Abstract
For the projected 1,638,910 patients with a diagnosis of cancer this year, the great majority of them (75–90 %) will experience cancer-related pain. A growing number of these patients will turn to complementary and alternative therapies to assist with the management of their pain and other cancer-related symptoms. The World Health Organization’s suggested approach to pain management begins with the use of time honored opioids, but recommends the use of adjuvant therapies early in the management process. Complementary and alternative therapies are being used by more patients each year to assist with the management of their pain. Practitioners and researchers must be aware of the evidence that exists to support or refute the use of these therapies. In this manuscript we review evidence from the recent past on complementary and alternative therapies for pain with emphasis on more common modalities including acupuncture, bio-energy, massage, and music.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pain Prevalence
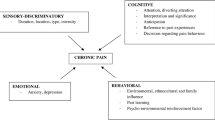
About 1,638,910 new cancer cases are expected to be diagnosed in 2012 [1]. Seventy-five to ninety percent of patients with cancer experience pain some time during their illness. It is estimated that up to 50 % of cancer patients who have pain, are under-treated. The International Association for the Study of Pain (IASP), defines pain as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage” [2]. Pain occurs in approximately one quarter of patients with newly diagnosed malignancies, one-third of patients undergoing treatment, and three-quarters of patients with advanced disease, and is one of the symptoms patients fear most [3]. Cancer pain is especially prevalent in cases where the cancer has spread, or metastasized to the bone. In fact, up to 80 % of patients who have bone metastasis experience pain [4].
Pain that continues, or is unrelieved, significantly impacts the patient and his/her family making the diagnosis of cancer and the progression of the disease even more difficult. The importance of relieving pain and the availability of effective therapies make it imperative that health care providers caring for these patients be adept at the assessment and treatment of cancer pain [3].
Pain is classified into three different types: somatic, neuropathic, and visceral. Somatic pain is the result of activity by pain receptors in the deep tissues of the body, or on the surface. An example of deep tissue pain would be that of cancer that has spread to the bone. This type of pain is often described as dull and achy. An example of surface pain is pain at a surgical incision site. People describe this pain as being sharp, and possibly have a burning sensation. In contrast, surface pain is easily pinpointed and is sharp or burning [3].
Neuropathic pain is the most severe of the three types of pain. It can be difficult to isolate, and patients may describe this as a burning or tingling sensation. Injury to the nervous system, or disrupted transmission such as occurs when a tumor puts pressure on the spinal cord or nerves is the culprit in this type of pain. Chemotherapy or radiation can also cause chemical damage to the nervous system resulting in pain [3].
Visceral pain is pain felt in or near internal organs caused by the activity of pain receptors in these areas. In cancer, the activation of pain receptors can be caused by a tumor putting pressure on one or more of the organs, the stretching of the viscera, or general invasion of cancer [3]. Patients describe this type of pain as having a throbbing, pressured sensation.
Cancer is associated with all three types of pain. Because patients may be experiencing visceral, somatic, and neuropathic pain at any point, or all at once, it is crucial that both patients and providers consider multimodal approaches to pain control.
Pharmacotherapeutic Pain Treatment
When cancer pain is only partially treated, or left untreated, the patient experiences a decrease in function, appetite, and sleep. This leads to increased depression and a lower quality of life. Cancer pain is a frustrating and debilitating concern for patients as well as caregivers [5]. Health care practitioners depend heavily on opioid therapies for pain of this magnitude, and this therapy is very effective. However, as effective as this treatment modality is, it is not without side effects. For example, side effects of opioids include constipation, urinary retention, nausea, sedation, respiratory depression, myoclonus, delirium, sexual dysfunction and hyperalagesia [5]. These side effects are significant, often debilitating, and further add to the loss of function and decreased quality of life.
The American Cancer Society and the National Comprehensive Cancer Network guidelines suggest patients who report a pain score of 4 or greater on a ten-point scale after analgesic adjustment, non-pharmacologic treatment should be added to the plan of care [5]. Twenty-five years ago, the World Health Organization (WHO) listed opioid analgesics at the top of the pharmacological pain control ladder; integrative therapies was listed at the bottom (sixth rung) [6]. Today, relaxation training, guided imagery, hypnosis and biofeedback are strategies that should be regarded as mainstream adjunctive treatments for reduction of pain and anxiety, improved coping and increased self-efficacy [6]. The most current WHO analgesic ladder is a three-step process, with adjuvants listed at all three levels [7]. Nonopioid therapies, along with an adjuvant therapy, are listed at step 1 of the ladder for use in mild pain. If pain is not relieved, an opioid appropriate for mild to moderate pain can be added as well as continued use of adjuvant therapies at step 2. Step 3 suggests choice of an opioid appropriate for moderate to severe pain, the use of non-opioids, and adjuvant therapies [7].
Complementary Therapies
Many people with cancer, along with traditional Western treatments, use one or more non-traditional kinds of alternative or complementary therapies. The National Comprehensive Cancer Network, cited by Bardia et al. [8], provided an overview of the complementary therapies currently recommended to patients undergoing cancer treatment (Table 1).
The Current Evidence
A systematic literature review conducted in 2006 revealed only 18 trials on which to report regarding utilization of complementary and alternative medicine therapies in relieving cancer pain [8]. The researchers concluded that hypnosis, imagery, support groups, acupuncture and healing touch seemed promising, “but none could be recommended because of a paucity of rigorous trials” [8]. The authors recommended methodologically stronger studies to better understand the potential efficacy of complementary and alternative medical (CAM) interventions.
One year later, in 2007, two publications [9, 10] provided a review and concluded that integrative therapies incorporated into practice have the ability to “reduce the perception of pain and improve the quality of life” [9]. One of these authors, Cassileth et al. [9], further stated, “acupuncture, massage therapy, mind-body medicine, music therapy and exercise are safe and effective” for pain relief in cancer patients. Pujol and Monti [10] concurred, noting traditional Chinese medicine (acupuncture and herbs), mind body medicine, and therapeutic massage all have some supportive empirical evidence or preliminary data to support their use in clinical practice with cancer pain.
Kassab et al. [11] reviewed the literature related to homeopathic medicines in search of adverse effects in conjunction with Western cancer treatments. The authors did not find any contraindications to homeopathic medicines, and were able to find preliminary support for the efficacy of topical homeopathic remedies for acute dermatitis related to radiotherapy and oral washes for chemotherapy-induced stomatitis [11].
Landier and Tse [12] performed an integrative review of complementary and alternative medical interventions for the management of pain, anxiety, and distress in pediatric oncology patients, revealing 32 studies meeting inclusion criteria for the review. The authors found two level I studies, 18 level II studies, nine level III studies, one level IV and one level V study. None of the studies reported on biologically based practices, energy therapies, or manipulative or body-based practices. “The three most common CAM interventions identified for procedural pain, anxiety and distress included hypnosis, distraction and imagery” [12]. Forty-six percent of those studies reviewed from 1999–2009 included pharmacological interventions as opposed to only 28 % of studies from earlier reports reflecting the adoption of more aggressive pharmacological management of pain in children [12].
Literature on the potential impact on pain for cancer patients who used massage therapy, acupuncture and psychological/behavioral interventions was reviewed by Casileth and Keefe [13]. The authors found those therapies are inexpensive, safe, non-invasive and absent of side effects. They also noted that evidence for those modalities continues to accumulate and encouraged their use in light of increasing costs and decreasing availability of physicians.
More recently, Running and Turnbeaugh [14] reported evidence exists from well-designed randomized controlled trials (level II) supporting the use of acupuncture for bone pain, visceral pain and neuropathic pain and analgesic care to increase function, decrease pain intensity, numbness tingling and analgesic use. Level II evidence is also available that supports the use of massage therapy for increasing immune function and mood, decreasing anxiety, and lessening bone and visceral pain, depression, blood pressure, nausea and constipation [14]. With each passing year, more evidence is available to support the use of complementary therapies in the treatment of cancer pain.
This manuscript will serve as a review of research related to complementary therapies used for cancer pain from the recent past in an effort to provide evidence for or against their efficacy and appropriateness. It is the authors’ aim to assist practitioners in decision-making and patient education choices regarding the use of CAM as adjuvant therapy for their patients with cancer related pain.
Acupuncture and Cancer Pain
Acupuncture is thought to directly modulate the affective-cognitive aspect of pain perception and changes in brain-functional magnetic resonance imaging (MRI) signals are observed during acupuncture. The Society for Integrative Oncology’s (SIO) Integrative Oncology Practice Guidelines [15] strongly support the use of acupuncture as a recommended complementary therapy for pain control when pain is poorly controlled, when side effects from other modalities are clinically significant, or when reducing the amount of pain medicine becomes a clinical goal. The SIO also recommends acupuncture as a complementary therapy when nausea and vomiting associated with chemotherapy are poorly controlled. These recommendations, published in 2007, are in keeping with the literature reviewed related to acupuncture. In addition to these recommendations, new research shows promise for acupuncture in additional areas of treatment.
O’Regan and Filshie [16] reviewed randomized clinical trials in an effort to determine acupuncture’s effect on various common cancer symptoms. They note that while there are reports in the literature supporting acupuncture for cancer symptoms, the trials are of varying quality. The authors conclude acupuncture has a potential role in managing the following cancer symptoms: pain, nausea and vomiting, xerostomia, hot flushes, fatigue, anxiety, depression, and insomnia [16]. They also determined that because acupuncture is safe with very minimal side effects, health care practitioners should be open to the use of acupuncture with their cancer patients.
Paley et al. [17] reviewed databases and synthesized the evidence related to physiotherapists and the use of acupuncture in treating bone pain. This review revealed more than 50 % of cancer patients use complementary therapies for pain and other symptoms. The reviewers found that acupuncture is used extensively in palliative care programs to manage pain and cancer-related nausea and vomiting, breathlessness, fatigue, xerostomia and vasomotor symptoms. They were not able to identify any particular studies specifically related to the use of acupuncture for bone pain. As physiotherapists, they argued that while patients are not typically referred to them for care, they are well suited to provide this service to patients who would benefit from the treatment for breakthrough and long-term pain relief.
Hopkins-Hollis [18] analyzed 9 years of published research on the use of acupuncture as a treatment modality for cancer pain. She found 11 articles that were suitable for review, including four level I studies (one pilot and three RCTs), two level III studies (non-experimental) and four level V studies (experiential evidence). Hopkins-Hollis concluded that because of a lack of level I and II studies pertaining to acupuncture as a direct intervention, and because the non-experimental studies could not infer causality and lack generalizability, additional studies must be conducted. Conduct of these level I and II studies will shed light on the mechanisms of acupunctures actions and have the potential to make acupuncture more accessible.
Bao et al. [19] conducted a randomized trial evaluating the effect of acupressure in relieving procedural pain for patients undergoing bone marrow aspiration and biopsy. The authors found that in this sample (N = 77) they were able to significantly reduce the incidence of severe pain in the treatment group compared with the sham group when using magnetic acupuncture. They did not find any significant differences in median pain for their sample.
Johnstone [20] first published in 2001 regarding the use of acupuncture for oncological symptom relief. He and fellow researchers have followed that first publication with further reviews describing the results of ten other studies on the use of acupuncture. They noted that in 2010 there were three randomized clinical trials reported in the Journal of Clinical Oncology alone, indicating that acupuncture should no longer be considered a mere complementary therapy in the milieu of cancer symptom management. Johnstone also pointed out recent changes to Medicare should make acupuncture more accessible for those patients with chronic illness or symptomatology who could not access this treatment modality in the past.
Donald et al. [21] reported the outcome of their pilot study in patients with peripheral neuropathy. Their sample included 17 patients with a diagnosis of chemotherapy-induced peripheral neuropathy (PN) who received 6 weeks of acupuncture and 85 % of those patients reported improved neuropathy symptoms. Only 18 % reported no change. Forty-seven percent, or nearly half of the sample reported additional benefits, including increased sleep and relaxation. The authors suggest their findings support more studies on the efficacy of acupuncture for PN.
In a 2011 Cochrane review of acupuncture-point stimulation for chemotherapy-induced nausea or vomiting, Ezzo et al. [22] pooled 11 studies and found overall that acupuncture-point stimulation of all methods combined reduced the incidence of acute vomiting, but not acute or delayed nausea severity compared with the control. Acupuncture findings related to nausea and vomiting were used by Gilmour et al. [23] to illuminate the importance of health care providers’ knowledge of CAM therapies when assisting parents to make decisions regarding the care of their child with life-threatening cancer diagnoses. In a 2009 report, Bennet et al. [24] suggested health care providers give their older patients information related to CAM therapies because this age group may not have access to as much information as a younger demographic.
Finally, in 2011, Paley et al. [25] provided a Cochrane systematic review regarding the use of acupuncture for cancer pain in adults. The authors concluded only three studies met their inclusion criteria. Of these, only one was judged to be of high methodological quality. That single study revealed auricular acupuncture reduced cancer-related pain compared with auricular acupuncture at non-acupuncture points. The reviewers discovered methodological design flaws and potential bias as reasons to conclude there was insufficient evidence to judge whether acupuncture is effective in relieving cancer-related pain in adults [25].
In conclusion, the literature supports the use of acupuncture for cancer-related pain in part, but there are concerns related to methodology and sampling bias. Other CAMs are also showing promise as adjuvants for cancer pain control. Bio-field therapies are one such CAM and while the evidence for the effectiveness of such therapies is not as robust, there is more evidence available regarding its reported benefits.
Bio-field Therapies and Cancer Pain
Bio-field therapies interact with energy fields that surround and penetrate the body. The more common bio-field therapies are reiki, healing touch, cranial stimulation, and qi gong. The Society for Integrative Oncology (SIO) recommends bio-field or energy therapies because they are safe, but stop short of encouraging their use for cancer patients listing limited evidence on efficacy as their rationale [15]. This category of therapy views the person as a physical, emotional, mental and spiritual being and the practitioner/s use their hands either on or above the individual’s body to direct healing energy to facilitate general health and well-being through modification of the energy field [26].
One year after the publication of the SIO report, Jackson et al. [27] published a literature review related to therapeutic touch, which is defined as “an energy therapy involving hand movements to equalize and balance energy flow” (p. 113). Healing is thought to occur when the body’s energy is balanced. These authors found 12 studies specifically related to therapeutic touch for review. One of the articles was a level I, four were level II, one was level III and the rest were level IV or higher. They conclude that the literature reviewed supported the use of therapeutic touch to reduce pain and anxiety in patients with cancer [27].
Most recently, Anderson and Taylor [26] utilized broader search criteria regarding bio-field therapies and searched the literature for studies that included reiki, therapeutic touch, healing touch, Johrei, and polarity therapy. In their search for clinical evidence on the efficacy of these therapies, they list methodological shortcomings such as small sample size, inadequate levels of blinding and moderate overall quality as limitations to the review and potential incompleteness of the evidence. They also question the possibility of publication bias because there were no negative study findings available for review. However, in spite of the critical review provided, they conclude that more research is required to prove or support the potential clinical effectiveness of bio-field therapies for patients with cancer pain. Additionally, they point out to the reader that while there may be methodological difficulties with this treatment modality, there are no known adverse effects for those patients receiving biotherapies.
Massage Therapy and Cancer Pain
Similar to earlier recommendations for bio-energy therapies in the treatment of anxiety and pain, massage therapy is recommended by the SIO [15] for patients experiencing those same symptoms (p. 73). The SIO cautions against the use of deep or intense pressure near cancer lesions or enlarged lymph nodes or anatomic distortions (postoperative changes) or in patients with bleeding tendencies, however.
Falkensteiner et al. [28] conducted a review of significant databases and found six appropriate articles to review related to the use of massage in patients with a cancer diagnosis (four level I and two level III). The authors found that massage therapy can achieve a reduction of pain lasting up to 18 h, and while they were not able to identify a statistically significant drop in the consumption of analgesics for pain they did note that the dosage of analgesics did not fluctuate as much in the study participants (p. 3). This review supports the use of massage therapy for reducing anxiety, provided of course that the patient can accept close physical contact (p. 6). Finally, massage was shown to have a favorable influence on depression as well. In summary, they found that massage therapy was effective in reducing the subjectively perceived symptoms of pain in oncology patients receiving palliative care (p. 7).
Using the case reporting method, similar findings were reported by Cunningham et al. [29] in a single participant report regarding the use of manual therapy (massage) for a patient with chemotherapy-induced peripheral neuropathy (CIPN). CIPN symptoms include tingling, hypersensitivity, weakness in hands and feet, along with peeling of the skin and difficulty maintaining body temperature. After a 6-week course of manual therapy (massage) given in three sessions per week, the CIPN symptoms were reduced from grade 2 to grade 1. The patient reported dramatic reductions in tingling and numbness in all four extremities, complete resolution of pain, and his extremities were warm for the first time since beginning chemotherapy, with corresponding improvement in quality of life (p. 1475). Other types of stimulation are known to reduce pain, including cranial, music and foot baths.
Cranial Stimulation, Music Therapy, and Foot Baths for Cancer Pain
In an effort to determine the effectiveness of cranial stimulation for symptom management in breast cancer patients, Lyon et al. [30] provided cranial electrical stimulators (CES) to the intervention arm of their pilot study. While they were able to show that levels of depression were lower in the intervention arm, the differences were not statistically significant.
The SIO [15] recommends music therapy as useful but commented on the paucity of research (p. 73) related to the topic. Since that time, Li et al. [31] reported evidence that music therapy is effective. China has the largest number of breast cancer diagnoses in the world. As a result of mastectomies, Chinese women typically develop chronic pain (20–50 %). In a randomized clinical study, these researchers were able to show statistically significant pain reduction in women with radical mastectomies using music therapy [31].
More recently, music therapy was used to reduce pain and anxiety in children with cancer undergoing lumbar puncture [32]. The results of this study indicated music reduced pain scores, heart rate, respiratory rate and anxiety scores for the 20 children in the intervention group.
Yamamoto and Nagata [33] implemented a wrapped, warm foot-bed (WWF) treatment for Japanese patients with incurable cancer to assess the effect of this therapy to induce relaxation. They found this intervention significantly reduced cortisol levels (saliva), provided significant pain relief, and allowed for relaxation in their treatment group.
Conclusions
While the recommendations from research reports are varied, researchers from around the world are beginning to learn more about methodology and protocol in order to further expand the evidence related to complementary and alternative therapies for the treatment of cancer pain. In general, while more level I and II studies are being conducted, this review points out the importance of continued exploration of CAM interventions using rigorous methodologies (see Table 2).
The Consortium of Academic Health Centers for Integrative Medicine is an example of the momentum present in the scientific and practice communities to improve the quality of research and enhance patient care [34]. Other resources include the OncoRx data base. This repository provides information regarding anticancer drug interactions with complementary and alternative medicines used in cancer treatment [35]. The Society for Integrative Oncology’s purpose is to encourage scientific evaluation, dissemination of evidence based information and appropriate clinical integration of complementary therapies in to the practice of integrative oncology (2007).
For the 1,638,910 new cancer patients that are expected to be diagnosed in 2012, and for the 75–90 % of them who will experience pain sometime during their illness, it is incumbent upon scientists and practitioners to work together to develop and evaluate interventions that address cancer related pain and thereby improve the quality of each patient’s life.
References
Papers of particular interest, published recently, have been highlighted as: •• Of importance
American Cancer Society. Cancer Facts & Figures 2012. Atlanta: American Cancer Society; 2012. http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-031941.pdf.
International Association for the Study of Pain. (2011). IASP Taxonomy. http://www.iasp-pain.org/Content/NavigationMenu/GeneralResourceLinks/PainDefinitions/default.htm.
NCCN Clinical Practice Guidelines in Oncology. (2010). Adult cancer pain. J Natl Compr Canc Netw 8(9). http://www.nccn.org/JNCCN/toc/2010september.asp#adult.
Fayed, L. (2009). About cancer: Cancer pain. http://cancer.about.com/od/endoflifeissues/a/cancerpaintypes.htm.
Induru RR, Lagman RL. Managing cancer pain: frequently asked questions. Cleve Clin J Med. 2011;78(7):449–64.
Portenoy RK. Treatment of cancer pain. Lancet. 2011;377(9784):2236–47.
World Health Organization. (2011). WHO’s pain relief ladder. http://www.who.int/cancer/palliative/painladder/en/.
Bardia A, Barton DL, Prokop LJ, Bauer BA, Moynihan TJ. Efficacy of complementary and alternative medicine therapies in relieving cancer pain: a systematic review. J Clin Oncol. 2006;24(34):5457–64.
Cassileth B, Trevisan C, Gubili J. Complementary therapies for cancer pain. Curr Pain Headache Rep. 2007;11(4):265–9. doi:10.1007/s11916-007-0202-8.
Pujol L, Monti D. Managing cancer pain with nonpharmacologic and complementary therapies. J Am Osteopath Assoc. 2007;107(12 Suppl 7):ES15-21.
Kassab S, Cummings M, Berkovitz S, et al. Homeopathic medicines for adverse effects of cancer treatments. Cochrane Database Syst Rev. 2009;(2):CD0048455. doi:10.1002/14651858.CD004845.pub2.
Landier W, Tse AM. Use of complementary and alternative medical interventions for the management of procedure-related pain, anxiety, and distress in pediatric oncology: an integrative review. J Pediatr Nurs. 2010;25(6):566–79.
Cassileth BR, Keefe FJ. Integrative and behavioral approaches to the treatment of cancer-related neuropathic pain. Oncologist. 2010;15(Suppl 2):19–23.
•• Running A, Turnbeaugh E. Oncology pain and complementary therapy. Clin J Oncol Nurs. 2011;15(4):374–9. This article reviews evidence related to the use of CAM therapies for oncology pain.
Deng GE, et al. Integrative oncology practice guidelines. J Soc Integr Oncol. 2007;5(2):65–84. doi:10.2310/7200.2007.002.
O’Regan D, Filshie J. Acupuncture and cancer. Auton Neurosci. 2010;157(1–2):96–100.
Paley CA, Johnson JI, Bennett MI. Should physiotherapists use acupuncture for treating patients with cancer-induced bone pain? A discussion paper. Physiotherapy. 2011;97(2011):256–63. doi:10.1016/j.physio.2010.08.008.
•• Hopkins-Hollis AS. Acupuncture as a treatment modality for the management of cancer pain: the state of the science. Oncol Nurs Forum. 2010;37(5):E344–348. This manuscript reviews recent evidence related to the use of acupuncture for cancer pain.
Bao T, Ye X, Skinner J, Cao B, Fisher J, Nesbit S, Grossman SA. The analgesic effect of magnetic acupressure in cancer patients undergoing bone marrow aspiration and biopsy: a randomized, blinded, controlled trial. J Pain Symptom Manage. 2011;41(6):995–1002. doi:10.1016/j.jpainsymman.2010.08.012.
Johnstone PAS. Acupuncture as cancer symptom therapy: what a difference a decade makes. J Acupunct Meridian Stud. 2011;4(4):209–13. doi:10.1016/j.jams.2011.09.011.
Donald G, Tobin I, Stringer J. Evaluation of acupuncture in the management of chemotherapy-induced peripheral neuropathy. Acupunct Med. 2011;29(3):230–3. doi:10.1136/acupmed.2011.0100265.
Ezzo JM et al. Acupuncture-point stimulation for chemotherapy-induced nausea or vomiting. Cochrane Database Syst Rev. 2006;(2):CD002285. doi:10.1002/14651858.CD002285.pub2.
Gilmour J, Harrison C, Asadi L, Cohen MH, Vohra S. Informed consent: advising patients and parents about complementary and alternative medicine therapies. Pediatrics. 2011;128(4):S187–92. doi:10.1542/peds.2010-2720H.
Bennett JA, Cameron LD, Whitehead LC, Porter D. Differences between older and younger cancer survivors in seeking cancer information and using complementary/alternative medicine. J Gen Intern Med. 2009;24(10):1089–94. doi:10.1007/s11606-009-0979-8.
Paley CA, Johnson MI, Tahsani OA, Bagnall AM. Acupuncture for cancer pain in adults. Cochrane Database Syst Rev. 2011;(1):CD007753. doi:10.1002/14651858.
•• Anderson JG, Taylor AG. Bio-field therapies and cancer pain. Clin J Oncol Nurs. 2012;16(1):43–8. This manuscript reviews recent evidence related to the use of bio-field therapies for cancer pain.
Jackson E, Kelley M, McNeil P, Meyer E, Schlegel L, Eaton M. Does therapeutic touch help reduce pain and anxiety in patients with cancer? Clin J Oncol Nurs. 2008;12(1):113–20.
Falkensteiner M, Mantovan F, Muller I, Them C. The use of massage therapy for reducing pain, anxiety, and depression in oncological palliative care patients: a narrative review of the literature. ISRN Nurs. 2011;2011:929868. doi:10.5402/2011/929868.
Cunningham JE, Kelechi T, Sterba K, et al. Case report of a patient with chemotherapy-induced peripheral neuropathy treated with manual therapy (massage). Support Care Cancer. 2011;19(9):1473–6.
Lyon DE, Schubert C, Taylor AG. Pilot study of cranial stimulation for symptom management in breast cancer. Oncol Nurs Forum. 2010;37(4):476–83.
Li X-M, Yan H, Zhou K-N, Dang S-N, Wang D-L, Zhang Y-P. Effects of music therapy on pain among female breast cancer patients after radical mastectomy: results from a randomized controlled trial. Breast Cancer Res Treat. 2010;128:411–9. doi:10.1007/s10549-011-1533-z.
Nguyen TN, Nilsson S, Hellsrom A, Bengtson A. Music therapy to reduce pain and anxiety in children with cancer undergoing lumbar puncture: a randomized clinical trial. J Pediatr Oncol Nurs. 2012;27(3):146–55. doi:101177/1043454209355983.
Yamamoto K, Nagata S. Physiological and psychological evaluation of the wrapped warm footbath as a complementary nursing therapy to induce relaxation in hospitalized patients with incurable cancer a pilot study. Cancer Nurs. 2011;34(3):185–92. doi:10.1097/NCC.0b013e3181fe4d2d.
Ali A, Vitulano LA. A brief report: Yale Research Symposium on Complementary and Integrative Medicine. Yale J Biol Med. 2010;83(3):123–5.
Yap KY-L, Kuo EY, Lee JJJ, Chui WK, Chan A. An onco-informatics database for anticancer drug interactions with complementary and alternative medicines used in cancer treatment and supportive care: an overview of the OncoRx project. Support Care Cancer. 2010;18(7):883–91. doi:10.1007/s00520-009-0729-9.
Disclosures
No conflicts of interest relevant to this article were reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Running, A., Seright, T. Integrative Oncology: Managing Cancer Pain with Complementary and Alternative Therapies. Curr Pain Headache Rep 16, 325–331 (2012). https://doi.org/10.1007/s11916-012-0275-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11916-012-0275-x