;111(supplement 2):S94–S102.
Bölsterli BK, Gardella E, Pavlidis E, Wehrle FM, Tassinari CA, Huber R, Rubboli G. Remission of encephalopathy with status epilepticus (ESES) during sleep renormalizes regulation of slow wave sleep. Epilepsia. 2017;58(11):1892–901.
Licchetta L, et al. Profile of neuropsychological impairment in Sleep-related Hypermotor Epilepsy. Sleep Med. 2018;48:8–15.
Busonera G, Cogoni M, Puligheddu M, Ferri R, Milioli G, Parrino L, Marrosu F, Zanetti GEEG. Spectral coherence analysis in nocturnal epilepsy. IEEE Trans Biomed Eng. 2018;65:2713.
Marcus C. Orexin and epilepsy: potential role of REM sleep. Sleep. 2017;40(3).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Miano, S. (2021). Sleep in Seizure Disorders. In: DelRosso, L.M., Ferri, R. (eds) Sleep Neurology. Springer, Cham. https://doi.org/10.1007/978-3-030-54359-4_11
Download citation
DOI: https://doi.org/10.1007/978-3-030-54359-4_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-54358-7
Online ISBN: 978-3-030-54359-4
eBook Packages: MedicineMedicine (R0)