Abstract
Introduction and hypothesis
The aim of the study was to assess the sensory and motor effects of antimuscarinic treatment on the bladder in women with overactive bladder, detrusor overactivity demonstrated on urodynamics and a mean bladder wall thickness (BWT) greater than 5 mm.
Methods
Fifty-eight women underwent treatment with antimuscarinics in 12 weeks. Before treatment and at 1, 2, 6 and 12 weeks of treatment, women completed the patient perception of bladder condition (PPBC) single-item global questionnaire, indicated the severity of their urgency on a visual analogue scale (VAS) and underwent transvaginal ultrasound to determine mean bladder wall thickness (BWT).
Results
PPBC and VAS scores for urgency declined throughout the treatment course whereas mean BWT declined during the first 6 weeks of treatment and then reached a plateau after falling to below 5 mm.
Conclusion
The mechanism of action of antimuscarinics appears to be a complex interaction of sensory and motor components.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Idiopathic detrusor overactivity is a urodynamic diagnosis with an unknown aetiology. It is characterised by involuntary contractions of the detrusor muscle during the filling phase of urodynamics that may be spontaneous or in response to provocation such as listening to running water [1].
Detrusor overactivity is associated with the overactive bladder syndrome [2] of which the cardinal symptom is urgency which may or may not be associated with urge urinary incontinence [1]. The two main theories for the development of this condition are of mechanical, myogenic origin, or of sensory origin and results from altered bladder sensation. Brading supported the myogenic view upon reviewing the available evidence including analysis of detrusor myocytes, smooth muscle strips and miscroscopic analysis of the bladder wall and demonstrated changes in both structure, denervation and properties of the bladder wall in overactive bladder [3].The sensory function is altered as evidenced by Oliver and co-authors who used a validated method of recording urgency severity using a keypad during filling cystometry and demonstrated rising urgency scores associated with filling in the absence of involuntary detrusor contractions [4] and studies that demonstrate when the bladder is desensitised there is a reduction in urgency episodes [5].
The first line drug treatment for this condition is antimuscarinics which have been presumed to work by blocking muscarinic receptors in the bladder and as a result impair contractions of the detrusor muscle. Ambulatory urodynamics has shown that antimuscarinics reduce the number of non-voiding detrusor contractions and the area under the detrusor pressure curves when compared to placebo [6]. This opinion is now under scrutiny as further evidence does not strongly support this point of view. Finney and co-authors carried out a review of the available evidence for the mechanism of action of antimuscarinics and found them to be associated with a significant effect on bladder sensation such as urgency, time to first sensation to void, and voiding frequency. The authors also demonstrated that four studies did not show any effect on bladder contractility [7].
A more recent review of the current evidence for the mechanism of action concluded that there was evidence from animal studies that suggested that antimuscarinics may exert an inhibitory effect on bladder afferent nerves. The review also identified that the presence of muscarinic receptors in the urothelium and suburothelial myofibroblasts may indicate their role in urothelial sensory function. It is therefore proposed that the blockade of these muscarinic receptors may lead to improvement in OAB symptoms in patients taking antimuscarinics [8].
The measurement of the bladder wall thickness in women was first described in 1994 [9]. It was based on the principle that repetitive contractions of the detrusor muscle against a closed sphincter would result in muscle hypertrophy as a result of isometric contractions which manifest as an increase in the ultrasound measurement of the bladder wall thickness. The original technique described transvaginal measurements of three anatomical sites: on the anterior bladder wall, at the dome as well as the trigone of the bladder containing less than 50 ml of urine. From these three measurements, the mean bladder wall thickness (BWT) was obtained with a value of greater than 5 mm found to be associated with detrusor overactivity [9, 10].
The aim of the study was to assess the sensory and motor effects of antimuscarinic treatment on the bladder in women with overactive bladder and detrusor overactivity demonstrated on urodynamics. Changes in sensation were determined using a VAS for urgency and mean BWT measurements were used to assess changes in the detrusor muscle in response to antimuscarinic treatment. We also wanted to assess the effect of antimuscarinics on womens’ overall perception of their bladder problem using the PPBC and whether these changes were linked to either mean BWT or the symptom of urgency.
Methods
Women were recruited from attenders to a urodynamics and urogynaecology clinic at a tertiary referral centre. All women gave a history of overactive bladder symptoms and no stress urinary incontinence. All women also had a urodynamic diagnosis of detrusor overactivity with no urodynamic evidence of stress urinary incontinence.
No subjects had co-existent symptomatic pelvic organ prolapse or POP-Q scores higher than −2 for anterior or posterior parameters. Subjects with symptoms or objective evidence of acute or chronic cystitis were excluded from the study. No women were actively taking any antimuscarinic medication at the time of recruitment to the study. Women who had previously taken antimuscarinic medication were admitted as long as they had not taken any such treatment in the previous 6 months. All women gave their informed consent to participate in the study and ethical approval for the study was obtained from the St. Mary’s LREC.
At the initial visit, women were asked to complete the patient perception of bladder condition (PPBC) is a validated, single-item global questionnaire [11] with a six-point scale that ranges from the answer ‘my bladder causes me no problems at all’ to ‘my bladder causes me many severe problems’.
Subjects were also asked to determine the degree of severity of their urgency symptoms using a visual analogue scale (VAS) consisting of a horizontal line measuring 10 cm marked from 1 to 10. Women were asked to indicate the severity of the urgency they had experienced during the course of the last 7 days along this scale giving a score ranging from 1 to 10.
Women also underwent transvaginal ultrasound measurement of the thickness of the bladder wall at three anatomical sites: the trigone, dome of the bladder and anterior bladder wall [9, 10]. From these three measurements, the mean BWT was determined and only women with a mean BWT of greater than 5 mm were included. PPBC scored between 1 and 6 whilst VAS scores ranged between 1 and 10 depending on where the subject marked along the horizontal line.
Following this initial assessment, women were then commenced on antimuscarinic treatment. The antimuscarinic of choice was determined by the individual clinician, but those women that had previously used a specific antimuscarinic that had been ineffective were given an alternative.
Women were subsequently seen at weeks 1, 2, 6 and 12 following antimuscarinic treatment. At each of these visits, the PPBC and VAS was completed and transvaginal ultrasound measurement for mean BWT was conducted.
Women who stopped antimuscarinic treatment due to unwanted side effects or personal choice, at any stage of the study, were removed from the study. Women who were changed to an alternative antimuscarinic during the course of the study were excluded from the study.
The data obtained was analysed using SPSS 14.0 for Windows.
Results
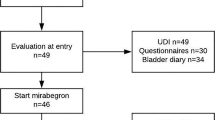
Fifty-eight women attended all visits, completed all questionnaires, underwent transvaginal ultrasound scan for mean BWT at each of the visits and responded to the antimuscarinic treatment. The mean age of subjects is 61 (range 39–81 years).
Of these 58 women, 23 were given tolterodine SR, 19 were prescribed solifenacin, 11 were treated with oxybutynin SR, four were treated with fesoterodine and one was treated with darifenacin. The percentage reduction in each of the measured components is shown in Fig. 1. The mean scores for BWT, VAS and PPBC and 95% confidence intervals at each visit, for each parameter are shown in Figs. 2, 3 and 4.
There is a downward trend from the beginning for PPBC, VAS and BWT until week 6 which is statistically significant (Friedman test p < 0.001). From week 6 to week 12 there is a statistically significant reduction in PPBC and VAS scores but BWT remains unchanged thus the improvement in symptoms continues without a corresponding change in BWT (Table 1).
Prior to commencing treatment the mean BWT of all subjects was greater than 5 mm but subsequent to treatment the mean BWT subsequently fell to below 5 mm which is within the normal range. Table 2 shows the VAS and PPBC scores when related to women who whose mean BWT was greater than 5 mm and those with a mean BWT that was less than 5 mm during the study. From these data it can be seen that a BWT greater than 5 mm was associated with statistically significantly higher PPBC and VAS scores.
Discussion
In this study, we have demonstrated a trend of a falling sensation of urgency and overall bladder problems as demonstrated by the reduction in scores of the VAS for urgency and PPBC as well as a reduction in mean BWT in response to treatment with antimuscarinics in the first 6 weeks of treatment. This demonstrates that there is a reduction in bladder wall thickness associated with an improvement in urgency severity. We believe that this study reveals an important clinical finding, specifically, that elevated mean bladder thickness is reversible with treatment with antimuscarinics. This is related to the reduction in urgency but the precise mechanism of this cannot be ascertained. The reduction of mean bladder wall thickness may imply that recognised features of overactive bladder syndrome such as trabeculations may also be reversible with antimuscarinic treatment.
In the following 6 weeks the reduction in PPBC and VAS scores continues, but the reduction in mean BWT reaches a plateau. We can conclude that the overall improvement of the womens’ bladder demonstrated by the reduction in PPBC scores seems to be more closely associated with VAS score for urgency which also continue to decline. The mean bladder wall thickness seems to be therefore unrelated to continuing improvement of bladder condition during this time period. This may represent the return of mean bladder wall thickness to within the normal range (less than 5 mm) where it is no longer associated with overactive bladder symptoms. The sharpest reduction in urgency severity and PPBC scores are associated with the reduction of mean bladder wall thickness from benign abnormally high to below the threshold of 5 mm.
This is supported by assessing those women with a mean BWT of greater than 5 mm at any stage during the study, and those with a mean BWT of less than 5 mm at any point during the study; there is a clear association between mean BWT and VAS for urgency and PPBC with both scores being statistically significantly higher in women with a mean BWT of greater than 5 mm. Alternatively, sensory mechanisms that determine women’s symptoms of urgency may act independently of mean bladder wall thickness.
The interaction between symptoms, bladder sensation and motor activity appears to be complex. Finney and co-authors assessed the interaction between the motor and sensory components within the bladder wall and the role of antimuscarinics in their study of intravesical pressures within isolated bladders from guinea pigs exposed to both muscarinic receptor agonists and M2 and M3 selective antagonists. Based on their findings the authors proposed the existence of three interrelated mechanisms that contributed to contractile activity: a mechanism to effect a global contraction of the bladder, a pacemaker and a conductive. The latter two mechanisms serve to produce and propagate contractions, respectively, locally in the bladder wall [12]. Interestingly, the authors found that the pacemaker component was more sensitive to the M3 specific antimuscarinic used, darifenacin. Studies such as these may provide further insight into the mechanism of the overactive bladder syndrome and the action of antimuscarinics routinely used to treat this condition.
Conclusion
Whilst we demonstrated a rapid progressive reduction in bladder wall thickness associated with an improvement in urgency and perception of bladder condition, this did not persist after 6 weeks of treatment with antimuscarinics. The sensory parameters we assessed continued to improve up until 12 weeks of treatment leading to the conclusion that the effect of antimuscarinics on the bladder appears to be predominantly sensory especially during prolonged use of these therapies. The mechanism of action by which antimuscarinics improve urgency remains complex.
References
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, van KP, Victor A, Wein A (2002) The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Am J Obstet Gynecol 187:116–126
Digesu GA, Khullar V, Cardozo L, Salvatore S (2003) Overactive bladder symptoms: do we need urodynamics? Neurourol Urodyn 22:105–108
Brading AF (1997) A myogenic basis for the overactive bladder. Urology 50:57–67
Oliver S, Fowler C, Mundy A, Craggs M (2003) Measuring the sensations of urge and bladder filling during cystometry in urge incontinence and the effects of neuromodulation. Neurourol Urodyn 22:7–16
Silva C, Silva J, Castro H, Reis F, Dinis P, Avelino A, Cruz F (2007) Bladder sensory desensitization decreases urinary urgency. BMC Urol 7:9
Abrams P, Cardozo L, Chapple C, Serdarevic D, Hargreaves K, Khullar V (2006) Comparison of the efficacy, safety, and tolerability of propiverine and oxybutynin for the treatment of overactive bladder syndrome. Int J Urol 13:692–698
Finney SM, Andersson KE, Gillespie JI, Stewart LH (2006) Antimuscarinic drugs in detrusor overactivity and the overactive bladder syndrome: motor or sensory actions? BJU Int 98:503–507
Yamaguchi O (2010) Antimuscarinics and overactive bladder: other mechanism of action. Neurourol Urodyn 29(1):112–115
Khullar V, Salvatore S, Cardozo L, Bourne TH, Abbott D, Kelleher C (1994) A novel technique for measuring bladder wall thickness in women using transvaginal ultrasound. Ultrasound Obstet Gynecol 4:220–223
Khullar V, Cardozo LD, Salvatore S, Hill S (1996) Ultrasound: a noninvasive screening test for detrusor instability. Br J Obstet Gynaecol 103:904–908
Coyne KS, Matza LS, Kopp Z, Abrams P (2006) The validation of the patient perception of bladder condition (PPBC): a single-item global measure for patients with overactive bladder. Eur Urol 49:1079–1086
Finney SM, Stewart LH, Gillespie JI (2007) Cholinergic activation of phasic activity in the isolated bladder: possible evidence for M3- and M2-dependent components of a motor/sensory system. BJU Int 100:668–678
Acknowledgments
We would like to express our gratitude for the support provided by the NIHR Biomedical Research Centre funding scheme.
Conflicts of interest
D. C. Panayi: funded by Pfizer for travel and accommodation -- International Continence Society Cairo 2008. V. Khullar: paid consultant to Astellas, Lilly, Allergan, Pfizer, Gynecare, Cook, Bioxell. R. Fernando: paid consultant to Astellas, Pfizer. P. Tekkis: no disclosures.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Panayi, D.C., Tekkis, P., Fernando, R. et al. Is the beneficial effect of antimuscarinics related to motor or sensory changes in the bladder?. Int Urogynecol J 21, 841–845 (2010). https://doi.org/10.1007/s00192-010-1123-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-010-1123-3