Abstract
Overactive bladder (OAB) is a clinical syndrome characterized by urinary urgency, frequency, and nocturia with or without accompanying urinary incontinence. Thus, using this operational definition based on symptoms at presentation, urodynamic testing is not required for an initial diagnosis of OAB. An increasing body of evidence suggests that, although there is a relationship between the urodynamic finding of detrusor overactivity and OAB, these are quite separate findings, and successful response to nonsurgical and surgical interventions for OAB does not depend on finding detrusor overactivity on urodynamic testing. The role of urodynamics in the setting of OAB is not well defined at present, but there are several clinical scenarios where such testing may be useful. However, at this time, the evidence to support their routine use in patients with OAB is limited.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The International Continence Society defines overactive bladder (OAB) as “urgency, with or without urge incontinence, usually with frequency and nocturia” [1], with the presumption that other causes such as infection have been excluded. The essential symptom of OAB is urgency, a sudden compelling desire to void, which should be distinguished from pain, which may be more associated with painful bladder syndrome [2]. This definition specifically precludes the need for immediate pressure-flow urodynamic testing (UDS) for a diagnosis of OAB in the individual patient, and also suggests that the initiation of inexpensive, completely reversible, and noninvasive management strategies such as behavioral therapy and pharmacologic therapy is acceptable without UDS. What then is the role of UDS in the setting of OAB?
It is clear that the necessary components for an initial diagnosis of OAB in an uncomplicated, previously untreated patient include a relevant history, physical examination, and urinalysis. Other conditions that may precipitate lower urinary tract symptoms, including infection, pelvic organ prolapse, pelvic masses, and bladder cancer, often can be excluded using this simple diagnostic paradigm (Table 1). In this uncomplicated population, the need for UDS is, at best, questionable. Furthermore, patients with OAB often will be managed without the use of UDS. In fact, an increasing body of evidence suggests that although there is a relationship between the urodynamic finding of detrusor overactivity (DO) and OAB, successful responses to nonsurgical and surgical interventions for OAB do not absolutely correlate with a finding of preintervention DO on UDS [3••, 4••, 5, 6•]. Thus, although UDS are not necessary for a diagnosis or initial management of OAB, these studies certainly have a role in the evaluation of lower urinary tract symptoms in a variety of circumstances. This article will attempt to define the evolving role of UDS in the setting of OAB.
Overactive Bladder and Detrusor Overactivity
DO is the urodynamic observation of involuntary detrusor contractions during the filling phase of cystometry [1]. DO is exclusively a urodynamic diagnosis and only can be found on UDS. It often, but not invariably, is associated with OAB. The diagnosis of OAB does not require urodynamic confirmation of DO [2••]. OAB symptoms (eg, urgency, frequency, and nocturia) are certainly suggestive of a subsequent finding of DO, but Digesu et al. [7] found that only 54% of females with OAB demonstrated DO on UDS. While this study used older definitions of OAB and DO, a later report by Hashim and Abrams [8] found only 44% of women with OAB but not incontinence (OAB-dry) and 58% of women with urgency urinary incontinence (UUI) and OAB (OAB-wet) demonstrated DO. Of note, in the same analysis, the correlation between OAB and DO was much higher in men (90% of OAB-wet men).
The connection between OAB symptoms and DO is somewhat obscured by studies that attempt to assess the temporal relationship between the two to establish cause and effect. While it often is stated that the patient-reported sensation of urinary urgency is the result of a concomitant involuntary detrusor contraction, this clearly is not invariably accurate. Lowenstein et al. [9] described continuous recording of patient-reported urgency during UDS of 33 patients who demonstrated DO. They found substantial variability between the patient-reported sensations of urinary urgency with respect to the onset of the DO episode. Increases in reported urgency were as likely to occur before an episode of DO as after a episode. In fact, 29% of DO episodes were not associated with an increase in urgency at all [9]. To further blur the issue, a recent report questions whether interpretation of DO in multicenter trials is sufficiently reliable to properly evaluate the correlation of DO with OAB. Renganathan et al. [10] compared the agreement rate between central and peripheral readers with respect to DO in a multicenter phase 2 drug trial of an OAB medication. While the agreement among central reviewers was excellent, there was poor agreement between the peripheral readers and the central readers. This suggests that interpretation of DO on an isolated urodynamic tracing may be somewhat variable and possibly subject to misinterpretation.
The apparent rate of DO in asymptomatic patients also casts some doubt as to the role DO plays in OAB syndrome. Heslington and Hilton [11] recruited 22 asymptomatic volunteers to attempt to establish normal ranges for cystometric variables on ambulatory urodynamic monitoring. Using conventional and ambulatory UDS monitoring, they found DO in 18% and 68% of patients, respectively. It is unclear if the high rates of DO in the ambulatory studies in these asymptomatic individuals reflect a true rate of DO or were simply provoked by the monitoring/testing situation or by the UDS catheter [11]. Recently, Lee et al. [12] have shown that the rates of DO are higher in patients with OAB when compared to patients without OAB. Ho et al. [13] demonstrated rates of DO that were significantly higher than controls in female patients with diabetes and OAB, though the overall rate was quite low at 29%. The most common urodynamic finding was increased bladder sensation. Nevertheless, there are objective differences between patients with OAB who have DO and those who do not. Guaralnick et al. [14] reviewed 146 women with OAB, comparing those with and without DO. While the symptomatology was similar between the two groups, the patients with OAB with DO tended to be older, have smaller maximum voided volumes, have more incontinent episodes, and be more likely to report early strong desire and urgency.
Is Overactive Bladder a Motor or Sensory Condition?
Historically, antimuscarinic drugs were thought to provide a primary therapeutic benefit in OAB by blocking parasympathetic input to muscarinic receptor subtypes, thus inhibiting detrusor contractility. This view was bolstered by the theory that OAB symptoms were chiefly the result of uninhibited detrusor contractions seen on UDS. Previous studies had provided this framework for attempting to understand the etiology of OAB by showing structural changes in detrusor myocytes that suggested a motor dysfunction as the root cause [15, 16]. More recently, there has been accumulating evidence to suggest a sensory disorder is the principal cause of OAB symptoms in some individuals. Researchers have begun to identify possible neurochemical changes that occur in patients with lower urinary tract dysfunction that correspond to an afferent as well as efferent etiology for OAB [17, 18]. Furthermore, oxybutynin, darifenacin, and tolterodine treatments all have been shown to affect bladder afferent neural pathways, including C fibers and A-δ fibers [19–21]. Lee et al. [12] attempted to evaluate the sensory threshold of patients with OAB using the current perception threshold test, which uses an intravesical electrode to test sensation. They found that patients with OAB had significantly lower perception thresholds compared with patients without OAB, suggesting that the patients with OAB had increased bladder sensitivity.
While an afferent component likely contributes to etiology of OAB, there also is evidence to suggest that involuntary detrusor contractions are not primary etiologies of OAB as once was believed. In a comprehensive review, Finney et al. [22] found that, at clinically relevant doses, antimuscarinics have little effect on bladder contractility. Instead, he suggests that these agents primarily act on sensory variables such as urgency, time to first sensation to void, and urinary frequency. Panayi et al. [23] utilized bladder wall thickness and patient perception of condition as metrics for motor and sensory dysfunction, respectively. They found that while improvement in bladder wall thickness stopped 6 weeks following initiation of antimuscarinic therapy, improvement of sensory parameters such as urgency continued to improve throughout the 12 weeks of treatment, suggesting that sensory rather than motor benefit was the primary action of the treatment. It can be hypothesized that the association between OAB symptoms and DO seen in some studies actually may be the result of afferent signals provoking the motor dysfunction. Juszczak et al. [24] induced OAB in an animal model with the administration of cyclophosphamide. They treated some of the OAB-induced animals with capsaicin or lidocaine instillation before performing UDS, comparing the treated animals to healthy controls. While they found that DO was higher than that in normal controls, modulation of unmyelinated afferent C fibers with capsaicin and lidocaine reduced DO. These data suggest that the afferent signals blocked by the capsaicin and lidocaine treatments were somewhat responsible for the DO.
Response to Intervention in Overactive Bladder
The diagnosis of DO might be important before initiating therapy for OAB if it predicts response to therapy. Trials evaluating the effects of antimuscarinic treatments on OAB provide insight into whether the diagnosis of DO has any effect on response to treatment. Nitti et al. [3••] found that the response to fesoterodine in patients with OAB and UUI was independent of the urodynamic finding of DO. Patients with and without DO had similar changes in voids per 24 hours and UUI episodes. Malone-Lee et al. [4••] found similar results in a 12-week evaluation of tolterodine ER (extended release) for the treatment of OAB. While patients on antimuscarinic treatment showed greater improvement in mean voided volume and mean voiding frequency compared to placebo, the drug effect did not depend on demonstrating DO. Both of these studies concur with prior work showing the lack of a clear relationship between DO and response to pharmacologic or behavioral therapy.
It has been suggested that when planned therapy is expensive or invasive, such as with botulinum toxin or sacral neuromodulation, urodynamic evaluation may provide some guidance or prognostic information [25]. The data on botulinum toxin A is mixed in this regard. Sahai et al. [26] sought to identify urodynamic parameters that might predict the patients treated with botulinum toxin who would require intermittent catheterization for urinary retention. In their assessment of 67 patients injected with 200 units, 29% were started on intermittent catheterization for de novo urinary retention. Measures of detrusor contraction strength were found to be associated with postprocedure need for intermittent catheterization. It is not clear if these values might be independently predictive of this need. In their evaluation of treatment of idiopathic OAB with 100 versus 150 units of botulinum toxin A, Cohen et al. [27] performed UDS before and after injection and found that, although postvoid residuals were increased at 12 weeks, other urodynamic parameters, including presence of DO, were unchanged by treatment despite improvement in symptoms and quality of life. In an abstract presented at the 2010 American Urological Association meeting, response to botulinum toxin A was likewise independent of the finding of DO at baseline [5].
Finally, several studies have suggested that the response to sacral neuromodulation is not dependent on the preoperative demonstration of DO. South et al. [6•] retrospectively reviewed 104 patients with refractory UUI who underwent a sacral neuromodulation test stimulation. They found no correlation linking presence or absence of DO with the likelihood of response. They concluded that sacral neuromodulation testing could proceed in the absence of demonstrated DO. Groenendijk et al. [28•] prospectively studied 111 patients with nonneurogenic urgency incontinence, with 67 patients demonstrating DO on preoperative UDS. Presence of preoperative DO did not predict a better clinical outcome, a finding which echoes that of South et al. [6•], who demonstrated no correlation between DO and neuromodulation test stimulation. Thus, while sacral neuromodulation may result in decreased DO seen on postprocedure UDS [28•], this does not appear to equate with clinical response in many cases.
Indications for Urodynamic Testing in the Setting of Overactive Bladder
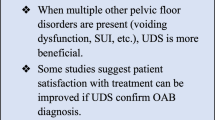
Significant questions and controversy remain about who should be evaluated with UDS testing when presenting with symptoms of urgency or UUI. While some will argue that patients with OAB may be treated safely without the additional information gleaned from UDS, others would argue that it may be difficult to sort out patients with idiopathic OAB from those with other underlying causes for their lower urinary tract symptoms. In general, if the expected findings on UDS will change management strategy in an individual patient, it is reasonable to pursue this type of testing. In addition, in cases where there exists the suspicion that the upper urinary tract is at risk due to potential lower urinary tract disturbances such as decreased compliance, assessment of the lower urinary tract with UDS should be pursued. As such, and in the absence of evidence-based guidelines, several scenarios may be suggested as prompts for UDS in the patient with OAB (see Table 2). However, there is little high-level evidence to guide the clinician in choosing the timing of UDS in these settings.
Conclusions
The appropriate application of UDS in the evaluation and management of OAB remains controversial. Optimally balancing the cost, invasiveness, and potential morbidity of UDS against the potential diagnostic and prognostic information gained from its utilization is an ongoing process. While DO is found in a large percentage of patients evaluated with UDS for OAB, DO also is found in a significant number of patients without urinary symptoms. Current data suggest that presence or absence of DO is not wholly predictive of successful response to therapy, whether this treatment is pharmacologic or otherwise. This lack of predictive power validates the current theory that OAB may be as much a sensory as a motor dysfunction. When UDS is expected to alter management strategy or is relied upon to provide prognostic data such as risk of upper tract deterioration, this expensive and somewhat invasive testing is justified. However, at this time, the evidence to support their routine use in patients with OAB is limited.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Abrams P, Cardozo L, Fall M, et al.: The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Am J Obstet Gynecol 2002, 187:116–126.
Abrams P: Describing bladder storage function: overactive bladder syndrome and detrusor overactivity. Urology 2003, 62(5 Suppl 2):28–37.
•• Nitti VW, Rovner ES, Bavendam T: Response to fesoterodine in patients with an overactive bladder and urgency urinary incontinence is independent of the urodynamic finding of detrusor overactivity. BJU Int 2010, 105:1268–1275. In this report from a randomized placebo-controlled trial of fesoterodine, response of overactive bladder symptoms to antimuscarinic treatment was not dependent on finding of detrusor overactivity on pretreatment urodynamics.
•• Malone-Lee JG, Al-Buheissi S: Does urodynamic verification of overactive bladder determine treatment success? Results from a randomized placebo-controlled study. BJU Int 2009, 103:931–937. In this trial of tolterodine-ER, patients were stratified into groups of patients with and without pretreatment detrusor overactivity. Presence of detrusor overactivity could not be used to predict response to treatment or placebo, suggesting that urodynamic assessment of detrusor overactivity may not be required before treatment of overactive bladder with antimuscarinic therapy.
Eric R: Urodynamic results and clinical outcomes with intravesical botulinum toxin a (onabotuliumtoxina) in a randomized, placebo-controlled, dose-finding study in idiopathic overactive bladder. J Urol 2010, 183(4 Suppl):e591–e592.
• South MM, Romero AA, Jamison MG, et al.: Detrusor overactivity does not predict outcome of sacral neuromodulation test stimulation. Int Urogynecol J Pelvic Floor Dysfunct 2007, 18:1395–1398. This retrospective review found that patients characterized as responders to test neurostimulation for overactive bladder were not more likely to have detrusor overactivity on pretreatment urodynamics than those who failed to respond to a test stimulation, suggesting that detrusor overactivity is not a requirement for test neurostimulation.
Digesu GA, Khullar V, Cardozo L, Salvatore S: Overactive bladder symptoms: do we need urodynamics? Neurourol Urodyn 2003, 22:105–108. (Published erratum appears in Neurourol Urodyn 2003, 22:356.)
Hashim H, Abrams P: Is the bladder a reliable witness for predicting detrusor overactivity? J Urol 2006, 175:191–194.
Lowenstein L, Pham T, Abbasy S, et al.: Observations relating to urinary sensation during detrusor overactivity. Neurourol Urodyn 2009, 28:497–500.
Renganathan A, Cartwright R, Cardozo L, et al.: Quality control in urodynamics: Analysis of an international multi-center study. Neurourol Urodyn 2009, 28:380–384.
Heslington K, Hilton P: Ambulatory monitoring and conventional cystometry in asymptomatic female volunteers. Br J Obstet Gynaecol 1996, 103:434–441.
Lee SR, Kim HJ, Kim A, Kim JH: Overactive bladder is not only overactive but also hypersensitive. Urology 2010, 75:1053–1059.
Ho CH, Tai HC, Yu HJ: Urodynamic findings in female diabetic patients with and without overactive bladder symptoms. Neurourol Urodyn 2010, 29:424–427.
Guralnick ML, Grimsby G, Liss M, et al.: Objective differences between overactive bladder patients with and without urodynamically proven detrusor overactivity. Int Urogynecol J Pelvic Floor Dysfunct 2010, 21:325–329.
Brading AF: A myogenic basis for the overactive bladder. Urology 1997, 50(6A Suppl):57–67.
Maake C, Landman M, Wang X, et al.: Expression of smoothelin in the normal and the overactive human bladder. J Urol 2006, 175:1152–1157.
Rapp DE, Lyon MB, Bales GT, Cook SP: A role for the P2X receptor in urinary tract physiology and in the pathophysiology of urinary dysfunction. Eur Urol 2005, 48:303–308.
Ford AP, Gever JR, Nunn PA, et al.: Purinoceptors as therapeutic targets for lower urinary tract dysfunction. Br J Pharmacol 2006, 147(Suppl 2):S132–S143.
De Laet K, De Wachter S, Wyndaele JJ: Systemic oxybutynin decreases afferent activity of the pelvic nerve of the rat: new insights into the working mechanism of antimuscarinics. Neurourol Urodyn 2006, 25:156–161.
Iijima K, De Wachter S, Wyndaele JJ: Effects of the M3 receptor selective muscarinic antagonist darifenacin on bladder afferent activity of the rat pelvic nerve. Eur Urol 2007, 52:842–847.
Boy S, Schurch B, Mehnert U, et al.: The effects of tolterodine on bladder-filling sensations and perception thresholds to intravesical electrical stimulation: method and initial results. BJU Int 2007, 100:574–578.
Finney SM, Andersson KE, Gillespie JI, Stewart LH: Antimuscarinic drugs in detrusor overactivity and the overactive bladder syndrome: motor or sensory actions? BJU Int 2006, 98:503–507.
Panayi DC, Tekkis P, Fernando R, Khullar V: Is the beneficial effect of antimuscarinics related to motor or sensory changes in the bladder? Int Urogynecol J Pelvic Floor Dysfunct 2010, 21:841–845.
Juszczak K, Ziomber A, Wyczolkowski M, Thor PJ: Urodynamic effects of the bladder C-fiber afferent activity modulation in chronic model of overactive bladder in rats. J Physiol Pharmacol 2009, 60:85–91.
Goldman HB, Vasavada SP: Female urology: a practical clinical guide. Totowa, NJ: Humana Press; 2007.
Sahai A, Khan MS, Le Gall N, et al.: Urodynamic assessment of poor responders after botulinum toxin-A treatment for overactive bladder. Urology 2008, 71:455–459.
Cohen BL, Barboglio P, Rodriguez D, Gousse AE: Preliminary results of a dose-finding study for botulinum toxin-A in patients with idiopathic overactive bladder: 100 versus 150 units. Neurourol Urodyn 2009, 28:205–208.
• Groenendijk PM, Lycklama a Nyeholt AA, Heesakkers JP, et al.: Urodynamic evaluation of sacral neuromodulation for urge urinary incontinence. BJU Int 2008, 101:325–329. This study of patients with neurostimulator placement for overactive bladder found that even those patients with pretreatment detrusor overactivity on urodynamics who had resolution of their detrusor overactivity 6 months later while the stimulator was on had no difference in rates of improvement in symptoms over those patients who had no resolution of detrusor overactivity.
Disclosures
No potential conflicts of interest relevant to this article have been reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rovner, E.S., Goudelocke, C.M. Urodynamics in the Evaluation of Overactive Bladder. Curr Urol Rep 11, 343–347 (2010). https://doi.org/10.1007/s11934-010-0130-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11934-010-0130-8