Abstract
In the last decade, many authors reported single center experiences of “off-clamp”, “clamp-less”, or “unclamped” minimally invasive partial nephrectomy (MIPN). These procedures, despite the potential risk of increased intraoperative blood loss, attempted to minimize the loss of renal function by eliminating ischemic renal injury. “Zero ischemia” MIPN has emerged as new treatment option in 2011, initially performed under controlled hypotension, and later mainly by performing a “superselective microdissection”. The former technique minimizes the arterial bleeding from the renal stump, allowing surgeon to dissect the tumor in a bloodless field; the latter consists of identifying, antegradely from the renal hilum, the tertiary and quaternary arterial branches directly supplying the kidney neoplasm, and then selectively controlling them before dissecting the renal mass. This review critically analyzes these techniques, focusing on perioperative, oncologic and functional outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since radical nephrectomy (RN) has been proven to increase the risk of chronic kidney disease (CKD) and cardiovascular events, and thus to negatively affect overall survival of patients, minimally invasive partial nephrectomy (MIPN) has emerged as a possible standard of care for cT1 renal masses [1, 2].
Although initially performed for T1a renal tumors, several reports also addressed feasibility, safety and oncologic effectiveness of MIPN for T1b renal tumors [3, 4].
Despite the increasing evidence of warm ischemia time (WIT) as the only variable that the surgeon can significantly impact to minimize the loss of renal function after partial nephrectomy (PN), MIPN is today conventionally performed after clamping hilar vessels (artery only or artery and vein).
If hilar clamping during PN has the clear advantage of obtaining a bloodless field and consequently of performing an easy dissection of tumor, especially in case of mostly endophytic renal tumors, there is no consensus on the WIT threshold over which the ischemic injury definitively turns to a permanent and significant loss of renal function.
In 2010, Thompson et al. found 25 min to be the best WIT threshold to discriminate patients at risk of developing postoperative acute renal failure (ARF). However, in this report, the authors demonstrated WIT to also be a significant determinant of postoperative renal function loss as a continuous variable, finding each incremental minute of WIT to be associated with a 5 % and 6 % increased risk of ARF and IV stage CKD, respectively [5••].
In 2011, Gill et al. introduced “Zero-Ischemia” partial nephrectomy as a new technique to perform MIPN without clamping hilar vessels [6•].
In this review, we used the term “zero-ischemia” to define all non-ischemic PNs, referring to all PN techniques performed without clamping the hilar vessels.
Laparoscopic Background
In 2007, we first reported on a series of 50 patients treated with MIPN after preoperative superselective transarterial embolization for small and peripheral renal tumors. The angiographic procedure consisted of a superselective catheterization of secondary arterial renal branches followed, through a coaxial catheter, by delivery of polyvinyl alcohol compressible 500 to 700 μm microspheres (Terumo Bead Block Microspheres) into tertiary arterial branches feeding the tumor and some mm of healthy surrounding parenchyma. Once the complete devascularization of tumor was verified, a clamp-less MIPN was performed through a transperitoneal approach without isolating hilar vessels [7•].
Perioperative outcomes were encouraging, with a 4 % complication rate that compared favorably with the literature.
Later, in 2009 and 2011, we reported mid-term oncologic and functional outcomes of 210 patients treated with the same technique. Interestingly, after also expanding indications to renal tumors with moderate nephrometry score, perioperative outcomes were similar to those reported in the preliminary experience, with Clavien ≥ 3 complications occurring in eight patients (3.8 %), and two patients experiencing disease recurrence at a 46-month median follow-up and a median serum creatinine level increase of 0.24 mg/dL at 1-year follow-up. No patient experienced de novo CKD, defined as estimated glomerular filtration rate (e-GFR) < 60 mL/min, and (99 m)Tc diethylenetetramine pentacetic (DTPA) renal scintigraphy, performed preoperatively, 3-months and 1-year postoperatively; demonstrating a 5 % decrease of split renal function in the treated kidney at 1-year follow-up [8, 9].
In 2011, we reported perioperative, oncologic and functional outcomes of 101 consecutive patients treated with “zero ischemia sutureless laparoscopic partial nephrectomy for renal tumors with a low nephrometry score” [10].
Key steps of this technique were a simple enucleation or a minimal margin enucleoresection in most cases, a clamp-less approach without isolation of hilar vessels and a sutureless procedure, which was feasible in 96 % of cases. All these steps were aimed at guaranteeing the maximal preservation of healthy renal parenchyma surrounding the tumor.
This technique, performed in 101 highly selected patients with cT1a exophytic renal tumors, demonstrated to be feasible, safe and to provide excellent functional outcome, with no patient experiencing ARF, an 8.9 % complication rate (no Clavien ≥ 3 complications), a 1 % decrease of ispilateral renal function measured with 99mTc DTPA renal scintigraphy 1-yr postoperatively, and a recurrence rate <1 % [10].
Rais-Bahrami et al. retrospectively compared perioperative and functional outcomes of 126 and 264 patients who between 2006 and 2010 underwent off-clamp and hilar-clamp MIPN, respectively. Despite the acknowledged limitation of selection bias inherent to all retrospective analyses, complication rate of off-clamp group compared favorably with hilar-clamp group, and a significant improvement in terms of percent change in serum creatinine levels was reported in favor of off-clamp procedure (p = 0.04) [11].
Robotic Era
In 2011, Gill et al. first introduced a novel minimally invasive technique called “zero ischemia” partial nephrectomy in a series of 15 patients (12 performed laparoscopically and three robotically). After preparing hilar vessels, they performed PN without hilar clampig by using controlled hypotensive (CH) anesthesia during the deeper part of resection, or by performing a selective blunt microdissection of renal artery’s tertiary or quaternary branches. The CH was induced by inhalational isoflurane and nitroglycerin infusion to obtain a Mean Arterial Pressure (MAP) of 60 mmHg (median value 60, range 52–65) during the resection of the deep part of the tumor, while the reconstruction was completed with normal pressure. During CH anesthesia hemodynamic, cardiopulmonary, cerebral oxygenation and electroencephalographic parameters were measured to ensure safety perfusion of vital organs. In this preliminary experience, they demonstrated the feasibility of MIPN avoiding hilar clamping without increased complication rate (one Clavien grade 1, one Clavien grade 2 and one Clavien Grade 4a) and with insignificant eGFR modifications [6•].
In 2012, Papalia et al. confirmed feasibility and safety of “zero ischemia” MIPN in 60 consecutive cases. The only exclusion criterion was the unfitness for CH anesthesia due to an America Society of Anesthesiologists (ASA) score ≥ 3. Forty laparoscopic and 20 robotic MIPN were successfully performed, with negative margins in all cases and a 5 % complication rate (one Clavien grade 2, one Clavien grade 3A, one Clavien grade 3B). Median absolute and percent postoperative eGFR decrease was 11.6 mL/min and 13.3 %, respectively [12].
Later, the same group reported feasibility of “zero ischemia” MIPN in 121 consecutive patients fitting for CH anesthesia (ASA score < 3) comparing perioperative outcomes of patients divided into two group according to tumor diameter (≤ 4 cm versus > 4 cm). Overall and Clavien grade ≥ 3 perioperative complication rate were significantly higher in patients with tumor > 4 cm (18.6 % versus 6.4 % and 9.3 % versus 3.8 %, respectively). Preoperative and 3-month postoperative 99mTc-mercaptoacetyltriglycine renal scintigraphy demonstrated insignificant change in estimated renal plasma flow in the treated kidney in both groups [4].
In this paper, Papalia et al. highlighted the lack of data supporting the hypothesis that CH could be detrimental to vital organs. Induced hypotensive anaesthesia is a well-established blood-sparing technique in major surgery. Studies on the cerebral effects of hypotensive anaesthesia showed no significant differences in cognitive performance between the hypotensive and normotensive anaesthesia groups [13, 14].
The heart and the kidney are other organs that are believed to be commonly affected by hypotensive anaesthesia. Based on the best current evidence, deliberate hypotension stood the test of time and proved to cause no additional adverse effects on the cardiovascular system and renal perfusion [15].
The anatomic vascular microdissection (VMD) technique was described in a paper by Casey et al., comparing two series of MIPN performed with or without dissection of tumor specific tertiary or higher order renal arterial branches (Group 1 = 22 patients with VMD and Group 2 = 22 patients without VMD). Nevertheless, masses of group 1 were more complex (more medial, hilar, with lower C-index and higher RENAL score) while complication rate and 2-month postoperative median serum creatinine levels were comparable. Once confidence with superselective VMD was achieved satisfactorily, the authors no longer used CH anesthesia to perform MIPN [16].
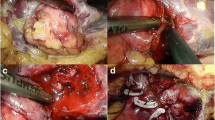
Figure 1 shows tertiary arterial branches feeding the renal tumor that were selectively identified during the enucleation, clip ligated and divided.
In order to improve and to extend anatomic MVD to most of the renal masses, 3D reconstruction of renovascular tumor anatomy was studied to facilitate “zero ischemia” MIPN. A prototype computer software was developed by Ukimura et al. to fuse three anatomical aspects: 3D surface rendered renal tumor, semitransparent kidney and 3D course of extrarenal and intrarenal arteries. Each patient underwent a preoperative 0.5-mm slice thickness computed tomography (CT) scan including arterial and venous phase. Intraoperative snapshots of 3D images from anterior, lateral, posterior and laparoscopic views and 3D video clips were created and presented to surgeon. In this report of four cases with completely intrarenal tumors, and thus not emerging from renal parenchyma, the authors experienced significant facilitated performance of zero ischemia, thanks to a precise identification and microdissection of the renal artery branches [17].
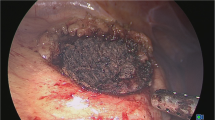
In a more recent series reported by Gill et al., 57 out of 58 patients underwent zero ischemia PN (15 robotic and 43 laparoscopic PN) performed with VMD using neurosurgical aneurysm microbulldog clamp. All margins were negative, and high-grade complication rate (Clavien Grade 3 to 5) was 3.5 %. Mean absolute and percent change in preoperative versus 4-month postoperative eGFR was 11.4 ml/min and 13 %, respectively. Mean percentage of renal function decrease was 10 % in 11 patients who underwent preoperative and six-month postoperative MAG3 renal scan [18]. Another useful tool to facilitate superselective arterial clamping is Near Infrared Fluorescence (NIRF) imaging, described by Borofsky et al. in a series of 34 patients undergoing Robotic PN. Out of 34 patients, in 29 cases, successful zero ischemia robotic PN was completed, while five patients underwent main renal artery clamping. Once the microsurgical bulldogs were applied on the tumor specific branches, 7.5 mg of indocyanine green (ICG) was administered intravenously. The robotic view was switched to NIRF to visualize the uptake. The tumor and the immediate peritumoral area remained dark circumferentially, while the surrounding parenchyma was fluorescent. This view confirmed the superselective tumor devascularization and the excision could be performed. Except for longer operative time for zero ischemia PN, perioperative outcomes were comparable between the zero ischemia and conventional hilar clamp MIPN groups. Short-term follow-up demonstrated a superior renal functional preservation documented by a percentage decrease of 1.8 % in e-GFR versus 14.9 % in the group of patients performed with conventional arterial clamping. Another advantage of this technique was the better visualization of tumor excision ensuring a negative margin, but further studies are needed to demonstrate this opportunity [19].
More recently, Krane et al. compared three different techniques in a series of robotic PN (artery only in 58 cases, artery and vein in 18 cases, unclamped in 19 cases).
Despite insignificant differences (p = 0.79) between groups in terms of percent change in e-GFR at last follow-up, the unclamped group showed the lower e-GFR decrease (2 %) compared to both clamped groups (6 %).
The authors concluded supporting minimal ischemia as a variable not adversely affecting postoperative renal function; however, when considering the small sample size and the low median WIT (< 20 min) in both clamped groups, the key message still remains a positive impact of unclamped PN on renal function recovery [20].
Laparo-Endoscopic Single Site (LESS) MIPN
Springer et al. reported a series of 14 unclamped LESS-PN under CH for highly selected cT1a exophytic and laterally based renal tumors. A single Clavien grade 1 perioperative complication occurred in one patient, all surgical margins were negative, no recurrences occurred at a 1-year median follow-up, and absolute preoperative and 6-month median e-GFR were not statistically different (106.5 mL/min versus 103.1 mL/min) [21].
In a multi-institutional outcome analysis of LESS PN, robotic platform proved to reduce the overall risk of postoperative complications (OR 20.92 [2.66–164.64] versus conventional LESS; p = 0.003) [22].
Ideal Partial Nephrectomy
According to European Association of Urology guidelines, PN should be the first treatment option for cT1 renal tumors. However, despite extensive evidence of feasibility of MIPN, open nephron sparing surgery remains the standard of care [23].
Notwithstanding, Sun et al. recently reported data collected in the surveillance, epidemiology and end results (SEER) database analyzing the trend in the management of 26468 cT1a renal tumors between 1988 and 2008. Although the rate of PN increased (4.7 % in 1988 to 40.4 % in 2008, p < 0.001) and RN trended lower over time (92.9 % in 1988 to 41.4 % in 2008, p < 0.001), RN still was the most performed treatment for cT1a renal tumors in United States [24].
Hung et al. recently introduced “trifecta” outcomes in PN as the combination of:
-
Negative cancer margin
-
Minimal renal functional decrease
-
No urological complications.
In a single surgeon series of 534 patients treated with MIPN between 1999 and 2011, the authors evaluated the outcomes described above in four chronologic eras (139 patients treated in the “discovery era” from September 1999 to December 2003, 213 patients treated in the “conventional hilar clamping era” from January 2004 to December 2006, 104 patients treated in the “early unclamping era” from January 2007 to November 2008, and 78 patients treated in the “anatomical zero-ischemia era” from March 2010 to October 2011).
Positive cancer margins were uniformly lower than 1 %.
Across the four eras, despite tumors trended toward larger size and increasing complexity, e-GFR decrease was > 15 % in 60 %, 68 %, 48 % and 18 % (p < 0.0001) and postoperative complication rate was 12 %, 5 %, 4 % and 5 % (p = 0.01) for “discovery”, “hilar clamping”, “early unclamping” and “zero-ischemia” eras, respectively [25].
All papers dealing with “zero-ischemia” MIPN proved to guarantee adequate cancer control, with complication rate comparable to that of conventional clamping PN, and to provide an optimal renal function preservation, as in terms of e-GFR and ipsilateral renal function decrease at renal scintigraphy [4, 5••, 6•, 7•, 10–12, 16–22, 25].
Perioperative data and functional outcomes of available series are summarized in Table 1.
Thus, looking at “trifecta” outcomes in PN, “zero-ischemia” MIPN demonstrated non-inferiority versus conventional PN in terms of cancer control and complication rate, and a possible superiority in terms of renal function preservation.
In a recent opposing views article, Campbell tried to “rewrite” a decade of Literature on WIT, highlighting the role of “quantity of preserved parenchyma” as the key variable not analyzed in the past, and thus considering WIT as a surrogate of this variable [26].
Despite a clear correlation between these two variables, awaiting evidence supporting this intriguing hypothesis, we would recommend caution when considering 25 min as a safe WIT threshold for PN.
Detractors of zero ischemia MIPN continue to raise the question about the real benefit of this procedure compared with conventional MIPN. Also, when considering that minimal ischemia (10–20 min) could not determine a significant ischemic injury and a consequent renal function loss in terms of e-GFR, the median WIT of most published MIPN series was > 20 min.
A recent experience from Texas University showed mean WIT raising from 29 min for tumors with low nephrometry score to 39 min for those with high score [27].
However, data about the ispilateral renal function loss in series of conventional MIPN are lacking. Therefore, the loss of renal function in the treated kidney could be underestimated when split renal function was not measured with renal scintigraphy [9].
In a large series of patients undergoing open or laparoscopic PN at a tertiary referral center, with hilar clamp performed in 94 % of cases, the new onset of V stage CKD was experienced by 2.2 % of patients (26/1164) [28].
Over the last decade, out of 439 patients underwent zero-ischemia LPN in our center, the incidence of III, IV and V stage CKD was 1.8 % and 0.2 %, and 0 %, respectively [4, 7•, 8–10, 12].
Finally, a publication bias should be considered with regard to the estimation of hilar vessels injury and of arterial intimal injuries when applying Satinsky clamp or bulldogs, especially at the beginning of learning curve.
All papers cited and discussed in this review were reported by tertiary referral centers, with skilled surgeons; thus, the impact of MIPN learning curve on feasibility and safety of “zero-ischemia” PN for complex renal tumors must be acknowledged [4, 5••, 6•, 7•, 8–12, 16–22, 25].
However, the intrinsic risks of MIPN mainly depend on nephrometry score and on surgeon skills, more than on clamping or unclamping PN approach; thus, the only recommendation should be to tailor the PN approach to these two variables.
Conclusion
“Zero-ischemia” MIPN proved to be a safe and effective technique to manage cT1 renal tumors regardless of their nephrometry score, and to provide comparable or higher trifecta outcomes than conventional MIPN.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Zini L, Perrotte P, Capitanio U, et al. Radical versus partial nephrectomy: Effect on overall and noncancer mortality. Cancer. 2009;115:1465–71.
Huang WC, Elkin EB, Levey AS, et al. Partial nephrectomy versus radical nephrectomy in patients with small renal tumors—is there a difference in mortality and cardiovascular outcomes? J Urol. 2009;181:55–62.
Simmons MN, Weight CJ, Gill IS. Laparoscopic radical versus partial nephrectomy for tumors >4 cm: intermediate-term oncologic and functional outcomes. Urology. 2009;73:1077–82.
Papalia R, Simone G, Ferriero M, et al. Laparoscopic and robotic partial nephrectomy without renal ischaemia for tumours larger than 4 cm: perioperative and functional outcomes. World J Urol. 2012;30:671–6.
•• Thompson RH, Lane BR, Lohse CM, et al. Every minute counts when the renal hilum is clamped during partial nephrectomy. Eur Urol. 2010;58:340–5. This article first demonstrated the detrimental effect of warm ischemia time during PN on renal function loss and proved WIT to be a continuous variable, with each incremental WIT minute, determining a 5 % and 6 % increased risks of ARF and IV stage CKD, respectively.
• Gill I, Eisenberg MS, Aron M, et al. “Zero Ischemia” partial nephrectomy: novel laparoscopic and robotic technique. Eur Urol. 2011;59:128–34. Gill et al. first introduced the term “Zero Ischemia” to the literature, describing a novel non-ischemic approach for MIPN.
• Gallucci M, Guaglianone S, Carpanese L, et al. Superselective Embolization as First Step of Laparoscopic Partial Nephrectomy. Urology. 2007;69:642–6. This article first reported a series of Zero Ischemia MIPN after superselective transarterial tumor embolization, highlighting feasibility and safety of the procedure.
Simone G, Papalia R, Guaglianone S, Forestiere E, Gallucci M. Preoperative superselective transarterial embolization in laparoscopic partial nephrectomy: technique, oncologic, and functional outcomes. J Endourol. 2009;23:1473–8.
Simone G, Papalia R, Guaglianone S, Carpanese L, Gallucci M. Zero ischemia laparoscopic partial nephrectomy after superselective transarterial tumor embolization for tumors with moderate nephrometry score: long-term results of a single-center experience. J Endourol. 2011;25:1443–6.
Simone G, Papalia R, Guaglianone S, Gallucci M. ‘Zero ischaemia’ sutureless laparoscopic partial nephrectomy for renal tumours with a low nephrometry score. BJU Int. 2011;110:124–30.
Rais-Bahrami S, George AK, Herati AS, Srinivasan AK, Richstone L, Kavoussi LR. Off-clamp versus complete hilar control laparoscopic partial nephrectomy: comparison by clinical stage. BJU Int. 2011;109:1376–81.
Papalia R, Simone G, Ferriero M, et al. Laparoscopic and Robotic Partial Nephrectomy With Controlled Hypotensive Anesthesia to Avoid Hilar Clamping: Feasibility, Safety and Perioperative Functional Outcomes. J Urol. 2012;187:1190–4.
Sartcaoglu F, Celiker V, Basgul E, et al. The effect of hypotensive anaesthesia on cognitive functions and recovery at endoscopic sinus surgery. Eur J Anaesthesiol. 2005;22:157–9.
Voldby B, Enevoldsen EM, Jensen FT, et al. Cerebrovascular reactivity in patients with ruptured intracranial aneurysms. J Neurosurg. 1985;62:59–67.
Choi WS, Samman N. Risks and benefits of deliberate hypotension in anaesthesia: a systematic review. Int J Oral Maxillofac Surg. 2008;37:687–703.
Ng CK, Gill IS, Patil MB, et al. Anatomic renal artery branch microdissection to facilitate zero-ischemia partial nephrectomy. Eur Urol. 2012;61:67–74.
Ukimura O, Nakamoto M, Gill I. Three-dimensional reconstruction of renovascular-tumor anatomy to faciltate zero-ischemia partial nephrectomy. Eur Urol. 2012;61:211–7.
Gill IS, Patil MB, de Castro Abreu AL, et al. Zero ischemia anatomical partial nephrectomy: a novel approach. J Urol. 2012;187:807–15.
Borofsky MS, Gill IS, Hemal AK et al. Near-infrared fluorescence imaging to facilitate super-selective arterial clamping during zero-ischaemia robotic partial nephrectomy. BJU Int. 2012 2013; 111: 604–10.
Krane LS, Mufarrij PW, Manny TB, Hemal AK. Comparison of clamping technique in robotic partial nephrectomy: does unclamped partial nephrectomy improve perioperative outcomes and renal function? Can J Urol. 2013;20:6662–7.
Springer C, Veneziano D, Wimpissinger F, Inferrera A, Fornara P, Greco F. Clampless laparoendoscopic single-site partial nephrectomy for renal cancer with low PADUA score: technique and surgical outcomes. BJU Int. 2013;111:1091–8.
Greco F, Autorino R, Rha KH et al. Laparoendoscopic Single-site Partial Nephrectomy: A Multi- institutional Outcome Analysis. doi:pii: S0302-2838(13)00094-8.10.1016/j.eururo.2013.01.025.
Ljungberg B, Cowan NC, Hanbury BC, et al. EAU guidelines on renal cell carcinoma: the 2010 update. Eur Urol. 2010;58:398–406.
Sun M, Abdollah F, Bianchi M, et al. Treatment management of small renal masses in the 21st century: a paradigm shift. Ann Surg Oncol. 2012;19:2380–7.
Hung AJ, Cai J, Simmons MN, Gill IS. “Trifecta” in partial nephrectomy. J Urol. 2013;189:36–42.
Aron M, Gill IS, Campbell SC. A nonischemic approach to partial nephrectomy is optimal. J Urol. 2012;187:387–90.
Liu ZW, Olweny EO, Yin G et al. Prediction of perioperative outcomes following minimally invasive partial nephrectomy: role of the R.E.N.A.L nephrometry score. World J Urol DOI 10.1007/s00345-012-0876-3.
Lane BR, Babineau DC, Poggio ED, et al. Factors Predicting Renal Functional Outcome After Partial Nephrectomy. J Urol. 2008;180:2363.
Compliance with Ethics Guidelines
Conflict of Interest
Dr. Giuseppe Simone, Dr. Mariaconsiglia Ferriero, Dr. Rocco Papalia, Dr. Manuela Costantini, Dr. Salvatore Guaglianone, and Dr. Michele Gallucci reported no potential conflicts of interest relevant to this article.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Simone, G., Ferriero, M., Papalia, R. et al. Zero-Ischemia Minimally Invasive Partial Nephrectomy. Curr Urol Rep 14, 465–470 (2013). https://doi.org/10.1007/s11934-013-0359-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11934-013-0359-0