Abstract
Purpose of Review
Bisphosphonates (BPs) have long been the gold-standard anti-remodeling treatment for numerous metabolic bone diseases. Since these drugs are excreted unmetabolized through the kidney, they are not recommended for individuals with compromised kidney function due to concerns of kidney and bone toxicity. The goal of this paper is to summarize the preclinical BP work in models of kidney disease with particular focus on the bone, kidney, and vasculature.
Recent Findings
Summative data exists showing positive effects on bone and vascular calcifications with minimal evidence for bone or kidney toxicity in animal models.
Summary
Preclinical data suggest it may be worthwhile to take a step back and reconsider the use of bisphosphonates to lessen skeletal/vascular complications associated with compromised kidney function.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Using bisphosphonates (BPs) in the setting of chronic kidney disease (CKD) is kind of like talking about politics at work—the general consensus is you just should not do it. Bisphosphonates have long been the gold-standard anti-remodeling treatment for numerous metabolic bone diseases [1]. Yet because these drugs are not metabolized, kidney function plays a central role in the drug pharmacology [2]. BPs are not recommended for individuals with a creatinine clearance below 30–35 ml/min (estimated glomerular filtration rates (eGFR) lower than 30 ml/min/1.73 m2) due to concern of kidney toxicity as well as drug accumulation in the bone [3]. But what exactly is the basis for the lack of use and concern of negative effects in CKD? Is it evidence based, theoretical, or somewhere in between? While companion articles in this issue address this question using human data, the goal of this paper is to summarize the preclinical BP work in CKD models with particular focus on the bone, kidney, and vasculature (Fig. 1).
Overview of bone, vascular, and renal findings from preclinical models of chronic kidney disease treated with bisphosphonates. Trabecular bone dynamic histomorphometry images from animal with CKD (top) and CKD + zoledronate (bottom). Vascular images adapted from [4] from animal with CKD (right) and CKD + etidronate (left). Kidney data, depicting BUN (blood urea nitrate) from normal animals, animals with CKD, and animals with CKD treated with zoledronate; adapted from [5•, 6]
Bisphosphonates: Some Basics
There are more than a half dozen BPs that are FDA approved in the USA and used for the treatment/prevention of skeletal disease. All BPs have a common phosphate–carbon–phosphate (P–C–P) moiety and two side chains (termed R1 and R2) as their basic structure. The central carbon atom confers a resistance to chemical and enzymatic breakdown, while the two side chains, which differ among the various BPs, determine the mineral binding affinity and biochemical effects on osteoclast enzyme activity [7]. Early BPs did not contain a nitrogen atom and are often referred to as either “early generation” or “non-nitrogen containing” compounds (clodronate and etidronate are examples). More recent BPs, such as alendronate, risedronate, ibandronate, and zoledronate contain a nitrogen atom and are typically referred to as “nitrogen-containing” or “second generation” BPs [8]. There are a number of important differences between nitrogen-containing and non-nitrogen containing classes of BPs (reviewed in [7, 9]) such that any effects (positive or negative) from one class cannot be assumed for the other. Beyond that, even within the newer generation BPs, there are sufficient enough differences that the effects from one cannot be assumed to translate to the others [8]. This becomes important in the setting of CKD as such little data exits that it is often confined to just one or two of the agents. Drug comparison studies are urgently needed in animals (and humans) with CKD.
Skeletal Accumulation of BPs
There exists a solid foundation of data detailing how bisphosphonates accumulate and are cleared in animals with normal kidney function. Upon dosing, the high affinity of BPs for hydroxyapatite results in most of the drug becoming bound to the skeleton (reviewed here [10]). In healthy animals, roughly 60% of administered dose is found within the skeleton 24-h post dose, most of which becomes bound within the first 6 h [11]. Any drug that is not bound is cleared, unmetabolized, primarily by the kidney through passive glomerular filtration and active secretion from the proximal tubule [2].
The skeleton is saturable for an individual dose of BP, but not if that same dose is fractionated [12]. This means cumulative dose, as opposed to amount of drug given at each dose, is a key factor when thinking about BP accumulation in the skeleton. In addition to dose, the route of administration plays a significant role in determining BP levels in the bone [11]. Oral absorption, primarily in the stomach and jejunum, is nonlinearly dose-dependent [11]. Intravenous dosing leads to significantly higher levels of skeletal accumulation relative to oral dosing. Even when bioavailability is matched between oral and intravenous dosing (giving tenfold higher doses orally), there is still tenfold higher plasma concentration and a 30-fold higher concentration of skeletally bound BP with intravenous dosing [13]. Despite the number of studies that have examined the kinetics of skeletal accumulation under various conditions, there exists no direct evidence that levels in the bone have a direct influence on physiology. That is, having more drugs within the skeleton has not been shown to be advantageous or detrimental. In vitro studies clearly illustrate the potential for negative effects of accumulation, as multiple studies have shown that while low concentrations of BPs have beneficial effects (such as reduced osteocyte apoptosis), higher concentrations have negative effects (cell death) [14, 15]. Unfortunately, there are no data from animal BP accumulation studies that present levels in concentrations that relate to these in vitro studies.
Skeletal release of BP has received less attention in the literature. In vivo, hydroxyapatite-bound BP freely dissociates from resting surfaces and is actively liberated at resorption surfaces [16, 17]. Data from drug withdrawal studies, in which animals are dosed with BPs for a period of time and then stopped, suggest that binding properties could influence physiological function as those with higher binding affinity have slower recovery of bone remodeling [18]. Yet, there exists very little in vivo data documenting the dynamics of drug liberation from the skeleton and how it then becomes reattached or excreted over time. This is a significant limitation in our understanding of how levels of drug in the bone are modulated over time in normal animals, not to mention in animals with conditions such as CKD.
Collectively, the preclinical work highlights the complexities that intertwine both chemical and biological effects to determine skeletal accumulation. Furthermore, each BP has its own chemical and biological properties making it necessary to consider each specific drug individually to truly understand its pharmacokinetics and pharmacodynamics. Simply stated, the results from one BP are not generalizable to the others. Given this is the case and the state of knowledge for normal bone, it is not surprising that hesitation exists to use these drugs in conditions of kidney disease, where the primary route of excretion is compromised.
Effects of BPs on Kidney Tissue and Function
Early in vitro work documented that kidney accumulation of BP occurred for first generation BPs (1-hydroxyethylidene—1,1 bisphosphonate; HEBP) in a time-, concentration-, and temperature-dependent manner [19]. BPs passively enter kidney cells through the basolateral membrane and then appear to be bound in the cytosol as nonstochiometric “polynuclear complexes” with bivalent cations or as calcium complexes in the renal tubules [20]. This entry/binding is calcium/phosphate-dependent [19] and exceeds the glomerular filtration rate suggesting active tubular secretion. Using newer generation BPs, it has been shown that roughly 0.5% of an intravenous dose is retained in kidney tissue 2-h post injection; 24-h post dose this level was 0.3% [21•]. The half-life of BP in the kidney tissue of rats is estimated to be just over 3 weeks [21•].
The concern over accumulation of drug in the kidney is the potential effect it could have on cell function or tissue viability. In vitro experiments show that high concentrations of BPs are toxic to kidney cells, as they are to most cells that have been studied in culture [22]. Clodronate (given at supraphysiological dosages) resulted in a consistent mild to moderate proximal tubular necrosis after 3 days of treatment in rats [23]. In the same way, ibandronate produced tubular degeneration/single cell necrosis in a subset of animals [24]. Zoledronate yielded higher levels of damage with the highest doses showing tubular degeneration in the outer medullar and tubular atrophy in the cortex (in some cases in all animals) [24]. Both zoledronate and ibandroante caused hypertrophy and hyperplasia of the collecting ducts and distal tubules after intermittent dosing [24]. Despite these focal histopathalogical effects in some animals, changes in kidney function are noted only at extremely high BP doses [20, 25]. It is important to note, however, that these doses that produce kidney damage are above and beyond those necessary for suppression of bone remodeling.
Effects of BP on Bone in the Setting of CKD
Several experiments have been undertaken to understand how BPs affect the skeleton in the setting of animals with compromised kidney function. These studies have utilized an array of different BPs, animal models (all rodent), and outcome measures. When condensed down to a few clinically relevant parameters, the results are quite consistent and the gaps in knowledge become clear.
Turnover (Remodeling)
CKD can manifest as either high or low-turnover bone disease [26, 27]. High-turnover disease is driven by secondary hyperparathyroidism and the associated metabolic changes. This is the patient population in which BP intervention makes the most sense given their potent remodeling suppression efficacy. Yet, there is concern that the use of BPs will result in adynamic bone—a term originally used to describe the histological phenotype of patients with aluminum toxicity in which there was no bone formation (and few to no cells) [28]. Unfortunately, this term has more recently been used to describe low (not absent) bone remodeling without regard to the cellular composition of the bone. This is problematic because using the definition of low remodeling, most individuals on anti-remodeling treatment such as bisphosphonates (whether or not they have CKD) would be classified as having adynamic bone disease given that most osteoporotic drugs will induce 70–90% suppression of bone remodeling, yet bone cells remain.
Bone remodeling is assessed in animals much the same as it is in humans, using fluorescent agents given in vivo followed by histological analysis. The main difference from the human assessment is the skeletal site, where long bones and vertebra are most common in animals, as opposed to the iliac crest in humans. Histological analysis can yield a multitude of outcome parameters, but the one most often used to indicate bone remodeling/turnover rate is bone formation rate (BFR). For sites of trabecular bone, this variable captures the formation at sites that are assumed to have previously undergone resorption as part of the standard coupled remodeling process (resorption–formation). This, along with the idea that the bone is in a steady state at the time when the labels are given, are two of several assumptions that are made when using histological assessment of bone tissue [29, 30].
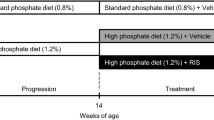
A number of animal models that display high-turnover CKD have been assessed for the effects of BPs on bone turnover. CKD-induced models, using adenine [31•] or nephrectomy (2/3 or 5/6) [32, 33], consistently show elevated trabecular bone remodeling (using BFR as a surrogate). Etidronate, pamidronate, and ibandronate each have been shown to significantly reduce BFR in trabecular bone of animals with CKD. The suppression was dose-dependent, with some doses bringing BFR down to levels found in nonaffected animals and others suppressing BFR beyond that of normal animals [31•]. Using a progressive model of CKD, our group showed that a single intraperitoneal dose of zoledronate treatment (at two different doses, 5× different than each other) over 5 weeks significantly reduced trabecular BFR to levels below those of untreated CKD animals and normal animals, but not significantly different than normal animals treated with zoledronate [34]. A follow-up study in the same animal model, extending the time period to 10-week post dose, again documented significant reductions in BFR compared to untreated CKD, but rates were essentially equivalent to normal untreated animals [5•]. While the number of papers is not overwhelming, the data are consistent and clear. When trabecular BFR is high in the setting of CKD, BPs effectively reduce it to levels that are comparable to animals with normal renal function treated with the same drug. Most importantly, there is no indication of adynamic bone (defined as the complete suppression of activity and cells).
Treating low-turnover CKD with BPs makes less intuitive sense, yet because patients can spontaneously transition from high to low turnover, it is important to study this extreme as a worse case scenario. The question would be if adding BP treatment on top of a low-turnover disease could produce true adynamic bone by suppression of cell function. The experimental literature, albeit limited, says no. Using the progressive CKD model, but this time with the addition of calcium supplementation (which lowers PTH and BFR in this model), there was modest additional suppression of BFR when adding zoledronate treatment [5•]. Importantly, as seen with high-turnover disease, the remodeling rates did not differ from treatment of normal animals or CKD animals with calcium alone. This would suggest that BPs do not push low-turnover CKD to a state of adynamic bone, although this study used a modest dosing schedule (single dose assessed 10 weeks later).
Volume, Density, and Mineralization
Animal data concerning how BP treatment affects bone density are highly variable, in part due to variable effects of CKD in the animal models. Studies from each of the common models have documented no effect of disease on trabecular bone volume, matching multiple pieces of data from humans. BP treatment either has no effect [31•] or leads to higher BV/TV and/or BMD [5•, 33,34,35,36]. The effects on correcting cortical porosity are modest, although only one paper has actually assessed this variable [5•]. This is quite surprising given the known preferential effect of CKD on cortical bone [37]. The effects of BP on tissue mineralization, or other aspects of the matrix for that matter (mineral crystallinity, heterogeneity, collagen structure/cross-linking, hydration, microdamage), are nonexistent in part because the effects of CKD alone have only recently been explored [38, 39]. Given that BPs are known to affect tissue properties in ways that have both positive and negative influence on bone integrity [40], these ultra structural assessments are desperately needed to understand the full picture of BP effects.
Mechanical Properties
Few data exist concerning the effects of BPs on mechanical properties of CKD bone. In a nephrectomy model, there was no effect of pamidronate on mechanical properties of the femoral diaphysis, although there was also no effect of nephrectomy alone, and only one variable was presented (ultimate load) [32]. Using the progressive CKD model, which develops reductions in the whole bone and material mechanical properties when untreated, 5 or 10 weeks of zoledronate treatment failed to fully normalize femoral diaphysis properties [5•, 34]. In these same animals, zoledronate was able to only partially normalize the deficits in vertebral mechanical properties induced by CKD [36]. Although limited, these data are somewhat surprising given BPs typically preserve mechanical properties of the bone in rodent models of other diseases (such as ovariectomy or disuse). This highlights the importance of incorporating mechanical assessment in animal studies. Although changes in remodeling and density are important, ultimately the goal of treatment is to preserve mechanical integrity and animal studies afford a unique opportunity to actually assess mechanic properties. There is growing evidence from animal work that CKD has numerous effects on bone quality (reviewed in a companion article in this issue), and these alterations ultimately combine with the structural changes to determine fracture resistance.
Skeletal Accumulation
There are no data concerning how compromised kidney function affects skeletal accumulation of BPs. This is somewhat surprising given that accumulation of BP is often cited as a reason why these agents should not be used in patients with kidney disease.
Effects of BP on Kidney Function/Structure in the Setting of CKD
Very little data exists regarding effects of BP on kidney structure/function in animals with altered kidney function. In a uninephrectomized rat model (young female rats) that resulted in animals having about a 70% reduction in kidney function, a clinically relevant dose of ibandronate was injected either once or nine times (every 3 weeks) over an 18-week experiment. Concentrations of ibandronate in the kidney of normal animals were 1.6× higher in animals that received nine injections compared to those who received one. Animals with compromised kidney function had a difference of 1.8× between the two dosing groups but, most importantly, the levels of drug in the kidneys of animals given nine injections of ibandronate were significantly higher in animals with reduced kidney function [21•]. Despite this apparent higher level of accumulation in renal tissue, there is no clear effect on kidney function as assessed by BUN [6, 34] or creatinine clearance [32, 33, 35, 41] in animals with CKD, perhaps due to the limitations of these biochemical markers to detect minor changes.
Effects of BP on Vasculature Calcification
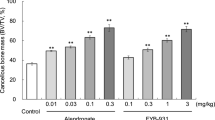
The consequences of vascular calcification in the setting of CKD are well established [42]. Given the clinical concern surrounding the use of BPs in CKD patients, the goal of all the animal studies focused on vascular calcification to date has been to find a BP dose that inhibits vascular calcification but does not affect bone remodeling. It is important to note that animal studies focused on vascular calcification in CKD often employ additional interventions, beyond nephrectomy or adenine, to promote calcification (either low protein diet or warfarin and vitamin D treatment). In animals with normal kidney function treated with calcification-inducing vitamin D and warfarin, both alendronate and ibandronate inhibit the formation of calcification, as assessed histologically for presence of mineral in the aortic wall [43]. In animals with CKD that are given calcification stimuli, ibandronate, pamidronate, and etidronate all inhibit calcification formation, although the latter was only found at very high doses [4, 6, 31•]. For both ibandronate and pamidronate, the dose needed to inhibit vascular calcification parallel that needed to suppress bone remodeling [43]. This supports other evidence that there may be a link between vessel calcification and bone resorption. The challenge in interpreting such data is that these studies used doses that exceed those used clinically, and they administer BP prior to the formation of calcification. Thus, although prevention of calcification development can be achieved with BPs, studies showing effects on progression would be more clinically relevant. Using the progressive CKD model, treatment with a single dose of zoledronate was not sufficient to significantly alter the higher level of aortic calcium content that develops naturally in this model [5•].
Gaps in Knowledge
Assessment of the preclinical literature highlighted several gaps in our knowledge about bisphosphonates in the setting of CKD. A select few of these are presented here in hopes that they will stimulate readers to engage in this line of research and help propel the field forward.
-
How is skeletal distribution of bisphosphonate affected in settings of compromised kidney function and does this differ among the various drugs (and routes and doses)?
-
Are there optimal dosing regimens that can be utilized long-term to suppress bone remodeling and vascular calcification while not damaging kidney function?
-
How do bisphosphonates work in the setting of CKD to affect tissue-level properties and how does this affect bone mechanical properties?
-
Are rodent models telling us the whole story about CKD and BPs? Given the preferential effects of CKD on cortical bone, and the lack of normal osteonal remodeling in rodents, there would seem to be value in assessing key skeletal properties (remodeling rate, cortical porosity, mechanics) in a large animal model of CKD treated with BPs.
Conclusions
Despite the prominent role of bisphosphonates in prevention/treatment of numerous skeletal conditions, they are notably absent in the treatment plan of patients with renal disease. In the introduction, we posed the question of whether concerns surrounding the negative effects of bisphosphonates in the setting of compromised renal function were evidence based, theoretical, or somewhere in between? Based on the preclinical data, it seems clear that the benefits are many and the concerns are almost all manifest only when doses far exceed those that are clinically relevant. There is no evidence that skeletal levels of drug reach toxic levels, and no evidence that the level of remodeling suppression in CKD is more than that in animals without CKD. Although the data on the vascular benefits are minimal, they are intriguingly positive. There is also no evidence that clinically relevant doses have negative effects on kidney function in animal models. These data suggest it may be worthwhile to take a step back and reconsider using bisphosphonates to lessen skeletal/vascular complications associated with compromised kidney function.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Russell RGG. Bisphosphonates: the first 40 years. Bone. 2011;49:2–19.
Troehler U, Bonjour J-P, Fleisch H. Renal secretion of diphosphonates in rats. Kidney Int. 1975;8:6–13.
Miller PD. The kidney and bisphosphonates. Bone. 2011;49:77–81.
Tamura K, Suzuki Y, Matsushita M, Fujii H, Miyaura C, Aizawa S, et al. Prevention of aortic calcification by etidronate in the renal failure rat model. Eur J Pharmacol. 2007;558:159–66.
• Moe SM, Chen NX, Newman CL, Gattone II VH, Organ JM, Chen X, et al. A comparison of calcium to zoledronic acid for improvement of cortical bone in an animal model of CKD. J Bone Miner Res. 2014;29:902–10. One of the few studies to examine effects of bisphosphonates on bone remodeling and mechanics in animals with compromised kidney function.
Price PA, Roublick AM, Williamson MK. Artery calcification in uremic rats is increased by a low protein diet and prevented by treatment with ibandronate. Kidney Int. 2006;70:1577–83.
Ebetino FH, Hogan A-ML, Sun S, Tsoumpra MK, Duan X, Triffitt JT, et al. The relationship between the chemistry and biological activity of the bisphosphonates. Bone. 2011;49:20–33.
Russell RGG, Watts N, Ebetino FH, Rogers M. Mechanisms of action of bisphosphonates: similarities and differences and their potential influence on clinical efficacy. Osteoporos Int. 2008;19:733–59.
Rogers MJ, Crockett JC, Coxon FP, Mönkkönen J. Biochemical and molecular mechanisms of action of bisphosphonates. Bone. 2011;49:34–41.
Allen MR. Skeletal accumulation of bisphosphonates: implications for osteoporosis treatment. Expert Opin Drug Metab Toxicol. 2008;4:1371–8.
Lin J. Bisphosphonates: a review of their pharmacokinetic properties. Bone. 1996;18:75.
Lin JH, Chen IW, Duggan DE. Effects of dose, sex, and age on the disposition of alendronate, a potent antiosteolytic bisphosphonate, in rats. Drug Metab Dispos. 1992;20:473–8.
Usui T, Watanabe T, Higuchi S. Pharmacokinetics of YM175, a new bisphosphonate, in rats and dogs. Drug Metab Dispos. 1995;23:1214–9.
Plotkin L, Weinstein R, Parfitt A, Roberson P, Manolagas S, Bellido T. Prevention of osteocyte and osteoblast apoptosis by bisphosphonates and calcitonin. J Clin Invest. 1999;104:1363–74.
Plotkin L, Manolagas S, Bellido T. Dissociation of the pro-apoptotic effects of bisphosphonates on osteoclasts from their anti-apoptotic effects on osteoblasts/osteocytes with novel analogs. Bone. 2006;39:443–52.
Masarachia P, Weinreb M, Balena R. Comparison of the distribution of 3H-alendronate and 3H-etidronate in rat and mouse bones. Bone. 1996;19:281–90.
Kimmel D. Mechanism of action, pharmacokinetic and pharmacodynamic profile, and clinical applications of nitrogen-containing bisphosphonates. J Dent Res. 2007;86:1022.
Fuchs R, Phipps R. Recovery of trabecular and cortical bone turnover after discontinuation of risedronate and alendronate therapy in ovariectomized rats. J Bone Min Res. 2008;23:1689–97.
Troehler U, Bonjour JP, Fleisch H. Renal transport of bisphosphonates: accumulation by renal cortical slices enhanced by calcium phosphate ions. J Lab Clin Med. 1985;106:23–9.
Pfister T, Atzpodien E, Bohrmann B, Bauss F. Acute renal effects of intravenous bisphosphonates in the rat. Basic Clin Pharmacol Toxicol. 2005;97:374–81.
• Bergner R, Siegrist B, Kränzlin B, Gretz N, Faust H, Pfister T. Determination of renal tissue ibandronate levels in rats with normal and mildly impaired renal function. J Pharmacol Toxicol Methods. 2013;68:225–30. Excellent study that examines renal handing of bisphosphonates in animals with compromised kidney function.
Lühe A, Künkele K-P, Haiker M, Schad K, Zihlmann C, Bauss F, et al. Preclinical evidence for nitrogen-containing bisphosphonate inhibition of farnesyl diphosphate (FPP) synthase in the kidney: implications for renal safety. Toxicol in Vitro. 2008;22:899–909.
Alden CL, Parker RD, Eastman DF. Development of an acute model for the study of chloromethanediphosphonate nephrotoxicity. Toxicol Pathol. 1989;17:27–32.
Pfister T, Atzpodien E, Bauss F. The renal effects of minimally nephrotoxic doses of ibandronate and zoledronate following single and intermittent intravenous administration in rats. Toxicology. 2003;191:159–67.
Green JR, Seltenmeyer Y, Jaeggi KA, Widler L. Renal tolerability profile of novel, potent bisphosphonates in two short-term rat models. Pharmacology & toxicology. 1997;80:225–30.
Moe S, Drüeke T, Cunningham J, Goodman W, Martin K, Olgaard K, et al. Definition, evaluation, and classification of renal osteodystrophy: a position statement from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int. 2006;69:1945–53.
Malluche HH, Porter DS, Monier-Faugere M-C, Mawad H, Pienkowski D. Differences in bone quality in low- and high-turnover renal osteodystrophy. J Am Soc Nephrol. 2012;23:525–32.
Andress DL, Maloney NA, Endres DB, Sherrard DJ. Aluminum-associated bone disease in chronic renal failure: high prevalence in a long-term dialysis population. J Bone Miner Res. 1986;1:391–8.
Dempster DW, Compston JE, Drezner MK, Glorieux FH, Kanis JA, Malluche H, et al. Standardized nomenclature, symbols, and units for bone histomorphometry. J Bone Miner Res. 2013;28:2–17.
Recker R, Kimmel D, Dempster D, Weinstein R, Wronski T, Burr DB. Issues in Histomorphometry. Bone. 2011;49:955–64.
• Lomashvili KA, Monier-Faugere M-C, Wang X, Malluche HH, O'Neill WC. Effect of bisphosphonates on vascular calcification and bone metabolism in experimental renal failure. Kidney Int. 2009;75:617–25. One of the few studies to examine effects of bisphosphonates on vascular calcification in animals with compromised kidney function.
Jokihaara J, Pörsti IH, Kööbi P, Jolma PM, Mustonen JT, Saha HHT, et al. Treatment of experimental renal osteodystrophy with pamidronate. Kidney Int. 2008;74:319–27.
Geng Z, Monier-Faugere MC, Bauss F, Malluche HH. Short-term administration of the bisphosphonate ibandronate increases bone volume and prevents hyperparathyroid bone changes in mild experimental renal failure. Clin Nephrol. 2000;54:45–53.
Allen MR, Chen NX, Gattone VH, Chen X, Carr AJ, LeBlanc P, et al. Skeletal effects of zoledronic acid in an animal model of chronic kidney disease. Osteoporos Int. 2012;24:1471–81.
Tomat A, Gamba CA, Mandalunis P, De Grandi MC, Somoza J, Friedman S, et al. Changes in bone volume and bone resorption by olpadronate treatment in an experimental model of uremic bone disease. J Musculoskelet Nueronal Interact. 2005;5:174–81.
Newman CL, Chen NX, Smith E, Smith M, Brown D, Moe SM, et al. Compromised vertebral structural and mechanical properties associated with progressive kidney disease and the effects of traditional pharmacological interventions. Bone. 2015;77:50–6.
Parfitt AM. A structural approach to renal bone disease. J Bone Miner Res. 1998;13:1213–20.
Newman CL, Moe SM, Chen NX, Hammond MA, Wallace JM, Nyman JS, et al. Cortical bone mechanical properties are altered in an animal model of progressive chronic kidney disease. PLoS One. 2014;9:e99262.
Allen MR, Newman CL, Chen N, Granke M, Nyman JS, Moe SM. Changes in skeletal collagen cross-links and matrix hydration in high- and low-turnover chronic kidney disease. Osteoporos Int. 2014;26:977–85.
Allen MR, Burr DB. Bisphosphonate effects on bone turnover, microdamage, and mechanical properties: what we think we know and what we know that we don’t know. Bone. 2011;49:56–65.
Fischer D-C, Jensen C, Rahn A, Salewski B, Kundt G, Behets GJ, et al. Ibandronate affects bone growth and mineralization in rats with normal and reduced renal function. Pediatr Nephrol. 2010;26:111–7.
Moe SM, Chen NX. Mechanisms of vascular calcification in chronic kidney disease. J Am Soc Nephrol. 2008;19:213–6.
Price PA, Faus SA, Williamson MK. Bisphosphonates alendronate and ibandronate inhibit artery calcification at doses comparable to those that inhibit bone resorption. Arterioscler Thromb Vasc Biol. 2001;21:817–24.
Acknowledgements
This work is supported by funding from VA Merit award (BX003025).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Matthew Allen and Mohammad Aref declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Kidney and Bone
Rights and permissions
About this article
Cite this article
Allen, M.R., Aref, M.W. What Animal Models Have Taught Us About the Safety and Efficacy of Bisphosphonates in Chronic Kidney Disease. Curr Osteoporos Rep 15, 171–177 (2017). https://doi.org/10.1007/s11914-017-0361-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-017-0361-4