Abstract
Purpose of Review
Management of metastatic head and neck squamous cell cancers (HNSCC) can be challenging. This review gives an insight of current treatment options for patients with synchronous metastatic HNSCC and suggests a therapeutic algorithm.
Recent Findings
With the rise of novel therapeutic techniques and medications, many treatment options for both locoregional and distant metastatic disease have become available. The evolving paradigm of metastatic disease now integrates the concept of oligometastatic disease. On top of systemic treatments, patients with low metastatic burden can benefit from curative approaches such as local therapies (surgery, radiotherapy) directed to either primary tumour and distant metastasis. However, data integrating these considerations in the management of metastatic HNSCC is still lacking.
Summary
Based on this algorithm, we can provide a tailored treatment to each patient with synchronous metastatic HNSCC, according to their age, general condition and metastatic burden.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite improvements in locoregional control due to chemotherapy, radiation therapy and surgical techniques, little improvements have been achieved in terms of survival rates for head and neck cancers, with head and neck squamous cell carcinoma (HNSCC) being the most frequent histologic type (90%). Distant metastasis rates, both synchronous and metachronous, are reported to be between 4 and 24% [1]. Median overall survival in metastatic HNSCC is 10 months [2]. Distant metastases from HNSCC are defined by secondary lesions located below the claviculas. Lungs are the most common sites of metastatic spread, followed by bone and liver [1, 3]. Validated clinical risk factors for distant metastasis in HNSCC are tumour site, size and nodal status, according to the UICC staging system. Other factors include locoregional control, histological grade or differentiation and age at diagnosis [4, 5]. Human papillomavirus (HPV) infection, mostly related to oral sex, is now recognized as an emerging risk factor [6, 7] for developing a unique subset of HNSCC, particularly those arising from the oropharynx. However, a better prognosis is reported for patients with HPV-positive oropharyngeal tumours compared to those with HPV-negative tumours [8]. Current data suggest HPV-positive tumours confer a survival advantage in distant metastatic disease [9], even though distant metastatic rate is equivalent among the two groups [10]. According to a series of retrospective studies, HPV-positive tumours display an atypical pattern of distant metastatic recurrence including the involvement of multiple organs and unusual sites (skin, intra-abdominal lymph nodes, brain) [10, 11]. These observations raise a need to implement a unique diagnostic and therapeutic strategy for this particular subset of patients. The presence of distant metastases is associated with a poor outcome and the optimal treatment strategy in this population is debatable. For patients with metastatic disease, the association of systemic therapy and supportive care remains the standard-of-care. The main objectives are to prolong survival and/or alleviate symptoms. However, the rise of the concept of oligometastatic disease described by Hellman and Weichselbaum [12, 13] is changing treatment paradigms, with better prognosis and even possible cure. Aggressive treatment modalities such as surgery or radiation therapy are now increasingly used based on prolonged survival in oligometastatic diseases [14]. This article reviews the current treatment patterns in the management of previously untreated HNSCC patients with distant synchronous metastases and suggests a therapeutic algorithm based on individual features for an optimal and personalized continuum of care.
Systemic Treatment
The EXTREME regimen, a combination of cetuximab, platinum (cisplatin or carboplatin) and 5-fluorouracile (5-FU) is the standard first-line treatment for metastatic HNSCC patients, as it resulted in a 2.7 months increase of median survival and 2.3 months prolongation of PFS compared to chemotherapy without cetuximab [2]. The addition of cetuximab to platinum-based chemotherapy led to a significant reduction in pain, improved eating and speech, thereby positively impacting social functioning and quality of life for patients receiving this treatment. The toxicity profile of the EXTREME regimen has been shown to be predictable and manageable [2].
A variation of the EXTREME protocol, the TPEx regimen, in which 5-FU is replaced by a taxane, showed promising activity in a phase II trial by Guigay et al., as first-line treatment in fit patients with metastatic HNSCC. The primary endpoint was met significantly with an objective response rate (ORR) of 44.4%. Median OS and PFS were respectively 14 months and 6.2 months [15]. The use of taxanes instead of 5-FU is an interesting therapeutic option since fluoropyrimidines present potential high toxicity in case of dihydropyrimidine deshydrogenase (DPD) deficiency, resulting in accumulation of FU in the blood. Severe toxicities (grades 3–4) occur in 10 to 40% of patients [16]. Further studies are needed to compare TPEx vs. EXTREME regimen in this population to determine which regimen should be chosen as first-line treatment. An ongoing phase II trial led by GORTEC is comparing TPEx vs. EXTREME in the first-line treatment of recurrent or metastatic HNSCC (NCT02268695), with OS as the primary endpoint and ORR. A variation of TPEx as first-line treatment is the PCE regimen (combination of paclitaxel, carboplatin and cetuximab), which also showed promising outcomes and tolerable toxicity in a phase II study [17]. For patients not fit enough for EXTREME, various options are used in clinical practice, including cetuximab or monochemotherapy such as methotrexate, docetaxel, paclitaxel, cisplatin, carboplatin and 5-FU [18, 19]. However, there are no data showing benefit from any of these treatments (monotherapy or combination) in controlled randomized trials. First-line cetuximab vs. methotrexate monotherapy is currently being evaluated in the unfit elderly (≥ 70 years of age) with metastatic HNSCC in a randomized phase III trial (ELAN-UNFIT, NCT01884623).
Recently there have been advances in immunotherapy in various tumour types including HNSCC. The understanding of the molecular mechanisms and immune environment in HNSCC supports the potential efficacy of such an option [20]. Following high response rates observed with pembrolizumab and nivolumab, these molecules have been approved in the US for patients with recurrent (including metastatic) HNSCC in second-line treatment [21, 22]. Ongoing phase III trials are currently investigating the role of immune check point inhibitors such as nivolumab (CheckMate 651, NCT02741570), pembrolizumab (KEYNOTE-048, NCT02358031) and durvalumab (KESTREL, NCT02551159) as first-line treatments for fit patients with HNSCC recurrent or metastatic disease. For all trials, the EXTREME regimen was chosen as the reference arm. In the KEYNOTE-048 study, pembrolizumab significantly improved OS over EXTREME, with favourable safety in an interim analysis presented during the ESMO 2018 congress.
Local Treatment of Metastatic Sites
On top of general control of the disease enabled by systemic treatment, local control of the secondary sites may be improved by metastasis-directed therapies like surgical resection, stereotactic radiation, and to a lesser extent radiofrequency ablation and cryotherapy. These treatment options aim at limited metastatic stages, as an alternative or in combination with systemic therapies. Delaying systemic treatment may eventually be discussed in case of low metastatic burden or multiple comorbidities. However, determining the advantages or superiority of this approach compared to palliative systemic therapy or best supportive care is challenging because of the predominantly retrospective nature of existing data.
Surgical Resection of Lung Metastases
Surgery in the management of oligometastatic disease is now standard practice in almost all tumour types, with the aim of improving local control and overall survival. In patients with a solitary pulmonary lesion, to differentiate a second primary lung tumour from metastatic disease is often challenging. Wedge resection of metastatic nodules in the lung is therefore appropriate in such situations. Selection criteria are good performance status (PS), absence of extra-pulmonary metastases, control of the primary tumour, possibility of complete resection and adequate respiratory function [23]. A systematic review of 47 retrospective studies was conducted into meta-analysis of survival rates of 387 patients with metastatic HNSCC following lung metastasectomy. Five-year OS rate was 29% [24]. The most commonly reported poor prognostic factors following lung metastasectomy in patient with HNSCC include age greater than 50 or 60 [25, 26], disease-free interval less than 2 years [25], oral cavity primary tumour [24, 27], lymph node metastasis [24, 27] and squamous cell histology [26]. Following pulmonary metastasectomy in HNSCC, the decision of undertaking adjuvant systemic therapy or observation only is still a matter of debate.
Stereotactic Body Radiation Therapy of Lung Metastases
Stereotactic body radiation therapy (SBRT), also referred to as stereotactic ablative radiotherapy (SABR), is another modality for treating oligometastatic disease with the goal of achieving high rates of tumour control with minimal morbidity and non-invasively. This technique allows precise delivery of high radiation dose, defined as “ablative dose”, with a maximum sparing of normal tissue using a steep fall-off dose outside the target. Data on metastatic HNSCC patients undergoing SBRT are rare and pooled with other tumour types.
Ricco et al. reported on 447 patients with pulmonary metastases, including 51 patients with head and neck primary tumours, treated with a median dose of SBRT of 50 Gy delivered in three fractions. Median OS for the entire group was 26 months, with actuarial 1-, 3- and 5-year OS of 74.1%, 33.3, and 21.8%, respectively [28]. Patients with head and neck cancer had median OS of 37 months. The median local control for all patients was 53 months, with actuarial 1-, 3-, and 5-year local control rates of 80.4, 58.9, and 46.3%, respectively. There was no difference in local control according to the primary histologic type. However, different total doses and schedules were used between studies. Toxicity seems to be moderate in most cases, although complications such as vertebral fractures have been reported in case of vertebral radiation. The OMET trial (NCT03070366) is currently investigating the possibility to avoid systemic treatments first hand by comparing systemic treatment associated with SBRT on HNSCC metastases vs. SBRT only.
Direct comparisons between surgery and SBRT are scarce. Metastasectomies should still be regarded as the standard therapeutic option for pulmonary oligometastases, as SBRT has not yet been evaluated in a large prospective study. However, the use of SBRT on pulmonary metastases is particularly interesting in unfit and/or medically inoperable patients. Undertaking invasive treatment like surgery is problematic when treating HNSCC metastatic patients in poor general condition due to advanced locoregional disease. Multidisciplinary discussions are mandatory to choose the best option based on patient’s characteristics.
Local Treatments of Other Metastatic Sites
Although treatments of lung metastases are well documented owing to their frequency, local treatments can also be used in other metastatic sites of HNSCC. For patients with solitary bone metastasis, SBRT is increasingly used with the aim of durable pain relief and local tumour control while sparing vital structures like the spinal cord in case of vertebral lesions [29]. As for liver metastases, existing treatment modalities are the same as for lung metastases: systemic therapy, surgery, SBRT and radiofrequency ablation. Data about management of liver metastases from HNSCC are rare in the literature. Local ablative treatments seem to be appropriate for patients with limited involvement of the liver. Adam et al. analysed survival rates of 1452 patients who underwent hepatic resection for their non-colorectal, non-neuroendocrine liver metastases. The 5- and 10-year OS rates were 36% and 23%, respectively [30]. These data are consistent with those reported by other studies about liver metastases from squamous cell cancers treated with hepatic resection [31, 32]. Five-year OS rates were around 20%. For inoperable patients, SBRT may offer long-term remission with minimal morbidity. Studies in the literature about SBRT for liver metastases are heterogenous in terms of primary histologic types, tumour volumes, total dose and dose per fraction. Median survival rate reported is approximately 17–20 months with promising results in LC and OS [33]. No specific data on head and neck primary cancers is available.
Intracranial metastases from HNSCC are rare. Whole brain irradiation associated with corticotherapy is currently the standard treatment for most patients with multiple brain metastases. However, surgical resection and stereotactic radiation therapy are also efficient for patients with good PS and well-controlled systemic disease. These techniques are increasingly advocated as whole brain irradiation generates important neurocognitive toxicity without any difference in OS [34, 35]. In a retrospective analysis, Patel et al. demonstrated that stereotactic radiation therapy provides good tumour control without major toxicity (asymptomatic radionecrosis) [36], thus making this approach an appropriate therapeutic option for brain metastases limited in number.
Locoregional Treatment of Primary Disease
The role of radiotherapy is well-defined in advanced locoregional HNSCC but in metastatic disease at presentation, its use is debated. Evidence on up-front use of radiotherapy in metastatic setting is lacking since this scenario is rare. The objective of radiotherapy is to achieve reduction in tumour size in order to alleviate symptoms such as dysphagia, hoarseness and dyspnoea. Previous studies have shown that this approach significantly improves quality of life of metastatic patients [37], but little has been published about the effect on survival outcomes. The benefit of radiotherapy was proved in a retrospective study led by Kabarriti et al. It demonstrated a 2.3-month improvement in OS and a 29% reduction in the relative risk of death with the addition of radiotherapy to chemotherapy in the up-front management of patients with metastatic disease [38••]. Chemotherapy was administered concurrently with radiotherapy or after or before radiotherapy. Specific details regarding chemotherapy agents were not available. However, patients who did not receive radiotherapy were more likely to receive multi rather than single-agent chemotherapy. Based on those data, it seems that radiotherapy to the primary HNSCC might play a significant role not only in symptomatic palliation but also in prolongation of survival.
In some cases, the addition of locoregional therapy to systemic therapy might be discussed despite limited data available. Locoregional progression represents the primary cause of morbidity and mortality, through disturbance of basic human functions such as breathing and eating. A retrospective study based on the SEER database showed an increased survival associated with surgery and/or radiation in HNSCC metastatic patients, over those who did not receive such local treatments. The mean survival was 8.4 months for patients who did not undergo any therapy. In comparison, patients who underwent radiation therapy alone, surgery alone, or surgery with radiation therapy had mean survivals of 18, 31 and 40 months, respectively [39•]. However, it is not clear whether chemotherapy had been used among the patients in the “no therapy” cohort, since this information was missing. Therefore, no comparison between the use of locoregional treatment and chemotherapy can be made. If chemotherapy was integrated in the management of the patients enrolled in the “no therapy arm”, the role of locoregional treatment would appear even more beneficial. A recent analysis of the National Cancer Data Base investigated the effects of high-intensity local treatment defined as radiation doses superior to 60 Gy or oncologic resection of the primary tumour in patients with distant metastatic HNSCC. Patients included all received systemic treatment. OS was significantly higher for those receiving combined local therapy and systemic therapy in comparison to patients receiving systemic therapy alone. Two-year OS rates were 34% vs. 20.6%, respectively [40••]. Conclusions however, should be analysed with caution as selection bias are likely to exist in these retrospective studies, driving patients with better performance status and minimal metastatic burden to receive more intensive treatment. Locoregional treatment modalities should be discussed for selected metastatic patients, independent of chemotherapy administration.
With respect to modalities of radiation therapy on primary disease, a few trials have assessed the best regimen for advanced HNSCC with metastatic disease. Chen et al. analysed the efficacy of various radiotherapy fractionation schemes used for palliation of HNSCC in 60 individuals with metastatic disease [41]. They claimed that all treatment schedules were effective at providing relief. The Radiation Therapy Oncology Group 8502 regimen (44 Gy administered twice a day for two consecutive days at 2- to 3-week intervals for three total cycles) was associated with less toxicity compared with the other schedules (i.e. 70 Gy in 35 fractions, 30 Gy in 10 fractions, 37.5 Gy in 15 fractions, and 20 Gy in four fractions). Similarly, some investigators favour treating patients with advanced HNSCC (including metastatic disease) with a palliative intent using short-course hypofractionated radiotherapy schemes. The Quad Shot regimen (14 Gy in four fractions over 2 days, twice daily, repeated at four weekly interval for a further two courses if there was no tumour progression) resulted in an improved quality of life in 44% of patients, 63% for those who received the full three courses [42]. Porceddu et al. in the Hypo Trial (30 Gy in five fractions, two fractions per week) also reported improvement in quality of life in 62% of patients with acceptable toxicity (26% grade 3 mucositis) [43]. A wide range of regimens have been used but there is no clear evidence in favour of one specific regimen since comparisons between studies are limited due to variable quality. However, short hypofractionated regimens are promising treatment options, ensuring both symptomatic relief and minimal side effects whilst reducing overall treatment time, knowing that average patient life expectancy is less than a year for metastatic HNSCC [2].
Considering the subsequent toxicity of the locoregional approach, optimal selection of candidates remains to be a difficult challenge. Prospective trials on the role of local treatment combined to systemic therapy are warranted, particularly for oligometastatic disease.
Therapeutic Strategy for HPV-Negative HNSCC
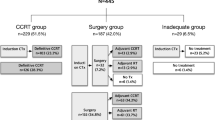
With the rise of novel local treatment modalities, patients with synchronous HNSCC metastatic disease can now benefit from a multidisciplinary approach including systemic therapy, radiation therapy and in some cases surgery. Recent NCCN guidelines 2018 on metastatic patients at initial presentation suggests a combination of treatments including systemic therapy, best supportive care and locoregional treatments (radiotherapy or surgery) for selected patients with limited metastases and good general conditions (PS 0–1). As for patients with a PS 2–3, no locoregional treatment is advocated [18]. We hereby propose a detailed algorithm for the management of HNSCC patients with metastatic disease at presentation (Fig. 1).
A careful baseline assessment must be made, based on patients’ characteristics (age, comorbidities), the disease history (number of metastases and their location) as well as treatment availability. The management of patients older than 70 years old remains a challenge since these patients are rarely included in trials. This population is heterogenous and therefore deserves better assessment for a tailored treatment. In this regard, a large prospective clinical programme, ELAN (Elderly head and neck cancer-oncology evaluation) has been developed to improve the multidisciplinary management of elderly (≥ 70 years old) HNSCC patients unsuitable for surgery. Four hundred and forty-eight patients are selected in three distinct trials after being classified as “fit” or “unfit” following a geriatric evaluation applicable to the daily practice proposed by the ELAN-ONCOVAL study [44]. Fit patients are defined by a Karnofsky performance score of 70 or more and adequate haematological, renal and hepatic functions.
For fit patients with limited metastatic disease burden defined as oligometastatic (≤ 3 lesions) according to a definition made by the GORTEC in the OMET trial, a triple modality approach can be proposed. The aim is maximal local control of both the primary and the metastatic sites, for a curative intent. First, we can administer 2 cycles of chemotherapy, using the EXTREME protocol, validated as first-line treatment in the metastatic setting. TPEx could be an alternative as it yielded promising PFS and OS rates in a phase II study [15]. No more than 2 cycles should be administered in order not to compromise the feasibility of the second phase of treatment which is concomitant chemoradiotherapy on the primary tumour. Patients eligible for chemoradiotherapy must display a good response to initial chemotherapy following radiologic assessment. As patients are deemed fit enough to receive aggressive treatments, the choice of the concurrent molecule remains the same as for locoregional HNSCC. Cisplatin 100 mg/m2 every 3 weeks is the preferred regimen [45]. In case of contraindication, carboplatin-5FU or cetuximab are alternatives [18]. The choice of the radiation scheme is open to discussion as data in literature are rare in this setting. If good local control of distant metastases is achievable, and eventually translated into prolonged survival rates, standard radiotherapy doses and fractionation (70 Gy in 35 fractions) may be suggested. Altered fractionation protocols may be considered as alternative options. A study using simultaneous integrated boost technique (SIB) for delivering dose per fraction slightly higher than 2 Gy thus shortening the treatment time concluded that this approach was safe and effective as no increased toxicity was observed [46]. Patients with progressive disease after initial chemotherapy should receive immunotherapy [21, 22]. Distant metastases, if limited in number, are amenable to SBRT in a third phase. Surgery is also a theoretical treatment option, for both the primary tumour and the metastatic sites. It may be discussed in particular cases but given the poor prognosis of metastatic HNSCC, patients are more likely to benefit from a less invasive approach such as radiation therapy, with the advantages of efficient relief, convenience and lower morbidity.
Unfit patients older than 70 years old with less than three metastases would generally be treated with radiation therapy alone on the primary tumour associated with SBRT on distant metastatic sites. Regarding radiotherapy scheme, hypofractionated schedules were effective in terms of symptomatic relief and less toxic than standard radiotherapy.
Patients with three metastases or more should be treated with a combination of systemic therapy and palliative radiotherapy for symptomatic relief, both at primary and distant metastatic sites if needed. The decision of undertaking a locoregional treatment must take into consideration the patient’s general condition and is therefore subject to multidisciplinary discussion. Hypofractionated radiotherapy protocols are available for unfit patients whilst keeping in mind the possibility of offering best supportive care only. As for the choice of chemotherapy regimens, fit patients are primarily treated with the standard regimen EXTREME as first-line treatment. Options for unfit patients should be discussed, with various agents (chemotherapy and targeted therapy) used in monotherapy or combination.
Treatment strategy for metastatic HPV- positive HNSCC
Tumour HPV status is now established as an independent prognostic factor for OS and PFS among patients with locoregionally advanced oropharyngeal squamous-cell carcinomas at initial presentation [8]. Prognosis for HPV-positive patients is significantly better than for HPV-negative ones. However, HPV prognostic and predictive utility remains to be defined in metastatic settings. Only recently was the relationship between HPV and outcomes in recurrent and/or metastatic evaluated in large trials. No specific data is available about metastatic patients at presentation. Three main retrospective studies [47,48,49] support the association between HPV positivity and improved survival. In the EXTREME study [47], 442 patients all treatment-naïve, were randomly assigned to receive chemotherapy (platinum + 5-FU) with or without cetuximab. In subgroup analyses, survival benefits of chemotherapy plus cetuximab were observed over chemotherapy alone independent of tumour HPV, p16 or combined HPV/p16 status. Patients with HPV-positive or p16-positive disease had longer survival, although without statistical significance. In the SPECTRUM trial [48], 657 previously untreated patients were randomly assigned to receive chemotherapy (platinum + 5-FU) with or without an anti-EGFR antibody, panitumumab. In the control group, p16-positive patients had longer overall survival but not statistically, than did p16-negative patients. However, within the p16-positive group, it was reported a shorter median survival in the experimental arm than in the control arm, not statistically significant. A retrospective study analysed the HPV status in 65 and 66 patients from two ECOG trials, E1395 and E3301, respectively [49]. Chemotherapy doublets were tested in those studies: cisplatin/5-FU vs cisplatin/paclitaxel in E1395 and docetaxel/irinotecan in E3301. Statistically significant better response rate and survival were seen in p16/HPV-positive population. These findings support a prognostic role for tumour HPV status [47,48,49] but the impact of anti-EGFR antibodies on outcome in HPV-positive and HPV-negative remains unclear [47, 48]. These data have significant limitations such as smoking status, small numbers of p16-positive/HPV-positive patients and inaccurate HPV classification based on non-standardized detection method. Within these limitations, Spreafico et al. did a pooled analysis of these three studies [50]. The analysis suggests that with chemotherapy alone, HPV- or p16-positive patients have better overall survival, with the studies showing a 30% to 40% reduction in the risk of death over time. In the same analysis, the combined EXTREME and SPECTRUM studies show no predictive value of p16 overexpression for response with the addition of an EGFR inhibitor to chemotherapy. As for the treatment strategy of synchronous metastatic HPV-positive patients, evidenced-based data is still lacking. The therapeutic algorithm remains for now the same as suggested for HPV-negative patients. Considering the growing incidence of HPV-positive HNSCC, further prospective studies with HPV status as standard stratification factor are warranted, particularly in metastatic settings. Understanding the biologic differences between HPV-positive et HPV-negative is key for developing directed therapies. Future directions should explore cancer vaccination and immunotherapy for this virus-driven cancer.
Summary
The management of patients with metastatic HNSCC is complex. A multimodality approach has to be proposed based on a careful baseline assessment of each patient. Systemic treatment such as chemotherapy and targeted treatment, best supportive care and local ablation techniques such as radiation therapy are now the main options in this setting. Advances in techniques like SBRT enable long-term local control for limited metastatic disease, whilst remaining non-invasive. Some main issues remain unsolved, including the best treatment to give to primary tumours. Frail patients with advanced disease suffering from locoregional symptoms would be amenable to locoregional treatment if the benefit ratio to provide symptomatic relief is manageable. The challenge is to offer the most efficacious treatment whilst sparing toxicity as much as possible. In this regard, immunotherapy will likely play a major role in the treatment of metastatic HNSCC. The major pillars of the decision are based on a thorough clinical assessment of the patient’s baseline function and co-morbidities, as well as discussions with the multidisciplinary tumour board.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Ferlito A, Shaha AR, Silver CE, Rinaldo A, Mondin V. Incidence and sites of distant metastases from head and neck cancer. ORL. 2001;63:202–7.
Vermorken J, Mesia R, Rivera F, Remenar E. Platinum-based chemotherapy plus Cetuximab in head and neck cancer. N Engl J Med. 2008;359:1116–27.
Kotwall C, Sako K, Razack MS, Rao U, Bakamjian V, Shedd DP. Metastatic patterns in squamous cell cancer of the head and neck. Am J Surg. 1987;154:439–42.
Garavello W, Ciardo A, Spreafico R, Gaini RM. Risk factors for distant metastases in head and neck squamous cell carcinoma. Arch Otolaryngol Neck Surg. 2006;132:762–6.
Kuperman DI, Auethavekiat V, Adkins DR, Nussenbaum B, Collins S, Boonchalermvichian C, et al. Squamous cell cancer of the head and neck with distant metastasis at presentation. Head Neck. 2011;33:714–8.
Fakhry C, Gillison ML. Clinical implications of human papillomavirus in head and neck cancers. J Clin Oncol. 2006;24:2606–11.
Taberna M, Mena M, Pavón MA, Alemany L, Gillison ML, Mesía R. Human papillomavirus-related oropharyngeal cancer. Ann Oncol. 2017;28:2386–98.
Ang KK, Harris J, Wheeler R, Weber R, Rosenthal DI, Nguyen-Tân PF, et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med. 2010;363:24–35.
Fakhry C, Zhang Q, Nguyen-Tan PF, Rosenthal D, El-Naggar A, Garden AS, et al. Human papillomavirus and overall survival after progression of oropharyngeal squamous cell carcinoma. J Clin Oncol. 2014;32:3365–73.
Huang SH, Perez-Ordonez B, Liu F-F, Waldron J, Ringash J, Irish J, et al. Atypical clinical behavior of p16-confirmed HPV-related oropharyngeal squamous cell carcinoma treated with radical radiotherapy. Int J Radiat Oncol. 2012;82:276–83.
Müller S, Khuri FR, Kono SA, Beitler JJ, Shin DM, Saba NF. HPV positive squamous cell carcinoma of the oropharynx. Are we observing an unusual pattern of metastases? Head Neck Pathol. 2012;6:336–44.
Hellman S, Weichselbaum RR. Oligometastases. J Clin Oncol. 1995;13:8–10.
Weichselbaum RR, Hellman S. Oligometastases revisited. Nat Rev Clin Oncol. 2011;8:378–82.
Lee DH, Kim MJ, Roh J-L, Kim S-B, Choi S-H, Nam SY, et al. Distant metastases and survival prediction in head and neck squamous cell carcinoma. Otolaryngol-Head Neck Surg. 2012;147:870–5.
Guigay J, Fayette J, Dillies AF, Sire C, Kerger JN, Tennevet I, et al. Cetuximab, docetaxel, and cisplatin as first-line treatment in patients with recurrent or metastatic head and neck squamous cell carcinoma: a multicenter, phase II GORTEC study. Ann Oncol. 2015;26:1941–7.
Boisdron-Celle M, Capitain O, Faroux R, Borg C, Metges JP, Galais MP, et al. Prevention of 5-fluorouracil-induced early severe toxicity by pre-therapeutic dihydropyrimidine dehydrogenase deficiency screening: assessment of a multiparametric approach. Cancer Screen Still Work Prog. 2017;44:13–23.
Tahara M, Kiyota N, Yokota T, Hasegawa Y, Muro K, Takahashi S, et al. Phase II trial of combination treatment with paclitaxel, carboplatin and cetuximab (PCE) as first-line treatment in patients with recurrent and/or metastatic squamous cell carcinoma of the head and neck (CSPOR-HN02). Ann Oncol. 2018;mdy040–mdy040.
Pfister DG, Foote RL, Gilbert J, Gillison ML, Ridge JA, Rocco J. NCCN Guidelines Index Table of Contents Discussion 2018;227.
Gregoire V, Lefebvre J-L, Licitra L, Felip E. On behalf of the EHNS-ESMO-ESTRO guidelines working group. Squamous cell carcinoma of the head and neck: EHNS-ESMO-ESTRO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2010;21:v184–6.
Economopoulou P, Agelaki S, Perisanidis C, Giotakis EI, Psyrri A. The promise of immunotherapy in head and neck squamous cell carcinoma. Ann Oncol. 2016;27:1675–85.
Seiwert TY, Burtness B, Mehra R, Weiss J, Berger R, Eder JP, et al. Safety and clinical activity of pembrolizumab for treatment of recurrent or metastatic squamous cell carcinoma of the head and neck (KEYNOTE-012): an open-label, multicentre, phase 1b trial. Lancet Oncol. 17:956–65.
Harrington KJ, Ferris RL, Blumenschein G, Colevas AD, Fayette J, Licitra L, et al. Nivolumab versus standard, single-agent therapy of investigator’s choice in recurrent or metastatic squamous cell carcinoma of the head and neck (CheckMate 141): health-related quality-of-life results from a randomised, phase 3 trial. Lancet Oncol. 2017;18:1104–15.
Kaifi JT, Gusani NJ, Deshaies I, Kimchi ET, Reed MF, Mahraj RP, et al. Indications and approach to surgical resection of lung metastases. J Surg Oncol. 2010;102:187–95.
Young ER, Diakos E, Khalid-Raja M, Mehanna H. Resection of subsequent pulmonary metastases from treated head and neck squamous cell carcinoma: systematic review and meta-analysis. Clin Otolaryngol. 2015;40:208–18.
Liu D, Labow DM, Dang N, Martini N, Bains M, Burt M, et al. Pulmonary metastasectomy for head and neck cancers. Ann Surg Oncol. 1999;6:572–8.
Haro A, Yano T, Yoshida T, Ito K, Morodomi Y, Shoji F, et al. Results of a surgical resection of pulmonary metastasis from malignant head and neck tumor. Interact Cardiovasc Thorac Surg. 2010;10:700–3.
Shiono S, Kawamura M, Sato T, Okumura S, Nakajima J, Yoshino I, et al. Pulmonary metastasectomy for pulmonary metastases of head and neck squamous cell carcinomas. Ann Thorac Surg. 2009;88:856–60.
Ricco A, Davis J, Rate W, Yang J, Perry D, Pablo J, et al. Lung metastases treated with stereotactic body radiotherapy: the RSSearch® patient Registry’s experience. Radiat Oncol. 2017;12.
Bhattacharya IS, Hoskin PJ. Stereotactic body radiotherapy for spinal and bone metastases. Clin Oncol. 2015;27:298–306.
Adam R, Chiche L, Aloia T, Elias D, Salmon R, Rivoire M, et al. Hepatic resection for noncolorectal nonendocrine liver metastases: analysis of 1452 patients and development of a prognostic model. Trans Meet Am Surg Assoc. 2006;124:189–200.
Pawlik TM, Gleisner AL, Bauer TW, Adams RB, Reddy SK, Clary BM, et al. Liver-directed surgery for metastatic squamous cell carcinoma to the liver: results of a multi-center analysis. Ann Surg Oncol. 2007;14:2807–16.
Adam R, Wicherts DA, de Haas RJ, Ciacio O, Lévi F, Paule B, et al. Patients with initially unresectable colorectal liver metastases: is there a possibility of cure? J Clin Oncol. 2009;27:1829–35.
Scorsetti M, Clerici E, Comito T. Stereotactic body radiation therapy for liver metastases. J Gastrointest Oncol. 2014;5:190.
Aoyama H, Shirato H, Tago M, Nakagawa K, Toyoda T. Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases. JAMA. 2006;295:2483–91.
Chang EL, Wefel JS, Hess KR, Allen PK, Lang FF, Kornguth DG, et al. Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol. 2009;10:1037–44.
Patel RA, Bell JB, Kim T, Agulnik M, Chandler JP, Mittal BB, et al. Stereotactic radiosurgery for brain metastases from primary head and neck carcinomas: a retrospective analysis. J Neuro-Oncol. 2017;134:197–203.
Roland NJ, Bradley PJ. The role of surgery in the palliation of head and neck cancer. Curr Opin Otolaryngol Head Neck Surg. 2014;22:101–8.
•• Kabarriti R, Baliga S, Ohri N, Guha C, Kalnicki S, Garg MK. Radiation therapy for patients with newly diagnosed metastatic head and neck squamous cell carcinoma. Head Neck. 2018;41(1):130–8 First clinical study to demonstrate a survival benefit for the use of radiotherapy in the initial management of metastatic HNSCC.
• Patel TD, Marchiano E, Chin OY, Kilic S, Eloy JA, Baredes S, et al. Utility of surgery/radiotherapy in distant metastatic head and neck squamous cell carcinoma: a population-based approach. Otolaryngol-Head Neck Surg. 2016;154:868–74 Study reporting longer survival in metastatic HNSCC patients treated with radiotherapy and/or surgery compared to patients who did not undergo any therapy.
•• Zumsteg ZS, Luu M, Yoshida EJ, Kim S, Tighiouart M, David JM, et al. Combined high-intensity local treatment and systemic therapy in metastatic head and neck squamous cell carcinoma: an analysis of the National Cancer Data Base: local treatment in metastatic HNSCC. Cancer. 2017;123:4583–93 Study reporting an association between prolonged OS and the addition of high-intensity local treatment (radiotherapy delivered at curative dose or surgery) to systemic therapy in metastatic HNSCC patients.
Chen AM, Vaughan A, Narayan S, Vijayakumar S. Palliative radiation therapy for head and neck cancer: toward an optimal fractionation scheme. Head Neck. 2008;30:1586–91.
Corry J, Peters LJ, Costa ID, Milner AD, Fawns H, Rischin D, et al. The ‘QUAD SHOT’—a phase II study of palliative radiotherapy for incurable head and neck cancer. Radiother Oncol. 2005;77:137–42.
Porceddu SV, Rosser B, Burmeister BH, Jones M, Hickey B, Baumann K, et al. Hypofractionated radiotherapy for the palliation of advanced head and neck cancer in patients unsuitable for curative treatment – “Hypo Trial.”. Radiother Oncol. 2007;85:456–62.
Mertens C, Le Caer H, Ortholan C, Blot E, Even C, Rousselot H, et al. The ELAN-ONCOVAL (ELderly heAd and neck cancer-oncology eValuation) study: evaluation of the feasibility of a suited geriatric assessment for use by oncologists to classify patients as fit or unfit. Ann Oncol. 2017;28.
Adelstein DJ, Li Y, Adams GL, Wagner H, Kish JA, Ensley JF, et al. An intergroup phase III comparison of standard radiation therapy and two schedules of concurrent chemoradiotherapy in patients with unresectable squamous cell head and neck cancer. J Clin Oncol. 2003;21:92–8.
Leclerc M, Maingon P, Hamoir M, Dalban C, Calais G, Nuyts S, et al. A dose escalation study with intensity modulated radiation therapy (IMRT) in T2N0, T2N1, T3N0 squamous cell carcinomas (SCC) of the oropharynx, larynx and hypopharynx using a simultaneous integrated boost (SIB) approach. Radiother Oncol. 2013;106:333–40.
Vermorken JB, Psyrri A, Mesía R, Peyrade F, Beier F, de Blas B, et al. Impact of tumor HPV status on outcome in patients with recurrent and/or metastatic squamous cell carcinoma of the head and neck receiving chemotherapy with or without cetuximab: retrospective analysis of the phase III EXTREME trial. Ann Oncol. 2014;25:801–7.
Vermorken JB, Stöhlmacher-Williams J, Davidenko I, Licitra L, Winquist E, Villanueva C, et al. Cisplatin and fluorouracil with or without panitumumab in patients with recurrent or metastatic squamous-cell carcinoma of the head and neck (SPECTRUM): an open-label phase 3 randomised trial. Lancet Oncol. 2013;14:697–710.
Mehra R, Egloff AM, Li S, Yang D, Wang L, Zhu F, et al. Analysis of HPV and ERCC1 in recurrent or metastatic squamous cell carcinoma of the head and neck (R/M SCCHN). J Clin Oncol. 2013;31:6006.
Spreafico A, Amir E, Siu LL. Demystifying the role of tumor HPV status in recurrent and/or metastatic squamous cell carcinoma of the head and neck. Ann Oncol. 2014;25:760–2.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Eliane Tang, Lucien Lahmi, Nicolas Meillan, Gianandrea Pietta, Sébastien Albert, and Philippe Maingon declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Head and Neck Cancers
Rights and permissions
About this article
Cite this article
Tang, E., Lahmi, L., Meillan, N. et al. Treatment Strategy for Distant Synchronous Metastatic Head and Neck Squamous Cell Carcinoma. Curr Oncol Rep 21, 102 (2019). https://doi.org/10.1007/s11912-019-0856-5
Published:
DOI: https://doi.org/10.1007/s11912-019-0856-5