Abstract
Regucalcin plays a pivotal role in regulating intracellular calcium homeostasis and consequently has a profound effect on multiple intracellular signal transduction pathways. The regucalcin transgenic rat displays pronounced bone loss, and bone marrow from these animals exhibits significantly elevated osteoclast formation. Consistent with these effects exogenous regucalcin promotes osteoclastogenesis in mouse bone marrow cultures, but interestingly regucalcin suppresses the differentiation and mineralization of MC3T3 osteoblast precursors. However, the molecular mechanisms involved are presently unclear. As the nuclear factor-kappa B (NF-κB) signal transduction pathway is critical to osteoclastogenesis but inhibitory of osteoblastogenesis, we hypothesized that regucalcin may promote osteoclastogenesis and suppress osteoblastogenesis upregulating NF-κB signal transduction. In this study, we examined the effect of regucalcin on receptor activator of NF-κB (RANK) ligand (RANKL) -induced osteoclast formation using the RAW264.7 monocytic cell line and osteoblast formation using the pre-osteoblastic cell line MC3T3. As expected, culture with exogenous regucalcin was found to enhance RANKL-induced osteoclastogenesis. Consistent with this effect regucalcin increased basal and RANKL-induced NF-κB activation as assessed by NF-κB luciferase assay. The capacity of regucalcin to augment RANKL-induced NF-κB activity was inhibited by menaquinone-7, a potent NF-κB antagonist, while the Erk inhibitor PD98059 and staurosporine had no effect, demonstrating a specific effect on NF-κB signaling. By contrast, regucalcin inhibited mineralization of MC3T3 cells and enhanced tumor necrosis factor-α (TNFα)-induced NF-κB activation. As with NF-κB induction in osteoclasts, NF-κB activation was abolished by addition of the NF-κB antagonist menaquinone-7, but not by PD98059 and staurosporine. Transforming growth factor-β (TGFβ) and bone morphogenic protein-2 (BMP2) are potent early commitment and late osteoblast differentiation factors, respectively, and both mediate their actions through the Smad-signal transduction pathway, a system that is extremely sensitive to and inhibited by TNFα-induced NF-κB. We consequently examined the effect of regucalcin on TGFβ and BMP2-induced Smad activation in the presence and absence of TNFα. While regucalcin had no effect on basal Smad activation by TGFβ and BMP2, it enhanced the suppressive effect of TNFα on both TGFβ- and BMP2-induced Smad activations. Taken together, present data suggest that regucalcin may induce bone loss in vivo by promoting osteoclasts and simultaneously suppressing osteoblasts through amplification of basal and/or cytokine-induced NF-κB activation. Regucalcin may have a role as a modulator in NF-κB activation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The calcium ion (Ca2+) plays an important role in the regulation of many cell functions. Ca2+ can regulate muscle contraction, neurotransmission, hormone secretion, cell mitosis, and gene expression. Furthermore, Ca2+ plays well-documented roles as a second messenger for mediating hormonal action [1]. Calcium signals mediate intracellular responses, through a family of calcium-binding proteins and protein kinase C. The effect of Ca2+ is amplified through calmodulin and protein kinase C [1–3].
Regucalcin was discovered in 1978 as a calcium-binding protein that does not contain the EF-hand motif of the calcium-binding domain [4–7]. The name regucalcin was proposed for this calcium-binding protein, due to its capacity to regulate Ca2+-dependent enzyme activation in liver cells [5]. There is growing evidence that regucalcin plays a multifunctional role as a regulatory protein in Ca2+ dependent and independent signaling processes in many cell types and that consequently the protein has a profound effect on multiple intracellular signal transduction pathways [reviewed in References 8–11].
Regucalcin and its gene (RGN) have been identified in over 15 species comprising the regucalcin family [7]. Comparison of the nucleotide sequences of regucalcin from vertebrate species shows high levels of evolutionary conservation in their coding region. The regucalcin gene is localized on the X chromosome, and the organization of the regucalcin gene consists of seven exons and six introns [7]. The expression of the regucalcin gene is regulated through calcium signaling itself through activation of various transcription factors including AP-1, NF1-A1, RGPR-p117, β-catenin, and other factors [7].
Regucalcin plays a pivotal role as a regulatory protein for calcium signaling in the regulation of intracellular Ca2+ homeostasis in many cell types through activation of membrane Ca2+ pumps [8–11]. Regucalcin has a suppressive effect on calcium signaling from the cytoplasm to the nucleus in proliferating cells due to hormonal stimulation. Regucalcin has also been demonstrated to localize in the nucleus, where it can inhibit Ca2+-dependent protein kinase and protein phosphatase activities, Ca2+-activated deoxyribonucleic acid (DNA) fragmentation, and DNA and ribonucleic acid (RNA) synthesis in the nucleus [9–11]. Moreover, overexpression of regucalcin suppresses cell death and apoptosis in response to various stimuli suggesting a role of endogenous regucalcin in the maintenance of cell homeostasis [9–11].
A regucalcin transgenic rat has been generated to determine the role of regucalcin in metabolic disorders [12]. Osteoporosis and hyperlipidemia have been documented in regucalcin transgenic rats, indicating a physiologic role of regucalcin in bone and lipid metabolism in vivo [12–14]. Regucalcin transgenic rats display loss of bone mass in young modeling animals (5 weeks old), a property that persists in aging (50 weeks old) animals [13]. Ex vivo bone marrow cultures from regucalcin transgenic rats show enhanced osteoclastogenesis [14–16] consistent with data demonstrating that exogenous regucalcin stimulates osteoclastogenesis in mouse bone marrow culture in vitro [17].
By contrast, exogenous regucalcin has a suppressive effect on the differentiation and mineralization of osteoblasts and downregulates Runx2 and alkaline phosphatase expression in pre-osteoblastic MC3T3-E1 cells in vitro [18]. Regucalcin is expressed in the bone marrow [13] and osteoblastic MC3T3-E1 cells [19, 20]. The expression of regucalcin mRNA in osteoblastic MC3T3-E1 cells is stimulated by parathyroid hormone, insulin-growth factor-I and 17β-estradiol and suppressed by 1,25-dihydroxyvitamin D3 and TNFα [19]. Regucalcin overexpression-induced bone loss thus appears to result from the enhancement of osteoclastic bone resorption and the suppression of osteoblastic bone formation.
RANKL plays a pivotal role in osteoclastogenesis by bone marrow monocytes, and numerous studies have demonstrated that NF-κB signal transduction, which is activated by RANKL, is a critical pathway for osteoclast development, function, and survival [21–26]. In contrast to the potent NF-κB-inducer, TNFα is well established to suppress osteoblast formation through multiple poorly understood actions [27–29].
Osteoblasts are derived from pluripotent bone marrow stromal cells, the progeny of mesenchymal stem cells that commit to the osteoblast lineage under the influence of environmental factors including osteogenic cytokines and growth factors. These include TGFβ, a potent early osteoblast commitment factor [30] and a potent recruiter of bone marrow stromal cells to sites of bone resorption [31]. BMPs further promote the differentiation of committed stromal cells into mature osteoblasts. Osteoblast differentiation is controlled by key stage-dependent transcription factors, including runt-related transcription factor 2 (Runx2) [32] and osterix [33].
BMPs stimulate bone formation as potent inducers of osteoblast differentiation and angiogenesis [34], while TGFβ is thought to play important roles in early osteoblast lineage commitment [30]. In the coupling of osteoclasts and osteoblasts, TGFβ release during bone resorption induces migration of bone marrow stromal cells to bone resorptive sites through a SMAD-dependent signaling pathway [31]. It has been recently demonstrated that one mechanism by which TNFα suppresses osteoblast differentiation is through NF-κB-mediated antagonism of TGFβ- and BMP2-induced SMAD signaling in differentiating osteoblasts [35]. These findings are consistent with the demonstration that NF-κB signaling upregulates SMAD7, an inhibitor of SMAD activation in osteoblastic cells [36] and that TNFα promotes systemic bone loss by promoting proteasomal degradation of bone morphogenetic signaling proteins through upregulation of SMAD ubiquitination regulatory factor 1 (Smurf1) [37].
In this study, we demonstrate that the capacity of regucalcin to stimulate osteoclast formation and resorption, and to suppress osteoblast differentiation and mineralization, may be explained by regucalcin’s tendency to stimulate basal and cytokine-induced NF-κB activation. Our data provide a unified mechanism, centered on NF-κB activation, to explain both resorptive and anti-anabolic actions of regucalcin.
Materials and methods
Materials
α-Minimal essential medium (α-MEM) and antibiotics (penicillin and streptomycin) were purchased from Invitrogen Corp. (Carlsbad, CA). Fetal bovine serum (FBS) was from Hyclone. Regucalcin was isolated from rat liver [4]. RANKL, TGFβ, TNFα, and BMP2 were from R&D Systems (Minneapolis, MN). Antibodies for Western blot were purchased from Santa Cruz Biotech. (Santa Cruz, CA). Menaquinone-7 (MK-7; vitamin K2) was obtained from J-Oil Mills (Tokyo, Japan). Mouse anti-poly-histidine antibody was obtained from RD Systems (Minneapolis, MN). PD98059, staurosporine, 5,6-dichloro-1-β-D-ribofuranosylbenzimidazole (DRB), and all other reagents were purchased from the Sigma Chemical Corporation, (St. Louis, MO) unless otherwise specified.
Cell culture
The monocytic cell line RAW264.7 and the pre-osteoblastic cell line MC3T3-E1, clone 14 (MC3T3), were purchased from the American Type Culture Collection (Manassas, VA) and cultured as previously described [38, 39].
Osteoclastogenesis assays and TRAP staining
RAW264.7 cells were cultured in 96-well plates in α-MEM supplemented with 10% FBS and 100 IU/ml penicillin, and 100 μg/ml streptomycin at a density of 1 × 104 cells/well. Cells were cultured for 6 days with RANKL (30 ng/ml) pre-incubated for 10 min with crosslinking anti-poly-histidine antibody (2.5 μg/ml) to induce osteoclast formation. Regucalcin was added in the range 0.01 to 100 nM. After 6 days of culture, the cells were fixed and stained for tartrate resistant acid phosphatase (TRAP) activity using a leukocyte acid phosphatase kit (Sigma). TRAP+ cells with three or more nuclei were defined as osteoclasts and were quantitated under light microscopy and five wells per group averaged.
Osteoblast differentiation assays and alizarin red-S staining
MC3T3 cells were plated and cultured for 72 h in α-MEM (1.0 ml/well) containing 10% FBS in 12-well dishes at a density of (1.0 × 105 cells per well). Medium was aspirated and changed to mineralization medium (α-MEM supplemented with 10% FBS, l-ascorbic acid (100 μg/ml), and 4 mM β-glycerophosphate) as previously described [38, 39]. Regucalcin or vehicle was added at a dose of 0.1, 1.0, or 10 nM and cells replenished with fresh medium every 3 days. At 21 or 28 days, cells were rinsed with PBS and calcium deposition was visualized by fixing the cells in 75% ethanol for 30 min at 4°C followed by staining with alizarin red-S (40 mM, pH 6.2) for 30 min at room temperature. Excess stain was removed by copious washing with distilled water. Plates were imaged using a flatbed scanner (Epson Perfection V600 Photo) and quantitated using Image J [38, 39].
NF-κB and Smad reporter constructs and luciferase assays
The NF-κB responsive reporter pNF-κB-Luc (BD Biosciences) and the SMAD responsive reporter pGL3-SMAD were used as previously described by us [33]. The SMAD reporter is responsive to both TGFβ- and BMP-induced SMADS. Briefly, reporter plasmids were transfected into RAW264.7 or MC3T3 cells (2 × 104 cells/well) using Lipofectamine 2000 reagent (Invitrogen) in α-MEM without FBS and antibiotics. Five hours later, the medium was changed to α-MEM containing 10% FBS plus antibiotics and cells treated with TNFα (MC3T3) or RANKL (RAW264.7) to stimulate NF-κB activity, or with TGFβ (1 ng/ml) or BMP2 (0.5 μg/ml) to stimulate SMAD activity and treated with or without TNFα. Parallel groups received vehicle or regucalcin in the dose range 0.01 to 100 nM. Cells were extracted with passive lysis buffer (Promega Corporation, Madison WI) 24 h later, and luciferase activity measured using the Luciferase Assay System of Promega, on a microplate luminometer (Turner Designs, Sunnyvale, CA, USA).
Statistical analysis
Statistical significance was determined using GraphPad InStat version 3 for Windows XP (GraphPad Software Inc. La Jolla, CA). Multiple comparisons were performed by one-way analysis of variance (ANOVA) with Tukey–Kramer multiple comparisons post-test for parametric data. P < 0.05 was considered statistically significant.
Results
Regucalcin dose-dependently stimulates osteoclast differentiation in vitro
Regucalcin is reported to stimulate osteoclastogenesis in vivo [13, 15, 16]. To further examine the mechanisms of regucalcin activity on osteoclastogenesis, we utilized the RAW264.7 monocytic cell line, which was induced to differentiate into osteoclasts by addition of the key osteoclastogenic cytokine RANKL. The effect of regucalcin on the differentiation of RAW264.7 cells into osteoclasts, was quantitated following staining of the cultures for TRAP, a specific marker of the osteoclast phenotype, 7 days later. Regucalcin significantly and dose-dependently stimulated osteoclastogenesis in the range 1 to 100 nM (Fig. 1A). Regucalcin at 10 and 100 nM concentration significantly enhanced RANKL (10 ng/ml) -induced osteoclastogenesis (Fig. 1B).
Effect of regucalcin (RGN) on osteoclastogenesis in RAW264.7 cells in the presence or absence of RANKL. RAW264.7 cells were cultured in the presence of either vehicle or RGN (0.1–100 nM) without (A) or with RANKL (B; 10 ng/ml). After 7 days of culture, the cells were fixed and stained for TRAP and TRAP+ cells with more than three nuclei counted as osteoclasts. Data sets represent the mean ± SD of five replicate wells and are representative of two independent experiments. a P < 0.05 versus white bar; b P < 0.001 versus white bar; c P < 0.05 versus RANKL only bar; d P < 0.01 versus RANKL only bar. All statistics were performed using one-way ANOVA with Tukey–Kramer multiple comparisons test
Regucalcin stimulates basal and RANKL-induced NF-κB activation in osteoclast precursors
To determine whether regucalcin has an effect on basal and RANKL-induced NF-κB activation in osteoclast precursors, RAW264.7 cells were transfected with an NF-κB luciferase reporter and treated with RANKL in the presence or absence of a dose range of 1 to 100 nM regucalcin. Addition of regucalcin with 1 to 100 nM was found to significantly stimulate basal NF-κB activity (Fig. 2). RANKL-induced NF-κB activity was significantly enhanced by regucalcin in a dose between 10 and 100 nM (Fig. 2).
Effect of regucalcin (RGN) on NF-κB luciferase activity in RAW264.7 cells. RAW264.7 cells were cultured for 24 h in the presence of either vehicle, RGN (A; 1.0–100 nM), RANKL (30 ng/ml), or RANKL (30 ng/ml) plus RGN (B; 0.01–100 nM). Data sets represent as the mean ± SD of five replicate wells and are representative of two independent experiments. a P < 0.05 versus white bar control; b P < 0.001 versus white bar control. All statistics were performed using one-way ANOVA with Tukey–Kramer multiple comparisons test
We next examined in RAW 264.7 cells whether regucalcin-induced NF-κB activity in the presence or absence of RANKL, was altered by PD98059, an inhibitor of ERK, staurosporine, an inhibitor of protein kinases, or DRB, an inhibitor of transcriptional activity (Fig. 3). The enhanced effect of regucalcin (10 nM) on RANKL (30 ng/ml) -increased NF-κB activity was not affected by PD98059 (Fig. 3A) or staurosorine (Fig. 3B), but was blocked by DRB (Fig. 3C).
Effect of kinase and transcriptional inhibitors on regucalcin-induced NF-κB luciferase activity in RAW274.2 cells. RAW264.7 cells were transfected with NF-κB luciferase reported (1 ng/ml) and treated with either vehicle, PD98059 (A; 0.1–10 μM), staurosporine (B; 0.01–1 μM), DRB (C; 0.1–10 μM), RGN (10 nM), or RANKL (30 ng/ml) plus RGN (10 nM). Luciferase activity was quantitated 24 h later. Data represent the mean ± SD of five replicate wells and are representative of two independent experiments. A a P < 0.01 versus white bar control; b P < 0.001 versus white bar control; c P < 0.05 versus white bar control; d P < 0.01 versus RANKL only (gray bar). P = NS: RANKL versus RANKL + PD98059; RANKL + RGN versus RANKL + RGN + PD98059. B a P < 0.001 versus white bar control; b P < 0.01 versus RANKL only (gray bar). C a P < 0.001 versus control (white bar); b P < 0.01 versus control (white bar); c P < 0.001 versus RANKL only (gray bar); d P < 0.01 versus RANKL only (gray bar). All statistics were performed using one-way ANOVA with Tukey–Kramer multiple comparisons test
Regucalcin suppresses osteoblast mineralization and osteoblast differentiation in vitro
Regucalcin is reported to suppress osteoblast differentiation and mineralization in vitro [18]. We consequently verified the capacity of regucalcin to enhance osteoblast mineralization and calcium deposition, visualized by alizarin red-S staining, in vitro and found pronounced suppression in the range of 1 and 10 nM in MC3T3 cells cultured for 28 (Fig. 4A) or 21 days (Fig. 4B).
Effect of regucalcin (RGN) on mineralization in pre-osteoblastic MC3T3-E cells. MC3T3 cells were cultured in mineralizing medium containing ascorbic acid (100 ng/ml) and 4 mM β-glycerophosphate in the presence of either vehicle or RGN (0.1–10 nM) for 28 (A) or 21 (B) days. C MC3T3 cells were cultured in mineralizing medium in the presence of either vehicle, TNFα (1 or 2.5 ng/ml of medium), RGN (1 nM) plus TNFα (1 ng/ml), or RGN (10 nM) plus TNFα (2.5 ng/ml) for 21 days. Cells were washed with PBS and stained with alizarin red stain for calcium deposition
Pathological concentrations of TNFα are established to promote bone loss in part through downregulation of osteoblastic bone formation in vivo in a number of conditions including postmenopausal osteoporosis and rheumatoid arthritis. TNFα potently inhibits bone formation in vivo under basal physiological conditions and acts in large measure through NF-κB activation [33, 38, 39]. Consequently, the capacity of regucalcin to enhance the suppressive action of TNFα on osteoblast differentiation in vitro was examined (Fig. 4C). The mineralization of MC3T3 cells was suppressed in the presence of TNFα (1 and 2.5 ng/ml) (Fig. 4C) as previously reported by us. Addition of regucalcin at the dose of 1 and 10 nM slightly enhanced the suppressive effect of TNFα on mineralization (Fig. 4C).
Regucalcin enhances TNFα-induced activation of NF-κB in osteoblast precursors in vitro
A major mechanism by which TNFα mediates its suppressive action on osteoblasts is through NF-κB activation [33, 38, 39]. Given the capacity of regucalcin to increase NF-κB activity in osteoclast precursors and to promote osteoblast differentiation in vitro, we next examined whether regucalcin may mediate its suppressive effects on bone formation in vivo through NF-κB activation in osteoblasts. We examined this in vitro using MC3T3 cells transiently transfected with an NF-κB luciferase reporter plasmid and treated with or without TNFα (1 ng/ml) and with regucalcin in the range 0.01 to 10 nM. Regucalcin (10 nM) significantly increased basal NF-κB activity and significantly enhanced NF-κB activation by TNFα (Fig. 5).
Effect of regucalcin (RGN) on TNFα (1 ng/ml)-stimulated NF-κB activity in MC3T3 pre-osteoblastic cells. Cells were cultured transfected with NF-κB reporter vector (1 ng/ml). Five hours later, the cells were treated with either vehicle, RGN (0.01–10 nM), TNFα (1 ng/ml), or TNFα (1 ng/ml) plus RGN (0.01–10 nM). Luciferase activity was quantitated 24 h later. Data points represent the mean ± SD of five replicate wells and are representative of two independent experiments. a P < 0.05 versus white bar control; b P < 0.001 versus white control bar only; c P < 0.001 versus TNFα gray bar. All statistics were performed using one-way ANOVA with Tukey–Kramer multiple comparisons test
To examine whether regucalcin enhances the effect of TNFα on NF-κB activity in MC3T3 cells by Erk, protein kinase, or transcriptional events in general, we used PD98059, staurosporin, and DRB, respectively. The enhanced effect with regucalcin (10 nM) on TNFα (1 ng/ml)-increased NF-κB activity was not changed in the presence of PD98059 (Fig. 6A) or staurosorine (Fig. 6B), but was blocked by DRB (Fig. 6C).
Effect of various inhibitors on the regucalcin (RGN)- or TNFα plus RGN-stimulated NF-κB luciferase activity in osteoblastic cells. MC3T3 cells were transfected with NF-κB luciferase reporter and cultured in the presence of either vehicle, PD98059 (A; 0.1–10 μM), staurosporine (B; 0.01–1 μM), or DRB (C; 0.1–10 μM) and luciferase activity quantified 24 h later. Data represented as the mean ± SD of five replicate wells and are representative of two independent experiments. A a P < 0.001 versus white bar control; b P < 0.001 versus TNFα only (gray bar); No difference with PD98059. B a P < 0.001 versus control (white bar); b P < 0.01 versus TNFα only (gray bar); No difference with staurosoprine. C a P < 0.001 versus white bar control; b P < 0.01 versus TNFα only (gray bar); d P < 0.001 versus white bar control; no difference with DRB. All statistics were performed using one-way ANOVA with Tukey–Kramer multiple comparisons test
Regucalcin enhances the inhibitory effect of TNFα on TGFβ-induced Smad activation
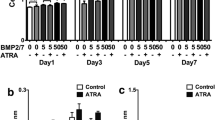
One mechanism by which TNFα likely inhibits osteoblast differentiation and activity under basal and pathological conditions is by antagonizing TGFβ- and BMP-mediated Smad signaling pathways [35, 38, 39]. We thus investigated the capacity of regucalcin to modulate the suppressive effect of TNFα on Smad-signal transduction. MC3T3 pre-osteoblasts were transiently transfected with a Smad responsive luciferase reporter and treated with TGFβ or BMP2 as a Smad-inducing stimulus, in the presence or absence of TNFα and/or a dose range of regucalcin from 0.01 to 10 nM. Regucalcin did not have a significant effect on basal Smad activity and TGFβ (Fig. 7A) and BMP2 (Fig. 7B)-induced Smad activation.
Effect of regucalcin (RGN) on TGFβ- or BMP2-stimulated Smad promoter activity in osteoblastic cells. Osteoblastic cells were transfected with Smad reporter vector and cultured with either RGN (1 or 10 nM), TGFβ (A; 1 ng/ml), or BMP2 (B; 0.5 μg/ml) with or without RGN (0.01–10 nM). Data represented as the mean ± SD of five replicate wells and are representative of two independent experiments. A a P < 0.001 versus white bar control; P = NS versus TNFα gray bar. B a P < 0.001 versus white bar control; P = NS versus TNFα gray bar. All statistics were performed using one-way ANOVA with Tukey–Kramer multiple comparisons test
While TNFα potently inhibited both basal and TGFβ (Fig. 8A)- and BMP2 (Fig. 8B)-induced Smad activation, regucalcin significantly and dose-dependently enhanced the suppressive activity of TNFα.
Effect of regucalcin (RGN) on the suppressive effect of TNFα on TGFβ- or BMP2-increased Smad reporter activity in osteoblastic cells. Osteoblastic cells were transfected with Smad reporter vector and treated with either vehicle, RGN (0.01–10 nM), TGFβ (A; 1 ng/ml), or BMP2 (B; 0.5 μg/ml). Luciferase activity was quantitated 24 h later. Data represented as the mean ± SD of five replicate wells and are representative of two independent experiments. A a P < 0.001 versus white bar control; b P < 0.001 versus TGFβ only gray bar; c P < 0.01 versus TGFβ + TNFα. B a P < 0.00 versus white bar control; b P < 0.001 versus TNFα gray bar; c P < 0.01 versus BMP2 + TNFα. All statistics were performed using one-way ANOVA with Tukey–Kramer multiple comparisons test
Enhancing effect of regucalcin on RANKL- or TNFα-induced activation of NF-κB is antagonized by MK-7
We next examined the effect of MK-7, a specific inhibitor for NF-κB activation [38], on the enhancing effect of regucalcin on RANKL- or TNFα-induced activation of NF-κB in RAW264.7 cells (Fig. 9A) and MC3T3 cells (Fig. 9B). The effect of RANKL (30 ng/ml) or TNFα (1 ng/ml) in increasing NF-κB activity in the presence or absence of regucalcin (10 nM) was significantly inhibited by MK-7 (10 μM). The stimulatory effect of regucalcin (10 nM) on basal NF-κB activity in RAW264.7 cells (Fig. 9A) and MC3T3 cells (Fig. 9B) was also suppressed by MK-7.
Effect of menaquinone-7 (MK-7), a potent antagonist for NF-κB activation on regucalcin (RGN)-enhanced NF-κB luciferase activity. A RAW267.4 cells or MC3T3 osteoblastic cells (B) were transfected with NF-κB luciferase reporter and cultured in the presence of either vehicle, RANKL (A; 30 ng/ml), TNFα (B; 1 ng/ml) with or without RGN (10 nM) or MK-7 (10 μM) and assayed for luciferase activity 24 h later. Data represented as the mean ± SD of five replicate wells and are representative of two independent experiments. A a P < 0.001 versus control (white bar); b P < 0.01 versus RANKL plus RGN (gray bar). B a P < 0.001 versus control (white bar); b P < 0.01 versus TNFα plus RGN (gray bar). All statistics were performed using one-way ANOVA with Tukey–Kramer multiple comparisons test
Discussion
Regucalcin is known to play a multifunctional role as a regulatory protein in intracellular signaling systems in various cell types [10, 11]. It has been recently found that osteoporosis and hyperlipidemia are induced in regucalcin transgenic rats in vivo [12–14] and that bone marrow cells from regucalcin transgenic rats undergo elevated osteoclast formation in the presence of macropharge colony-stimulating factor (M-CSF) and RANKL ex vivo [15, 16]. Exogenous regucalcin stimulates osteoclastogenesis in culture of bone marrow cells obtained from wild-type rats in vitro [17]. In addition, exogenous regucalcin has a suppressive effect on mineralization and differentiation in MC3T3-E1 cells in vitro [18]. Bone loss by overexpression of regucalcin in vivo is thus a consequence of both elevated osteoclastogenesis and suppressed osteoblastogenesis [13], suggesting a common mechanism. In this study, we demonstrate that the molecular mechanism by which regucalcin promotes osteoclastogenesis and suppresses osteoblastogenesis is related to a stimulatory effect on NF-κB signaling.
NF-κB signal transduction is a critical pathway for osteoclast development, function, and survival [21–25]. Additional support for a role of NF-κB in osteoclast formation and activity come from studies showing that the NF-κB subunit RelB plays a key role in osteoclast differentiation [24], while the p65 NF-κB subunit prevents JNK-mediated apoptosis during RANKL-induced commitment to the osteoclast phenotype [23]. Moreover, the p65 NF-κB subunit is reported to inhibit vitamin D-stimulated osteocalcin transcription in osteoblastic cells [27], and the potent NF-κB-inducer TNF-α is well established to suppress osteoblast formation through multiple poorly understood actions [21, 22].
Exogenous regucalcin stimulated basal osteoclastogenesis and NF-κB activity and enhanced RANKL-stimulated osteoclastogenesis and NF-κB activity in RAW267.4 cells. This finding suggests that exogenous regucalcin stimulates osteoclastogenesis through NF-κB activation in RAW264.7 cells.
The protein kinase C family enzyme has a role in the regulation of osteoclast formation and function potentially by participating in the ERK signaling pathway downstream of M-CSF and RANKL [40]. The enhancing effect of regucalcin on RANKL-induced increase in NF-κB activation was not inhibited by PD98059, an inhibitor of ERK, or staurosporine, a general inhibitor of protein kinases, suggesting that regucalcin stimulation is not related to the activation of kinase.
Culture with exogenous regucalcin was found to suppress differentiation and mineralization in osteoblastic MC3T3 cells, and it stimulated basal NF-κB activity and enhanced TNFα-increased NF-κB activity in the cells. The potent NF-κB-inducer TNFα is demonstrated to suppress osteoblast formation [33]. This finding suggests that exogenous regucalcin suppress osteoblastogenesis through NF-κB activation in MC3T3 cells.
The enhancing effect of regucalcin on TNFα-induced increase in NF-κB activity was not inhibited by PD98059 and staurosporine. This result suggests that the stimulatory effect of regucalcin is not related to kinase activity.
BMPs are potent inducers of osteoblast differentiation and angiogenesis and stimulate bone formation [30]. TGFβ plays important roles in early osteoblast lineage commitment [31]. In the coupling of osteoclasts and osteoblasts, TGFβ release during bone resorption induces migration of bone marrow stromal cells to bone resorptive sites. The effects of BMPs and TGFβ are mediated through a SMAD-dependent signaling pathway [30, 31]. Exogenous regucalcin did not have an effect on basal Smad activity in MC3T3 cells and it was not changed by TGFβ- or BMP2-increased Smad activity in the cells. This result suggests that the suppressive effect of regucalcin on osteoblastogenesis is not related to direct suppression of Smad activity.
One mechanism by which TNFα suppresses osteoblast differentiation is through NF-κB-mediated antagonism of TGFβ- and BMP2-induced SMAD signaling in differentiating osteoblasts [35]. This is consistent with the demonstration that NF-κB signaling upregulates SMAD7, an inhibitor of SMAD activation in osteoblastic cells [36] and that TNFα promotes systemic bone loss by promoting proteasomal degradation of bone morphogenetic signaling proteins through upregulation of SMAD Smurf1 [37].
The stimulatory effect of TGFβ or BMP2 on Smad activity was markedly suppressed in the presence of TNFα, and the suppressive effect of TNFα was found to be upregulated in the presence of regucalcin. This may involve exogenous regucalcin enhancing TNFα-induced NF-κB activation in MC3T3 cells. The suppressive effect of exogenous regucalcin on differentiation and mineralization in MC3T3 cells may be partly related to upregulation of TNFα-induced inhibition of Smad signaling through NF-κB activation.
At present, the mechanism by which exogenous regucalcin stimulates basal and RANKL- or TNFα-induced increase in NF-κB activity is unknown. Vitamin K2 (menaquinone-7) action on osteoblast and osteoclast formation and activity is accomplished by downregulating basal and cytokine-induced NF-κB activation, by increasing IκB mRNA, in a γ-carboxylation-independent manner [38]. We found that the stimulatory effect of exogenous regucalcin on basal and RANKL- or TNFα-induced increase in NF-κB activity was completely abolished by culture with MK-7 in RAW264.7 and MC3T3 cells. In addition, the enhancing effect of regucalcin on the cytokine-induced NF-κB activation in RAW267.4 and MC3T3 cells was completely prevented after culture with DRB, an inhibitor of transcriptional activity through RNA polymerase II inhibition, suggesting that exogenous regucalcin modulates the gene expression that is involved in NF-κB activation.
Exogenous regucalcin can bind to the plasma membranes of liver cells [40]. It is possible that regucalcin binds the plasma membranes of RAW264.7 and MC3T3 cells. The receptor protein RANK (receptor activator of NF-κB) is expressed on the surface of osteoclast progenitors [41, 42]. The interaction of RANKL with its receptor RANK leads to the recruitment of the signaling adaptor molecules TRAFs (TNF receptor-associated factors) to the receptor complex and the activation of NF-κB and c-Jun N-terminal kinase (JNK) [42, 43]. It is speculated that exogenous regucalcin binds the surface of pre-osteoclast and osteoblastic cells and activates TRAFs and that regucalcin modulates the effect of RANKL and TNFα on TRAFs. It is possible, moreover, that regucalcin upregulates TNF-α receptor and/or RANK expressions. In addition, it is well known that endogenous regucalcin plays a role in the regulation of intracellular Ca2+ homeostasis in various cell types [5, 8, 10]. We cannot exclude the possibility that exogenous regucalcin acts on calcium and other signaling systems in osteoblastic cells and RAW267.4 cells.
In conclusion, this study demonstrates that exogenous regucalcin stimulates osteoclastogenesis and suppresses osteoblastogenesis through NF-κB activation in vitro. This finding provides one mechanism by which overexpression of regucalcin induces bone loss in vivo. Regucalcin may play a role as a cytokine in the regulation of bone homeostasis.
References
Kraus-Friedman N, Feng L (1996) The role of intracellular Ca2+ in the regulation of gluconeogenesis. Metabolism 48:389–403
Cheung WY (1980) Calmodulin plays a pivotal role in cellular regulation. Science 202:19–27
Nishizuka Y (1986) Studies and perspectives of protein kinase C. Science 233:305–312
Yamaguchi M, Yamamoto T (1978) Purification of calcium binding substance from soluble fraction of normal rat liver. Chem Pharm Bull 26:1915–1918
Yamaguchi M (1992) A novel Ca2+-binding protein regucalcin and calcium inhibition. Regulatory role in liver cell function. In: Kohama K (ed) Calcium inhibition. Japan Science Society Press, Tokyo, pp 19–41
Shimokawa N, Yamaguchi M (1993) Molecular cloning and sequencing of the cDNA coding for a calcium-binding protein regucalcin from rat liver. FEBS Lett 327:251–255
Yamaguchi M (2011) The transcriptional regulation of regucalcin gene expression. Mol Cell Biochem 346:147–171
Yamaguchi M (2000) Role of regucalcin in calcium signaling. Life Sci 66:1769–1780
Yamaguchi M (2000) The role of regucalcin in nuclear regulation of regenerating liver. Biochem Biophys Res Commun 276:1–6
Yamaguchi M (2005) Role of regucalcin in maintaining cell homeostasis and function. Int J Mol Med 15:372–389
Yamaguchi M (2011) Regucalcin and cell regulation: role as a suppressor protein in signal transduction. Mol Cell Biochem 353(1–2):101–137
Yamaguchi M (2010) Regucalcin and metabolic disorders: osteoporosis and hyperlipidemia are induced in regucalcin transgenic rats. Mol Cell Biochem 341:119–133
Yamaguchi M, Misawa H, Uchiyama S, Morooka Y, Tsurusaki Y (2002) Role of endogenous regucalcin in bone metabolism: bone loss is induced in regucalcin transgenic rats. Int J Mol Med 10:377–383
Yamaguchi M, Igarashi A, Uchiyama S, Sawada N (2004) Hyperlipidemia is induced in regucalcin transgenic rats with increasing age. Int J Mol Med 14:647–651
Yamaguchi M, Sawada N, Uchiyama S, Misawa H, Ma ZJ (2004) Expression of regucalcin in rat bone marrow cells: involvement of osteoclastic bone resorption in regucalcin transgenic rats. Int J Mol Med 13:437–443
Uchiyama S, Yamaguchi M (2004) Bone loss in regucalcin transgenic rats: enhancement of osteoclastic cell formation from bone marrow of rats with increasing age. Int J Mol Med 14:451–455
Yamaguchi M, Uchiyama S (2005) Regucalcin stimulates osteoclast-like cell formation in mouse marrow cultures. J Cell Biochem 94:794–803
Yamaguchi M, Kobayashi M, Uchiyama S (2005) Suppressive effect of regucalcin on cell differentiation and mineralization in osteoblastic MC3T3-E1 cells. J Cell Biochem 96:543–554
Otomo Y, Yamaguchi M (2006) Regulatory effect of exogenous regucalcin on cell function in osteoblastic MC3T3–E1 cells: involvement of intracellular signaling factor. Int J Mol Med 18:321–327
Yamaguchi M, Otomo Y, Uchiyama S, Nakagawa T (2008) Hormonal regulation of regucalcin mRNA expression in osteoblastic MC3T3-E1 cells. Int J Mol Med 21:771–775
Boyce BF, Xing L, Franzoso G, Siebenlist U (1999) Required and nonessential functions of nuclear factor-kappa B in bone cells. Bone 25:137–139
Hall TJ, Schaeublin M, Jeker H, Fuller K, Chambers TJ (1995) The role of reactive oxygen intermediates in osteoclastic bone resorption. Biochem Biophys Res Commun 207:280–287
Varia S, Alhawagri M, Anwisye I, Kitaura H, Faccio R, Novack DV (2008) RelA/p65 promotes osteoclast differentiation by blocking a RANKL-induced apoptotic JNK pathway in mice. J Clin Invest 118:2088–2097
Varia S, Johanson T, Hirbe AC, Alhawagri M, Anwisye I, Sammut B, O’Neal J, Zou W, Weilbaecher KN, Faccio R, Novack DV (2008) RelB is the NF-kappaB subunit downstream of NIK responsible for osteoclast differentiation. Proc Natl Acad Sci USA 105:3897–3902
Liu J, Wang S, Zhang P, Said-Al-Naief N, Michalek SM, Feng X (2009) Molecular mechanism of the bifunctional role of lipopolysaccharide in osteoclastogenesis. J Biol Chem 284:12512–12523
Iotsova V, Caamano J, Loy J, Yang Y, Lewin A, Bravo R (1997) Osteopetrosis in mice lacking NF-kappaB1 and NF-kappaB2. Nat Med 3:1285–1289
Lu X, Farmer P, Rubin J, Nanes MS (2004) Integration of the NF-kappaB p65 subunit into the vitamin D receptor transcriptional complex: identification of p65 domains that inhibit 1,25-dihydroxyvitamin D3-stimulated transcription. J Cell Biochem 92:8330–8848
Gilbert LC, Rubin J, Nanes MS (2005) The p55 TNF receptor mediates TNF inhibition of osteoblast differentiation independently of apoptosis. Am J Physiol Endocrinol Metab 288:E1011–E1018
Nanes MS (2003) Tumor necrosis factor-alpha: molecular and cellular mechanism in skeletal pathology. Gene 321:1–15
Janssens K, Ten Dijke P, Janssens S, Van Hul W (2005) Transforming growth factor-beta1 to the bone. Endocr Rev 26:743–774
Tang Y, Wu X, Lei W, Pang L, Wan C, Shi Z, Zhao L, Nagy TR, Peng X, Hu J, Feng X, Van Hul W, Wan M, Cao X (2009) TGF-beta1-induced migration of bone mesenchymal stem cells couples bone resorption with formation. Nat Med 15:757–765
Ducy P, Zhang R, Geoffroy V, Ridall AL, Karsenty G (1997) Osf2/Cbfa1: a transcriptional activator of osteoblast differentiation. Cell 89:747–754
Nakashima K, Zhou X, Kunkel G, Zhang Z, Deng JM, Behringer RR et al (2002) The novel zinc finger-containing transcription factor osterix is required for osteoblast differentiation and bone formation. Cell 108:17–29
Zhang F, Qiu T, Wu X, Wan C, Shi W, Wang Y, Chen JG, Wan M, Clemens TL, Cao X (2009) Sustained BMP signaling in osteoblasts stimulates bone formation by promoting angiogenesis and osteoblast differentiation. J Bone Miner Res 24:1224–1233
Li Y, Li A, Strait K, Zhang H, Nanes MS, Weitzmann MN (2007) Endogenous TNFα lowers maximum peak bone mass and inhibits osteoblastic Smad activation, through NF-kappaB. J Bone Miner Res 22:646–655
Eliseev RA, Schwarz EM, Zuscik MJ, O’Keefe RJ, Drissi H, Rosier RN (2006) Smad7mediates inhibition of Saos2 osteosarcoma cell differentiation by NFkappaB. Exp Cell Res 312:40–50
Guo R, Yamashita M, Zhang Q, eZjou Q, Chen D, Reynolds DG, Awad HA, Yanoso L, Zhao L, Schwarz EM, Zhang YE, Boyce BF, Xing L (2008) Ubiquitin ligase Smurf1 mediates tumor necrosis factor-induced systemic bone loss by promoting proteasomal degradation of bone morphogenetic signaling proteins. J Biol Chem 283:23084–23092
Yamaguchi M, Weitzmann MN (2011) Vitamin K2 stimulates osteoblastogenesis and suppresses osteoclastogenesis by suppressing NF-κB activation. Int J Mol Med 27:3–14
Yamaguchi M, Weitzmann MN (2011) Zinc stimulates osteoblastogenesis and suppresses osteoclastogenesis by antagonizing NF-κB activation. Mol Cell Biochem 355:179–186
Yamaguchi M, Mori S, Kato S (1988) Calcium-binding protein regucalcin is an activator (Ca2+–Mg2+) -adenosine triphosphatase in the plasma membranes of rat liver. Chem Pharm Bull 36:3532–3539
Zaidi M, Blair HC, Moonga BS, Abe E, Huang CLH (2003) Osteoclastogenesis, bone resorption, and osteoblast-based therapeutics. J Bone Miner Res 18:599–609
Anderson DM, Maraskovsky E, Billingsley WL, Dougall WC, Tometsko ME, Roux ER, Teepe MC, DuBose RF, Cosman D, Gailibert L (1997) A homologue of the TNF receptor and its ligand enhance T-cell growth and dendritic-cell function. Nature 390:175–195
Lee ZH, Kwack K, Kim KK, Lee SH, Kim HH (2000) Activation of c-Jun N-terminal kinase and activator protein 1 by receptor activator of NF-κB. Mol Pharmacol 58:1536–1545
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yamaguchi, M., Neale Weitzmann, M. & Murata, T. Exogenous regucalcin stimulates osteoclastogenesis and suppresses osteoblastogenesis through NF-κB activation. Mol Cell Biochem 359, 193–203 (2012). https://doi.org/10.1007/s11010-011-1014-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-011-1014-z