Abstract
Pelvic organ prolapse (POP) is a generalized term that refers to prolapse of any of the three vaginal compartments: anterior (cystocele), posterior (rectocele), and apical (uterine and vault prolapse). POP may affect up to 50% of parous women, and as a result, one in nine women will undergo at least one surgery for POP in her lifetime. Native tissue repair is the cornerstone of prolapse surgery, especially in light of the scrutiny placed on the use of mesh for prolapse. Refinements in the procedures over time have been based on both basic anatomy and fundamentals of surgery, as well as the ongoing acquisition of new knowledge through clinical studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pelvic organ prolapse is defined as the loss of support for the pelvic organs leading to prolapse of one or more of these organs into the vagina [1]. Specific types of POP are classified according to the herniating organ: cystocele, or anterior compartment prolapse, is descent of the bladder into the vagina; rectocele, or posterior compartment prolapse, is herniation of the rectum into the posterior vagina; vault prolapse, or apical prolapse, occurs when the apex of the vagina descends into the lower vagina. Vault prolapse is often associated with an enterocele, which is a herniation of the small bowel into the vagina. The term vault prolapse implies that the uterus is absent, as opposed to the term uterine prolapse when the uterus is still present.
Pelvic organ prolapse (POP) is a condition that affects up to 50% of women. Not only does it cause significant psychological distress and negatively affect quality of life, but it also places a tremendous financial burden on the healthcare system. Between 2005 and 2006, the treatment of POP cost the US healthcare system upwards of $300 million dollars [2]. This number will continue to rise as the prevalence of POP increases with the growing elderly female population. Contemporary reports estimate the prevalence of POP to be between 3 and 6% [3].
Parity is one of the main risk factors for development of POP, with the risk of POP increasing with increasing parity. Mant et al. concluded that compared to nulliparous women, primiparous women had a fourfold increased risk of hospital admission for POP, and this risk increased with each subsequent vaginal delivery [4]. Furthermore, vaginal delivery is associated with an increased risk of POP compared to Cesarean section. Larsson and colleagues examined this correlation and concluded that of women with POP, 92.9% had vaginal deliveries while 1.9% delivered by Cesarean section [5]. Among Cesarean section patients, Lukacz et al. found a statistically significant increase in POP rates in women who were in labor prior to Cesarean section versus those who underwent elective Cesarean section without trial of labor [6]. Other risk factors for POP include increasing age, prior pelvic surgery, chronic constipation, and obesity [5, 7, 8].
The majority of surgical procedures for POP are performed with the patient’s own tissue; however, recurrence rates after native tissue repair have been reported up to 29% [9]. As such, surgeons began to augment native tissue repairs with biologic grafts and synthetic mesh. Although synthetic mesh can improve anatomic outcomes, mesh-related complications prompted the Food and Drug Administration to issue safety communications regarding its use [10,11,12].
Considering the current prevalence of POP and the future expected increase, combined with the controversy regarding the use of mesh for POP surgery, it is of vital importance that the clinician be familiar with native tissue repairs for POP.
Cystocele
The first description of the etiology of cystocele development is attributed to Dr. George White. In 1909, he described that cystocele is the result of the lateral detachment of the pubocervical fascia from the arcus tendineus fascia pelvis (white line) [13]. Dr. White also described a vaginal paravaginal repair for this defect, but likely due to its surgical difficulty, the Kelly plication was popularized despite its intended indication for stress incontinence and high rate of failure [14].
Anatomy
Prolapse of the anterior vaginal compartment can occur either because of connective tissue defects in the vaginal wall itself (central defect) or failure of the lateral attachments (lateral defect). Although White originally described lateral detachment causing cystocele, Richardson expanded this explanation to include three additional areas of deficiency: the pubocervical fascia, the pubourethral ligament, and the anterior vaginal wall itself [15].
Traditionally the term “fascia” has been used when referring to connective tissue of the vagina; however, there is no true fascial layer of the vaginal wall. Instead, the vagina is comprised of an epithelium, a fibromuscular layer, and an adventitia [16]. The tissue that is plicated during colporrhaphy is the muscularis and adventitial layers [16,17,18].
Surgical Outcomes
Historically, cystocele repair has been associated with suboptimal outcomes. When success of cystocele repair is measured only by anatomic outcomes, the rate of success is low (30%). On the contrary, when symptoms are also considered, then 1-year success rates are significantly higher at 89% [19]. Lavelle and colleagues demonstrated that success rates can be sustained long term (greater than 5 years) using a modified vaginal paravaginal repair technique [20•]. Success rates can be improved even more if a concomitant apical procedure is performed, such as uterosacral or sacrospinous ligament suspension. When an apical procedure is performed in conjunction with cystocele repair, the recurrence rate decreases almost 50% at 10 years [21••].
Anterior Colporrhaphy
As mentioned previously, anterior colporrhaphy refers to plication of the muscularis and adventitial layers of the vaginal wall. A Kelly plication refers to placement of additional sutures at the urethra and bladder neck to also treat incontinence [14]. Anterior colporrhaphy, with or without Kelly plication, is straightforward and relatively unchanged from its initial description over a century ago. Anterior colporrhaphy alone has reported success of only 30% when limited to the use of native tissue, but suture type and placement may improve success rates. Both absorbable suture with slower absorption and permanent suture can decrease recurrence rates, and Song et al. reported 98% success at 4 years when anterior colporrhaphy was reinforced with three additional purse-string sutures [22,23,24]. Success rates can also be improved up to 5 years if the term “native tissue” is expanded to include the use of autologous fascia as described by Cormio [25].
Paravaginal Repair
The majority of anterior compartment prolapse cases are associated with lateral defects [15]. As such, an argument could be made that a paravaginal repair for cystocele is a superior operation. During a paravaginal repair, the perivesical tissue is reattached to the arcus tendineus (white line) with multiple sutures.
Transabdominal paravaginal cystocele repair, both open and laparoscopic, is the most widely reported approach for a paravaginal repair. The surgery is relatively unchanged from Richardson’s initial description of the procedure in 1976. Traditionally, the procedure was performed through a Pfannenstiel incision, but a laparoscopic approach is currently favored as it provides better visualization and shorter recovery. A series of synthetic, nonabsorbable sutures are placed to reapproximate the perivesical fascia to the white line. Placement of the surgeon’s fingers in the vagina can aid in placement of the sutures during the procedure. Success rates of laparoscopic and open transabdominal paravaginal repair range from 60 to 93% [26, 27].
The amount of data regarding vaginal paravaginal repair is small compared to the open approach, and long-term data is limited. Furthermore, native tissue vaginal paravaginal repair lacks the visualization afforded by the abdominal approach and thus has more potential for complications. Mallipeddi et al. reported 2-year outcomes following vaginal paravaginal repair in 45 women with 3% cystocele recurrence; however, length of hospital stay was 2.6 ± 1.1 days, one patient had bilateral ureteral obstruction, one patient required reoperation for hematoma, and two patients received transfusions [28]. Young et al. reported 1-year outcomes for 100 consecutive women undergoing vaginal paravaginal repair. Twenty-two patients had cystocele recurrence between 3 and 11 months after surgery, and 21 major and 14 minor inpatient complications occurred [29]. A prospective study by Hosni and colleagues comparing vaginal, open, and laparoscopic approaches to paravaginal repair found similar effectiveness between all groups [30].
Rectocele
Prolapse of the posterior compartment of the vagina may be the result of enterocele, sigmoidocele, rectocele, or a combination thereof; however, rectocele generally refers to prolapse of the anterior rectum into the posterior vaginal wall. Richardson was the first to classify defects in the rectovaginal fascia [31]. His initial description classified rectoceles into low (visible just inside the hymen due to attenuation of the perineal body), mid-vaginal (loss of support from the lateral attachments of the arcus tendineus fascia rectovaginalis), and high (result of weakening of the cardinal and uterosacral ligament complex).
Anatomy
The upper third of the posterior vaginal wall is supported by the cardinal-uterosacral ligament complex, the middle third by the arcus tendineus fascia, and the lower third fuses with the perineal body. The levator ani, primarily the puborectalis, plays an important role in supporting the posterior vaginal wall. These attachments maintain the vagina and rectum in a horizontal orientation, rather than a vertical position, through the levator hiatus [32].
Damage to the connective tissue and musculature of the pelvic floor and/or neurologic damage, commonly related to childbirth, predisposes to rectocele. This is compounded by increased rectal pressure with defecation that places strain on the fibromuscular layer of the posterior vaginal wall and results in formation of a rectocele [15].
Transvaginal Rectocele Repair
Transvaginal rectocele repair is by far the most common surgical approach. After the posterior vaginal epithelium is dissected off the rectovaginal fascia, midline plication of the fascia is typically performed with interrupted sutures starting at the proximal posterior vagina. Care must be taken not to narrow the vaginal canal during plication as this could cause dyspareunia. De novo dyspareunia after native tissue rectocele repair has been reported as high as 33%, and dyspareunia rates are also higher when levatorplasty, as opposed to plication of the rectovaginal fascia alone, is performed [33]. On the contrary, Maher and colleagues reported on 38 women who had a statistically significant reduction in dyspareunia following rectocele repair with midline fascial plication for symptomatic rectoceles [34]. Although relatively uncommon, inadvertent rectal injury can occur during rectocele repair. Hence, it is advised to perform a rectal exam when plication is complete when there is concern for rectal injury.
Mellgren et al. evaluated 25 patients who underwent transvaginal rectocele repair and found a 96% anatomic cure rate at 12 months. In addition, constipation was noted to be improved in 88% of patients. The most common side effect was de novo dyspareunia in 8% of patients [35••].
Site-Specific Rectocele Repair
In addition to classifying types of rectocele, Richardson also popularized the site-specific rectocele repair as an alternative to the traditional midline plication in an effort to minimize complications [31]. The goal of this procedure is to restore vaginal anatomy by closing discrete defects in the rectovaginal fascia as opposed to plicating the entire area. Isolated defects are usually identified with the surgeon’s examining finger and repaired.
Current evidence is conflicting as to whether site-specific rectocele repair has a lower incidence of dyspareunia, but most reports indicate that success rates are not equivalent compared to a traditional repair. Porter et al. retrospectively examined outcomes for site-specific rectocele repair and noted that patients who underwent this procedure had statistically significant improvement in defecatory dysfunction, pelvic pain, and dyspareunia [36]. In another retrospective study, Abramov et al. reported that subjective and objective rectocele recurrence rates were significantly increased with a site-specific repair compared to traditional posterior colporrhaphy, and there was no statistically significant difference in postoperative dyspareunia rates between the two groups [37].
Transrectal Rectocele Repair
In 1968, Sullivan and colleagues first described the transrectal approach to rectocele repair based on the belief that by dissecting through the rectum, rather than the vagina, postoperative dyspareunia is minimized. Colorectal surgeons generally perform transrectal (transanal) repairs, while gynecologists and urologists prefer the transvaginal approach. Although dyspareunia is avoided by the transrectal approach, recurrence rates are uniformly reported as higher for this approach. Roman et al. retrospectively analyzed long-term (30–128-month follow-up) outcomes of transanal rectocele repair and discovered a 50% recurrence rate [38]. In a prospective study comparing transanal to transvaginal approach to rectocele repair, Nieminen et al. found that after 12 months, the recurrence rate was significantly higher for the transrectal group (7 vs. 40%, p = 0.04), but there was no de novo dyspareunia reported in either group [39].
Insight as to why site-specific and transrectal repairs have higher recurrence rates compared to the traditional approach may be found in a recent study by Haylen et al. that describes the main anatomic defects in posterior vaginal compartment prolapse [40]. Interestingly, they determined that the great majority of anatomic defects are at the vaginal vault and introitus, with only a small number of defects at the mid-vagina. Neither a site-specific or transanal repair simultaneously addresses defects at the vaginal vault and introitus to the same degree that a traditional rectocele repair would.
Role of Perineorrhaphy
Perineorrhaphy is a commonly performed procedure, often in conjunction with other prolapse procedures, yet there is a paucity of data regarding indications and outcomes. Kanter and colleagues surveyed attendees of the 2014 Society for Genitourinary Surgeons annual meeting to determine why and how they decided to perform perineorrhaphy [41]. Most surgeons (60%) reapproximated the bulbocavernosus and transverse perineii muscles together, while 30% each reapproximated the bulbocavernosus or transverse perineii muscles individually. In this study, the most common reason perineorrhaphy was performed was for an enlarged genital hiatus. Other reasons included patient request and cosmesis.
On the issue of cosmesis, so-called vaginal rejuvenation is a term commonly used to describe reconstruction of the vaginal canal and introitus including labiaplasty and perineorrhaphy. Beyond cosmesis, there is a lack of sufficient data regarding improvement of sexual satisfaction or self-image and the term vaginal rejuvenation should be considered a marketing term only [42, 43].
Vault Prolapse
The International Continence Society defines vaginal vault prolapse as descent of the vaginal cuff past a point that is 2 cm less than the total vaginal length [44]. Vault prolapse is very commonly associated with apical enterocele as it mainly occurs after hysterectomy, and there is often associated high cystocele and rectocele as well [45].
The annual incidence of vaginal vault prolapse has been reported between 900 and 1200 women [46]. Furthermore, 18.2% of women with any type of POP are found to have vault prolapse. Another method of estimating the incidence of vault prolapse is to determine the number of surgeries performed for the condition. Aigmueller et al. calculated the frequency of vault prolapse that required surgical intervention to be between 6 and 8% in Austria [47].
Anatomy
The main structural support of the vaginal apex is provided by the cardinal-uterosacral ligament complex. The insertion of these ligaments to the cervix, or vaginal cuff following hysterectomy, is at the level of the ischial spines. Vault prolapse occurs when the cardinal-uterosacral ligament complex detaches from the vaginal cuff at the level of the ischial spines [45]. Enterocele results when concomitant disruption in the endopelvic fascia permits protrusion of peritoneum through the fascial defect. The enterocele sac extends into the rectovaginal space at the site of separation between the pubocervical and rectovaginal fascia [48].
Uterosacral Ligament Suspension
Uterosacral ligament suspension (USLS) is arguably the most common native tissue procedure performed to address vault prolapse. Traditionally, USLS has involved entry into the peritoneal cavity to facilitate identification of the uterosacral ligaments; however, an extraperitoneal method has been described [49]. Sutures are placed bilaterally through the uterosacral ligaments at the level of the ischial spine and include the lateral pubocervical and rectovaginal fascia. In doing so, tying down these sutures elevates and anchors the vaginal cuff to the uterosacral ligaments [50, 51]. This technique simultaneously addresses any enterocele defect.
By virtue of the procedure, there is considerable risk of ureteral injury with vaginal USLS. Contemporary reports comparing laparoscopic and vaginal approaches to USLS suggest that both procedures have comparable clinical outcomes with similar rates of complications except for a lower rate of ureteral injury when the procedure is performed laparoscopically [52, 53]. Regardless of what surgical approach is used, intraoperative cystoscopy is vital to identify ureteral compromise.
Sacrospinous Ligament Suspension
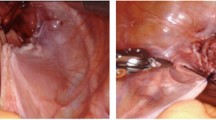
Sacrospinous ligament suspension (SSLS) is another common transvaginal approach for apical prolapse. This procedure was popularized when transvaginal mesh-based kits were introduced. Both anterior and posterior approaches to the sacrospinous ligament have been described. Sutures are carefully placed through the sacrospinous ligament medial to the ischial spine to avoid the pudendal neurovascular bundle. The use of a suture device can facilitate placement of sutures into the sacrospinous ligament [54]. The vaginal muscularis is then secured to the sacrospinous ligament. Consideration may be given to securing the suspension suture unilaterally on the right side given the position of the sigmoid and rectum on the left side [55]. As expected, complications of this procedure include hemorrhage and gluteal pain, which are generally self-limited, and bladder or rectal injury.
The OPTIMAL Trial is a multicenter, randomized, prospective study comparing USLS with SSLS for the treatment of apical prolapse. The primary outcome measures were both anatomic and subjective, with an emphasis on postoperative bothersome bulge. Results of the trial demonstrated no difference between the treatment arms with comparable surgical success rates: USLS 64.5% and SSLS 63.1%. The rate of serious adverse events with USLS and SSLS was less than 5% over a 24-month follow-up. All incidents of ureteral obstruction occurred in the USLS arm (3.7%) [56•].
Iliococcygeus Fascia Fixation
Possibly in an effort to avoid injury to the pudendal neurovascular bundle, vault suspension by iliococcygeal fixation was described by Sze and Karram [57]. This procedure involves suturing the vaginal apex to the iliococcygeal fascia below the ischial spine. Contemporary reports indicate cure rates up to 89% at a median follow-up of 68.8 months [58]. Furthermore, relief of subjective symptoms was similar when iliococcygeus fixation was compared to abdominal sacral colpopexy [59].
Autologous Fascia Abdominal Sacrocolpopexy
It is generally accepted that the most durable procedure for vault prolapse is an abdominal sacral colpopexy (ASC) as it has the lowest recurrence rate compared to vaginal procedures [60]. The disadvantages of ASC include longer operative time, longer postoperative convalescence, and increased cost.
Traditionally, ASC has been performed with synthetic graft material, but in response to concerns with synthetic mesh, there has been an increased interest in the use of autologous fascia including rectus fascia and fascia lata [61, 62]. Advantages of autologous fascia over synthetic mesh include decreased risk of infection and erosion. In a randomized controlled trial comparing synthetic mesh and cadaveric fascia lata, synthetic mesh was superior in regard to anatomic failure rate (9% mesh vs. 32% fascia lata); however, there was a 3.7% risk of erosion in the synthetic mesh arm [63]. Long-term follow-up in the CARE trial demonstrated a mesh erosion rate of 10.5% at 7 years [64]. As of preparation of this manuscript, there have been no reported episodes of extrusion with autologous fascia for ASC [61].
In a small case series, Maloney et al. demonstrated a 90% cure rate of vault prolapse using rectus fascia for ASC [65]. Tate and colleagues performed a randomized trial of fascia lata and mesh for ASC with 5-year follow-up [66]. Although mesh had superior anatomic outcomes, clinical success rates were comparable between mesh and fascia.
Inherently, it would be advantageous to harvest a rectus fascia graft and perform the colpopexy through the same abdominal incision. When a fascia lata graft is used, then consideration should be given to a laparoscopic approach. The graft is sutured to the anterior and posterior vagina then fixed to the anterior longitudinal ligament near the sacral promontory. The promontory itself is to be avoided as this is usually the location of the disc, and discitis is a known potential complication of ASC [67, 68].
Uterine Prolapse
Uterine-Sparing Procedures
Uterosacral Plication
The uterosacral ligaments are the main support of the cervix and upper vagina. In addition, they are responsible for maintaining vaginal length and orientation. Loss of support from these ligaments results in prolapse of the vaginal apex, including the uterus. In patients with uterine prolapse, uterosacral plication is an option when a woman desires uterine preservation. Uterosacral plication can be performed either transvaginally or abdominally. In a recent meta-analysis, Margulies and colleagues concluded that 98.3% of women had successful anatomic outcomes after transvaginal uterosacral ligament plication, having defined success as POP-Q stage 0 or 1. Given the numerous studies that comprised this meta-analysis, only POP-Q scoring was reported and subjective patient outcomes were not included. Ureteral obstruction was reported at 1.8% due to narrow suturing in the pelvis via the transvaginal approach. In addition, given, the abundant vascular supply in the pelvis, excessive bleeding requiring transfusion occurred in 1.3% of patients. As with other vaginal reconstructive procedures, the need for intraoperative cystoscopy to ensure ureteral patency is of paramount importance [69].
Manchester Procedure
The Manchester procedure is a uterine-sparing procedure that achieves prolapse repair by amputation of the cervix and suturing to the cardinal ligaments [70]. Although the technique is not commonly performed, it remains an effective uterine-sparing alternative for patients. A recent meta-analysis by Tolstrup and colleagues evaluated prolapse recurrence rates after the Manchester procedure and vaginal hysterectomy. Not only were recurrence rates higher for the vaginal hysterectomy group, but this group also had higher reoperation rates. Furthermore, vaginal hysterectomy patients had higher operative blood loss and inadvertent bladder injury. [71].
Colpocleisis
For women who are not ideal surgical candidates and/or vaginal penetration is not essential for sexual activity, colpocleisis is viable treatment option. Colpocleisis is considered an obliterative, as opposed to reconstructive, procedure. When there is no uterus or cervix colpectomy is performed, and when a uterus is present, then Le Fort (partial) colpocleisis is performed. The latter allows passage of discharge from the cervix. The basic premise is to remove the anterior and posterior vaginal epithelium and sequentially suture the anterior and posterior vaginal walls together until the prolapse is reduced.
Glavind and Kempf reported on a series of 42 elderly patients who had either colpectomy or colpocleisis. No severe complications occurred, and at 3 months, there were no recurrences [71]. Follow-up telephone interviews at a mean of 46 months after surgery revealed 90% of patients were satisfied with the operation. Krissi et al. reported on their series of 47 women aged 61 to 91 years who underwent Le Fort colpocleisis [72]. At a mean follow-up of 14.8 months, the objective and subjective cure rates were 80.9 and 91.5%, respectively. Recurrence was associated with longer postoperative vaginal length and larger genital hiatus. Extrapolation of this data suggests that it may be beneficial to perform perineorrhaphy at the time of colpocleisis.
Hysterectomy
Hysterectomy continues to play a major role in the treatment of POP. A common belief is that if the uterus is not removed, then there is a significantly increased risk of postoperative prolapse; however, not all current data overwhelmingly supports this belief. Dietz et al. compared transvaginal sacrospinous hysteropexy to vaginal hysterectomy with uterosacral suspension of the vaginal vault and found a statistically significant increase in the recurrence rates among women who underwent hysteropexy rather than hysterectomy (27 vs. 3%) [73]. When Carramão et al. compared similar groups, although they found a similar increase in prolapse recurrence in the hysteropexy group, they did not find a statistically significant difference [74]. The main consideration when hysterectomy is contemplated is associated morbidity.
Conclusions
Pelvic organ prolapse is a condition that affects a large percent of the female population. As life expectancy continues to increase, the prevalence of POP will also continue to rise. Some native tissue repairs may be associated with higher rates of prolapse recurrence compared to synthetic mesh repairs; however, POP surgery with synthetic mesh has higher postoperative complication rates [75]. In addition, with the ongoing controversy surrounding the use of synthetic mesh for POP, it is important for the clinician to be familiar with a variety of native tissue repairs.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Wein AJ, Kavoussi LR, Campbell MF, Walsh PC. Campbell-Walsh urology. 10th ed.
Sung VW, Washington B, Raker CA. Costs of ambulatory care related to female pelvic floor disorders in the United States. Am J Obstet Gynecol. 2010;202(5):483 e1–4. doi:10.1016/j.ajog.2010.01.015.
Barber MD, Maher C. Epidemiology and outcome assessment of pelvic organ prolapse. Int Urogynecol J. 2013;24(11):1783–90. doi:10.1007/s00192-013-2169-9.
Mant J, Painter R, Vessey M. Epidemiology of genital prolapse: observations from the Oxford family planning association study. Br J Obstet Gynaecol. 1997;104(5):579–85.
Larsson C, Kallen K, Andolf E. Cesarean section and risk of pelvic organ prolapse: a nested case-control study. Am J Obstet Gynecol. 2009;200(3):243 e1–4. doi:10.1016/j.ajog.2008.11.028.
Lukacz ES, Lawrence JM, Contreras R, Nager CW, Luber KM. Parity, mode of delivery, and pelvic floor disorders. Obstet Gynecol. 2006;107(6):1253–60. doi:10.1097/01.AOG.0000218096.54169.34.
Swift S, Woodman P, O'Boyle A, Kahn M, Valley M, Bland D, et al. Pelvic organ support study (POSST): the distribution, clinical definition, and epidemiologic condition of pelvic organ support defects. Am J Obstet Gynecol. 2005;192(3):795–806. doi:10.1016/j.ajog.2004.10.602.
Kudish BI, Iglesia CB, Sokol RJ, Cochrane B, Richter HE, Larson J, et al. Effect of weight change on natural history of pelvic organ prolapse. Obstet Gynecol. 2009;113(1):81–8. doi:10.1097/AOG.0b013e318190a0dd.
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997;89(4):501–6. doi:10.1016/S0029-7844(97)00058-6.
Nguyen JN, Burchette RJ. Outcome after anterior vaginal prolapse repair: a randomized controlled trial. Obstet Gynecol. 2008;111(4):891–8. doi:10.1097/AOG.0b013e31816a2489.
FDA Public Health Notification. Serious complications associated with transvaginal placement of surgical mesh in repair of pelvic organ prolapse and stress urinary incontinence. 2008. http://www.fda.gov/cdrh/safety/102008-surgicalmesh.html.
FDA Safety Communication. UPDATE on serious complications associated with transvaginal placement of surgical mesh for pelvic organ prolapse. 2011.
White GR. Cystocele--a radical cure by suturing lateral sulci of the vagina to the white line of pelvic fascia. 1909. Int Urogynecol J Pelvic Floor Dysfunct. 1997;8(5):288–92.
Kelly HA, Dumm WM. Urinary incontinence in women, without manifest injury to the bladder. 1914. Int Urogynecol J Pelvic Floor Dysfunct. 1998;9(3):158–64.
Richardson AC, Lyon JB, Williams NL. A new look at pelvic relaxation. Am J Obstet Gynecol. 1976;126(5):568–73.
Weber AM, Walters MD. Anterior vaginal prolapse: review of anatomy and techniques of surgical repair. Obstet Gynecol. 1997;89(2):311–8. doi:10.1016/S0029-7844(96)00322-5.
Delancey JO. Fascial and muscular abnormalities in women with urethral hypermobility and anterior vaginal wall prolapse. Am J Obstet Gynecol. 2002;187(1):93–8.
Hsu Y, DeLancey J. Functional anatomy and pathophysiology of pelvic organ prolapse. In Female Urology; 2008. p. 542–555.
Weber AM, Walters MD, Piedmonte MR, Ballard LA. Anterior colporrhaphy: a randomized trial of three surgical techniques. Am J Obstet Gynecol. 2001;185(6):1299–304. discussion 304-6 doi:10.1067/mob.2001.119081.
• Lavelle RS, Christie AL, Alhalabi F, Zimmern PE. Risk of prolapse recurrence after native tissue anterior vaginal suspension procedure with intermediate to long-term Followup. J Urol. 2016;195(4P1):1014–20. doi:10.1016/j.juro.2015.10.138. Established that modifited vaginal paravaginal repair can lead to significantly improved cystocele repair outcomes.
•• Eilber KS, Alperin M, Khan A, Wu N, Pashos CL, Clemens JQ, et al. Outcomes of vaginal prolapse surgery among female Medicare beneficiaries: the role of apical support. Obstet Gynecol. 2013;122(5):981–7. doi:10.1097/AOG.0b013e3182a8a5e4. Published further data supporting the utility to apical repair with cystocele repair to further decrease cystocele recurrence rates.
Zebede S, Smith AL, Lefevre R, Aguilar VC, Davila GW. Reattachment of the endopelvic fascia to the apex during anterior colporrhaphy: does the type of suture matter? Int Urogynecol J. 2013;24(1):141–5. doi:10.1007/s00192-012-1862-4.
Bergman I, Soderberg MW, Kjaeldgaard A, Ek M. Does the choice of suture material matter in anterior and posterior colporrhaphy? Int Urogynecol J. 2016;27(9):1357–65. doi:10.1007/s00192-016-2981-0.
Song HS, Choo GY, Jin LH, Yoon SM, Lee T. Transvaginal cystocele repair by purse-string technique reinforced with three simple sutures: surgical technique and results. International neurourology journal. 2012;16(3):144–8. doi:10.5213/inj.2012.16.3.144.
Cormio L, Mancini V, Liuzzi G, Lucarelli G, Carrieri G. Cystocele repair by autologous rectus fascia graft: the Pubovaginal cystocele sling. J Urol. 2015;194(3):721–7. doi:10.1016/j.juro.2015.03.104.
Chinthakanan O, Miklos JR, Moore RD. Laparoscopic paravaginal defect repair: surgical technique and a literature review. Surgical technology international. 2015;27:173–83.
Demirci F, Ozdemir I, Somunkiran A, Gul OK, Gul B, Doyran GD. Abdominal paravaginal defect repair in the treatment of paravaginal defect and urodynamic stress incontinence. Journal of obstetrics and gynaecology : the journal of the Institute of Obstetrics and Gynaecology. 2007;27(6):601–4. doi:10.1080/01443610701497603.
Mallipeddi P, Kohli N, Steele AC, Owens RG, Karram MM. Vaginal paravaginal repair in the surgical treatment of anterior vaginal wall prolapse. Primary care update for Ob/Gyns. 1998;5(4):199–200.
Young SB, Daman JJ, Bony LG. Vaginal paravaginal repair: one-year outcomes. Am J Obstet Gynecol. 2001;185(6):1360–6. discussion 6-7 doi:10.1067/mob.2001.119073.
Hosni MM, El-Feky AE, Agur WI, Khater EM. Evaluation of three different surgical approaches in repairing paravaginal support defects: a comparative trial. Arch Gynecol Obstet. 2013;288(6):1341–8. doi:10.1007/s00404-013-2927-4.
Richardson AC. The rectovaginal septum revisited: its relationship to rectocele and its importance in rectocele repair. Clin Obstet Gynecol. 1993;36(4):976–83.
Nichols DH. Posterior colporrhaphy and perineorrhaphy: separate and distinct operations. Am J Obstet Gynecol. 1991;164(3):714–21.
Madsen LD, Nussler E, Kesmodel US, Greisen S, Bek KM, Glavind-Kristensen M. Native-tissue repair of isolated primary rectocele compared with nonabsorbable mesh: patient-reported outcomes. Int Urogynecol J. 2016; doi:10.1007/s00192-016-3072-y.
Maher CF, Qatawneh AM, Baessler K, Schluter PJ. Midline rectovaginal fascial plication for repair of rectocele and obstructed defecation. Obstet Gynecol. 2004;104(4):685–9. doi:10.1097/01.AOG.0000139833.48063.03.
•• Mellgren A, Anzen B, Nilsson BY, Johansson C, Dolk A, Gillgren P, et al. Results of rectocele repair. A prospective study. Dis Colon rectum. 1995;38(1):7–13. Established the utlity and efficacy of transvaginal rectocele repair, excellent short and long term efficacy rates.
Porter WE, Steele A, Walsh P, Kohli N, Karram MM. The anatomic and functional outcomes of defect-specific rectocele repairs. Am J Obstet Gynecol. 1999;181(6):1353–8. discussion 8-9
Abramov Y, Gandhi S, Goldberg RP, Botros SM, Kwon C, Sand PK. Site-specific rectocele repair compared with standard posterior colporrhaphy. Obstet Gynecol. 2005;105(2):314–8. doi:10.1097/01.AOG.0000151990.08019.30.
Roman H, Michot F. Long-term outcomes of transanal rectocele repair. Dis Colon rectum. 2005;48(3):510–7.
Nieminen K, Hiltunen KM, Laitinen J, Oksala J, Heinonen PK. Transanal or vaginal approach to rectocele repair: a prospective, randomized pilot study. Dis Colon rectum. 2004;47(10):1636–42.
Haylen BT, Naidoo S, Kerr SJ, Yong CH, Birrell W. Posterior vaginal compartment repairs: where are the main anatomical defects? Int Urogynecol J. 2016;27(5):741–5. doi:10.1007/s00192-015-2874-7.
Kanter G, Jeppson PC, McGuire BL, Rogers RG. Perineorrhaphy: commonly performed yet poorly understood. A survey of surgeons. Int Urogynecol J. 2015;26(12):1797–801. doi:10.1007/s00192-015-2762-1.
Shaw D, Lefebvre G, Bouchard C, Shapiro J, Blake J, Allen L, et al. Female genital cosmetic surgery. Journal of obstetrics and gynaecology Canada: JOGC = Journal d'obstetrique et gynecologie du Canada: JOGC. 2013;35(12):1108–14.
Committee on Gynecologic Practice ACoO, Gynecologists. ACOG Committee opinion no. 378: vaginal “rejuvenation” and cosmetic vaginal procedures. Obstet Gynecol. 2007;110(3):737–8. doi:10.1097/01.AOG.0000263927.82639.9b.
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the standardisation sub-committee of the international continence society. Neurourol Urodyn. 2002;21(2):167–78.
Uzoma A, Farag KA. Vaginal vault prolapse. Obstet Gynecol Int. 2009;2009:275621. doi:10.1155/2009/275621.
Winters JC, Cespedes RD, Vanlangendonck R. Abdominal sacral colpopexy and abdominal enterocele repair in the management of vaginal vault prolapse. Urology. 2000;56(6 Suppl 1):55–63.
Aigmueller T, Dungl A, Hinterholzer S, Geiss I, Riss P. An estimation of the frequency of surgery for posthysterectomy vault prolapse. Int Urogynecol J. 2010;21(3):299–302. doi:10.1007/s00192-009-1033-4.
Paraiso MF, Falcone T, Walters MD. Laparoscopic surgery for enterocele, vaginal apex prolapse and rectocele. Int Urogynecol J Pelvic Floor Dysfunct. 1999;10(4):223–9.
Ow LL, Walsh CE, Rajamaheswari N, Dwyer PL. Technique of extraperitoneal uterosacral ligament suspension for apical suspension. Int Urogynecol J. 2016;27(4):637–9. doi:10.1007/s00192-015-2873-8.
Karram M, Goldwasser S, Kleeman S, Steele A, Vassallo B, Walsh P. High uterosacral vaginal vault suspension with fascial reconstruction for vaginal repair of enterocele and vaginal vault prolapse. Am J Obstet Gynecol. 2001;185(6):1339–42. discussion 42-3 doi:10.1067/mob.2001.119077.
Shull BL, Bachofen C, Coates KW, Kuehl TJ. A transvaginal approach to repair of apical and other associated sites of pelvic organ prolapse with uterosacral ligaments. Am J Obstet Gynecol. 2000;183(6):1365–73. discussion 73-4 doi:10.1067/mob.2000.110910.
Turner LC, Lavelle ES, Shepherd JP. Comparison of complications and prolapse recurrence between laparoscopic and vaginal uterosacral ligament suspension for the treatment of vaginal prolapse. Int Urogynecol J. 2016;27(5):797–803. doi:10.1007/s00192-015-2897-0.
Barbier HM, Smith MZ, Eto CU, Welgoss JA, Von Pechmann W, Horbach N, et al. Ureteral compromise in laparoscopic versus vaginal uterosacral ligament suspension: a retrospective cohort. Female pelvic medicine & reconstructive surgery. 2015;21(6):363–8. doi:10.1097/SPV.0000000000000202.
Vaudano G, Gatti M. Correction of vaginal vault prolapse using Capio suture capturing device: our experience. Minerva Ginecol. 2015;67(2):103–11.
Karram M, Walters MD. Surgical treatment of vaginal vault prolapse and enterocele. Urogynecology and Reconstructive Pelvic Surgery, 3rd ed. Philadelphia: Mosby Elsevier; 2007. p. 271.
• Barber MD, Brubaker L, Burgio KL, Richter HE, Nygaard I, Weidner AC, et al. Comparison of 2 transvaginal surgical approaches and perioperative behavioral therapy for apical vaginal prolapse: the OPTIMAL randomized trial. JAMA. 2014;311(10):1023–34. doi:10.1001/jama.2014.1719. Concluded that no difference exists in either efficacy or complication rates between USLS and SSLS.
Sze EH, Karram MM. Transvaginal repair of vault prolapse: a review. Obstet Gynecol. 1997;89(3):466–75. doi:10.1016/S0029-7844(96)00337-7.
Serati M, Braga A, Bogani G, Leone Roberti Maggiore U, Sorice P, Ghezzi F, et al. Iliococcygeus fixation for the treatment of apical vaginal prolapse: efficacy and safety at 5 years of follow-up. Int Urogynecol J. 2015;26(7):1007–12. doi:10.1007/s00192-015-2629-5.
Milani R, Cesana MC, Spelzini F, Sicuri M, Manodoro S, Fruscio R. Iliococcygeus fixation or abdominal sacral colpopexy for the treatment of vaginal vault prolapse: a retrospective cohort study. Int Urogynecol J. 2014;25(2):279–84. doi:10.1007/s00192-013-2216-6.
Maher C, Feiner B, Baessler K, Schmid C. Surgical management of pelvic organ prolapse in women. The Cochrane database of systematic reviews. 2013;4:CD004014. doi:10.1002/14651858.CD004014.pub5.
Abraham N, Quirouet A, Goldman HB. Transabdominal sacrocolpopexy with autologous rectus fascia graft. Int Urogynecol J. 2016;27(8):1273–5. doi:10.1007/s00192-016-2987-7.
Latini JM, Brown JA, Kreder KJ. Abdominal sacral colpopexy using autologous fascia lata. J Urol. 2004;171(3):1176–9. doi:10.1097/01.ju.0000103925.56765.bc.
Culligan PJ, Blackwell L, Goldsmith LJ, Graham CA, Rogers A, Heit MH. A randomized controlled trial comparing fascia lata and synthetic mesh for sacral colpopexy. Obstet Gynecol. 2005;106(1):29–37. doi:10.1097/01.AOG.0000165824.62167.c1.
Nygaard I, Brubaker L, Zyczynski HM, Cundiff G, Richter H, Gantz M, et al. Long-term outcomes following abdominal sacrocolpopexy for pelvic organ prolapse. JAMA. 2013;309(19):2016–24. doi:10.1001/jama.2013.4919.
Maloney JC, Dunton CJ, Smith K. Repair of vaginal vault prolapse with abdominal sacropexy. The Journal of reproductive medicine. 1990;35(1):6–10.
Tate SB, Blackwell L, Lorenz DJ, Steptoe MM, Culligan PJ. Randomized trial of fascia lata and polypropylene mesh for abdominal sacrocolpopexy: 5-year follow-up. Int Urogynecol J. 2011;22(2):137–43. doi:10.1007/s00192-010-1249-3.
Api M, Kayatas S, Boza A. Spondylodiscitis following sacral colpopexy procedure: is it an infection or graft rejection? Eur J Obstet Gynecol Reprod Biol. 2015;194:43–8. doi:10.1016/j.ejogrb.2015.08.003.
Feng TS, Thum DJ, Anger JT, Eilber KS. Sacral osteomyelitis after robotic sacrocolpopexy. Female pelvic medicine & reconstructive surgery. 2016;22(1):e6–7. doi:10.1097/SPV.0000000000000219.
Margulies RU, Rogers MA, Morgan DM. Outcomes of transvaginal uterosacral ligament suspension: systematic review and metaanalysis. Am J Obstet Gynecol. 2010;202(2):124–34. doi:10.1016/j.ajog.2009.07.052.
Gutman R, Maher C. Uterine-preserving POP surgery. Int Urogynecol J. 2013;24(11):1803–13. doi:10.1007/s00192-013-2171-2.
Glavind K, Kempf L. Colpectomy or Le fort colpocleisis--a good option in selected elderly patients. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16(1):48–51. discussion doi:10.1007/s00192-004-1218-9.
Krissi H, Aviram A, Eitan R, From A, Wiznitzer A, Peled Y. Risk factors for recurrence after Le fort colpocleisis for severe pelvic organ prolapse in elderly women. Int J Surg. 2015;20:75–9. doi:10.1016/j.ijsu.2015.06.026.
Dietz V, van der Vaart CH, van der Graaf Y, Heintz P, Schraffordt Koops SE. One-year follow-up after sacrospinous hysteropexy and vaginal hysterectomy for uterine descent: a randomized study. Int Urogynecol J. 2010;21(2):209–16. doi:10.1007/s00192-009-1014-7.
Carramao S, Auge AP, Pacetta AM, Duarte E, Ayrosa P, Lemos NL, et al. A randomized comparison of two vaginal procedures for the treatment of uterine prolapse using polypropylene mesh: hysteropexy versus hysterectomy. Revista do Colegio Brasileiro de Cirurgioes. 2009;36(1):65–72.
Maher C, Feiner B, Baessler K, Christmann-Schmid C, Haya N, Marjoribanks J. Transvaginal mesh or grafts compared with native tissue repair for vaginal prolapse. The Cochrane database of systematic reviews. 2016;2:CD012079. doi:10.1002/14651858.CD012079.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Justin Houman and James M. Weinberger each declare no potential conflicts of interest. Karyn S. Eilber is an investigator for Boston Scientific.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Female Urology
Rights and permissions
About this article
Cite this article
Houman, J., Weinberger, J.M. & Eilber, K.S. Native Tissue Repairs for Pelvic Organ Prolapse. Curr Urol Rep 18, 6 (2017). https://doi.org/10.1007/s11934-017-0648-0
Published:
DOI: https://doi.org/10.1007/s11934-017-0648-0