Opinion statement
When treating a person with epilepsy, one must consider many factors in addition to the obvious need to treat the seizures. Both epilepsy itself and treatment with antiepileptic drugs (AEDs) subject one to numerous potential secondary long-term health concerns. Poor bone health is one of these concerns. Studies suggest that persons with epilepsy treated with AEDs have an increased risk of fracture, low bone mineral density (BMD), and abnormalities in bone metabolism. Multiple factors likely contribute to the increased risk. Falls during generalized tonic-clonic seizures, secondary effects of AEDs on balance, inactivity, low BMD, reduced calcium intake, reduced active vitamin D metabolites, and a genetic predisposition to low BMD may all contribute. Studies suggest a differential influence of AEDs. Phenytoin, phenobarbital, and primidone are most consistently associated with a negative impact on bone. Carbamazepine and valproate may also result in bone abnormalities, but data are mixed. Current studies suggest that lamotrigine has limited (if any) effect, but again, data are inconsistent. Other AEDs have received limited study. Screening for poor bone health includes serologic testing of vitamin D metabolites (notably 25-hydroxyvitamin D) as well as BMD testing using dual energy x-ray absorptiometry. Optimizing intake of calcium and vitamin D is important for all persons with epilepsy treated with AEDs. Although many treatments for low BMD are available, these agents have not been studied in persons with epilepsy treated with AEDs. Overall, physicians treating persons with epilepsy must consider the potential effect of having epilepsy and its main treatment, AED therapy, on bone health. For patients in whom bone health is a particular concern (eg, those with diagnosed bone disease or with significant risk factors for bone disease, including glucocorticosteroid use), it is best to avoid AEDs known to negatively affect bone. In addition, practitioners should work with other treating physicians to optimize bone health in these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
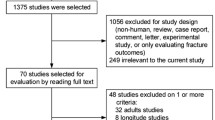
Epilepsy is a chronic condition that may affect individuals for years. Both seizures and treatment can have adverse effects. Optimizing the treatment for affected persons includes addressing long-term effects on bone health. Identification and treatment of poor bone health has gained increased attention. Osteoporosis is recognized as a significant disease process that should be prevented, identified, and treated. Efforts to increase public awareness of diseases of bone include the recent Decade of the Bone and Joint (2001 to 2011) and the first-ever US Surgeon General Report on Bone Health and Osteoporosis, released in 2004. Persons with epilepsy treated with antiepileptic drugs (AEDs) have an increased risk of fracture, low bone density, and abnormalities in bone metabolism. Studies suggest that enzyme-inducing AEDs, particularly phenytoin, phenobarbital, and primidone, are commonly associated with reduced vitamin D metabolites and low bone mineral density (BMD). Studies provide contradictory results for many other AEDs, including carbamazepine, valproate, and lamotrigine. This article reviews recent literature assessing the impact of epilepsy and AEDs on fracture, BMD, and bone metabolism. In addition, the differential effect of individual AEDs, potential mechanisms to explain reported abnormalities, and treatment for poor bone health will be discussed.
Fracture Risk
Persons with epilepsy treated with AEDs are at increased risk for fracture. Reports suggest that the risk of fracture in children and adults with epilepsy is two to six times greater than in the general population [1, Class IV]. A population-based study using the General Practice Research Database (GPRD) of over 40,000 patients with epilepsy found that after controlling for age and sex, the risk of fracture was approximately twofold higher than in a control group of over 80,000 individuals [2, Class III]. Multiple factors likely contribute to the increased risk. For example, the propensity to fall influences the risk of fracture. Persons with epilepsy are more likely to fall as a result of seizures as well as AED exposure. In a study of 29 ambulatory, community-dwelling twin and sibling pairs, balance performance was found to be impaired in the AED users, suggesting that balance impairment may contribute to the increased risk of fractures [3•, Class III]. The role of multiple factors is highlighted by a meta-analysis finding that in persons with epilepsy, BMD was significantly decreased and the risk of fracture was increased [4, Class IV]. The authors found that the reduction in BMD was not enough to explain the elevated fracture risk. The authors concluded that bone disease and seizure-related injury interact to increase the fracture risk.
The impact of seizures on fracture risk has received much study, with conflicting results. Population-based studies find that trauma related to seizures is not associated with fractures [5, Class IV]. Generalized tonic-clonic seizures, however, are associated with a higher risk for fracture than are partial seizures [6, Class III].
AED exposure likely increases fracture risk. Using the GPRD and a nested case–control study design, long-term AED use was associated with an increased risk of fracture, particularly in women [7, Class III]. Similarly, a case–control study using data from the Funen County, Denmark, hip register found that fracture risk was increased with AED use [8, Class III]. The use of enzyme-inducing AEDs independently increased the risk of fracture, but non-inducing AEDs did not. The risk was associated with higher daily doses of current and recent AED use. Results from a pharmacoepidemiologic, population-based, case–control study, also in Denmark, suggests that there may be a differential effect of AEDs on fracture risk [9, Class III]. After adjusting for significant confounders including a diagnosis of epilepsy, treatment with carbamazepine, clonazepam, phenobarbital, and valproate were all associated with a significant increase in fracture risk.
Bone Mineral Density
BMD is currently the most significant predictor of fracture. The most-studied and best-understood technique to assess BMD is dual-energy x-ray absorptiometry (DXA). Using DXA, the obtained BMD measurement (in g/cm2) is compared to large databases. This comparison yields two standard deviation scores: T-score and Z-score. The T-score compares the obtained BMD measurement to a population at peak BMD, matched by sex and race, whereas the Z-score compares the BMD measurement to an age-matched population. Currently, the World Health Organization defines osteoporosis and osteopenia in postmenopausal women and older men using the T-score. In young persons, Z-scores less than −2.0 are defined as low BMD. Using DXA, multiple studies have assessed BMD among persons with epilepsy treated with AEDs and found osteopenia or osteoporosis in 38% to 60% of persons with epilepsy treated with AEDs in tertiary epilepsy clinics [10–12, Class III]. Longer AED use was associated with decreased BMD in studies examining this association [10, 11, 13, Class III].
Osteoporosis does not affect only women. In the general population, evidence of osteoporosis is common in older men. Among persons with epilepsy, studies find that men have evidence of low BMD and are vulnerable to low-trauma fractures [14, Class III]. A prospective study of men with epilepsy treated with AEDs who were between the ages 25 and 54 found significant reductions in BMD, most notably significant femoral neck declines after 1 year of AED treatment among men in the youngest age group (ages 25–44) [10, Class III]. Similarly, young males with more chronic epilepsy (≥ 6 years) had the lowest BMD among a group of 108 ambulatory males and females with epilepsy who were between the ages of 6 and 18 years [14, Class III]. These authors concluded that age at onset of epilepsy, growth trends, and hormonal differences may influence the reported differences.
Childhood and adolescence are critical periods for bone development and mineralization. Peak BMD is obtained between the ages of 20 and 30 years. During childhood and adolescence, numerous factors, including diseases, inactivity, and low vitamin D intake, may lead to abnormal bone architecture and a subsequent increase in fractures [15, Class IV]. Epilepsy and chronic AED exposure contribute to abnormal bone mineralization and potentially abnormal bone accrual. Multiple studies using DXA have found low BMD in children and adolescents with epilepsy when compared with controls without epilepsy, not taking AEDs [13, 16, 17, Class III]. A cross-sectional study compared BMD of 82 ambulatory children (ages 6–18) with epilepsy for either less than 1 year, 1 to 5 years, or 6 or more years with that of healthy children [17, Class III]. Z-scores corrected for age and sex were used in the analysis. The total BMD Z-score was lower in children with epilepsy. Increasing duration of epilepsy was associated with a progressive reduction in BMD compared with controls.
Cerebral palsy and mental retardation are independently associated with low BMD. In a cohort of 117 children and adolescents with moderate to severe cerebral palsy, 77% of studied patients had evidence of low BMD [18, Class III]. AED use was among the factors that correlated with low BMD. Another study aimed to assess BMD in children, adolescents, and young adults with epilepsy alone or in association with cerebral palsy and/or mental retardation [16, Class III]. A total of 96 subjects were studied. Results were compared with those for 63 healthy controls. Abnormal BMD was found in almost 60% of children, adolescents, and young adults with cerebral palsy (n = 47). Among the total group, lack of autonomous gait, severe mental retardation, prolonged AED therapy, adjunctive topiramate therapy, and less physical activity all significantly correlated with abnormal BMD.
Bone Metabolism
Calcium and calciotropic hormones are integral to bone health and may be affected in persons with epilepsy who are taking AEDs. Calcium homeostasis is a tightly regulated process and an integral function of bone. Vitamin D, the parathyroid gland, and calcitonin are all directly and indirectly involved. In addition to playing a critical role in calcium homeostasis, vitamin D has direct effects on bone, such as promoting differentiation of osteoclasts. Studies suggest that persons with epilepsy often do not get enough calcium. A study of 144 patients with epilepsy in India found that all had low dietary calcium intake, compared with the recommended daily allowance [19, Class III]. Active vitamin D metabolites, notably 25-hydroxyvitamin D, also may be low in persons with epilepsy [1, 5, Class IV], but this is not a consistent finding. Enzyme-inducing AEDs are most commonly associated with lower levels of 25-hydroxyvitamin D [1, 5, Class IV]. In one study, healthy children treated with non–enzyme-inducing AEDs had no evidence of vitamin D deficiency [20, Class III]. Another study in children found an association between polytherapy and vitamin D deficiency [21, Class III].
Bone turnover markers are measurements of bone formation and bone resorption. Elevated bone turnover markers reflect increased bone remodeling activity, are associated with higher rates of bone loss, and are independent predictors of fracture [22, Class IV]. Elevations in bone formation and resorption markers have been reported during long-term AED therapy, as well as after initiation of AED therapy [1, 5, 15, Class IV].
Effect of Antiepileptic Drugs
Cytochrome P450 enzyme-inducing AEDs, including phenytoin, primidone, and phenobarbital, are most commonly associated with a negative impact on bone. For example, in a prospective study, women with epilepsy receiving phenytoin sustained significant bone loss in the femoral neck after 1 year [23, Class II]. Compared with a study of 614 healthy premenopausal women [24, Class III], the loss observed at this site in the women receiving phenytoin was more than 8 times greater. Similarly, among postmenopausal women in the Study of Osteoporotic Fractures [25, Class II], phenytoin use was the most significant factor found to negatively affect BMD. Persons treated with phenytoin, primidone, and phenobarbital are more likely to have lower active vitamin D metabolites and elevated markers of bone turnover [1, 5, 15, Class IV].
Carbamazepine
Although carbamazepine is an enzyme-inducing AED, the data conflict regarding its use. Some studies find changes in bone density and turnover, whereas others do not. One study found a change in bone turnover markers [26, 27, Class II] in children treated with carbamazepine. Prior to the initiation of carbamazepine treatment, adolescents had an evaluation of calcium, vitamin D metabolites, parathyroid hormone, and bone turnover markers and were compared with controls matched for age, sex, and pubertal stage. Significant changes in turnover markers but not in parathyroid hormone or vitamin D metabolites were found after 1 and 2 years of treatment, suggesting possible long-term effects on bone density in these adolescents secondary to elevated turnover. Similarly a 6-month longitudinal study found significant BMD reductions in persons treated with carbamazepine [28, Class III]. In contrast, premenopausal women had no significant bone loss after 1 year of treatment in another study [23, Class II].
Oxcarbazepine
Oxcarbazepine at higher doses is also an enzyme inducer. Adults treated with this AED had reduced vitamin D metabolites and elevated parathyroid hormone that was most significant at higher doses [29, Class III]. Children with newly diagnosed epilepsy who had normal BMD, biochemical markers of bone formation, and hormonal markers were treated with oxcarbazepine and then had repeat bone health assessments [30, Class III]. Serum 25-hydroxyvitamin D significantly decreased, and osteocalcin (a marker of bone formation) significantly increased, but these changes did not correlate with a decrease in BMD during 1.5 years of oxcarbazepine treatment.
Valproate
Although early reports found no effects of valproate on bone, some recent studies have found increased fracture rates, BMD loss, and laboratory markers of bone disease in children and adults [1, 5, Class IV; 12, Class III; 15, Class IV]. These findings are not consistent among all recently published reports [23, Class II]. Long-term valproate monotherapy in 40 adults resulted in decreased BMD and increased serum concentrations of calcium, low vitamin D metabolites, and increased markers of bone resorption and formation [12, Class III]. Similarly, children treated with valproate had decreased BMD and elevated markers of bone turnover when compared with children not treated with AEDs [13, 31, Class III] or treated with carbamazepine [13, Class III]. Twenty postpubertal males with newly diagnosed idiopathic generalized epilepsy showed significant elevation of markers of bone formation and resorption after 1 year of treatment [32, Class II]. In contrast, 14 premenopausal women treated with valproate monotherapy demonstrated no significant change in markers of bone turnover or bone loss after 1 year of treatment [23, Class II].
New-Generation Antiepileptic Drugs
There has been limited study of the potential effects on bone of the new generation of AEDs. Results from a large, prospective study in older men identified non–enzyme-inducing AEDs, mostly gabapentin, as being associated with bone loss [33•, Class II].
Of the new-generation AEDs, lamotrigine has received the most study. The data regarding its effects on bone are mixed, similar to other AEDs. Lamotrigine treatment for more than 2 years in children was associated with shorter stature, lower BMD, and reduced bone formation, but the major predictor of lower BMD was physical inactivity [31, Class III]. Another prospective study found elevated osteocalcin, a marker of bone formation, in association with lamotrigine treatment [28, Class III]. In contrast, premenopausal women treated with lamotrigine did not have significant reductions in BMD or changes in bone turnover markers [23, Class II]. As well, a study of children found no difference in BMD between those with epilepsy treated with lamotrigine monotherapy versus controls [34, Class III].
Topiramate and zonisamide are both carbonic anhydrase inhibitors. Treatment with these agents results in renal acidosis, which is associated with secondary abnormalities of bone. Interestingly, because carbonic anhydrase potentiates the action of osteoclasts, inhibitors may have a bone-sparing effect. This hypothesis is supported by findings in women with glaucoma treated with acetazolamide, another carbonic anhydrase inhibitor [35, Class III].
Data on levetiracetam’s effects on bone are also limited. An animal study found that levetiracetam therapy may affect bone quality [36]. Rats treated with low-dose levetiracetam had reduced bone strength and bone formation, with no changes in bone mass.
Mechanisms of AED Effects on Bone
As stated previously, cytochrome P450 enzyme-inducing AEDs are most consistently associated with abnormalities in bone. It has long been hypothesized that this effect is related to induction of the hepatic cytochrome P450 enzyme system. Treatment with liver-inducing AEDs increases activity of hepatic mixed-function oxidases and thus accelerates metabolism of vitamin D, resulting in less biologically active vitamin D. Reduced active vitamin D leads to decreased intestinal calcium absorption, decreased serum calcium concentration, and a compensatory increased serum parathyroid hormone concentration [1, 5, Class IV]. If hyperparathyroidism persists, BMD decreases. Osteomalacia results because of a mineralization defect secondary to chronically reduced vitamin D and calcium. Serologic studies revealing low calcium, low active vitamin D metabolites, and high parathyroid hormone support this mechanism [1, 5, Class IV].
In addition, these clinical findings are supported by basic studies evaluating the effect of enzyme-inducing AEDs on the expression of specific cytochrome P450 isoenzymes involved in vitamin D metabolism. Phenobarbital, phenytoin, and carbamazepine are among a class of drugs known as xenobiotics. Xenobiotics activate a nuclear receptor known as either the steroid and xenobiotic receptor (SXR) or the pregnane X receptor (PXR). One study found that xenobiotics upregulate 25-hydroxyvitamin D3-24-hydroxylase (CYP24) in the kidney through activation of PXR. This enzyme catalyzes the conversion of 25-hydroxyvitamin D to its inactive metabolite, 24,25-dihydroxyvitamin, rather than to its active metabolite, 1,25-dihydroxyvitamin D [37]. Other investigators found that xenobiotic activation of PXR did not upregulate CYP24 but did increase expression of a different isoenzyme, CYP3A4, in the liver and small intestine [38]. This enzyme converts vitamin D to more polar metabolites, which are inactive.
Results from many studies contradict the hypothesis that the enzyme-inducing properties of some AEDs lead to decreased vitamin D, low calcium, hyperparathyroidism, decreased BMD, and fracture. In some studies comparing groups treated with either enzyme-inducing AEDs or non–enzyme-inducing AEDs, 25-hydroxyvitamin D did not differ [39, 40, Class III]. Moreover, carbamazepine, an enzyme-inducing AED, is consistently not associated with decreased BMD [1, 5, 15, Class IV], whereas valproate, an enzyme inhibitor, often is [1, 5, Class IV; 12, 13, Class III; 15, Class IV].
Other potential mechanisms have been proposed and investigated [5, Class IV]. AEDs could have a direct impact on calcium absorption or on bone cells (osteoblasts or osteoclasts). AEDs may disrupt vitamin K metabolism, similar to the proposed effects on Vitamin D. Vitamin K is a cofactor required for the carboxylation of Gla proteins, which are synthesized by osteoblasts. In support of the vitamin K hypothesis, phenytoin administration decreases serum vitamin K2, serum osteocalcin, and BMD in animal models. Phenytoin’s effects are reversed with vitamin K2 supplementation [5, Class IV]. AEDs could affect calcitonin secretion. Calcitonin inhibits bone resorption induced by parathyroid hormone, and in animal studies, phenytoin treatment decreases calcitonin secretion. Enzyme-inducing AEDs may also adversely affect reproductive sex steroid hormones, which may have a direct impact on bone health, particularly as estrogen is a significant factor in bone modeling and remodeling.
It is also possible that epilepsy disrupts central nervous system control of bone metabolism and thus negatively affects bone. This effect may be mediated through the hormone leptin. Leptin activates adrenergic receptors on the surface of osteoblasts, decreasing osteoblast numbers and bone formation. In animal models, seizures increase serum leptin levels [41], potentially decreasing bone formation.
Genetics may influence the risk of low BMD and abnormal vitamin D metabolites. Genotyping of the vitamin D receptor (VDR) was performed in 73 ambulatory patients with epilepsy who were receiving long-term AED monotherapy [42•, Class III; 43, Class IV]. The results suggested that persons with epilepsy treated with AEDs are at increased risk for decreased BMD and decreased active vitamin D metabolites if they have the B allele of the BsmI polymorphism of the VDR gene. Restriction site polymorphisms in the VDR gene, including BsmI, are associated with both BMD changes and fracture [44, Class IV].
Screening
Currently, there are no official recommendations for screening bone health in persons with epilepsy treated with AEDs. As the most sensitive predictor of fracture at this time is BMD, it is reasonable to consider obtaining BMD measurements using DXA in persons at risk. The FRAX® tool [45] can be used to assess a patient’s risk of fracture. This tool was developed by the World Health Organization to evaluate fracture risk. It addresses the impact of low BMD and factors known to increase one’s risk of low BMD and fracture. A prior history of fracture, family history of osteoporosis and fracture, glucocorticoid steroid use, history of rheumatoid arthritis, tobacco use, and chronic alcohol use are among the factors addressed in this tool. In practice, these risk factors should be addressed in addition to the potential impact of having epilepsy and AED treatment. Routine screening of 25-hydroxyvitamin D should be considered, particularly in persons treated with enzyme-inducing AEDs. There is no defined role for obtaining bone turnover markers, although they may be useful if available.
Treatment
-
Limited study has been done on treatment for poor bone health in persons with epilepsy treated with AEDs. A randomized double-blind trial over 1 year compared supplementation with low-dose vitamin D (400 IU per day for adults and children) versus high-dose vitamin D (4000 IU per day for adults and 2000 IU per day for children) [46, Class II]. In the adults, the baseline BMD was reduced at all sites when compared with controls matched for age and gender. After 1 year, there were significant increases in BMD at all sites in those receiving high-dose vitamin D supplementation, but not low-dose. The children had normal BMD when compared with matched controls and had significant and comparable increases in BMD in both treatment groups. This study suggests that persons with epilepsy treated with AEDs should be counseled about adequate vitamin D intake. For those taking enzyme-inducing AEDs, higher doses of vitamin D than currently recommended are suggested. In addition, adequate calcium intake is advised, with supplementation if necessary.
-
The Institute of Medicine recently submitted a report regarding daily intake of calcium and vitamin D. The recommended daily allowance of calcium ranges between 700 and 1300 mg per day depending on age, sex, and reproductive status (Table 1) [47]. (Calcium intake greater than the recommended upper limit is associated with kidney stones.) The recommended daily allowance of vitamin D is 600 IU per day. The report cautions that the use of more than 4000 IU per day may increase the risk of potential harm, including renal and tissue damage.
Table 1 Recommended daily allowance and upper daily allowance of calcium across the lifespan -
There are no studies of the effects of bisphosphonates, selective estrogen receptor modulators, and parathyroid hormone in persons with epilepsy treated with AEDs.
-
For persons in whom bone health is of particular concern, such as those with diagnosed bone disease or with significant risk factors for bone disease, current data support avoiding AEDs known to adversely affect bones. Collaborating with other treating physicians to optimize bone health is also important.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance
Pack A. Bone health in people with epilepsy: Is it impaired and what are the risk factors? Seizure. 2008;17(2):18.
Souverein PC, Webb DJ, Petri H, et al. Incidence of fractures among epilepsy patients: a population-based retrospective cohort study in the General Practice Research Database. Epilepsia. 2005;46(2):304–10.
Petty SJ, Hill KD, Haber NE, et al. Balance impairment in chronic antiepileptic drug users: a twin and sibling study. Epilepsia 2010, 51(2):280–8.
Vestergaard P. Epilepsy, osteoporosis and fracture risk—a meta-analysis. Acta Neurol Scand. 2005;112(5):277–86.
Pack AM, Walczak TS. Bone health in women with epilepsy: clinical features and potential mechanisms. Int Rev Neurobiol. 2008;83:305–28.
Persson HB, Alberts KA, Farahmand BY, Tomson T. Risk of extremity fractures in adult outpatients with epilepsy. Epilepsia. 2002;43(7):768–72.
Souverein PC, Webb DJ, Weil JG, Van Staa TP, Egberts AC. Use of antiepileptic drugs and risk of fractures: case-control study among patients with epilepsy. Neurology. 2006;66(9):1318–24.
Tsiropoulos I, Andersen M, Nymark T, et al. Exposure to antiepileptic drugs and the risk of hip fracture: a case-control study. Epilepsia. 2008;49(12):2092–9.
Vestergaard P, Rejnmark L, Mosekilde L. Fracture risk associated with use of antiepileptic drugs. Epilepsia. 2004;45(11):1330–7.
Andress DL, Ozuna J, Tirschwell D, et al. Antiepileptic drug–induced bone loss in young male patients who have seizures. Arch Neurol. 2002;59(5):781–6.
Farhat G, Yamout B, Mikati MA, et al. Effect of antiepileptic drugs on bone density in ambulatory patients. Neurology. 2002;58(9):1348–53.
Sato Y, Kondo I, Ishida S, et al. Decreased bone mass and increased bone turnover with valproate therapy in adults with epilepsy. Neurology. 2001;57(3):445–9.
Sheth RD, Wesolowski CA, Jacob JC, et al. Effect of carbamazepine and valproate on bone mineral density. J Pediatr. 1995;127(2):256–62.
Sheth RD, Binkley N, Hermann BP. Gender differences in bone mineral density in epilepsy. Epilepsia. 2008;49(1):125–31.
Samaniego EA, Sheth RD. Bone consequences of epilepsy and antiepileptic medications. Semin Pediatr Neurol. 2007;14(4):196–200.
Coppola G, Fortunato D, Auricchio G, et al. Bone mineral density in children, adolescents, and young adults with epilepsy. Epilepsia. 2009;50(9):2140–6.
Sheth RD, Binkley N, Hermann BP. Progressive bone deficit in epilepsy. Neurology. 2008;70(3):170–6.
Henderson RC, Lark RK, Gurka MJ, et al. Bone density and metabolism in children and adolescents with moderate to severe cerebral palsy. Pediatrics. 2002;110(1 Pt 1):e5.
Menon B, Harinarayan CV. The effect of anti epileptic drug therapy on serum 25-hydroxyvitamin D and parameters of calcium and bone metabolism–a longitudinal study. Seizure. 2010;19(3):153–8.
Rauchenzauner M, Griesmacher A, Tatarczyk T, et al. Chronic antiepileptic monotherapy, bone metabolism, and body composition in non-institutionalized children. Dev Med Child Neurol. 2010;52(3):283–8.
Nettekoven S, Ströhle A, Trunz B, et al. Effects of antiepileptic drug therapy on vitamin D status and biochemical markers of bone turnover in children with epilepsy. Eur J Pediatr. 2008;167(12):1369–77.
Szulc P, Delmas PD. Biochemical markers of bone turnover in osteoporosis. In: Rosen CJ, editor. Primer on the metabolic bone diseases and disorders of mineral metabolism. New York: Lippincott Williams & Williams; 2009. p. 174–9.
Pack AM, Morrell MJ, Randall A, McMahon DJ, Shane E. Bone health in young women with epilepsy after one year of antiepileptic drug monotherapy. Neurology. 2008;70(18):1586–93.
Sowers M, Crutchfield M, Bandekar R, et al. Bone mineral density and its change in pre- and perimenopausal white women: the Michigan Bone Health Study. J Miner Res. 1998;13(7):1134–40.
Ensrud KE, Walczak TS, Blackwell T, Ensrud ER, Bowman PJ, Stone KL. Antiepileptic drug use increases rates of bone loss in older women: a prospective study. Neurology. 2004;62(11):2051–7.
Verrotti A, Greco R, Morgese G, Chiarelli F. Increased bone turnover in epileptic patients treated with carbamazepine. Ann Neurol. 2000;47(3):385–8.
Verrotti A, Greco R, Latini G, Morgese G, Chiarelli F. Increased bone turnover in prepubertal, pubertal, and postpubertal patients receiving carbamazepine. Epilepsia. 2002;43(12):1488–92.
Kim SH, Lee JW, Choi KG, Chung HW, Lee HW. A 6-month longitudinal study of bone mineral density with antiepileptic drug monotherapy. Epilepsy and Behavior. 2007;10(2):291–5.
Mintzer S, Boppana P, Toguri J, et al. Vitamin D levels and bone turnover in epilepsy taking carbamazepine or oxcarbazepine. Epilepsia. 2006;47(3):510–5.
Cansu A, Yesilkaya E, Serdaroğlu A, et al. Evaluation of bone turnover in epileptic children using oxcarbazepine. Pediatr Neurol. 2008;39(4):266–71.
Gou CY, Ronen GM, Atkinson SA. Long-term valproate and lamotrigine treatment may be a marker for reduced growth and bone mass in children with epilepsy. Epilepsia. 2001;42(9):1141–7.
Verrotti A, Agostinelli S, Coppola G, Parisi P, Chiarelli F. A 12-month longitudinal study of calcium metabolism and bone turnover during valproate monotherapy. Eur J Neurol. 2010;17(2):232–7.
Ensrud KE, Walczak TS, Blackwell TL, et al. Antiepileptic drug use and rates of hip bone loss in older men: a prospective study. Neurology 2008, 71(10):723–30.
Sheth RD, Hermann BP. Bone mineral density with lamotrigine monotherapy for epilepsy. Pediatr Neurol. 2007;37(4):250–4.
Pierce Jr WM, Nardin GF, Fuqua MF, et al. Effect of chronic carbonic anhydrase inhibitor therapy on bone and mineral density in white women. J Bone Miner Res. 1991;6(4):347–54.
Nissen-Meyer LS, Svalheim S, Tauboll E, et al. Levetiracetam, phenytoin, and valproate act differently on rat bone mass, structure, and metabolism. Epilepsia. 2007;48(10):1–11.
Pascussi JM, Robert A, Nguyen M, et al. Possible involvement of pregnane X receptor-enhanced CYP 24 expression in drug-induced osteomalacia. J Clin Invest. 2005;115(1):177–86.
Zhou C, Assem M, Tay JC, et al. Steroid and xenobiotic receptor and vitamin D receptor crosstalk mediates CYP24 expression and drug-induced osteomalacia. J Clin Invest. 2006;116(6):1703–12.
Pack AM, Morrell MJ, Marcus R, et al. Bone mass and turnover in women with epilepsy on antiepileptic drug monotherapy. Ann Neurol. 2005;57(2):781–6.
Stephen LJ, McLellan AR, Harrison JH, et al. Bone density and antiepileptic drugs: a case-controlled study. Seizure. 1999;8(6):339–42.
Bhatt R, Bhatt S, Hameed M, Rameshwar P, Siegel A. Amygdaloid kindled seizures can induce functional and pathological changes in thymus of rat: role of the sympathetic nervous system. Neurobiol Dis. 2006;21(1):127–37.
Lambrinoudaki I, Kaparos G, Armeni E, et al. BsmI vitamin D receptor’s polymorphism and bone mineral density in men and premenopausal women on long-term antiepileptic therapy. Eur J Neurol 2011;18(1):93–8.
Pack AM. Genetic variation may clarify the relationship between epilepsy, antiepileptic drugs, and bone health. Eur J Neurol. 2011;18(1):3–4.
Thakkinstian A, D’Este C, Eisman J, Nguyen T, Attia J. Meta-analysis of molecular association studies: vitamin D receptor gene polymorphisms and BMD as a case study. J Bone Miner Res. 2004;19:419–28.
FRAX®: WHO risk factor tool. Available at: http://www.sheffield.ac.uk/FRAX/. Accessed April 8, 2011.
Mikati MA, Dib L, Yamout B, et al. Two randomized vitamin D trials in ambulatory patients on anticonvulsants: impact on bone. Neurology. 2006;67(11):2005–14.
IOM (Institute of Medicine). 2011. Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: The National Academies Press. Available at: http://www.iom.edu/vitamind. Accessed April 8, 2011.
Disclosure
No potential conflicts of interest relevant to this article were reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pack, A.M. Treatment of Epilepsy to Optimize Bone Health. Curr Treat Options Neurol 13, 346–354 (2011). https://doi.org/10.1007/s11940-011-0133-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11940-011-0133-x