Abstract
Reports in the literature of high recurrence rates after native tissue repair for pelvic organ prolapse led to the development of alternative techniques, such as those using synthetic mesh. Transvaginal mesh (TVM) delivery systems were implemented in search of better outcomes. Despite reported recurrence as low as 7.1 % after posterior colporrhaphy, mesh kits were developed to correct posterior compartment prolapse. There is a paucity of data to substantiate better results with TVM for rectocele repair. Three randomized controlled trials comparing native tissue repair to synthetic mesh reported posterior compartment outcomes and two of these failed to show a significant difference between groups. Complications of TVM placement are not insignificant and mesh extrusion was reported in up to 16.9 %. Based on currently available data, native tissue repairs have similar outcomes to synthetic mesh without the risks inherent in mesh use and remain the standard of care for the typical patient.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pelvic organ prolapse is common in postmenopausal women and the lifetime risk of undergoing surgical intervention for prolapse or incontinence has been reported at 11.1 to 19 % [1, 2]. In one study, approximately 200,000 women underwent surgical correction of pelvic organ prolapse in the United States over a 1-year period [3]. In this population, 22.6 % underwent anterior and posterior colporrhaphy and 10.5 % underwent posterior colporrhaphy alone [3].
It is interesting to note that the reoperation rate after prolapse surgery has been reported to be 30 % [1]. To reduce recurrence of prolapse after surgical repair, alternative techniques have been developed, including the use of grafts to augment native tissue. In the past decade, the use of synthetic mesh has become more common, and this review aims to address both the benefits and risks of using synthetic mesh to correct posterior compartment prolapse.
Rationale for the Development of Synthetic Mesh Repair
Reported recurrence rates after traditional native tissue repair in the literature are high and the development of TVM repair was fueled by dissatisfaction with results of traditional repair. Recurrent anterior prolapse after anterior colporrhaphy occurs in 43 % to 70 % of patients [4, 5]. Novel techniques such as graft-augmented repairs were designed to improve outcomes. Allografts, xenografts, and synthetic materials all have been utilized in attempts to reduce recurrence rates in prolapse surgery. In 2001, the first TVM delivery system was approved by the U. S. Food and Drug Administration (FDA) [6]. Since that time, multiple “kits” for the correction of pelvic prolapse have passed the 510(k) process and are available on the market. These systems have been developed to treat anterior and posterior compartment prolapse, vaginal vault prolapse, and combinations thereof. Postmarket surveillance studies from manufacturers have been lacking and knowledge of published outcomes data is important for those treating women with pelvic organ prolapse.
Outcomes of Native Tissue Repair
Traditional native tissue repair of the posterior compartment includes midline plication of the fibromuscular fascial layer or site-specific defect repair. Reported outcomes of these techniques are acceptable and with low complication rates. Maher et al. [7] demonstrated high anatomic and subjective success in correction of symptomatic rectoceles with midline plication. The success rate, of course, depends on the definition of anatomic failure. Defining anatomic cure as pelvic organ prolapse quantification (POPQ) stage I or less, the objective success was 87 % at 12 months and 79 % at 24 months. Subjective success was measured using a visual analog scale and found to be 97 % at 12 months and 89 % at 24 months. In this series, 87 % had resolution of obstructed defecation [7].
Paraiso et al. [8] compared traditional midline plication, site-specific defect repair, and repair augmented with a biologic graft. Anatomic cure was defined as having a POPQ Bp point less than or equal to −2 [8]. At 1 year, the anatomic success rate in the posterior colporrhaphy group was 86 % compared to 78 % in the site-specific group. These rates were significantly better than those who underwent biologic graft repair, demonstrating anatomic success in only 54 % [8]. When the definition of success was changed to prolapse at or beyond the hymenal remnant, 20 % of patients in the graft-augmented group failed treatment at 1 year compared to 7.1 % of the posterior colporrhaphy group [8]. Reoperation for posterior compartment prolapse following posterior colporrhaphy is low, reported at 3 % [7, 8].
The second definition of success used in the Paraiso et al. [8] study highlights the dilemma in reporting outcomes after pelvic organ prolapse repair. Studies have shown that up to 62 % of women presenting for routine gynecologic screening will have stage 0 or I prolapse and 35 % will have stage II prolapse [9]. Many women with stage II prolapse will be asymptomatic and symptoms are more likely when the leading edge of prolapse extends beyond the level of the hymenal remnant [10]. The failure rates cited in the literature for native tissue repair, particularly for anterior colporrhaphy, have been criticized as unacceptable and continued development of alternative techniques thrived. The definition of anatomic failure in initial studies, however, has been questioned. One large series on anterior colporrhaphy often cited in the literature was recently revisited and failure redefined as prolapse beyond the hymen, the presence of symptoms, or the need for retreatment [5, 11]. When this definition was applied, success improved from 30 % to 88 % [11]. Once this composite definition is applied, success rates improve and are more clinically relevant [12].
Objective Outcomes of Transvaginal Synthetic Mesh for Correction of Rectocele
There is a paucity of randomized controlled trials (RCT) comparing TVM repair to traditional native tissue repair, and an even greater disparity in those that address the posterior compartment. There are three RCTs that address posterior prolapse; one study uses a surgeon-tailored mesh and two compare traditional repair to a TVM kit [13, 14••, 15••]. Although these studies address outcomes in the posterior compartment, detailed results regarding posterior compartment recurrence after treatment in that compartment are not presented in all. A comparison of outcomes from these three trials can be found in Table 1.
In a randomized study of 139 women with POPQ stage II or greater prolapse, traditional midline plication was compared to type I polypropylene mesh repair [13]. Patients in this study underwent both anterior and posterior compartment repair [13]. Posterior mesh repair was accomplished using a Y-shaped piece overlying the fascia with the two arms abutting the sacrospinous ligaments. Anatomic success at 1 year was 81 % in the mesh group compared to 65.6 % in the colporrhaphy group. Success was defined as POPQ stage I or less and this difference did not reach statistical significance. Outcome did not change after including patients lost to follow-up as either success or failure [13]. Although there is mention that most failures occurred in the anterior compartment, the failures were not broken down by compartment. Thus, a direct comparison between nonmesh repair and mesh repair for posterior prolapse is not known.
In a multicenter double-blinded RCT, traditional repair was compared to mesh repair with Prolift (Ethicon, Inc., Somerville, NJ) in patients with POPQ stage II or greater [14••]. Anatomic success, defined as POPQ stage I or less, was the primary outcome and the secondary outcome was success in each compartment. The study was halted after the predetermined cut-off for mesh extrusion was reached, and at that time, 32 patients underwent mesh surgery and 33 had traditional repair. The overall recurrence was 62.5 % in the mesh group and 69.7 % in those without mesh after a median follow-up of 12 months. This difference was not statistically significant. Compartment specific recurrences were not statistically different between the mesh and no mesh groups. In changing the definition of failure to prolapse beyond the hymenal remnant, the recurrence rate dropped to 25 % in the mesh group compared to 21.7 % in the no mesh group. Interestingly, the three patients who underwent a repeat operation for prolapse were in the mesh group, but this finding was not statistically significant [14••]. These results again highlight the dilemma of defining success.
Specific outcomes in the posterior compartment are available in the study by Sokol et al. [14••]. In the entire mesh group, posterior recurrence was 21.9 % compared to 18.2 % in the no mesh group, and this difference was not significant. The study reports that no association was identified between the site of mesh placement and the site of recurrence [14••]. In the eight Total Prolifts implanted, there were six recurrences and two of these occurred in the posterior compartment [14••, 16]. Extrapolating this data yields a 25 % anatomic recurrence in the posterior compartment following mesh repair in that compartment. These results are not better than reported outcomes for posterior colporrhaphy [8, 11].
A third RCT had a larger number of patients with posterior mesh placement and randomly assigned women with POPQ stage II or greater prolapse to conventional vaginal repair or repair with tension-free vaginal mesh [15••]. The study results were limited because it was not blinded and simultaneous sacrospinous ligament fixation or a modified Manchester-Fothergill procedure was permitted in the mesh group. Failure in the treated compartment was identified in 45.2 % after conventional repair compared to 9.6 % in the tension-free vaginal mesh group after 12 months [15••]. This difference remained significant even when the patients lost to follow-up were considered failures. Mesh was placed in the posterior compartment in 56 patients and 51 of these had stage II or greater posterior prolapse before surgery. Only two posterior recurrences were identified in the 49 patients available for follow up. This 4.1 % posterior recurrence after posterior mesh repair was significantly better than the 24.5 % recurrence after traditional repair [15••].
A concern of improving support in one compartment is the development or worsening of prolapse in the untreated compartments. In a secondary analysis of the study by Withagen et al. [17••], the occurrence of de novo prolapse in the untreated compartment was much greater in the mesh group than the conventional group, 47 % compared to 17 %. After posterior repair using mesh, 53 % had de novo prolapse in the untreated compartment compared to 17 % after posterior colporrhaphy. This difference was statistically significant [17••]. These results highlight the importance of recognizing the consequences of isolated compartment repair and shed light on the risks associated with synthetic mesh augmentation in the posterior compartment. This is only one risk of using synthetics and other complications will be discussed.
Data from these three RCTs can be supplemented and compared to retrospective reviews. One series looked at 2-year outcomes of transvaginal rectocele repair with surgeon-tailored mesh in 26 consecutive patients at the time of sacrospinous ligament fixation [18]. There was only one patient with stage II posterior recurrence [18]. Another retrospective review of 120 patients 1 year following Avaulta transvaginal mesh (CR Bard, Murray Hill, NJ) demonstrated an 81 % overall cure rate using a composite definition [6]. The cure rate for the 21 patients that received only posterior mesh was 90 % [6]. A 10.2 % overall recurrence of stage II or greater POP was identified 12 months following Prolift in 100 patients [19]. The study notes that the recurrence was in the untreated compartment when an anterior Prolift was used. For patients that underwent posterior Prolift, all recurrences were in the posterior compartment and the rate was 9.1 % [19].
As the level of concern for mesh-based complications increases, partially absorbable mesh kits have been implemented. A retrospective series of 127 patients following Prolift + M (Ethicon, Inc.) reported 77.4 % overall anatomic success in the treated compartment at 1 year [20]. Success increased to 89.5 % when failure was defined as the leading edge beyond the hymenal remnant [20]. Unfortunately, the failures were not reported by compartment, and thus, the number of posterior recurrences following posterior mesh is not known from the published data [20]. A series with shorter follow-up was published by Khandwala et al. [21], reporting 74.1 % success based on a composite definition. The published data list one stage II recurrence in the posterior mesh group (n = 42) and one in the total vaginal mesh group (n = 118), but it is not explicitly stated whether these were posterior recurrences in the treated compartment.
Subjective Outcomes of Transvaginal Synthetic Mesh for Rectocele
In the three published RCTs addressing outcomes in the posterior compartment, measured improvement in quality of life (QOL) and subjective overall improvement were analyzed as secondary outcomes. Carey et al. [13] noted an improvement in patient-reported scores on the Prolapse Symptom Inventory and Quality of Life questionnaire (PSI-QOL), Short-form Urogenital Distress inventory (UDI), Short-form Incontinence Impact questionnaire (IIQ), the Cleveland Clinic Continence score, and a visual analog scale in both the mesh and no mesh group. However, there was no statistically significant difference between groups. In the study by Sokol et al. [14••], similar QOL outcomes were measured with the Short Form Health Survey, short forms of Pelvic Floor Distress Inventory (PDFI), UDI, and Pelvic Floor Impact Questionnaire demonstrating a statistically significant improvement from baseline in both groups, but no statistically significant difference between groups. Withagen et al. [15••] reported that not all domains of the QOL measurements (PGII, UDI, IIQ) demonstrated significant improvement after surgical repair and there was no statistically significant difference between the mesh and conventional group in any measure.
Complications Associated with Transvaginal Synthetic Mesh
Although traditional native tissue repairs are not without complication, there has been increased concern recently about suspected higher rates of adverse outcomes associated with the use of TVM. Complications related to mesh can be broken down into perioperative or intraoperative and postoperative or delayed. Immediate complications include inadvertent visceral puncture or perforation, extensive bleeding, need for blood product transfusion, hematomas, and infection. Delayed complications include extrusion of mesh, mesh retraction, pelvic pain, sexual side effects, and voiding symptoms.
In the three RCTs discussed previously, most complications were related to total vaginal mesh or to anterior compartment repair with mesh. Mention of these complications remains pertinent to this review because patients often undergo correction of multiple compartments, and as such, would either have total vaginal mesh placed or a combination of anterior and posterior mesh. Regarding visceral perforations, in two of the RCTs, there were two bladder perforations in each of the total vaginal mesh groups compared to none in the traditional repair groups [14••, 15••]. In the retrospective series, the bladder perforation rate ranges from 0.7 % to 2.3 % [20, 22••]. Rectal perforations have been reported, usually with either no events or one event, leading to rates as low as 0.2 % [22••]. Postoperative hematomas were more common in the mesh group, 6 % versus 1 %, in the RCT published by Withagen et al. [15••]. Most other series reported a lower rate of postoperative hematomas [19, 22••]. Postoperative urinary retention was reported to be more common in the TVM group in the study by Withagen et al. [15••], but there were also a greater number of synthetic midurethral slings in this group. The impact of concomitant midurethral sling in higher rate of retention was not independently assessed.
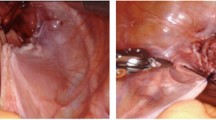
A significant risk with placement of TVM is extrusion, defined as a prosthetic’s passage gradually out of a body structure or tissue [23]. In the three RCTs that included posterior compartment outcomes, overall mesh extrusion ranged from 5.6 % to 16.9 % [13, 14••, 15••]. Withagen et al. [15••] identified 14 patients with mesh extrusion (16.9 %) that were equally distributed between the anterior and posterior compartments. Five required surgical excision and nine were treated with topical estrogen, but only two resolved by the last follow-up in the study. Five mesh extrusions (15.6 %) occurred in the study by Sokol et al. [14••] and two of these were in the posterior compartment. Surgical intervention was required in three patients. Of the four cases of mesh extrusion in the RCT with surgeon-tailored mesh, one was located posteriorly [13].
Complications related to mesh extrusion were equally prevalent in retrospective studies. The rate of mesh extrusion in the retrospective series mentioned earlier range from 2 % to 11.7 % [6, 19–21]. When the locations were reported, the extrusion usually occurred anteriorly or at the apex. In the series reported by Milani et al. [20], the overall mesh extrusion was 10.2 % and one posterior wall extrusion was identified after 11 Total Prolift + M. Larger retrospective series from the early work of the TVM group reported extrusion in up to 11.3 % [24]. Only 6.7 % required surgical treatment. Excluding those with simultaneous vaginal hysterectomy, the overall extrusion rate drops to 4.7 % and extrusion on the posterior wall was 2.1 % [24]. In a large 3-year retrospective series of 524 patients after Prolift, 3.6 % of patients required surgical intervention for mesh-related complications [22••]. Mesh extrusion occurred in 2.7 % and there were eight surgical interventions for extrusion of mesh on the posterior vaginal wall.
Patients with prolapse may experience sexual symptoms and dyspareunia that has been shown to resolve following corrective surgery. However, there are patients who will continue to have pain and those that will develop de novo dyspareunia following surgical repair. There was no significant reduction in dyspareunia after repair in the series by Carey et al. [13]. No differences were identified between the mesh and no mesh groups and there were no differences in the rates of de novo dyspareunia between groups. Withagen et al. [15••] demonstrated that the rate of dyspareunia decreased in both the mesh and no mesh groups after correction of prolapse, and de novo dyspareunia occurred in 8 % and 10 %, respectively. These differences were not statistically significant. De novo dyspareunia occurred in 9.1 % of patients in the TVM group in the study by Sokol et al. [14••], and this was not significantly different from those without mesh. Looking at the retrospective series previously discussed, the rate of de novo dyspareunia ranged from 2 % to 11.1 % after TVM [19–21].
Retraction or contraction of implanted vaginal mesh leads to changes in vaginal caliber or length and may be symptomatic. In the three RCTs that discuss outcomes of the posterior compartment, only one mentions data on mesh retraction [14••]. In that series, postoperative vaginal diameter, vaginal volume, and total vaginal length were all statistically significantly lower than preoperative values. The differences between the mesh and no mesh groups, however, were not different. In larger retrospective series on TVM delivery systems, the risk of symptomatic or severe mesh retraction is reported between 0.4 % and 11.7 % [19, 22••, 24]. In the posterior compartment alone, it has been reported in up to 5 % [24].
Conclusions
In assessing the need to augment rectocele repair with synthetic mesh, one must balance the risk of complications with the supposed benefit of improved outcomes. In light of the recent uproar regarding concerns for complications following transvaginal synthetic mesh in prolapse repair, one would hope that there is clear and convincing evidence for using synthetic mesh in rectocele repair. Unfortunately, the available data do not convincingly support the hypothesis that the outcomes are superior, and, additionally, there are the potential complications inherent to synthetic mesh use.
The adequacy of native tissue repair has been substantiated using newer definitions that are less strict than previous definitions set by the 2001 National Institutes of Health (NIH) Workshop on Standardization of Terminology for Researchers in Pelvic Floor Disorders [12]. Cure rates using composite definitions approach 90 % or better and the reoperation rate after posterior colporrhaphy is only 3 % [7, 8]. One then has to justify a mesh complication rate as high as 16.9 % even if posterior recurrence is as low as 4.1 to 9.1 % after mesh repair [17••, 19].
Paramount to answering the question about mesh use in the posterior compartment is knowledge from randomized controlled trials. There is paucity of such data. Most available studies do not discuss the rate of posterior recurrences following rectocele repair with mesh. The overall recurrence rate is presented, and the rate of posterior prolapse may be listed, but de novo occurrences are not always delineated from recurrence in a treated posterior compartment. This data is not entirely clear or available in the three RCTs or the retrospective series considered in this review. Assuming that the posterior prolapse after either posterior or total vaginal mesh in the RCTs by Sokol et al. [14••] and Withagen et al. [15••] are all recurrences in the treated compartment and not de novo occurrences, the true rate is as low as 4.1 % to 9.1 %.
Due to increased concern over mesh extrusion and complications with TVM delivery systems, the FDA released a safety communication to practitioners in 2008 and utilized the medical device adverse event reporting database, MAUDE, to gather additional information on such occurrences [25]. An update was released in July 2011 detailing an analysis of the reporting database that identified 2,874 additional mesh-related complications over a 3-year period and stressed that serious complications from TVM used to treat prolapse are not rare [25]. Although the true denominator remains largely unknown, concern remains that the rate of mesh complication is higher than expected. In response to this report, the number of lawsuits against the device manufacturers has skyrocketed, reported as high as 650 in a recent article in Bloomberg News [26]. The FDA has reclassified such devices and is calling for postmarket studies. With such changes in the forefront, perhaps there will be better data on the safety and efficacy of synthetic mesh based rectocele repairs in the near future.
Based on currently available data, however, it appears that for the typical patient with posterior wall prolapse, native tissue repairs have outcomes similar to synthetic mesh repairs without the risks inherent in mesh use. Given the data discussed in this article, until proven otherwise, native tissue repair for rectocele remains the standard of care with good outcomes and relatively low morbidity. Further studies may elucidate specific populations for whom posterior mesh augmented repair outcomes are superior to native tissue repair. Until that data is available, posterior repairs with native tissue remains the gold standard for the typical patient.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Olsen AL, Smith VJ, Bergstrom JO, et al. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997;89(4):501–6.
Smith FJ, Holman CD, Moorin RE, et al. Lifetime risk of undergoing surgery for pelvic organ prolapse. Obstet Gynecol. 2010;116(5):1096–100.
Shah AD, Kohli N, Rajan SS, et al. The age distribution, rates, and types of surgery for pelvic organ prolapse in the USA. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(3):421–8.
Sand PK, Koduri S, Lobel RW, et al. Prospective randomized trial of polyglactin 910 mesh to prevent recurrence of cystoceles and rectoceles. Am J Obstet Gynecol. 2001;184(7):1357–62. discussion 1362–4.
Weber AM, Walters MD, Piedmonte MR, et al. Anterior colporrhaphy: a randomized trial of three surgical techniques. Am J Obstet Gynecol. 2001;185(6):1299–304. discussion 1304–6.
Culligan PJ, Littman PM, Salamon CG, et al. Evaluation of a transvaginal mesh delivery system for the correction of pelvic organ prolapse: subjective and objective findings at least 1 year after surgery. Am J Obstet Gynecol. 2010;203(5):506.e1–6.
Maher CF, Qatawneh AM, Baessler K, et al. Midline rectovaginal fascial plication for repair of rectocele and obstructed defecation. Obstet Gynecol. 2004;104(4):685–9.
Paraiso MF, Barber MD, Muir TW, et al. Rectocele repair: a randomized trial of three surgical techniques including graft augmentation. Am J Obstet Gynecol. 2006;195(6):1762–71.
Swift S, Woodman P, O'Boyle A, et al. Pelvic Organ Support Study (POSST): the distribution, clinical definition, and epidemiologic condition of pelvic organ support defects. Am J Obstet Gynecol. 2005;192(3):795–806.
Swift SE, Tate SB, Nicholas J. Correlation of symptoms with degree of pelvic organ support in a general population of women: what is pelvic organ prolapse? Am J Obstet Gynecol. 2003;189(2):372–7. discussion 377–9.
Chmielewski L, Walters MD, Weber AM, et al. Reanalysis of a randomized trial of 3 techniques of anterior colporrhaphy using clinically relevant definitions of success. Am J Obstet Gynecol. 2011;205(1):69.e1–8.
Barber MD, Brubaker L, Nygaard I, et al. Defining success after surgery for pelvic organ prolapse. Obstet Gynecol. 2009;114(3):600–9.
Carey M, Higgs P, Goh J, et al. Vaginal repair with mesh versus colporrhaphy for prolapse: a randomised controlled trial. BJOG. 2009;116(10):1380–6.
•• Sokol AI, Iglesia CB, Kudish BI, et al. One-year objective and functional outcomes of a randomized clinical trial of vaginal mesh for prolapse. Am J Obstet Gynecol. 2012;206(1):86.e1–9. This RCT provides information on prolapse recurrence in the posterior compartment after correction with mesh compared to no mesh.
•• Withagen MI, Milani AL, den Boon J, et al. Trocar-guided mesh compared with conventional vaginal repair in recurrent prolapse: a randomized controlled trial. Obstet Gynecol. 2011;117(2 Pt 1):242–50. This RCT provides information on prolapse recurrence in the posterior compartment after correction with mesh compared to no mesh.
Iglesia CB, Sokol AI, Sokol ER, et al. Vaginal mesh for prolapse: a randomized controlled trial. Obstet Gynecol. 2010;116(2 Pt 1):293–303.
•• Withagen M, Milani A, de Leeuw J, et al. Development of de novo prolapse in untreated vaginal compartments after prolapse repair with and without mesh: a secondary analysis of a randomised controlled trial. BJOG. 2012;119(3):354–60. This article highlights the potential increased risk of de novo prolapse in the untreated compartment after mesh repair.
de Tayrac R, Picone O, Chauveaud-Lambling A, et al. A 2-year anatomical and functional assessment of transvaginal rectocele repair using a polypropylene mesh. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17(2):100–5.
Simon M, Debodinance P. Vaginal prolapse repair using the Prolift kit: a registry of 100 successive cases. Eur J Obstet Gynecol Reprod Biol. 2011;158(1):104–9.
Milani AL, Hinoul P, Gauld JM, et al. Trocar-guided mesh repair of vaginal prolapse using partially absorbable mesh: 1 year outcomes. Am J Obstet Gynecol. 2011;204(1):74.e1–8.
Khandwala S, Jayachandran C. Transvaginal mesh surgery for pelvic organ prolapse–Prolift + M: a prospective clinical trial. Int Urogynecol J. 2011;22(11):1405–11.
•• de Landsheere L, Ismail S, Lucot JP, et al. Surgical intervention after transvaginal Prolift mesh repair: retrospective single-center study including 524 patients with 3 years’ median follow-up. Am J Obstet Gynecol. 2012;206(1):83.e1–7. This retrospective review discusses surgical intervention after mesh in a large cohort after long follow-up.
Haylen BT, Freeman RM, Swift SE, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint terminology and classification of the complications related directly to the insertion of prostheses (meshes, implants, tapes) and grafts in female pelvic floor surgery. Neurourol Urodyn. 2011;30(1):2–12.
Caquant F, Collinet P, Debodinance P, et al. Safety of trans vaginal mesh procedure: retrospective study of 684 patients. J Obstet Gynaecol Res. 2008;34(4):449–56.
Food and Drug Administration: FDA Safety Communication: UPDATE on Serious Complications Associated with Transvaginal Placement of Surgical Mesh for Pelvic Organ Prolapse. Available at http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm262435.htm. Released July 13, 2011. Accessed February 2012.
Nussbaum A, Voreacos D.: J&J, C.R. Bard Must Study Safety of Vaginal Mesh, FDA Says. Bloomberg News. January 5, 2012. Available at http://www.bloomberg.com/news/2012-01-04/fda-orders-safety-studies-for-vaginal-implants-made-by-j-j-and-c-r-bard.html. Accessed February 2012.
Disclosures
Dr. Brian Marks has received travel expense compensation from Ferring Pharmaceuticals. Dr. Howard Goldman has received payment for the development of educational presentations from Ethicon, Inc.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Marks, B.K., Goldman, H.B. What is the Gold Standard for Posterior Vaginal Wall Prolapse Repair: Mesh or Native Tissue?. Curr Urol Rep 13, 216–221 (2012). https://doi.org/10.1007/s11934-012-0248-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11934-012-0248-y