Abstract
A considerable volume of evidence has accumulated to suggest that whole-body vibration (WBV) may have a therapeutic role to play in the prevention of osteoporotic fracture, particularly for individuals who are unable to tolerate vigorous exercise interventions. There is moderate to strong evidence that WBV will prevent falls (likely due to enhanced neuromuscular function), but also some indication that the effects of WBV do not outstrip those of targeted exercise. Animal data indicates that WBV will also improve bone mass, including preventing loss due to hormone withdrawal, disuse and glucocorticoid exposure. Human trials, however, have produced equivocal outcomes for bone. Positive trends are apparent at the hip and spine, but shortcomings in study designs have limited statistical power. The mechanism of the vibration effect on bone tissue is likely to be mechanical coupling between an oscillating cell nucleus and the cytoskeleton. More robust dose-response human data are required before therapeutic guidelines can be developed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Why Vibration?
It is well recognised that the risk of osteoporotic fracture increases with age-related loss of bone mass [1]. In fact, for every standard deviation decrease in femoral neck bone mineral density (BMD), there is an almost threefold increased risk of hip fracture [1]. Of even greater significance, over 90 % of hip fractures occur as a direct result of a fall [2] which also increase with age, largely reflecting a deterioration in neuromuscular function [3]. Thus, preventing age-related loss of bone and enhancing lower extremity muscle strength and balance to decrease falls [4] are both vital strategies to reduce the risk of osteoporotic fracture.
Pharmacological interventions are the most recognised and accepted therapies for osteoporosis, by virtue of their ability to induce the most marked improvement in bone mass and to reduce fractures [5]. However, adoption is low, non-response and side effects are common and compliance after 1 year is very poor [6–9]. Furthermore, while anti-resorptive treatment has been associated with a 42 % overall reduced risk for hip fracture [10], only a 26 % reduction in rate of recurrent fractures has been observed [11]. As medications do not maintain or enhance muscle strength or balance [12], they offer no protection from falls. There is, therefore, a clear need to identify alternative treatments to drug therapy in order to address the growing burden of osteoporotic fractures in ageing populations.
Animal models have shown that exercises involving high magnitude loads are anabolic to bone. The translation from ‘bench to bedside’ has been somewhat disappointing however, as the response of the ageing human skeleton to exercise is often quite modest. The latter situation may be a function of both reduced capacity and inclination of the elderly to tolerate the requisite loading intensity for exercise benefits to be realised. A less physically intense or passive source of mechanical stimulation of the skeleton would therefore be advantageous for those most at risk of osteoporotic fracture. For this reason, whole-body vibration (WBV), a low-magnitude but high-frequency form of mechanical stimulation, has been examined as a potential therapy to enhance bone mass and improve neuromuscular function.
What Exactly Is Whole Body Vibration?
It is difficult, if not impossible, to actively apply mechanical loads at very high frequency to the whole human body. To illustrate, the world 100-m sprint record holder Usain Bolt ran at a step frequency of only 4.49 Hz to clock a time of 9.58 s (Berlin 2009). Clearly then, vibration loads must be externally applied. For the ‘whole body’ to be stimulated, a person must stand on a floor-mounted vibrating plate. (As the upper extremity does not receive a weight bearing vibration, the whole body is not technically affected by the same stimulus.) WBV can be produced by the plate in a number of ways (e.g. Fig. 1): by alternate direction movements in a vertical plane, by alternating elevations of the right and left sides around a central axis or by a combination of movements in the horizontal, vertical and oblique planes (sometimes referred to as tri-planar vibration) [13]. Vertical vibration has been shown to transmit 85 % of a 0.2 g, 30 Hz vibration stimulus at the feet during standing to clinically relevant skeletal sites (hip and spine) [14]. Others have also demonstrated strong transmissibility of a broad range of vibration stimuli [15]. Some report considerable damping of the signal (reduced transmission) if joints are flexed rather than fully extended in standing [16], but others have observed the opposite effect in a semi-squat position [17].
Vibration intensity is best described in terms of acceleration, in g-forces. A g is calculated by dividing maximum acceleration by gravity (a max/9.81 ms−2); therefore, 1 g is equal to the acceleration of gravity. Acceleration can be modulated through the frequency (f) of plate movements per second (in Hz), or the amplitude (a) of plate movement (displacement of the plate from equilibrium, measured in mm), or both (Fig. 2). Increasing vibration amplitude most notably increases acceleration forces [17]. A vibration stimulus of <1 g is considered to be low intensity, whereas a stimulus if ≥1 g is considered high intensity.
Vibration parameters and terminology. Displacement can be described as amplitude (distance from plate equilibrium, in mm), or peak-to-peak distance (in mm), which, when combined with the sinusoidal cycle duration (frequency, in cycles per second, or Hz), can be described in terms of acceleration (g-force, ms−2)
There are now many WBV devices commercially available, producing a wide range of accelerations; from 0.3 g to more than 10 g. Depending on device, frequency and amplitude can be fixed by the manufacturer, or varied by adjusting a dial and/or foot placement (if the plate oscillates around a central fulcrum). Of concern, vibration intensity is frequently omitted from device specifications, as is the degree of change in intensity per unit adjustment on a control panel. As a consequence, it is likely that many devices operate at vibration intensities above the safety limits determined by the International Organisation for Standardisation (ISO 2631/3) (discussed below).
Efficacy and Mechanisms
What Is the Evidence for Efficacy?
Bone Response
Animal Data
A considerable volume of evidence from well-controlled animal studies is available to suggest a beneficial effect of vibration on bone. For example, decreased osteoclastic resorption [18] and improved tibial metaphyseal geometry and strength were observed in a murine model following 6 weeks of vibration [19]. ‘Postmenopausal’ bone loss was prevented in ovariectomised (OVX) rats exposed to 2 g acceleration at 50 Hz for 30 min/day, 5 days/week [20]. The addition of vibration enhanced the effect bisphosphonate treatment in one rat study [21] but not another [22]. Vibration at 90 Hz for 10 min/day prevented the decline in bone formation associated with disuse (hind limb suspension) in female rats, an effect that was not matched by 10 min/day weight bearing [23]. A protocol of 1 g at 60 Hz for 30 min/day, 5 days/week for 9 weeks, prevented glucocorticoid-induced bone loss [24]. Murine cell cultures subjected to 0.1–0.4 g at 30 Hz for 10–60 min/day also maintained bone formation and mineralisation during disuse with potentially enhanced preosteoblast differentiation [25]. Intriguingly, low-intensity vibration appears to stimulate preferential differentiation of mesenchymal stem cells into bone rather than fat cell precursors [26]. The first large-animal trial (20 min, 0.3 g vertical vibration at 30 Hz, 5 days/week for 12 months) increased trabecular bone in the proximal femora of sheep by 34.2 % [27]. Those trabeculae changed from rod to plate shaped in the plane of weight bearing, an effect that created a stiffer bone, less prone to fracture for a given load [28].
Human Data—Low-Intensity Vibration
Human trials of WBV have produced results that do not entirely reflect the animal findings. Twelve months of 20 min/day, 0.2 g at 30 Hz, in postmenopausal women produced no significant difference between treatment and control groups from intention to treat analysis, but WBV maintained femoral neck and lumbar spine BMD of those who complied 86 % or more, and the lightest women improved the most [29]. A recent similar but larger trial also observed no significant between-group differences at the same sites at 12 months; however, large variability reduced statistical power and notable trends for a beneficial effect of WBV were observed [30]. Another group reported no effect of a similar WBV protocol at 30 or 90 Hz on volumetric BMD from high-resolution peripheral quantitative computed tomography (HR-pQCT) [31]. Findings were arguably confounded by simultaneous supplementation of the whole sample with high doses of calcium and vitamin D, now considered to be a non-trivial independent intervention. A report that a 12-month daily 0.3 g protocol at 30 or 90 Hz tended to reduce calcaneal BUA in postmenopausal women with osteopenia [32], must also be interpreted with caution in light of the recognised low precision of quantitative ultrasound (QUS) measures. In the latter trial, the reported changes for all groups were considerably lower than the LSC calculations for short-term QUS measurement reproducibility.
Younger cohorts at risk of low bone mass have also been treated with low-intensity WBV. A 12-month trial of 15–20-year-old young women with low bone mass found a 0.3 g stimulus at 30 Hz increased lumbar spine trabecular bone 2.1 % and femoral mid-shaft cortical bone 3.4 %. Cross-sectional area of paraspinal musculature also improved 4.9 % more in the treatment group than in the controls [33]. A 6-month RCT of the same low-intensity protocol markedly improved trabecular bone volume at the proximal tibia and spine of 20 pre- and post-pubertal, disabled, ambulant children [34].
Human Data—High-Intensity Vibration
An 8-month high-intensity WBV intervention examined the effect of 4 min/day, 3–5 days/week vibration plus light exercise at 25 to 45 Hz, for maximum vertical accelerations of 2 to 8 g on young, healthy adults [35]. No effect on mass, structure or estimated strength of bone was observed at any skeletal site. The lack of effect in the young healthy cohort may reflect the diminishing returns of mechanical stimuli on an already robust skeleton. Untrained postmenopausal women increased hip BMD 4.3 % and balance 29 % after 8 months of 3 days/week, 6 × 1 min sessions of side-to-side oscillating WBV compared with walking [36]. Six months of 5 mm, 30 Hz, 10 min/day, 5 days/week WBV stimulated improvements in femoral neck and lumbar spine BMD and reduced chronic back pain in postmenopausal women with osteoporosis [37]. While 6 months of 5 min of 3.2 g vibration at 30 Hz 3/week improved lumbar spine BMD >2 % in postmenopausal women [38], 12 months of 10 × 1 min, 20 Hz (3–4 mm) vibration at 30° knee flexion 2–3/week produced no discernible change in indices of bone quality from HR-pQCT [39]. Interestingly, results of a high-protein diet study indicated 5 days of 3.5 g vibration at 30 Hz 10 min/day counteracted diet-induced increased excretion of bone resorption markers in young men and women [40].
High-intensity vibration protocols that have been combined with exercise (6 months 35–40 Hz, 2.3–5.1 g, 20 min/day and 12.6 Hz, 2 g, 3/week) have shown improvements in hip BMD 0.93–4.3 % and balance 29 % in postmenopausal women [36, 41], but study designs prevent the examination of WBV in isolation.
A direct comparison of two different vibration regimes of twice weekly low-level WBV (15 min, 30 Hz, 0.3 g) versus higher-level WBV (6 min, 12.5 Hz, 1 g) against a control group found that both forms of WBV preserved bone mass at the hip and spine compared to losses in controls (with no notable differences between) and enhanced lower extremity muscle function and mobility [42].
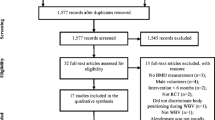
Systematic reviews of WBV effects on bone have reported that less than 1 % of potentially relevant studies are eligible for inclusion due to methodological shortcomings and that cohort and stimulus heterogeneity limit the ability to make strong conclusions from remaining data [43–46]. While the most recent meta-analysis concluded that WBV has no effect on BMD, each BMD analysis included only two or three trials [46]. All reviews identify a need for future trials to be of more robust design, with larger cohorts and longer interventions.
Muscle Response
Muscle weakness not only increases the risk of falling [47] but also minimises loads on bone which may contribute to disuse osteopenia. Conversely, increased muscle strength is typically associated with improvements in bone. Thus, enhancement of neuromuscular performance likely provides dual benefits for fracture prevention.
Vibration loading enlarges fast and slow twitch muscle fibres [48] and increases lower extremity muscle activation during squatting [49]. Larger displacements (4 mm) will activate muscles more and induce greater muscle fatigue than smaller displacements (1 mm) [50].
A systematic review of the scientific support for effects of WBV on muscle strength and jump performance concluded there is moderate to strong evidence that long-term WBV improves lower extremity muscle performance, but that the effect is primarily observed in the untrained and/or those who cannot exercise at a high level of intensity such as the elderly [51]. In young, healthy [52] and postmenopausal cohorts [53, 54], improvements in muscle strength and performance following WBV training are often similar to those derived from exercise alone; however, there is some evidence that even when WBV-induced strength gains do not exceed those derived from resistance training, functional performance (e.g. counter movement jump height) may be enhanced [35, 55–57] or falls reduced [58]. The most recent meta-analysis concluded that WBV improves lower extremity muscle strength and function, an effect that can be achieved in 6–10 weeks [46].
While there is inadequate evidence in the literature to determine the optimum WBV dose for muscle strength outcomes, two and three training sessions a week are reportedly more effective than one [59]. It is possible that an individualised vibration frequency is required to produce an optimum neuromuscular response [60].
Balance and Fall Response
There is evidence to suggest that WBV may minimise fracture risk by improving balance, thereby reducing the risk of falls [3]. During vibration, small changes in muscle length are elicited that enhance the excitability of the spinal reflex [61]. Experiments in anaesthetized cats indicate that single 1a afferents can respond on a 1:1 basis to up to 150 Hz vibration [62]. Hypothetically then, neuromuscular adaptation to WBV may improve postural control and prevent falls when balance is perturbed.
While WBV does not appear to improve balance performance in young, healthy adults [35], the results for older cohorts are more consistently positive. A range of trials testing WBV interventions for balance-related outcomes over periods ranging from 6 weeks to 8 months have reported improvements in timed up and go and balance scores [56], walking speed, step length and balance [63], balance and stability [64], risk of falls and improved quality of life [65] and ankle joint range of motion and improved foot plantar surface sensation [66] of nursing home residents, untrained postmenopausal women and elderly community-living, non-exercising women compared with walking [36], exercises alone and physiotherapy. A number of well-designed trials comparing WBV plus exercise training versus exercising controls report beneficial effects such as reduced sway in response to stance perturbation [67] and improved balance, gait and functional mobility [68], but that WBV effects are not greater than exercise alone.
Importantly, a large trial examining the efficacy of 18 months of 20-min low-intensity vibration, 5 days/week, in elderly men and women reported significantly fewer falls or fractures in the treatment group [69•]. A simultaneous improvement in reaction time, muscle strength and movement velocity may explain the reduction in falls. Fracture rate was also lower in the WBV group but did not reach significance.
Authors of systematic reviews frequently conclude that while there may be evidence from a number of acceptable quality studies that WBV benefits balance, mobility and muscle function, many other studies have been insufficiently robust to differentiate the influence of WBV from exercise [43, 70, 71]. A 2012 meta-analysis suggests simple balance abilities and mobility (but not gait) may be improved by WBV and that a reduction in falls may be evident in the most frail [72].
What Is the Mechanism of Action?
The transduction of large exercise-induced mechanical loads into a biological signal for bone adaptation is thought to be a function of the tissue deformation-induced fluid flow that occurs during relatively large bone strain events [73]. Beyond strain magnitude, however, the response of bone to mechanical loads is governed by a complex interaction of strain parameters including frequency, rate and cycle number [74–76]. For example, as vibration frequency increases, strain magnitude necessarily falls as peak velocity of each vibration cycle decreases [77]. Intuitively, if vibration loads are small in magnitude, the mechanism of action on bone is unlikely to be related to tissue deformation, and recent evidence confirms that to be the case [78]. In fact, vibration at 0.6 g that induced cortical surface strains of only 10 microstrain (με) increased bone formation rates in the proximal tibiae of mice [79•]. Further, the mere oscillation of a limb in anaesthetised mice at 0.3 g and 45 Hz for 10 min/day enhanced trabecular bone formation rate, percent of mineralising surface and morphology, as well as cortical thickness and area [80, 81].
The results of a microscale model of vibration loading of a vertebral body suggested that fluid shear stress on trabecular surfaces due to marrow movement governs the anabolic response of bone to a vibration stimulus [82]. However, others conclude, from finite element modelling, that vibration causes larger relative displacements of osteocyte-like cell nuclei than fluid shear and that gap junctional intracellular communication increases by 25 %, independent of vibration-induced fluid shear [83••]. The same group has now demonstrated that mesenchymal stem cell (MSC) response to vibration is may be driven by mechanical coupling between the cytoskeleton and the nucleus, inducing actin remodeling at the perinuclear domain [84]. It has also been reported that osteocytes respond to vibration by producing or downregulating soluble factors (COX-2, RANKL and PGE2) that result in the inhibition of osteoclast formation which reduces bone resorption [85].
While muscle activation may be enhanced by certain vibration protocols, there is considerable evidence to suggest that the response of bone to vibration is not dependent on a muscle response [78].
As is often the case in biological systems, it is possible that the mechanism of action of vibration on bone is driven through a number of parallel or serial pathways.
What Are the Applications and Indications?
Up to 85 % of nursing home residents may suffer from osteoporosis [86]. Female nursing home residents with low BMD have over twice the risk of osteoporotic fracture than those with higher BMD, and those independent in transfer have three times the risk [87]. Although the initial cost of an individual WBV device is not inconsequential, a single WBV device may be installed in a nursing home and utilised by many. The cost and risks of WBV are also considerably less than chronic drug therapy for osteoporosis.
Any therapy is only as effective as its adoption and adherence. A study of satisfaction and preference for low-magnitude WBV versus medication suggested that 95 % of elderly women (mean age 86) living in a Continuing Care Retirement community were satisfied or very satisfied with vibration therapy and that over half (57 %) of the sample preferred vibration treatment to medication (24 %) [88]. Compliance was 83 % over 6 months [88]. A separate cohort of 24 elderly nursing home residents demonstrated 96 % compliance with a WBV plus exercise protocol versus 86 % compliance with exercise alone [56].
Nursing home residents and others for whom physical disability limits exercise feasibility are therefore particularly suited to the application of WBV therapy for musculoskeletal outcomes.
What Dose Is Best?
It is apparent that increasing the magnitude of vibration acceleration beyond a recognised effective dose will not enhance the effect and may be unsafe (in other words, more is not better); however, only animal studies have examined dose-response to any appreciable degree. Bouts of 30 and 60 min of 0.3 g at 45 Hz were more effective for improving bone formation rate in mice than 15-min bouts, but increasing the number of bouts a day or partitioning a single daily bout into multiple shorter duration bouts did not improve the response [79•]. Others have also reported that the insertion of rest intervals does not potentiate the bone response to 15 min/day, 0.3 g, 45 Hz vibration in mice [18]. There is some evidence that a genetic predisposition to low bone mass may coincide with a greater response to vibration [89].
As animal observations cannot be directly applied to the human condition, considerably more data is required before therapeutic recommendations can be developed. Most human trials have been conducted using low to moderate vibration intensities (≤1 g) at or around a frequency of 30 Hz, for 10–20 min, 5–7 days a week, based on efficacy in animal studies and safety concerns. As results from those trials have been mixed, it remains unclear if such a dosage is optimal, and if not, which dosing parameters will be most efficacious or safe to modify. Minimal exposure appears to be required to stimulate a response, with benefits observed after as little as 2 min of daily exposure (15–20-year-old young women with low BMD and fracture) [90], or 15 min twice weekly in postmenopausal women [42].
It is important to note that there may be marked individual variations in response to different vibration frequencies [91], an effect that may reflect individual differences in transmission of the vibration stimulus to the body [17]. For this reason, the development of safe and effective dosimetry is unlikely to be straightforward, particularly for the frail elderly.
What Are the Risks?
As certain forms of occupational vibration are considered to be hazardous to the health [92–95], it is important to ensure that therapeutic applications do not replicate similar harmful vibration characteristics. In order to minimise occupational risk, the ISO has determined that a threshold of 0.3 g in the 20–50 Hz range is safe for human tolerance for up to 4 h at a time. Not all therapeutic devices have been developed to deliver vibration stimuli within those parameters.
Important differences exist between typical occupational and therapeutic vibrations however. Occupational exposures are normally less than 1 g but in the range of 3–10 Hz and can be very long duration. There is evidence from animal studies that deleterious bone effects (stimulation of resorption, impaired osteoid maturation) tend to occur at such frequencies (less than 10 Hz) [96••]. The effect may be a function of amplification of similar resonance frequencies of body segments of the small animals tested. In a human study of frequency-dependent transmissibility of vibration to ankles, knees and hips, frequencies of 10–90 Hz and accelerations of 0.04–19.3 g were examined [15]. It was observed that transmission of vibration to joints was virtually 100 % at resonant frequencies (ankle 10–40 Hz, knee 10–25 Hz, hip 10–20 Hz). Others have reported the highest vibration accelerations in the human body to occur at 20 Hz compared with 10 or 30 Hz [17]. The greatest accelerations will be observed at anatomical sites in the closest proximity to the vibration surface and when plate amplitudes are greatest (including when feet are positioned farthest away from the central axis of the teeter plate) [17].
A recent computational analysis of stress dispersion on a femur with multiple vibration displacements and frequencies concluded that stress levels during most vibration protocols are likely to be equivalent to walking and stair climbing [97]. The authors indicate, however, that as vibration displacement increased, so too did the peak stress on the femur suggesting displacement ranges between 2 and 12 mm may not be safe for individuals with low bone strength. Their lack of consideration of the influence of muscle loads on the model and the lack of data pertaining to other clinically relevant bones (spine) suggests their findings are less than conclusive with respect to the safety of all vibration loads.
It is important to note that WBV has been used with some success to treat low back pain [98], and reports of side effects from therapeutic WBV are uncommon. It is reasonable to conclude that at low intensity, WBV is safe, as the magnitude of forces are orders of magnitude below those that induce damage; however, more exposure-response data is needed for higher-intensity vibration [99], including long-term effects on multiple systems. Although ISO standards can provide some guidance, they do not specifically address the exposures and durations of vibration typically applied during therapeutic or training-related WBV.
Where to from Here?
The next steps in the field of vibration therapy is for the conduct of rigorously designed randomised controlled trials to determine optimum dose-response guidelines on which future vibration device development and therapy should be based. Those studies must include larger samples sizes, both sexes and relevant cohorts (those at increased risk of fracture) and utilise clearly described vibration protocols based on the prevailing best evidence.
At the very least, it will be important for researchers to speak the same language. Current terminology includes WBV, low-magnitude mechanical signals, non-invasive micromechanical stimulation, plantar-based vibration and vibration exercise. Many trials vary with respect to vibration protocol and the details reported (e.g. treatment time, number, frequency, amplitude, peak-to-peak displacement, maximum acceleration) and do not distinguish vibration from simultaneous exercise intervention. Without systematic testing of a variety of protocols, it will not be possible to develop optimal therapeutic guidelines, including the determination of minimum effective dose.
More quality human data is needed in virtually every area of this field.
Conclusions
There is preliminary evidence that WBV will improve bone mass and reduce risk of osteoporotic fracture by improving neuromuscular function. Regrettably, much of the human research on WBV has been of inadequate rigor, or so heterogeneous, that the ability to form strong conclusions with respect to efficacy or dose is limited. It must be assumed that the designs of many of the devices in the rapidly growing commercial market of WBV have therefore not been informed by a robust evidence base of safety and efficacy. While low-intensity vibrating plates (<1 g) appear to be safe, individuals with very low bone mass and prior fractures should exercise caution when considering the use of devices that deliver higher vibration accelerations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance • • Of major importance
Cummings SR, Black DM, Nevitt MC, Browner W, Cauley J, Ensrud K, et al. Bone density at various sites for prediction of hip fractures. The Study of Osteoporotic Fractures Research Group. Lancet. 1993;341(8837):72–5.
Kreisfeld R, Newson R. Hip fracture injuries. Adelaide: Australian Institute of Health and Welfare, National Injury Surveillance Unit2006 November Contract No.: 8.
Dargent-Molina P, Favier F, Grandjean H, Baudoin C, Schott AM, Hausherr E, et al. Fall-related factors and risk of hip fracture: the EPIDOS prospective study. [published erratum appears in Lancet 1996 Aug 10;348(9024):416]. Lancet. 1996;348(9021):145–9.
Wolfson L, Judge J, Whipple R, King M. Strength is a major factor in balance, gait, and the occurrence of falls. J Gerontol A Biol Sci Med Sci. 1995;50 Spec No:64–7.
Reginster JY. Antifracture efficacy of currently available therapies for postmenopausal osteoporosis. Drugs. 2011;71(1):65–78.
Compston JE, Seeman E. Compliance with osteoporosis therapy is the weakest link. Lancet. 2006;368(9540):973–4.
Eisman J, Clapham S, Kehoe L. Osteoporosis prevalence and levels of treatment in primary care: the Australian BoneCare Study. J Bone Miner Res. 2004;19(12):1969–75.
Rabenda V, Vanoverloop J, Fabri V, Mertens R, Sumkay F, Vannecke C, et al. Low incidence of anti-osteoporosis treatment after hip fracture. J Bone Joint Surg Am. 2008;90(10):2142–8.
Cooper C, Jakob F, Chinn C, Martin-Mola E, Fardellone P, Adami S, et al. Fracture incidence and changes in quality of life in women with an inadequate clinical outcome from osteoporosis therapy: the Observational Study of Severe Osteoporosis (OSSO). Osteoporos Int. 2008;19(4):493–501.
Nguyen ND, Eisman JA, Nguyen TV. Anti-hip fracture efficacy of biophosphonates: a Bayesian analysis of clinical trials. J Bone Miner Res. 2006;21(2):340–9.
Morin S, Rahme E, Behlouli H, Tenenhouse A, Goltzman D, Pilote L. Effectiveness of antiresorptive agents in the prevention of recurrent hip fractures. Osteoporos Int. 2007;18(12):1625–32.
Bemben D, Langdon D. Relationship between estrogen use and musculoskeletal function in postmenopausal women. Maturitas. 2002;2:119–27.
Pel JJ, Bagheri J, van Dam LM, van den Berg-Emons HJ, Horemans HL, Stam HJ, et al. Platform accelerations of three different whole-body vibration devices and the transmission of vertical vibrations to the lower limbs. Med Eng Phys. 2009;31(8):937–44.
Rubin C, Pope M, Fritton JC, Magnusson M, Hansson T, McLeod K. Transmissibility of 15-hertz to 35-hertz vibrations to the human hip and lumbar spine: determining the physiologic feasibility of delivering low-level anabolic mechanical stimuli to skeletal regions at greatest risk of fracture because of osteoporosis. Spine. 2003;28(23):2621–7.
Kiiski J, Heinonen A, Jarvinen TL, Kannus P, Sievanen H. Transmission of vertical whole body vibration to the human body. J Bone Miner Res. 2008;23(8):1318–25.
Matsumoto Y, Griffin M. Dynamic response of the standing human body exposed to vertical vibration: influence of posture and vibration magnitude. J Sound Vib. 1998;212(1):85–107.
Crewther B, Cronin J, Keogh J. Gravitational forces and whole body vibration: implications for prescription of vibratory stimulation. Phys Ther Sport. 2004;5(1):37–43.
Xie L, Jacobson JM, Choi ES, Busa B, Donahue LR, Miller LM, et al. Low-level mechanical vibrations can influence bone resorption and bone formation in the growing skeleton. Bone. 2006;39(5):1059–66.
Xie L, Rubin C, Judex S. Enhancement of the adolescent murine musculoskeletal system using low-level mechanical vibrations. J Appl Physiol. 2008;104(4):1056–62.
Flieger J, Karachalios T, Khaldi L, Raptou P, Lyritis G. Mechanical stimulation in the form of vibration prevents postmenopausal bone loss in ovariectomized rats. Calcif Tissue Int. 1998;63(6):510–4.
Chen GX, Zheng S, Qin S, Zhong ZM, Wu XH, Huang ZP, et al. Effect of low-magnitude whole-body vibration combined with alendronate in ovariectomized rats: a random controlled osteoporosis prevention study. PLoS ONE. 2014;9(5), e96181.
Hatori K, Camargos GV, Chatterjee M, Faot F, Sasaki K, Duyck J, et al. Single and combined effect of high-frequency loading and bisphosphonate treatment on the bone micro-architecture of ovariectomized rats. Osteoporos Int. 2015;26(1):303–13.
Rubin C, Xu G, Judex S. The anabolic activity of bone tissue, suppressed by disuse, is normalized by brief exposure to extremely low-magnitude mechanical stimuli. FASEB J. 2001;15(12):2225–9.
de Oliveira ML, Bergamaschi CT, Silva OL, Nonaka KO, Wang CC, Carvalho AB, et al. Mechanical vibration preserves bone structure in rats treated with glucocorticoids. Bone. 2010;46(6):1516–21.
Patel MJ, Chang KH, Sykes MC, Talish R, Rubin C, Jo H. Low magnitude and high frequency mechanical loading prevents decreased bone formation responses of 2T3 preosteoblasts. J Cell Biochem. 2009;106(2):306–16.
Luu YK, Capilla E, Rosen CJ, Gilsanz V, Pessin JE, Judex S, et al. Mechanical stimulation of mesenchymal stem cell proliferation and differentiation promotes osteogenesis while preventing dietary-induced obesity. J Bone Miner Res. 2009;24(1):50–61.
Rubin C, Turner AS, Bain S, Mallinckrodt C, McLeod K. Anabolism. Low mechanical signals strengthen long bones. Nature. 2001;412(6847):603–4.
Judex S, Boyd S, Qin YX, Turner S, Ye K, Muller R, et al. Adaptations of trabecular bone to low magnitude vibrations result in more uniform stress and strain under load. Ann Biomed Eng. 2003;31(1):12–20.
Rubin C, Recker R, Cullen D, Ryaby J, McCabe J, McLeod K. Prevention of postmenopausal bone loss by a low-magnitude, high-frequency mechanical stimuli: a clinical trial assessing compliance, efficacy, and safety. J Bone Miner Res. 2004;19(3):343–51.
Kiel DP, Hannan MT, Barton BA, Bouxsein ML, Sisson E, Lang T, et al. Low-magnitude mechanical stimulation to improve bone density in persons of advanced age: a randomized. Placebo Control Trial J Bone Miner Res. 2015;30(7):1319–28.
Slatkovska L, Alibhai SM, Beyene J, Hu H, Demaras A, Cheung AM. Effect of 12 months of whole-body vibration therapy on bone density and structure in postmenopausal women: a randomized trial. Ann Intern Med. 2011;155(10):668–79. W205.
Slatkovska L, Beyene J, Alibhai SM, Wong Q, Sohail QZ, Cheung AM. Effect of whole-body vibration on calcaneal quantitative ultrasound measurements in postmenopausal women: a randomized controlled trial. Calcif Tissue Int. 2014;95(6):547–56.
Gilsanz V, Wren TA, Sanchez M, Dorey F, Judex S, Rubin C. Low-level, high-frequency mechanical signals enhance musculoskeletal development of young women with low BMD. J Bone Miner Res. 2006;21(9):1464–74.
Ward K, Alsop C, Caulton J, Rubin C, Adams J, Mughal Z. Low magnitude mechanical loading is osteogenic in children with disabling conditions. J Bone Miner Res. 2004;19(3):360–9.
Torvinen S, Kannus P, Sievanen H, Jarvinen TA, Pasanen M, Kontulainen S, et al. Effect of 8-month vertical whole body vibration on bone, muscle performance, and body balance: a randomized controlled study. J Bone Miner Res. 2003;18(5):876–84.
Gusi N, Raimundo A, Leal A. Low-frequency vibratory exercise reduces the risk of bone fracture more than walking: a randomized controlled trial. BMC Musculoskelet Disord. 2006;7:92.
Ruan XY, Jin FY, Liu YL, Peng ZL, Sun YG. Effects of vibration therapy on bone mineral density in postmenopausal women with osteoporosis. Chin Med J (Engl). 2008;121(13):1155–8.
Lai CL, Tseng SY, Chen CN, Liao WC, Wang CH, Lee MC, et al. Effect of 6 months of whole body vibration on lumbar spine bone density in postmenopausal women: a randomized controlled trial. Clin Interv Aging. 2013;8:1603–9.
Liphardt AM, Schipilow J, Hanley DA, Boyd SK. Bone quality in osteopenic postmenopausal women is not improved after 12 months of whole-body vibration training. Osteoporos Int. 2015;26(3):911–20.
Cardinale M, Leiper J, Farajian P, Heer M. Whole-body vibration can reduce calciuria induced by high protein intakes and may counteract bone resorption: a preliminary study. J Sport Sci. 2007;25(1):111–9.
Verschueren SM, Roelants M, Delecluse C, Swinnen S, Vanderschueren D, Boonen S. Effect of 6-month whole body vibration training on hip density, muscle strength, and postural control in postmenopausal women: a randomized controlled pilot study. J Bone Miner Res. 2004;19(3):352–9.
Beck BR, Norling TL. The effect of 8 mos of twice-weekly low- or higher intensity whole body vibration on risk factors for postmenopausal hip fracture. Am J Phys Med Rehabil. 2010;89(12):997–1009.
Merriman H, Jackson K. The effects of whole-body vibration training in aging adults: a systematic review. J Geriatr Phys Ther. 2009;32(3):134–45.
Slatkovska L, Alibhai SM, Beyene J, Cheung AM. Effect of whole-body vibration on BMD: a systematic review and meta-analysis. Osteoporos Int. 2010;21(12):1969–80.
Mikhael M, Orr R, Fiatarone Singh MA. The effect of whole body vibration exposure on muscle or bone morphology and function in older adults: a systematic review of the literature. Maturitas. 2010;66(2):150–7.
Lau RWK, Liao LR, Yu FL, Teo T, Chung RCK, Pang MYC. The effects of whole body vibration therapy on bone mineral density and leg muscle strength in older adults: a systematic review and meta-analysis. Clin Rehabil. 2011;25(11):975–88.
Latham N, Anderson C, Bennett D, Stretton C. Progressive resistance strength training for physical disability in older people. Cochrane Database Syst Rev. 2003;2, CD002759.
Necking LE, Lundstrom R, Lundborg G, Thornell LE, Friden J. Skeletal muscle changes after short term vibration. Scand J Plast Reconstr Surg Hand Surg. 1996;30(2):99–103.
Roelants M, Verschueren SM, Delecluse C, Levin O, Stijnen V. Whole-body-vibration-induced increase in leg muscle activity during different squat exercises. J Strength Cond Res. 2006;20(1):124–9.
Torvinen S, Kannu P, Sievanen H, Jarvinen TA, Pasanen M, Kontulainen S, et al. Effect of a vibration exposure on muscular performance and body balance. Randomized cross-over study. Clin Physiol Funct Imaging. 2002;22(2):145–52.
Rehn B, Lidstrom J, Skoglund J, Lindstrom B. Effects on leg muscular performance from whole-body vibration exercise: a systematic review. Scand J Med Sci Sports. 2007;17(1):2–11.
Roelants M, Delecluse C, Goris M, Verschueren S. Effects of 24 weeks of whole body vibration training on body composition and muscle strength in untrained females. Int J Sports Med. 2004;25(1):1–5.
Roelants M, Delecluse C, Verschueren SM. Whole-body-vibration training increases knee-extension strength and speed of movement in older women. J Am Geriatr Soc. 2004;52(6):901–8.
Verschueren S, Roelents M, Delecluse C, Swinnen S, Vanderschueren D, Boonen S. Effect of 6-month whole body vibration training on hip density, muscle strength, and postural control in postmenopausal women: a randomized controlled pilot study. J Bone Miner Res. 2004;19(3):352–9.
Delecluse C, Roelants M, Verschueren S. Strength increase after whole-body vibration compared with resistance training. Med Sci Sports Exerc. 2003;35(6):1033–41.
Bautmans I, Van Hees E, Lemper JC, Mets T. The feasibility of whole body vibration in institutionalised elderly persons and its influence on muscle performance, balance and mobility: a randomised controlled trial [ISRCTN62535013]. BMC Geriatr. 2005;5:17.
Hawkey A, Griffiths K, Babraj J, Cobley JN. Whole body vibration training and its application to age-related performance decrements: an exploratory analysis. J Strength Cond Res. 2015 Jul 31.
Stengel SV, Kemmler W, Kalender WA, Engelke K. Effects of whole body vibration on bone mineral density and falls: results of the randomised controlled ELVIS study with postmenopausal women. Osteoporos Int. 2010 March 2010.
Furness TP, Maschette WE. Influence of whole body vibration platform frequency on neuromuscular performance of community-dwelling older adults. J Strength Cond Res. 2009;23(5):1508–13.
Di Giminiani R, Tihanyi J, Safar S, Scrimaglio R. The effects of vibration on explosive and reactive strength when applying individualized vibration frequencies. J Sports Sci. 2009;27(2):169–77.
Burke D, Hagbarth KE, Lofstedt L, Wallin B. The response of human muscle spindle endings to vibration during isometric contraction. J Physiol. 1976;261:695–711.
Matthews PB, Watson JD. Action of vibration on the response of cat muscle spindle Ia afferents to low frequency sinusoidal stretching. J Physiol. 1981;317:365–81.
Kawanabe K, Kawashima A, Sashimoto I, Takeda T, Sato Y, Iwamoto J. Effect of whole-body vibration exercise and muscle strengthening, balance, and walking exercises on walking ability in the elderly. Keio J Med. 2007;56(1):28–33.
Cheung WH, Mok HW, Qin L, Sze PC, Lee KM, Leung KS. High-frequency whole-body vibration improves balancing ability in elderly women. Arch Phys Med Rehabil. 2007;88(7):852–7.
Bruyere O, Wuidart MA, Di Palma E, Gourlay M, Ethgen O, Richy F, et al. Controlled whole body vibration to decrease fall risk and improve health-related quality of life of nursing home residents. Arch Phys Med Rehabil. 2005;86(2):303–7.
Yang F, King GA, Dillon L, Su X. Controlled whole-body vibration training reduces risk of falls among community-dwelling older adults. J Biomech. 2015 Jul 6.
Bogaerts A, Delecluse C, Claessens AL, Coudyzer W, Boonen S, Verschueren SM. Impact of whole-body vibration training versus fitness training on muscle strength and muscle mass in older men: a 1-year randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2007;62(6):630–5.
Sitja-Rabert M, Martinez-Zapata MJ, Fort Vanmeerhaeghe A, Rey Abella F, Romero-Rodriguez D, Bonfill X. Effects of a whole body vibration (WBV) exercise intervention for institutionalized older people: a randomized, multicentre, parallel, clinical trial. J Am Med Dir Assoc. 2015;16(2):125–31.
Leung KS, Li CY, Tse YK, Choy TK, Leung PC, Hung VW, et al. Effects of 18-month low-magnitude high-frequency vibration on fall rate and fracture risks in 710 community elderly—a cluster-randomized controlled trial. Osteoporos Int. 2014;25(6):1785–95. This large, cluster-randomised controlled trial examined the efficacy of 18 months of 20 min 0.3 g WBV, 5 days/week at 35 Hz, in 710 elderly men and women on fall rates and fracture risks and reported significantly fewer fall or fracture incidences in the treatment group.
Pollock RD, Martin CF, Newham DJ. The effect of whole body vibration on older people: a systemic review. PHYSICAL Therapy Reviews. 2012;17(2).
Sitja-Rabert M, Rigau D, Fort Vanmeerghaeghe A, Romero-Rodriguez D, Bonastre Subirana M, Bonfill X. Efficacy of whole body vibration exercise in older people: a systematic review. Disabil Rehabil. 2012;34(11):883–93.
Lam FMH, Lau RWK, Chung RCK, Pang MYC. The effect of whole body vibration on balance, mobility and falls in older adults: a systematic review and meta-analysis. Maturitas. 2012;72(3):206–13.
Duncan RL, Turner CH. Mechanotransduction and the functional response of bone to mechanical strain. Calcif Tissue Int. 1995;57(5):344–58.
Rubin CT, McLeod KJ. Promotion of bony ingrowth by frequency-specific, low-amplitude mechanical strain. Clin Orthop. 1994;298:165–74.
Turner CH, Owan I, Takano Y. Mechanotransduction in bone: role of strain rate. Am J Physiol. 1995;269(3 Pt 1):E438–42.
Rubin CT, Lanyon LE. Regulation of bone formation by applied dynamic loads. J Bone Joint Surg Am. 1984;66(3):397–402.
Uzer G, Manske SL, Chan ME, Chiang FP, Rubin CT, Frame MD, et al. Separating fluid shear stress from acceleration during vibrations in vitro: identification of mechanical signals modulating the cellular response. Cell Mol Bioeng. 2012;5(3):266–76.
Judex S, Rubin CT. Is bone formation induced by high-frequency mechanical signals modulated by muscle activity? J Musculoskelet Neuronal Interact. 2010;10(1):3–11.
Judex S, Koh TJ, Xie L. Modulation of bone’s sensitivity to low-intensity vibrations by acceleration magnitude, vibration duration, and number of bouts. Osteoporos Int. 2015;26(4):1417–28. This useful study examined acceleration magnitude and the number and duration of daily loading bouts in order to determine which of them modulated vibration efficacy. At a single frequency of 45 Hz, 1, 2 or 4 daily bouts were applied for 15, 30, or 60 min. All vibration combinations except 15 min/d at 0.3 g improved bone formation rates and 30 and 60 min bouts were more effective across the board than 15 min. Increasing the number of daily bouts or dividing the single daily bout into shorter bouts did not improve efficacy.
Garman R, Gaudette G, Donahue LR, Rubin C, Judex S. Low-level accelerations applied in the absence of weight bearing can enhance trabecular bone formation. J Orthop Res. 2007;25(6):732–40.
Garman R, Rubin C, Judex S. Small oscillatory accelerations, independent of matrix deformations, increase osteoblast activity and enhance bone morphology. PLoS ONE. 2007;2(7), e653.
Dickerson DA, Sander EA, Nauman EA. Modeling the mechanical consequences of vibratory loading in the vertebral body: microscale effects. Biomech Model Mechan. 2008;7(3):191–202.
Uzer G, Pongkitwitoon S, Ian C, Thompson WR, Rubin J, Chan ME, et al. Gap junctional communication in osteocytes is amplified by low intensity vibrations in vitro. PLoS ONE. 2014;9(3), e90840. This interesting paper advances what is known about the mechanism of action of WBV on bone, showing that mesenchymal stem cell response to vibration occurs via mechanical coupling between the nucleus and the cytoskeleton.
Uzer G, Thompson WR, Sen B, Xie Z, Yen SS, Miller S, et al. Cell mechanosensitivity to extremely low-magnitude signals is enabled by a LINCed nucleus. Stem Cells. 2015;33(6):2063–76.
Lau E, Al-Dujaili S, Guenther A, Liu DW, Wang LY, You LD. Effect of low-magnitude, high-frequency vibration on osteocytes in the regulation of osteoclasts. Bone. 2010;46(6):1508–15.
Zimmerman SI, Girman CJ, Buie VC, Chandler J, Hawkes W, Martin A, et al. The prevalence of osteoporosis in nursing home residents. Osteoporos Int. 1999;9(2):151–7.
Chandler JM, Duncan PW, Kochersberger G, Studenski S. Is lower extremity strength gain associated with improvement in physical performance and disability in frail, community-dwelling elders? Arch Phys Med Rehabil. 1998;79(1):24–30.
Hannan MT, Cheng DM, Green E, Swift C, Rubin CT, Kiel DP. Establishing the compliance in elderly women for use of a low level mechanical stress device in a clinical osteoporosis study. Osteoporos Int. 2004;15(11):918–26.
Judex S, Donahue LR, Rubin C. Genetic predisposition to low bone mass is paralleled by an enhanced sensitivity to signals anabolic to the skeleton. FASEB J. 2002;16(10):1280–2.
Demirbag D, Ozdemir F, Ture M. Effects of coffee consumption and smoking habit on bone mineral density. Rheumatol Int. 2006;26(6):530–5.
Cardinale M, Lim J. Electromyography activity of vastus lateralis muscle during whole-body vibrations of different frequencies. J Strength Cond Res. 2003;17(3):621–4.
Bovenzi M. Low back pain disorders and exposure to whole-body vibration in the workplace. Semin Perinatol. 1996;20(1):38–53.
Drerup B, Granitzka M, Assheuer J, Zerlett G. Assessment of disc injury in subjects exposed to long-term whole-body vibration. Eur Spine J. 1999;8(6):458–67.
Curry BD, Bain JL, Yan JG, Zhang LL, Yamaguchi M, Matloub HS, et al. Vibration injury damages arterial endothelial cells. Muscle Nerve. 2002;25(4):527–34.
Boshuizen HC, Bongers PM, Hulshof CT. Self-reported back pain in fork-lift truck and freight-container tractor drivers exposed to whole-body vibration. Spine (Phila Pa 1976). 1992;17(1):59–65.
Pasqualini M, Lavet C, Elbadaoui M, Vanden-Bossche A, Laroche N, Gnyubkin V, et al. Skeletal site-specific effects of whole body vibration in mature rats: from deleterious to beneficial frequency-dependent effects. Bone. 2013;55(1):69–77. This dose–response study of mature male rats examined the bone effects of differing vibration frequency (8, 52 and 90 Hz) at a constant acceleration (0.7 g). They observed the most beneficial effects from stimulation at 90 Hz and deleterious effects at 8 Hz. Although it is not known how those specific frequency responses translate to the human condition, they provide evidence that the nature of the vibration stimulus will be a vital element in the development of therapeutic WBV recommendations.
Ezenwa B, Yeoh HT. Multiple vibration displacements at multiple vibration frequencies stress impact on human femur computational analysis. J Rehabil Res Dev. 2011;48(2):179–89.
Rittweger J, Just K, Kautzsch K, Reeg P, Felsenberg D. Treatment of chronic lower back pain with lumbar extension and whole-body vibration exercise: a randomized controlled trial. Spine (Phila Pa 1976). 2002;27(17):1829–34.
Muir J, Kiel DP, Rubin CT. Safety and severity of accelerations delivered from whole body vibration exercise devices to standing adults. J Sci Med Sport. 2013;16(6):526–31.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Beck states that this article has no conflicts of interests.
Human and Animal Rights and Informed Consent
This article contains no studies with human or animal subjects performed by the author.
Additional information
This article is part of the Topical Collection on Skeletal Biology and Regulation
Rights and permissions
About this article
Cite this article
Beck, B.R. Vibration Therapy to Prevent Bone Loss and Falls: Mechanisms and Efficacy. Curr Osteoporos Rep 13, 381–389 (2015). https://doi.org/10.1007/s11914-015-0294-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-015-0294-8