Abstract
Purpose of review
This review summarizes recently published data on the effects of pregnancy and lactation on bone structure, mechanical properties, and mechano-responsiveness in an effort to elucidate how the balance between the structural and metabolic functions of the skeleton is achieved during these physiological processes.
Recent findings
While pregnancy and lactation induce significant changes in bone density and structure to provide calcium for fetal/infant growth, the maternal physiology also comprises several innate compensatory mechanisms that allow for the maintenance of skeletal mechanical integrity. Both clinical and animal studies suggest that pregnancy and lactation lead to adaptations in cortical bone structure to allow for rapid calcium release from the trabecular compartment while maintaining whole bone stiffness and strength. Moreover, extents of lactation-induced bone loss and weaning-induced recovery are highly dependent on a given bone’s load-bearing function, resulting in better protection of the mechanical integrity at critical load-bearing sites. The recent discovery of lactation-induced osteocytic perilacunar/canalicular remodeling (PLR) indicates a new means for osteocytes to modulate mineral homeostasis and tissue-level mechanical properties of the maternal skeleton. Furthermore, lactation-induced PLR may also play an important role in maintaining the maternal skeleton’s load-bearing capacity by altering osteocyte’s microenvironment and modulating the transmission of anabolic mechanical signals to osteocytes.
Summary
Both clinical and animal studies show that parity and lactation have no adverse, or a positive effect on bone strength later in life. The skeletal effects during pregnancy and lactation reflect an optimized balance between the mechanical and metabolic functions of the skeleton.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Worldwide, approximately 165 million women per year become pregnant; of which, at least 40% go on to breastfeed their infants for at least 6 months [1]. The health benefits of breastfeeding for newborns are well documented: breastfeeding has been associated with improved maternal health, including decreased risk of hemorrhage after delivery and reduced long-term risk of developing breast and ovarian cancers and type II diabetes [2]. As a result of these purported benefits to both the mother and child, public health initiatives have aimed to increase breastfeeding rates. Most notably, in 2012, the World Health Organization set a goal to increase the rate of exclusive breastfeeding for the first 6 months to at least 50% worldwide by 2025 as part of its Comprehensive Implementation Plan on Maternal, Infant and Young Child Nutrition [3].
Skeletal Effects of Pregnancy and Lactation
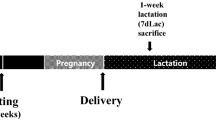
The maternal skeleton serves as an important source of calcium for fetal/infant bone growth and undergoes substantial reduction in bone mass during pregnancy and lactation. Notably, the reproductive process requires large quantities of calcium, as a growing fetus needs 60–350 mg of calcium per day (depending on gestational stage), and a breastfeeding infant needs an average of 200 mg of calcium per day to support healthy bone growth [4•]. Assuming a normal efficiency of intestinal absorption, an additional 1200 mg/day would be needed to meet the calcium requirement for pregnant women in the third trimester and an additional 800 mg/day for lactating women in the first 6 months [4•]. However, the actual calcium intakes for American and Canadian women between age 18 and 50 range from 800 to 1000 mg/day [5]. As a result, alternate mechanisms are activated during reproduction to meet this increased calcium demand, including increased intestinal absorption of calcium, alterations in the rate of renal calcium excretion, and, importantly, skeletal resorption [4•]. Thus, the mineral delivery to the fetus and production of breast milk required to support a growing infant has the potential to place significant strain on the maternal skeleton. In fact, the resulting bone resorption can lead to 1–4% decline in areal bone mineral density (aBMD) during pregnancy [6,7,8,9]. Moreover, lactation can result in up to 1–1.5% decreases in aBMD per month [10,11,12,13], which is substantially higher than the average rate of post-menopausal bone loss of 1–2% decrease in aBMD per year [14]. This bone loss is largely mediated through osteoclast resorption [15,16,17, 18•]. In addition, several groups have also demonstrated that osteocytes are able to remodel their pericellular matrix and alter the osteocytic lacunar and canalicular void spaces during lactation [19, 20, 21•]. This osteocyte-based perilacunar/canalicular remodeling (PLR) has the potential to directly alter bone tissue mineral density and material properties [21•] and has been hypothesized to be an important factor in the skeleton’s metabolic role in maintaining calcium homeostasis [22].
The precise endocrine signals responsible for pregnancy- and lactation-associated alterations in calcium metabolism are not fully understood [4•]. Throughout the course of pregnancy, women show dramatic elevations in serum estradiol and prolactin. Furthermore, progesterone levels are elevated during pregnancy, while serum levels of follicle-stimulating hormone and luteinizing hormone are depressed [23]. In addition to the dramatic changes in sex hormones, pregnancy also induces a slight reduction in levels of parathyroid hormone (PTH) during the first two trimesters, after which PTH levels return to normal [4•]. Serum levels of calcitriol are also generally elevated during pregnancy, which likely plays a role in the increase in intestinal calcium absorption. Finally, levels of parathyroid hormone-related protein (PTHrP) increase gradually throughout the course of pregnancy [4•]. The major factors mediating lactation-associated bone loss appear to be estradiol and PTHrP. During lactation, serum levels of estradiol have been shown to be lower while levels of PTHrP are elevated [4•]. Both factors contribute to the increased bone resorption that takes place during lactation [16, 24]. However, although a rodent study that simultaneously induced low levels of serum estradiol (through ovariectomy) and high levels of PTHrP (through continuous PTHrP infusion) showed that this combination led to increased rates of bone resorption compared with either factor alone, the total extent of bone loss remained lower than that which occurs during lactation [25]. Thus, other factors, such as elevated levels of prolactin and FGF-21, are likely also involved in mediating lactation bone loss [26, 27].
Skeletal Effects of Post-weaning Recovery
After weaning, hormone levels return to normal: in particular, serum levels of PTHrP decrease, while estradiol increases to normal [4•, 28]. In addition, immediately after weaning, osteoclasts undergo high rates of inactivation and apoptosis, the expression of receptor activator of nuclear factor-κB ligand (RANKL) is reduced, and the bone resorption process is slowed down [29, 30]. The skeleton then enters an anabolic phase, where osteoblast numbers and the bone formation rate are significantly elevated [31, 32]. Osteocyte PLR is also stopped after weaning, and osteocytes begin to deposit minerals on the perilacunar/canalicular surfaces [19, 21•]. Taken together, the dramatically altered activities of osteoblasts, osteoclasts, and osteocytes following weaning lead to a significant increase in bone mass [4•].
Purpose of this Review
During reproduction, as well as throughout an organism’s lifespan, the skeleton forms an important reservoir for minerals, notably calcium and phosphorus, which can be accessed to allow the body to maintain homeostasis. However, despite these important metabolic functions, the skeleton’s primary role is mechanical, as the structure provided by the bones is critical to nearly all aspects of an organism’s daily function. Bones such as the skull and ribs form vital protection for soft tissues, including the brain, heart, and lungs. The long bones also provide a resistance against which muscles can contract to allow for movement. Thus, together with other tissues of the musculoskeletal system, the bones play a crucial role in locomotion. The proper functioning of the skeleton in each of these diverse roles is critical for an organism’s survival. As a result, the skeleton’s structural and metabolic roles must be balanced throughout the lifespan.
The purpose of this review is to summarize recently published data on structural and mechanical adaptations of the skeleton in response to the metabolic challenges and hormonal effects of pregnancy and lactation. Until recently, the majority of clinical and animal studies used dual energy X-ray absorptiometry (DXA) for assessment of skeletal alterations during reproduction. However, DXA-derived areal bone mineral density (aBMD) is influenced by bone size [33,34,35] and cannot assess bone microarchitecture [36,37,38,39], an important determinant of bone strength. Pregnancy and lactation could alter the cortical and trabecular bone structure and bone mass in opposite directions, resulting in unchanged total aBMD. Also, increase/decrease in bone size may lead to over/under-estimation of aBMD by DXA. As a result, the precise impacts of reproduction on maternal skeletal health remain unclear. This review will mainly report recent findings on the effects of pregnancy and lactation on three-dimensional (3D) bone mass and bone structure, and bone mechanical properties derived from biomechanical testing or image-based computational simulation, in an effort to elucidate how the balance between the structural and metabolic functions of the skeleton are achieved in the face of reproduction-associated metabolic challenges.
This is not a systematic review of the literature on the skeletal and mineral physiology during reproduction and lactation (a comprehensive review on this topic has been provided by Kovacs [4•]), but rather, an introduction of a structural and mechanical perspective to the maternal mineral homeostasis through discussion of recent experimental and clinical studies. Due to space limitations, the review focuses on discoveries within the past 10 years (2010–2019).
Effects of Pregnancy and Lactation on Maternal Bone Structure and Mechanics
Changes in Bone Structure and Mechanics during Pregnancy
There are limited human data on changes in bone structure or mechanics during pregnancy, due to the concerns of fetal radiation exposure. By measuring a time-point before planned pregnancy and 1–6 weeks after delivery, results of aBMD indicate small but significant reductions in bone mass during pregnancy, although the extent of pregnancy-related bone loss in women appears to be variable and may be dependent on dietary calcium intake [4•]. Quantitative ultrasound (QUS) is an alternative imaging method that measures the effects of the bone on the velocity and attenuation of the sound waves, resulting in an indirect quantification of bone tissue mechanics, structure, and quantity. Longitudinal studies using QUS at the calcaneus have found decreased bone density and stiffness index, a parameter calculated based on ultrasound attenuation and speed of sound, during the second to third trimester transition [40, 41]. However, the correlation of the changes at the heel to other skeletal sites such as the spine and hip is unclear.
The animal data based on histomorphometry and DXA from earlier studies have been inconsistent [4•]. Moreover, the extent of bone changes may be highly dependent on animal species, genetic background, and skeletal sites. Only a limited number of studies assessed the effect of pregnancy on the three-dimensional (3D) bone microstructure and bone mechanical properties. Korecki et al. found that C57BL/6 mice had significantly greater trabecular bone volume fraction (BV/TV) at the distal femur, cortical area (Ct.Ar) at the midshaft, and ultimate load by 3-point bending at day 16 of pregnancy compared with day 9 [42] (rodents typically undergo 21 days of pregnancy). However, the extent of pregnancy-associated changes in comparison with pre-pregnancy or virgins was not clear. Vajda et al. compared mechanical properties of rat bone at the end of pregnancy with virgin controls and found no difference between groups in failure load of the vertebra by compression or femur by 3-point bending [43]. De Bakker et al. reported the first longitudinal data on bone microstructure and mechanical properties throughout multiple pregnancies in the rat tibia [44•]. Their results showed that during the first pregnancy, trabecular bone changed minimally during the first 14 days of pregnancy, but underwent more than 40% loss in BV/TV through trabecular thinning and reductions in trabecular number and connectivity between days 14 and 21. In contrast to the first cycle, two subsequent reproductive cycles revealed minimal changes in trabecular bone microstructure during the pregnancy phase. On the other hand, cortical thickness (Ct.Th), Ct.Ar, and polar moment of inertia (pMOI) at the tibia increased significantly during pregnancy in all three reproductive cycles. As a result, the axial whole bone stiffness estimated by finite element analysis of an unconfined compression test did not change over pregnancy in any of three reproductive cycles [44•].
In summary, the limited data from pregnant women indicate a modest decline in bone mass and stiffness index. However, pregnancy-associated fracture is extremely rare and women who do fracture during pregnancy may be exposed to secondary cause of bone disorders [45]. Meanwhile, animal data suggest that while skeletal alterations during pregnancy may lead to reduction in trabecular bone, concurrent increases in cortical bone appear to result in unchanged bone stiffness.
Changes in Bone Structure and Mechanics during Lactation
Numerous studies have reported significant declines in aBMD in women during breastfeeding [4•]. A longitudinal study analyzed hip geometry based on images from DXA scans and reported 1–3% decrease in the cross-sectional area of femoral neck, intertrochanter, and shaft, as well as 2% decreases in the derived femoral strength parameters such as intertrochanter section modulus and shaft buckling ratio [46]. Peripheral QUS has also been used to assess lactation-induced bone changes but did not detect bone loss at the calcaneus [40, 47] or mid-tibial shaft [48]. Recently, the development of high-resolution peripheral quantitative computed tomography (HR-pQCT) has enabled the low-dose assessment of bone microstructure and mechanical properties at the distal radius and distal tibia. A few recent studies using HR-pQCT confirmed 0–2% reduction in both cortical and trabecular bone compartments [49,50,51,52,53]. Bjornerem et al. reported reduced trabecular BV/TV and trabecular number (Tb.N) with increased trabecular thickness (Tb.Th) and separation (Tb.Sp) in lactating women. Additionally, cortical porosity (Ct.Po) increased while the degree of mineralization decreased [50]. However, to what extent the whole bone mechanics would be altered in response to lactation is unclear.
Studies of mouse bone microstructure by μCT indicated that, after 3 weeks of lactation, mice have 30–50% lower BV/TV than virgins at the skeletal sites with abundant trabecular bone, such as the lumbar spine, proximal tibia, and distal femur. Compared with virgins, lactating mice also have lower Tb.N, Tb.Th, trabecular connectivity density (Conn.D), plate-like trabeculae, and tissue mineral density (TMD) [25, 27, 29, 54]. As a result, whole bone stiffness was 60–70% lower in the lactating vs. virgin mice [54]. Similar results have also been reported in rats [18•, 44•]. An in vivo μCT study by de Bakker et al. found a 73% reduction in BV/TV and a significant decline in Tb.N, Tb.Th, Conn.D, and plate-like trabeculae at the proximal tibia over a 3-week lactation period during the first reproductive cycle in rats [44•]. Interestingly, in two subsequent reproductive cycles, trabecular bone loss in response to lactation reduced to 40–50% due to trabecular thinning while all other trabecular microstructure parameters remained unchanged. Moreover, Ct.Th, Ct.Area, and pMOI decreased significantly at the proximal tibia during lactation in all three reproductive cycles. As a result, whole bone stiffness declined more than 30% during lactation in the first reproductive cycle and ~ 15% in the subsequent cycles. For the lumbar vertebrae, two studies conducted compression tests and reported 50–60% reduction in peak load of the vertebra in lactating rats as compared with virgins [18•, 43]. At the predominantly cortical bone sites such as tibial and femoral midshafts, effects of lactation are less pronounced but remain significant, as lactating rodents have 13–30% reduced Ct.Th and Ct.Area, ~ 5% reduced Ct.TMD and 15–36% greater Ct.Po and endosteal perimeter than virgins [27, 29, 54, 55]. Three-point bending tests of both mouse and rat cortical bone also suggest reduced ultimate load and stiffness during lactation [42, 43, 56].
Two recent studies have investigated the changes in material properties of bone tissue in response to lactation. By performing micro-indentation tests, Kaya et al. discovered that the local elastic modulus of the mouse femur cortex was reduced 10–13% during lactation, which was likely caused by the 7% and 15% increases in the volumes of osteocyte lacunar and canalicular void space, respectively [21•]. De Bakker et al. conducted nano-indentation tests on rat vertebral trabecular bone and reported that tissue modulus at the nano-scale decreased significantly during lactation at both the center and surface of trabeculae [18•].
Both human and animal data suggest that compared with the pregnancy period, lactation results in more substantial bone loss, bone microstructure deterioration, and reduction in bone mechanical properties. Although lactation-associated fracture is uncommon, the transient decline in bone strength may result in a higher risk of fracture during breastfeeding in women with low bone mass or skeletal fragility prior to pregnancy.
Changes in Bone Structure and Mechanics Post-weaning
Many studies have documented that women undergo substantial increases in aBMD at the total body, lumbar spine, and hip after weaning [4•]. However, whether or not the lactation-associated skeletal alteration is completely reversible is still debated. The inconsistency between DXA data could come from discrepancies in the duration of lactation, duration of post-weaning recovery, and skeletal sites that were measured. HR-pQCT studies of the distal radius and tibia also suggest an anabolic period in both the cortical and trabecular compartments after weaning. However, the recovery is incomplete at these distal skeletal sites [49,50,51,52]. Bjørnerem et al. reported that a median of 2.6 years after cessation of breastfeeding, skeletal deficits, including Ct.Po, Ct.TMD, Tb.N, and higher Tb.Sp still remained, as compared with pre-breastfeeding [50]. By contrast, hip geometry analysis based on DXA scans suggested that the reduction in femoral cross-sectional area and derived measurements of femoral strength during lactation were completely recovered 6 months after weaning [46]. Wiklund et al. investigated the effects of lactation on bone size and strength 16–20 years after the last parturition and discovered that women who had breastfed for a total of 33 months or more had greater bone size, DXA-derived hip strength index, and pQCT-derived tibial bone strength index than mothers who breastfed less than 12 months [57]. By contrast, Specker et al. reported that high parity was associated with increased femoral neck size and estimated torsional bending strength of the distal radius but found no associations between bone size and breastfeeding duration [58].
Studies using μCT in rodent models revealed full recovery of bone microstructure at some skeletal sites, and permanent alterations at others. In general, trabecular bone in the vertebrae fully recovers its microstructure [18•, 29, 54], whole bone stiffness [18•, 43, 54], and maximal load [43] 2–4 weeks after weaning, while the metaphasis of the tibia and femur still have lower trabecular volume, number, and connectivity as well as 20–30% lower whole bone stiffness when compared with pre-lactation or virgin controls [18•, 27, 54, 56]. A longitudinal μCT study investigated the capacity of bone recovery after weaning during multiple reproductive cycles at the rat proximal tibia [44•] and found that BV/TV recovers incompletely during the first cycle while Tb.Th fully recovers to pre-pregnancy levels. By contrast, Tb.N, Tb.Sp, and plate-likeness of trabeculae show no recovery and remain unchanged compared with their post-lactation values for up to 6 weeks after weaning during the first cycle. During subsequent reproductive cycles, BV/TV fully recovers to the pre-pregnancy level of each cycle but remains lower than the pre-pregnancy level of the first cycle. By contrast, increases in Tb.Th during the subsequent cycles lead to a greater Tb.Th at the end of the third reproductive cycle when compared with both baseline and age-matched virgin controls. Cortical bone at the proximal tibia recovers fully during all three reproductive cycles. In fact, the combined effects of 3 reproductive cycles appear to lead to increased robustness of cortical bone, as the pMOI, Ct.Th, and Ct.Area were greater in rats after 3 reproductive cycles than the age-matched virgins. Whole bone stiffness has incomplete post-weaning recovery during the first and second cycles but recovers fully to the same level of baseline and virgin controls by the end of the third cycle [44•].
At the tibial and femoral midshaft, despite the recovery of cortical structure after weaning, most studies report that one or more cortical properties such as Ct.Th, Ct.Area, Ct.TMD, and Ct.Po remain inferior in post-weaning mice or rats than virgins [29, 54,55,56, 59]. Intriguingly, three-point bending tests of both mouse and rat bone indicate that ultimate load and stiffness are fully recovered post-weaning when compared with virgin controls [43, 56]. This suggests that tissue intrinsic mechanical properties may be enhanced in post-lactation bone. Micro- and nano-scale evaluations of bone material properties also indicate complete recovery of bone mechanics post-weaning. One week after weaning, volumes of osteocyte lacunar and canalicular void space and elastic modulus of the mouse femur cortex tested by micro-indentation returned to the same level as the virgin controls [21•]. Moreover, nano-indentation tests suggest that, by 6 weeks post-weaning, the elastic modulus of the central region of trabeculae at the rat lumbar vertebra recovers to the same level of virgin controls [18•].
Both human and animal studies demonstrate a remarkable anabolic response following cessation of lactation, which leads to recovery of bone mass and bone microstructure to different degrees, depending on the skeletal sites (central vs. appendicular) and compartments (trabecular vs. cortical). Intriguingly, the majority of studies show complete recovery of bone mechanical properties from nano-scale to the whole bone level after one or multiple reproductive cycles. These results of bone mechanics support the clinical findings that lactation generally confers a long-term neutral or protective effect on future risk of fractures [4•].
Mechanical Regulation of Site-Dependent Changes in Maternal Bone during Reproduction and Lactation
In the previous section, we reviewed the literature in the field which suggests that the extent of reproductive bone loss and recovery varies depending on the skeletal site, with the trabecular regions in particular showing incomplete recovery after weaning. However, while both clinical and animal studies suggest that reproduction and lactation may cause permanent alterations in skeletal structure, multiple clinical investigations also indicate that reproduction is not associated with increased risk of post-menopausal osteoporosis or fracture. Taken together, these findings lead us to hypothesize that the degree to which a given skeletal site/compartment is involved in physiological load-bearing may play a role in determining its response to reproduction and lactation.
De Bakker et al. compared the extent of lactation-induced bone loss and weaning-induced recovery between the lumbar spine and proximal tibia during a single reproductive cycle in rats [18•]. Compared with the tibia, trabecular bone at the lumbar vertebra plays a more critical load-bearing function, as the trabecular load-share fraction (defined as the proportion of the total load that is borne by the trabecular compartment) is 32% in the proximal tibia vs. 55% in the vertebra prior to reproduction. μCT analysis revealed that the extent of the deterioration in trabecular microstructure and resumption of its load-bearing function after weaning differed substantially between the two locations. At the tibia, there was a dramatic deterioration of trabecular bone microstructure during pregnancy as well as lactation. In contrast to this, at the lumbar vertebra, where the trabecular bone bears a substantially greater share of the total applied load, there was minimal deterioration of the trabecular network integrity, including number and connectivity of trabeculae. Differences in the two skeletal sites continued post-weaning. Although both sites showed dramatically elevated bone formation activities after weaning, the post-weaning bone formation rate was significantly higher at the vertebra than the proximal tibia. As a result, the trabecular bone at the vertebra showed only a transient reduction in load-share fraction during reproduction and resumed its full load-bearing function after weaning. By contrast, the tibial trabecular load-share fraction was not restored at the end of the post-weaning period [18•]. Because pregnancy and lactation are physiological processes, the differential trabecular response to these natural events at the lumbar vertebra vs. the tibia may indicate differences in the extent of the trabecular bone’s structural vs. metabolic functions at these two locations. Similar results of the lactation-associated bone loss and post-weaning recovery at the vertebra and tibia/femur have also been demonstrated in mice [18•, 27, 29, 54, 56]. Furthermore, clinical studies suggest that the post-weaning recovery of bone mass is greater at the spine than the long bones [4•, 13, 49, 60]. A recent HR-pQCT study showed that at 6 months after weaning, there were no deficits at the distal tibia, while persistent reductions in trabecular bone at the distal radius remained, further demonstrating that weight-bearing may mitigate lactation-associated bone loss [52, 53].
The trabecular bone at skeletal sites that undergo irreversible bone loss during reproduction may play more of a metabolic, rather than a mechanical role. This would allow for permanent alterations in trabecular structure at such sites without increasing risk of fracture. Studies of skeletal biology in egg-laying birds further support this possibility. Female birds undergo a high demand for calcium during the egg-laying period and are known to generate a highly metabolically active bone, termed “medullary bone” within the medullary cavities of certain long bones. This medullary bone is a rapidly formed woven bone that provides calcium needed for egg shell formation [61]. In contrast to cortical and trabecular bone, medullary bone is often formed in isolated clusters and does not appear to contribute substantially to bone mechanics [61] and thus is thought to play a primarily metabolic role. Although the mammalian skeleton does not contain a distinct bone type solely for metabolic functions, it is possible that the trabecular bone in some regions of the skeleton may play a similar role during times of high metabolic need such as reproduction. This is particularly likely in trabecular regions that are surrounded by thick cortices that are able to maintain the majority of the bone’s mechanical function, as the permanent deficit in trabecular bone during reproduction at such sites may be compensated by improved cortical bone structure. A longitudinal μCT study suggested that rat cortical bone at the proximal tibia becomes more robust and carries a greater percentage of load after three cycles of reproduction, which compensates for the permanent deficit and reduced load-bearing capacity of trabecular bone, resulting in unchanged whole bone stiffness [44•].
The balance between the mechanical vs. metabolic role of the skeleton is further demonstrated by alterations in the rodent femoral midshaft in response to lactation. Cortical structure of the femur midshaft deteriorates during lactation and remains lower in Ct.Area and pMOI post-weaning when compared with virgins [29, 54,55,56, 59]. However, improvements in intrinsic tissue mechanical properties appear to compensate for the structural deficit, resulting in no difference in femoral stiffness or peak load between post-weaning and virgin bone [43, 56].
The above findings in clinical and animal studies demonstrate that the mechanical integrity of the highly load-bearing regions, such as the vertebral trabecular bone and femur midshaft, is preserved either through maintenance of structural integrity (as in the vertebrae) or improved material properties (as in the femur). It appears that the skeletal system responds to increased calcium demands during pregnancy and lactation by selectively degrading bone structure, resulting in an alternate skeletal composition where bone structure may be optimized at the more load-bearing regions to allow maintenance of similar quality to virgin bone.
Mechano-Responsiveness of Maternal Bone during Pregnancy and Lactation
Bone is a dynamic organ which constantly alters its structure to adapt to the external load. If the structural adaptation during reproduction and lactation reflects the response of bone microstructure and tissue material properties to load-bearing in order to maintain mechanical integrity at the critical load-bearing sites, would maternal bone also have greater response to external loading?
In general, physical activity and exercise during pregnancy and postpartum improve women’s physical and psychological well-being, help with weight management, and reduce the risk of gestational diabetes [62]. However, based on limited evidence from clinical and animal studies, the effects of weight-bearing exercise on bone health during pregnancy and lactation are unclear. In a pilot study, Dimov et al. monitored the stiffness index at the calcaneus by QUS in 8 recreational tennis players and 9 control women who did not participate in any sport during pregnancy [63]. Their results suggest that activity level did not affect the extent of pregnancy-associated bone loss. A study by To et al., which compared changes in the calcaneus by QUS during pregnancy between 24 physically active women and 94 women who did not exercise, yielded the opposite conclusion. Their results suggest that physical activity in pregnancy is significantly associated with a reduced extent of BMD loss during pregnancy [64]. The skeletal response to disuse during pregnancy has also been investigated. Promislow et al. reported that women who were prescribed bed rest had 3-fold greater pregnancy-associated reduction in aBMD between gestational ages of 16 and 36 weeks at the ultra-distal radius than those who were not prescribed bed rest [65].
Weight-bearing exercise may also have the potential to reduce lactation-associated bone loss and augment post-weaning recovery. Lovelady et al. reported that women who were engaged in resistance and aerobic exercise had a significantly smaller lactation-induced decline in aBMD at the lumbar spine when compared with the control group [66]. However, another study by Little et al. comparing lactating women who exercise regularly to sedentary women showed no benefit of exercise on lactation-associated bone loss [67]. An animal study by Hemmatian et al. conducted ex-vivo loading on fibulae from lactating and virgin mice and found greater osteocytic responses in terms of β-catenin expression and Sclerostin suppression in lactating mouse bone, suggesting a greater skeletal response to loading during lactation [68]. Rosa et al. designed a raised cage to force rats to rise to an erect, bipedal stance to obtain food/water during the pregnancy period in order to study the effect of voluntary exercise during pregnancy on post-lactation bone quality [69]. Although they did not observe any benefit of weight-bearing exercise in aBMD measurements by DXA, results of pQCT measurements indicated that exercise reduced trabecular bone loss at the tibial metaphysis and increased the estimated strength index and cross-sectional moment of inertia at the tibial diaphysis at the end of the lactation period. Using a similar rat bipedal stance model, Shea et al. examined the effects of weight-bearing exercise during lactation and over a 6-week post-weaning period on the degree of bone recovery. Their results suggested that a modest increase in skeletal loading significantly augmented the increase in rat femoral BMD and tibial BV/TV 6 weeks after weaning [70].
Additional clinical and animal studies are needed to fully understand maternal bone’s mechano-responsiveness or mechano-sensitivity during pregnancy and lactation. Inclusion of a nulliparous group with and without weight-bearing exercise would help to elucidate whether enhanced mechano-sensitivity is a critical factor that facilitates the structural alterations in maternal bone to maintain an optimized balance between its metabolic and mechanical functions.
Lactation-Induced Osteocytic Perilacunar/Canalicular Remodeling (PLR) and Its Influence on Bone Mechanobiology
The potential interactions between the systematic changes of pregnancy and lactation and skeletal mechano-sensitivity are likely mediated by osteocytes, the primary mechano-sensory cells in bone. In addition to osteoblasts and osteoclasts, osteocytes are also able to directly modulate their surrounding tissue during reproduction, by removing mineral from the surrounding matrix and/or forming new bone tissue on the surfaces of their lacunae [71•, 72]. More recent studies have confirmed that this process of osteocyte PLR occurs in various conditions, most notably during lactation, and is thought to play a role in maintaining mineral homeostasis [19, 20, 21•, 73]. In addition to directly modulating their surrounding mineralized tissue, osteocytes also play critical roles in cell signaling and mechanotransduction. Embedded within the mineralized matrix, osteocytes form a network through the extension of dendritic processes that connects individual osteocytes to one another as well as to the osteoblasts and osteoclasts on the bone surface. This osteocyte network is housed in an equally extensive and highly organized pore system, which consists of the larger ellipsoidal lacunae (~ 10 × 10 × 20 μm) and numerous slender long canaliculi channels (~ 1 μm diameter × 30 μm length) emanating from each lacuna [74]. This lacunar-canalicular system (LCS) surrounding osteocytes plays an import role in osteocyte function: it is the lifeline for osteocytes, supplying nutrients to and removing waste from the cells, and also allows any biological factors released by osteocytes to be transported to their targets in nearby cells. Furthermore, the interstitial fluid flow in the LCS, driven by external mechanical loading, allows the well-positioned osteocytes to sense and respond to their mechanical environment. The fluid and solute transport in the LCS has been extensively studied both theoretically and experimentally in normal cortical bone [74, 75]. Changes in the LCS associated with aging and reduced pericellular matrix density have been found to alter fluid flow in the canaliculi and bone’s sensitivity to anabolic mechanical loading [76•].
Through PLR, lactation induces significant changes in the mineralized extracellular matrix surrounding osteocytes, which may alter the interstitial fluid flow within the LCS and affect the transmission of mechanical stimuli to osteocytes and their cell processes, thus changing osteocytes' mechano-sensitivity. Although direct measurement of interstitial fluid flow in the female skeleton during and after lactation has not yet been performed, the theoretical framework pioneered by Weinbaum et al. [77•] and experimental approaches developed by Wang et al. [76•, 78, 79] provide valuable tools to examine this issue qualitatively. The hydraulic permeability and poroelastic properties of bone tissue determine the magnitude of interstitial fluid flow in mechanically loaded bone. This fluid flow imparts fluid shear stress on the osteocyte cell process membrane [77•], fluid drag force on the pericellular matrix tethering the membrane and the canalicular wall [80, 81], as well as a bending moment on the primary cilium [82]. Weinbaum et al. derived bone permeability from the first principles at three levels: the first and the smallest level of permeability is determined by the effective spacing between tethering fiber arrays that fill the annular space surrounding the osteocyte cell process; the second level deals with the permeability of individual canaliculi, taking into account the non-slip effects of the canalicular wall and the surface of cell process at the canalicular center; the third level concerns the tissue-level permeability by averaging the contribution from all discrete canaliculi. The tissue-level permeability governs the spatiotemporal pattern of load-induced fluid pressurization, and the pressure gradients drive fluid to flow in individual canaliculi [82]. The most important aspect of Weinbaum’s fluid flow model is the Brinkman flow profile within the canaliculi due to the presence of tethering fibers within the fluid annulus, which was subsequently confirmed in experiments by TEM [81]. The tethers were further found to contain perlecan, a large linear proteoglycan [83], which was long and strong enough to serve as a flow sensor in mechanically loaded bone [84]. Using advanced imaging and hydraulic sieving modeling, the fiber spacing of male bones in young and aged groups of perlecan deficient and wildtype mice have been successfully measured, and reduction in the fiber density appeared to decrease the fluid drag force and attenuate bone’s response to anabolic loading [76•].
Whether or not fiber spacing changes in the female skeleton during and after lactation remains to be determined. However, the theoretical framework of bone permeability and the application of poroelasticity [82] allow for analysis of how the altered LCS anatomy alone in lactation may lead to changes of interstitial fluid flow. Enlarged lacunae and canaliculi in bone after lactation (up to 30% compared with those of virgins [19, 21•]) is anticipated to result in increased overall bone permeability and faster pore pressure relaxation, leading to decreased fluid velocity and lower fluid shear stress at the cell process membrane. However, the fluid drag force on the tethering pericellular matrix is anticipated to be higher, mainly due to the increased fluid area interacting with the tethering fibers. Similarly, we expect that primary cilia protruding from the cell bodies experience an elevated bending moment due to the increased fluid-solid interaction area. Moreover, the enlarged fluid space of the lacunae allows greater deflection of the primary cilia, which would result in improved mechanical signal transduction to the cell interior. Taking the above factors together, this model (summarized in Fig. 1) would predict an overall increase of flow-mediated mechanical stimulation on both cell processes and the cell body, suggesting an increased mechano-sensitivity of the female skeleton during lactation. In addition, the osteocyte LCS is the major transport conduit in cortical bone. The enlarged LCS dimensions will proportionally increase the transport flux of signaling molecules and nutrients and waste products among osteocytes and between osteocytes and cells residing on bone surface [74]. Overall, the altered LCS anatomy in lactation is predicted to regulate the osteocyte’s “outside-in” mechano-sensing process as well as “inside-out” responses as the factors released by excited osteocytes are transported through the extensive LCS system. Future work is needed to investigate whether and how lactation alters the sieving property (e.g., fiber spacing) of the pericellular matrix, which is important for both fluid flow and solute transport in the LCS [74, 75].
A schematic of lacunar-canalicular system (LCS) structure and fluid flow model predictions in (top) nulliparous vs. (bottom) lactating bone. Under mechanical loading, the enlarged size of lacunae and canaliculae in lactating bone is anticipated to result in lower interstitial fluid velocity, decreased shear stress on the osteocytic cell process but higher fluid drag on the tethering fibers, increased bending moment on the primary cilium protruding from the osteocyte cell body, as well as increased flux of nutrients and signaling molecules in comparison with nulliparous bone. These changes may be involved in the regulation of the skeletal homeostasis by optimizing the balance between mineral resorption and mechanical integrity of the maternal skeleton
Based on these experimental and simulation data, we propose that lactation-induced PLR plays a critical role in balancing the metabolic and mechanical functions of bone. Lactation initiates PLR to rapidly release mineral from the extracellular matrix of osteocytes, which facilitates the metabolic function of the skeleton to maintain calcium homeostasis during lactation. As a result, increased osteocytic fluid space in the LCS would magnify the transmitted mechanical signal, leading to increased sensitivity of osteocytes to external mechanical signals, which in turn enhances the structural and mechanical adaptation of maternal bone to maintain its critical load-bearing function. Therefore, by amplifying the mechanical signal received by osteocytes during loading, PLR likely serves as the key controller to regulate skeletal homeostasis by optimizing the balance between mineral resorption and mechanical integrity of the maternal skeleton.
Future Directions: Challenges and Unresolved Questions
Recent developments in clinical and laboratory imaging and biomechanical techniques have significantly advanced our understanding of the mechanical regulation of the maternal skeleton during pregnancy and lactation. However, mechanisms behind the observed cellular and tissue-level adaptation of bone structure and mechanical functions to reproduction and lactation are poorly understood.
Numerous hormones change their circulating concentrations during pregnancy, lactation, and after weaning, which have been reviewed in detail by Kovacs [4•]. However, limited data are available on the effects of these hormones on skeletal homeostasis or structural and mechanical adaptations during reproduction and lactation. Particularly, hormonal regulations of pregnancy-associated bone loss and post-weaning recovery are poorly understood. There is a relatively better understanding of the systemic regulation of bone metabolism during lactation. Crosstalk between breast, bone, and brain results in estrogen suppression and increased levels of circulating PTHrP, both of which contribute to rapidly increase osteoclastic resorption [4•, 85]. The influence of these hormones on balancing and maintaining the critical load-bearing bone structure is not well known. It has been proposed that estrogen modulates mechano-responsiveness of bone cells; however, previous studies regarding the involvement of endogenous estrogen or estrogen receptors of bone cells in the adaptive response to loading have yielded conflicting results [86, 87], suggesting complex skeletal responses to the interactive effect of estrogen signaling and mechanical loading. Despite the recent recognition of the therapeutic potential of PTHrP as an osteoanabolic treatment [88], little is known on the roles of circulating PTHrP in skeletal adaptation. Future studies are required to better understand the individual and combined effects of various hormonal changes on skeletal homeostasis and structural and mechanical adaptations during pregnancy, lactation, and post-weaning.
Furthermore, despite recent advances in our understanding of PLR and its role during reproduction and lactation [71•, 72], little is known on the exact signals that trigger osteocytic PLR and how PLR triggered by lactation may affect bone over the long-term. Recent data reported that compared with virgin rats, estrogen deficiency by ovariectomy triggers osteocytic PLR and improves mechano-responsiveness in rats with reproduction and lactation history [89]. Osteocytes are long-lived cells embedded inside the bone. We speculate that osteocytic PLR in response to reduced estrogen levels during lactation may form unique “memory” in these osteocytes, thus leading to similar response of PLR when subjected to estrogen deficiency later in life. Further studies are required to understand the long-term effect of reproduction and lactation on osteocyte signaling and its relationship with skeletal homeostasis and adaptation during menopause.
To prove the hypothesis that increased osteocytic fluid space by lactation-induced PLR magnifies the transmitted mechanical signal and increases osteocyte mechano-sensitivity, direct measurements of LCS fluid flow, shear stress, and drag force on osteocyte cell processes are required. Although these experimental measurements are extremely challenging, these could be achieved by using an in situ imaging approach based on fluorescence recovery after photobleaching (FRAP) imaging developed by Wang et al. [74, 78, 79]. By correlating the changes in LCS ultrastructure, pericellular space and fiber density with the load-induced fluid flow, shear stress, and drag force, important insight will be gained into the influence of PLR on mineral homeostasis and skeletal adaptation during both lactation and pathologic conditions.
Conclusions
While pregnancy and lactation induce significant changes in bone density and structure to provide calcium for fetal/infant growth, the maternal physiology also comprises several innate compensatory mechanisms that allow for the maintenance of skeletal mechanical integrity. The skeletal effects during pregnancy and lactation reflect an optimized balance between the mechanical and metabolic functions of the skeleton. The recent discovery of lactation-induced osteocytic PLR indicates a new means by osteocytes to modulate mineral homeostasis and tissue-level mechanical properties of the maternal skeleton. Furthermore, lactation-induced PLR may also play important roles in maintaining the maternal skeleton’s load-bearing capacity by altering the osteocyte microenvironment and thereby modulating the mechanical signal that is transmitted to the osteocytes and cell processes. Both clinical and animal studies show that parity and lactation have no adverse effect on fracture risk later in life and may even be beneficial for long-term bone health. Future studies are needed to better understand the physiology behind the long-term adaptation of bone structure, cellular activities, and mechanical functions of the female skeleton to reproduction and lactation, which may help to identify new, protective factors against osteoporosis development.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
2017 Global health observatory data. World Health Organization.
Horta BL, Victora CG. Long-term effects of breastfeeding. World Health Organization; 2013.
Global Nutrition Targets 2025: Breastfeeding policy brief. World Health Organization, UNICEF; 2014.
• Kovacs CS. Maternal mineral and bone metabolism during pregnancy, lactation, and post-weaning recovery. Physiol Rev. 2016;96(2):449–547 This paper provided a comprehensive review on skeletal and mineral physiology of the maternal skeleton and disorders of bone and mineral metabolism during pregnancy, lactation, and post-weaning recovery.
Ross AC, Manson JE, Abrams SA, Aloia JF, Brannon PM, Clinton SK, et al. The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: what clinicians need to know. J Clin Endocrinol Metab. 2011;96(1):53–8.
Moller UK, Vieth Streym S, Mosekilde L, Rejnmark L. Changes in bone mineral density and body composition during pregnancy and postpartum. A controlled cohort study. Osteoporos Int. 2012;23(4):1213–23.
Kaur M, Pearson D, Godber I, Lawson N, Baker P, Hosking D. Longitudinal changes in bone mineral density during normal pregnancy. Bone. 2003;32(4):449–54.
Black AJ, Topping J, Durham B, Farquharson RG, Fraser WD. A detailed assessment of alterations in bone turnover, calcium homeostasis, and bone density in normal pregnancy. J Bone Miner Res. 2000;15(3):557–63.
Naylor KE, Iqbal P, Fledelius C, Fraser RB, Eastell R. The effect of pregnancy on bone density and bone turnover. J Bone Miner Res. 2000;15(1):129–37.
Honda A, Kurabayashi T, Yahata T, Tomita M, Takakuwa K, Tanaka K. Lumbar bone mineral density changes during pregnancy and lactation. Int J Gynaecol Obstet. 1998;63(3):253–8.
Kalkwarf HJ, Specker BL, Bianchi DC, Ranz J, Ho M. The effect of calcium supplementation on bone density during lactation and after weaning. N Engl J Med. 1997;337(8):523–8.
Karlsson C, Obrant KJ, Karlsson M. Pregnancy and lactation confer reversible bone loss in humans. Osteoporos Int. 2001;12(10):828–34.
Sowers M, Corton G, Shapiro B, Jannausch ML, Crutchfield M, Smith ML, et al. Changes in bone density with lactation. Jama. 1993;269(24):3130–5.
Recker R, Lappe J, Davies K, Heaney R. Characterization of perimenopausal bone loss: a prospective study.[see comment]. J Bone Miner Res. 2000;15(10):1965–73.
Collins JN, Kirby BJ, Woodrow JP, Gagel RF, Rosen CJ, Sims NA, et al. Lactating Ctcgrp nulls lose twice the normal bone mineral content due to fewer osteoblasts and more osteoclasts, whereas bone mass is fully restored after weaning in association with up-regulation of Wnt signaling and other novel genes. Endocrinology. 2013;154(4):1400–13.
VanHouten JN, Wysolmerski JJ. Low estrogen and high parathyroid hormone-related peptide levels contribute to accelerated bone resorption and bone loss in lactating mice. Endocrinology. 2003;144(12):5521–9.
Honda A, Kurabayashi T, Yahata T, Tomita M, Matsushita H, Takakuwa K, et al. Effects of pregnancy and lactation on trabecular bone and marrow adipocytes in rats. Calcif Tissue Int. 2000;67(5):367–72.
• de Bakker CMJ, Tseng WJ, Li Y, Zhao H, Altman-Singles AR, Jeong Y, et al. Reproduction differentially affects trabecular bone depending on its mechanical versus metabolic role. J Biomech Eng. 2017;139(11) This study quantified the proportion of the load carried by the trabeculae, as well as the extent of reproductive loss and recovery in bone volume, structure, cellular activities, and mechanical properties, at two distinct skeletal sites: the tibia and lumbar vertebra. The differential trabecular response indicate differences in the extent of the trabecular bone’s structural vs. metabolic functions at these two locations.
Qing H, Ardeshirpour L, Pajevic PD, Dusevich V, Jahn K, Kato S, et al. Demonstration of osteocytic perilacunar/canalicular remodeling in mice during lactation. J Bone Miner Res. 2012;27(5):1018–29.
Jahn K, Kelkar S, Zhao H, Xie Y, Tiede-Lewis LM, Dusevich V, et al. Osteocytes acidify their microenvironment in response to PTHrP in vitro and in lactating mice in vivo. J Bone Miner Res. 2017;32(8):1761–72.
• Kaya S, Basta-Pljakic J, Seref-Ferlengez Z, Majeska RJ, Cardoso L, Bromage TG, et al. Lactation-induced changes in the volume of osteocyte lacunar-canalicular space alter mechanical properties in cortical bone tissue. J Bone Miner Res. 2017;32(4):688–97 This study demonstrates that tissue-level cortical bone mechanical properties are rapidly and reversibly modulated by osteocytes in response to lactation and weaning.
Bonewald LF. The amazing osteocyte. J Bone Miner Res. 2011;26(2):229–38.
Gordon MC. Maternal Physiology. Obstetrics: normal and problem pregnancies. 2012.
VanHouten JN, Dann P, Stewart AF, Watson CJ, Pollak M, Karaplis AC, et al. Mammary-specific deletion of parathyroid hormone-related protein preserves bone mass during lactation. J Clin Invest. 2003;112(9):1429–36.
Ardeshirpour L, Brian S, Dann P, VanHouten J, Wysolmerski J. Increased PTHrP and decreased estrogens alter bone turnover but do not reproduce the full effects of lactation on the skeleton. Endocrinology. 2010;151(12):5591–601.
Seriwatanachai D, Thongchote K, Charoenphandhu N, Pandaranandaka J, Tudpor K, Teerapornpuntakit J, et al. Prolactin directly enhances bone turnover by raising osteoblast-expressed receptor activator of nuclear factor kappaB ligand/osteoprotegerin ratio. Bone. 2008;42(3):535–46.
Bornstein S, Brown SA, Le PT, Wang X, DeMambro V, Horowitz MC, et al. FGF-21 and skeletal remodeling during and after lactation in C57BL/6J mice. Endocrinology. 2014;155(9):3516–26.
Lippuner K, Zehnder HJ, Casez JP, Takkinen R, Jaeger P. PTH-related protein is released into the mother’s bloodstream during lactation: evidence for beneficial effects on maternal calcium-phosphate metabolism. J Bone Miner Res. 1996;11(10):1394–9.
Ardeshirpour L, Dann P, Adams DJ, Nelson T, VanHouten J, Horowitz MC, et al. Weaning triggers a decrease in receptor activator of nuclear factor-kappaB ligand expression, widespread osteoclast apoptosis, and rapid recovery of bone mass after lactation in mice. Endocrinology. 2007;148(8):3875–86.
Miller SC, Bowman BM. Rapid inactivation and apoptosis of osteoclasts in the maternal skeleton during the bone remodeling reversal at the end of lactation. Anat Rec (Hoboken). 2007;290(1):65–73.
Bowman BM, Siska CC, Miller SC. Greatly increased cancellous bone formation with rapid improvements in bone structure in the rat maternal skeleton after lactation. J Bone Miner Res. 2002;17(11):1954–60.
Miller SC, Anderson BL, Bowman BM. Weaning initiates a rapid and powerful anabolic phase in the rat maternal skeleton. Biol Reprod. 2005;73(1):156–62.
Carter DR, Bouxsein ML, Marcus R. New approaches for interpreting projected bone densitometry data. J Bone Miner Res. 1992;7(2):137–45.
Cundy T, Cornish J, Evans MC, Gamble G, Stapleton J, Reid IR. Sources of interracial variation in bone mineral density. J Bone Miner Res. 1995;10(3):368–73.
Katzman DK, Bachrach LK, Carter DR, Marcus R. Clinical and anthropometric correlates of bone mineral acquisition in healthy adolescent girls. J Clin Endocrinol Metab. 1991;73(6):1332–9.
Goulet RW, Goldstein SA, Ciarelli MJ, Kuhn JL, Brown MB, Feldkamp LA. The relationship between the structural and orthogonal compressive properties of trabecular bone. J Biomech. 1994;27(4):375–89.
Keaveny TM, Morgan EF, Niebur GL, Yeh OC. Biomechanics of trabecular bone. Annu Rev Biomed Eng. 2001;3:307–33.
Kim HS, Al-Hassani ST. A morphological model of vertebral trabecular bone. J Biomech. 2002;35(8):1101–14.
Van Rietbergen B, Odgaard A, Kabel J, Huiskes R. Relationships between bone morphology and bone elastic properties can be accurately quantified using high-resolution computer reconstructions. J Orthop Res. 1998;16(1):23–8.
Hellmeyer L, Hahn B, Fischer C, Hars O, Boekhoff J, Maier J, et al. Quantitative ultrasonometry during pregnancy and lactation: a longitudinal study. Osteoporos Int. 2015;26(3):1147–54.
Della Martina M, Biasioli A, Vascotto L, Rinuncini D, Adorati Menegato A, Liva S, et al. Bone ultrasonometry measurements during pregnancy. Arch Gynecol Obstet. 2010;281(3):401–7.
Korecki CL, Zinser G, Liu X, Siedler J, Welsh J, Niebur GL. Effect of the vitamin D receptor on bone geometry and strength during gestation and lactation in mice. Calcif Tissue Int. 2009;85(5):405–11.
Vajda EG, Bowman BM, Miller SC. Cancellous and cortical bone mechanical properties and tissue dynamics during pregnancy, lactation, and postlactation in the rat. Biol Reprod. 2001;65(3):689–95.
• de Bakker CM, Altman-Singles AR, Li Y, Tseng WJ, Li C, Liu XS. Adaptations in the Microarchitecture and load distribution of maternal cortical and trabecular bone in response to multiple reproductive cycles in rats. J Bone Miner Res. 2017;32(5):1014–26 This study longitudinally tracked the bone structural changes in rat proximal tibia in response to 3 reproductive cycles and demonstrated that pregnancy and lactation resulted in both transient and long-lasting alterations in trabecular microstructure, improvement in the robustness of cortical bone, and increased proportion of the total load carried by the cortical bone, allowing the overall mechanical function of the tibia to be maintained.
Kovacs CS, Ralston SH. Presentation and management of osteoporosis presenting in association with pregnancy or lactation. Osteoporos Int. 2015;26(9):2223–41.
Laskey MA, Price RI, Khoo BC, Prentice A. Proximal femur structural geometry changes during and following lactation. Bone. 2011;48(4):755–9.
To WW, Wong MW. Changes in bone mineral density of the os calcis as measured by quantitative ultrasound during pregnancy and 24 months after delivery. Aust N Z J Obstet Gynaecol. 2011;51(2):166–71.
Yumusakhuylu Y, Turgut ST, Icagasioglu A, Baklacioglu HS, Atlig RS, Murat S, et al. Bone mineral changes during pregnancy and lactation. Gynecol Endocrinol. 2013;29(8):763–6.
Brembeck P, Lorentzon M, Ohlsson C, Winkvist A, Augustin H. Changes in cortical volumetric bone mineral density and thickness, and trabecular thickness in lactating women postpartum. J Clin Endocrinol Metab. 2015;100(2):535–43.
Bjornerem A, Ghasem-Zadeh A, Wang X, Bui M, Walker SP, Zebaze R, et al. Irreversible deterioration of cortical and trabecular microstructure associated with breastfeeding. J Bone Miner Res. 2017;32(4):681–7.
Brembeck P, Winkvist A, Ohlsson C, Lorentzon M, Augustin H. Determinants of microstructural, dimensional and bone mineral changes postpartum in Swedish women. Br J Nutr. 2016:1–9.
Kokolus S, Vrabel MB, Liu XS, Boutroy S, Rogers H, McMahon D, et al. High resolution peripheral quantitative CT (HRpQCT) reveals preferential inner trabecular bone loss in lactating women. American Society for Bone and Mineral Research Annual Meeting; 2010; Toronto. Canada. .
Kepley A, Boutroy S, Zhang C, Bucovsky M, Vrabel MB, Kokolus S, et al. In breastfeeding women, trabecular bone loss at the radius, seen by high resolution peripheral quantitative CT (HRpQCT), persists at 18 months postpartum. American Society of Bone and Mineral Research Annual Meeting; 2012; Minneapolis, MN.
Liu XS, Ardeshirpour L, VanHouten JN, Shane E, Wysolmerski JJ. Site-specific changes in bone microarchitecture, mineralization, and stiffness during lactation and after weaning in mice. J Bone Miner Res. 2012;27(4):865–75.
Ross RD, Meagher MJ, Sumner DR. Calcium restriction during lactation has minimal effects on post-weaning mineral metabolism and bone recovery. J Bone Miner Metab. 2019;37(4):648–57.
Gillies BR, Ryan BA, Tonkin BA, Poulton IJ, Ma Y, Kirby BJ, et al. Absence of calcitriol causes increased lactational bone loss and lower milk calcium but does not impair post-lactation bone recovery in Cyp27b1 null mice. J Bone Miner Res. 2018;33(1):16–26.
Wiklund PK, Xu L, Wang Q, Mikkola T, Lyytikainen A, Volgyi E, et al. Lactation is associated with greater maternal bone size and bone strength later in life. Osteoporos Int. 2012;23(7):1939–45.
Specker B, Binkley T. High parity is associated with increased bone size and strength. Osteoporos Int. 2005;16(12):1969–74.
de Bakker CMJ, Zhao H, Tseng WJ, Li Y, Altman-Singles AR, Liu Y, et al. Effects of reproduction on sexual dimorphisms in rat bone mechanics. J Biomech. 2018.
Pearson D, Kaur M, San P, Lawson N, Baker P, Hosking D. Recovery of pregnancy mediated bone loss during lactation. Bone. 2004;34(3):570–8.
Whitehead CC. Overview of bone biology in the egg-laying hen. Poult Sci. 2004;83(2):193–9.
ACOG Committee Opinion No. 650: Physical activity and exercise during pregnancy and the postpartum period. Obstet Gynecol. 2015;126(6):e135–42.
Dimov M, Khoury J, Tsang R. Bone mineral loss during pregnancy: is tennis protective? J Phys Act Health. 2010;7(2):239–45.
To WW, Wong MW. Bone mineral density changes during pregnancy in actively exercising women as measured by quantitative ultrasound. Arch Gynecol Obstet. 2012;286(2):357–63.
Promislow JH, Hertz-Picciotto I, Schramm M, Watt-Morse M, Anderson JJ. Bed rest and other determinants of bone loss during pregnancy. Am J Obstet Gynecol. 2004;191(4):1077–83.
Lovelady CA, Bopp MJ, Colleran HL, Mackie HK, Wideman L. Effect of exercise training on loss of bone mineral density during lactation. Med Sci Sports Exerc. 2009;41(10):1902–7.
Little KD, Clapp JF 3rd. Self-selected recreational exercise has no impact on early postpartum lactation-induced bone loss. Med Sci Sports Exerc. 1998;30(6):831–6.
Hemmatian H, Jalali R, Semeins CM, Hogervorst JMA, van Lenthe GH, Klein-Nulend J, et al. Mechanical loading differentially affects osteocytes in fibulae from lactating mice compared to osteocytes in virgin mice: possible role for lacuna size. Calcif Tissue Int. 2018;103(6):675–85.
Rosa BV, Blair HT, Vickers MH, Morel PC, Cockrem JF, Firth EC. Voluntary exercise in pregnant rats improves post-lactation maternal bone parameters but does not affect offspring outcomes in early life. J Musculoskelet Neuronal Interact. 2012;12(4):199–208.
Shea JE, Doody SL, Elsenman PA, Miller SC, editors. Augmentation of bone gains during the anabolic post-lactation recovery period utilizing a rat bipedal stance model. American Society of Bone and Mineral Research Annual Meeting; 2005; Nashville, TN.
• Tsourdi E, Jahn K, Rauner M, Busse B, Bonewald LF. Physiological and pathological osteocytic osteolysis. J Musculoskelet Neuronal Interact. 2018;18(3):292–303 This paper provided a comprehensive review on the peri-lacunar/canalicular remodeling in physiological and pathological conditions and the current understanding of molecular mechanisms behind this osteocyte function.
Yee CS, Schurman CA, White CR, Alliston T. Investigating osteocytic perilacunar/canalicular remodeling. Cur Osteopor Rep. 2019;17(4):157–68.
Tang SY, Herber RP, Ho SP, Alliston T. Matrix metalloproteinase-13 is required for osteocytic perilacunar remodeling and maintains bone fracture resistance. J Bone Miner Res. 2012;27(9):1936–50.
Wang L. Solute transport in the bone lacunar-canalicular system (LCS). Cur Osteopor Rep. 2018;16(1):32–41.
Fritton SP, Weinbaum S. Fluid and solute transport in bone: flow-induced mechanotransduction. Annu Rev Fluid Mech. 2009;41:347–74.
• Wang B, Lai X, Price C, Thompson WR, Li W, Quabili TR, et al. Perlecan-containing pericellular matrix regulates solute transport and mechanosensing within the osteocyte lacunar-canalicular system. J Bone Miner Res. 2014;29(4):878–91 This study linked cellular hydaulic forces (shear and drag) with in vivo bone formation and provided evidence that osteocyte pericellular matrix serves as a flow sensor in the lacunar-canalicular system.
• Weinbaum S, Cowin SC, Zeng Y. A model for the excitation of osteocytes by mechanical loading-induced bone fluid shear stresses. J Biomech. 1994;27(3):339–60 This paper established the theoritical framework demonstrating interstitial fluid flow in mechanically loaded bone imparts fluid shear stress on the osteocyte cell process membrane.
Price C, Zhou X, Li W, Wang L. Real-time measurement of solute transport within the lacunar-canalicular system of mechanically loaded bone: direct evidence for load-induced fluid flow. J Bone Miner Res. 2011;26(2):277–85.
Wang B, Zhou X, Price C, Li W, Pan J, Wang L. Quantifying load-induced solute transport and solute-matrix interaction within the osteocyte lacunar-canalicular system. J Bone Miner Res. 2013;28(5):1075–86.
You L, Cowin SC, Schaffler MB, Weinbaum S. A model for strain amplification in the actin cytoskeleton of osteocytes due to fluid drag on pericellular matrix. J Biomech. 2001;34(11):1375–86.
You LD, Weinbaum S, Cowin SC, Schaffler MB. Ultrastructure of the osteocyte process and its pericellular matrix. Anat Rec A Discov Mol Cell Evol Biol. 2004;278(2):505–13.
Malone AM, Anderson CT, Tummala P, Kwon RY, Johnston TR, Stearns T, et al. Primary cilia mediate mechanosensing in bone cells by a calcium-independent mechanism. Proc Natl Acad Sci U S A. 2007;104(33):13325–30.
Thompson WR, Modla S, Grindel BJ, Czymmek KJ, Kirn-Safran CB, Wang L, et al. Perlecan/Hspg2 deficiency alters the pericellular space of the lacunocanalicular system surrounding osteocytic processes in cortical bone. J Bone Miner Res. 2011;26(3):618–29.
Wijeratne SS, Martinez JR, Grindel BJ, Frey EW, Li J, Wang L, et al. Single molecule force measurements of perlecan/HSPG2: a key component of the osteocyte pericellular matrix. Matrix Biol. 2016;50:27–38.
Wysolmerski JJ. Interactions between breast, bone, and brain regulate mineral and skeletal metabolism during lactation. Ann N Y Acad Sci. 2010;1192:161–9.
Klein-Nulend J, van Oers RF, Bakker AD, Bacabac RG. Bone cell mechanosensitivity, estrogen deficiency, and osteoporosis. J Biomech. 2015;48(5):855–65.
Rooney AM, van der Meulen MCH. Mouse models to evaluate the role of estrogen receptor alpha in skeletal maintenance and adaptation. Ann N Y Acad Sci. 2017;1410(1):85–92.
Esbrit P, Herrera S, Portal-Nunez S, Nogues X, Diez-Perez A. Parathyroid hormone-related protein analogs as osteoporosis therapies. Calcif Tissue Int. 2016;98(4):359–69.
Li Y, De Bakker CM, Tseng WJ, Zhao H, Parajuli A, Wang L et al. Peri-lacunar/canalicular (PLC) remodeling enhances mechano-sensitivity in rat maternal bone when subjected to estrogen deficiency. American Society of Bone and Mineral Research Annual Meeting; 2018; Montreal, Canada.
Funding
This work was supported by NIH K01-AR066743 (to XSL), NIH R01-AR071718 (to XSL), NIH R01-AR054385 (to LW), and NSF #1653216 (to XSL).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
X. Sherry Liu, Liyun Wang, Chantal M. J. de Bakker, and Xiaohan Lai declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Biomechanics
Rights and permissions
About this article
Cite this article
Liu, X.S., Wang, L., de Bakker, C.M.J. et al. Mechanical Regulation of the Maternal Skeleton during Reproduction and Lactation. Curr Osteoporos Rep 17, 375–386 (2019). https://doi.org/10.1007/s11914-019-00555-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-019-00555-5