Abstract
Allogeneic hematopoietic stem cell transplant (HSCT) is an established treatment modality with curative potential for acute myeloid leukemia (AML). There has been a significant rise in the number of HSCT procedures performed over the past decade due in part to improved supportive care and innovative techniques such as reduced-intensity conditioning. Expanding alternative donor options such as umbilical cord blood and haploidentical HSCT, taken together with improved outcomes of matched unrelated donors, has resulted in a suitable donor for most patients with an HSCT indication. Recent advances in molecular diagnostics that incorporate genetic mutational analysis into existing cytogenetic-based models should improve selection of patients at high risk of relapse most likely to benefit from HSCT. Improvements in minimal residual disease monitoring hold promise for adding prognostic information, and informing the clinician of impending relapse. The choice of the conditioning regimen involves weighing a patient's unique toxicity and relapse risks. Despite improvements, relapse remains the primary source of treatment failure after HSCT for treatment of AML. The introduction of novel therapies into the clinic, together with improved patient selection, offers hope for decreasing relapse and improving outcomes for AML patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Allogeneic hematopoietic stem cell transplant (HSCT) is an established treatment modality with curative potential in poor-risk acute myeloid leukemia (AML). In the USA alone, approximately 9,000 HSCT procedures were performed annually in 2010, with AML being the commonest indication [1]. Considering relapse for AML treated with chemotherapy alone is high (more 50 % in most cases) [2•], many patients have a disease-specific indication for HSCT in an effort to reduce this risk. However, the role of HSCT has historically been limited owing to increased treatment-related mortality and lack of suitable donors. Significant improvements in HSCT outcomes have been observed in the past decade, likely related to reductions in organ damage from conditioning, improved infectious prophylaxis, and limiting severe graft-versus-host disease (GVHD) [3]. The concomitant expansion of donor registries and the emerging role of umbilical cord blood and haploidentical transplants have further increased the number of AML patients with suitable donors. Despite improved outcomes and availability of HSCT, relapse remains the principal cause of treatment failure, and other morbid sequelae such as GVHD and infection continue to pose ongoing challenges. This review is intended to update the reader on recent advances in the field pertaining to patient selection; with an emphasis on the prognostic role of cytogenetics, molecular genetics, and minimal residual disease (MRD) monitoring. The emerging role of alternative donor transplantation and strategies to limit and prevent post-HSCT relapse are highlighted.
Prognostic Markers
Cytogenetics and Role of HSCT in First Complete Remission
Cytogenetics continues to play a dominant role in determining the response to induction, the risk of relapse, and overall survival and thus remains the principal factor for selecting patients for HSCT. The decision to offer postremission chemotherapy is typically more straightforward for patients with favorable or poor-risk leukemia. With chemotherapy alone, the odds of long-term disease-free survival is approximately 65 % for patients with core binding factor leukemia [i.e., t(8;21) or inv(16)] receiving high-dose cytarabine-containing regimens, but falls to less than 20 % for those possessing poor-risk cytogenetics [2•]. Therefore, poor-risk cytogenetic cohorts derive the greatest benefit of HSCT in first remission, whereas HSCT for favorable-risk cytogenetic cohorts is deferred until relapse [4]. (Table 1) Despite extensive study, the role of HSCT in first complete remission (CR1) continues to be debated in patients with intermediate cytogenetic risk. A large meta-analysis of 24 prospective studies analyzed the outcomes of approximately 6,000 patients receiving either matched sibling donor transplant or consolidation chemotherapy according to donor availability. Patients in CR1 were stratified by cytogenetic risk [5]. Postremission therapy with HSCT showed significant overall and disease-free survival advantages for AML with intermediate and high cytogenetic risk, but not in patients with good-risk karyotype. A recent analysis reexamined the role of HSCT patients in CR1. The authors of the study indicate a 17 % long-term survival rate for patients younger than 50 years with intermediate-risk cytogenetics who relapse after consolidation chemotherapy (versus 7 % for individuals relapsing after HSCT) [6]. When adjusting for differences in postrelapse survival, they posit that the survival advantage for HSCT in intermediate-risk cytogenetic groups is marginal, suggesting use of HSCT in second complete remission (CR2), where its survival impact is greatest. Although these findings are provocative, it is difficult to interpret them in the context of recent HSCT outcomes, as the analysis included younger patients and unrelated donors in an era associated with higher treatment-related mortality.
Monosomal and 17p Karyotype as Very High Risk AML
Monosomal karyotype, consisting of two or more autosomal monosomies or the combination of one monosomy with structural abnormalities, can be found in up to 30 % of abnormal karyotypes. Outcomes for such patients are very poor, with remission rates of approximately 30 %. HSCT does improve survival when applied in patients in CR1 by significantly reducing relapse, but the magnitude of this benefit is marginal (5-year overall survival of 19 % for HSCT vs 9 % for chemotherapy) [7•, 8]. Abnormalities of chromosome arm 17p occur rarely (4 % of AML), but represent a very poor risk karyotype [9]. Only a third of patients were able to proceed to HSCT in remission. Overall survival at 3 years after HSCT was a dismal 11 %, which in multivariate analysis did not confer a survival advantage compared with chemotherapy. Data from the German Cooperative Transplant Study Group found similar poor results with HSCT in 17p AML, but better outcomes for patients with −5/-5q [leukemia-free survival (LFS) rate of 29 % at 2 years] [10•]. Interestingly, this analysis reported that excluding 17p or −5/-5q greatly lessens the poor prognostic value of complex and monosomal kayotypes. The dismal outcomes reported for subtypes such as 17p remind us of the wide biologic diversity of AML, suggesting such subtypes may be best treated with clinic protocols designed to address very high risk patients.
HSCT-Specific Cytogenetic Classification
Cytogenetic classification systems have been largely based on de novo AML patients receiving cytarabine-based chemotherapy, and therefore may lack prognostic capabilities similar to those for patients treated with HSCT. In 821 patients in the Center for International Blood and Marrow Transplant Research (CIBMTR) database undergoing HSCT in first or second remission, Armand et al. [11•] compared existing cytogenetic classifications and developed a new schema for predicting overall survival. Notably, the poor-risk grouping was revised to include only complex karyotypes with four or more cytogenetic abnormalities (as opposed to three or more abnormalities), good risk corresponded to only inv(16), and all other abnormalities were classified as intermediate risk. It is notable that patients with antecedent myelodysplastic syndrome (MDS) were excluded and the 84 % of patients were assigned to intermediate risk. It is not clear how best to incorporate these findings into clinical practice because it is unlikely to change who is recommended for HSCT; rather, these data may provide valuable prognostic information for patients considering HSCT (particularly patients in CR1) or for identifying high-risk cohorts for future clinical trials.
Integrating Genetic Mutations into Prognostic Models
c-KIT Mutations and Good-Risk AML
Genetic markers are now being incorporated into prognostic models for AML in CR1, and this may soon alter prognosis even for patients with favorable cytogenetic risk. For example, a c-KIT mutation in the presence of inv(16) or t(8:21) results in a higher relapse rate and intermediate prognosis (48 % overall survival at 5 years) compared with historically good outcomes, prompting some to recommend HSCT for patients in CR1 rather than consecutive cycles of high-dose cytarabine [2•, 12, 13]. These data may be practice-changing, but should be interpreted with caution considering the small patient numbers. Furthermore, some reports suggest that the negative prognostic impact of c-KIT mutation may be restricted to select core binding factor leukemias, i.e., t(8;21) [14•].
FLT3-ITD, NPM1, and CEBPA in Intermediate Cytogenetic Risk AML
More than 60 % of patients with AML are classified as intermediate risk by cytogenetics; thus, improving our ability to discriminate high-risk cohorts may allow better risk-adapted therapy [15]. To date, Fms-like tyrosine kinase 3 internal tandem duplications (FLT3-ITD) are the commonest and most prognostically significant genetic aberration in normal-karyotype AML. To better understand its prognostic impact after HSCT, Brunet et al. [16] performed a comparative analysis of outcomes for patients with normal karyotype according to FLT3-ITD mutational status. All patients were in CR1 and received myeloablative conditioning. The relapse incidence was significantly greater (30 % vs 16 %), resulting in inferior LFS in AML harboring FLT3-ITD mutations (58 % vs 71 %). Other single-center analyses have reported significantly a higher relapse incidence after HSCT for FLT3-ITD-positive AML [17]. These data confirm that FLT3-ITD is prognostic among HSCT patients, but most evidence supports consolidation of FLT3-ITD AML with HSCT in patients in CR1 given the proportionally higher risk of relapse with chemotherapy (Table 1) [18, 19•]. In the seminal work of Schlenk et al. [18], a significant benefit for matched related donor HSCT was observed in cytogenetically normal AML with FLT3-ITD mutation (independent of other genetic mutations). However, importantly, patients with wild-type FLT3-ITD who also lacked nucleophosmin member 1 (NPM1) and CCAAT/enhancer-binding protein a (CEBPA) also had poor survival and an apparent benefit from HSCT [18]. In contrast, HSCT as consolidation therapy did not improve survival in NPM1- or CEBPA-mutated AML with wild-type FLT3-ITD. Other groups have also shown that CEBPA mutations (single or double) in normal-karyotype AML lacking FLT3-ITD mutation are associated with improved outcomes owing to lower relapse risk [20].
FLT3-ITD Allelic Ratio
Current studies are investigating the prognostic impact of FLT3-ITD genomic burden. FLT3-ITD mutation is purported to outweigh any beneficial prognostic effects of mutated NPM1. More recently, the effect of FLT3-ITD allele ratio with concomitant NPM1 mutations was analyzed in 303 AML patients with intermediate-risk cytogenetics [21]. A low FLT3-ITD to FLT3 wild type ratio (below 0.5) correlated with improved LFS on par with good-risk-karyotype AML; but the ratios had no prognostic relevance in wild-type NPM1. Furthermore, HSCT as consolidation therapy reduced the risk of relapse for AML patients with FLT3-ITD, but not for the subgroup with NPM1 mutation and low allelic burden of FLT3-ITD. Allelic ratios provide another potential caveat to genetic mutational analysis, but are not standardized, nor are they routinely reported across laboratories. These results require further validation since mutations in FLT3-ITD and NPM1 commonly coexist.
Isocitrate Dehydrogenase Mutations
As AML genomics rapidly evolves, there will no doubt be new additions that add complexity by further stratifying disease risk. Mutations in the isocitrate dehydrogenase genes (IDH1 and IDH2) appear to further modulate risk within the favorable FLT3-ITD wild type/NPM1 mutated profile [22•]. AMLs harboring IDH1/IDH2 mutations have the best outcomes, equivalent to or even better than those of good-risk karyotype, whereas those lacking IDH1/IDH2 have less favorable survival (3-year overall survival of 89 % vs 31 %). It is critical that specific mutations are taken into account when interpreting this literature, since the benefits appear restricted to IDH1/IDH2 with the R140 mutation [14•]. The role of IDH1/IDH2 mutations merits further study as it could alter practice recommendations for patients in CR1 in good-risk subgroups.
MRD Monitoring
Conventional definitions of remission state in AML define less than 5 % myeloblasts by marrow aspirate examination in the context of peripheral count recovery. There is emerging data that detection of MRD by flow cytometry, cytogenetics, or molecular methods may independently predict outcomes following HSCT.
Flow Cytometry
In a recent study by Walter et al. [23], detection of MRD by ten-color multiparameter flow cytometry was correlated with a significantly increased risk of relapse (incidence of relapse of 65 % for MRD-positive patients), resulting in inferior survival compared with MRD-negative patients. The broad applicability of MRD reporting in the current era is limited by the need for technical expertise in discriminating minute blast populations. Furthermore, current methods are only useful in a minority of AML patients who possess an identifiable leukemia-associated phenotype (approximately 25 % in the study by Walter et al.).
Morphologic Remission Without Cytogenetic Remission ("Cytogenetic MRD")
The significance of complete morphologic, without cytogenetic, remission was recently reported by a group from the MD Anderson Cancer Center. Persistent cytogenetic abnormalities were identified in 28 % of patients in complete morphologic remission, resulting in a median relapse-free survival of only 6 months versus 21 months for complete remission with cytogenetic remission [24]. The impact of a persistent abnormal karyotype at HSCT was also reported for patients with poor-risk cytogenetics [25]. Complete cytogenetic remissions predicted survival rates similar to those for patients with intermediate-risk karyotype, whereas cytogenetic persistence of the clone conferred the worst prognosis, with a cumulative incidence of relapse approaching 60 %. Taken together, these data suggest that patients with any persistence of AML have unacceptably high rates of relapse, approaching those of patients not in morphologic remission at HSCT.
Persistence of Host Chimerism and WT1
Following HSCT, the presence of residual host hematopoietic cells can be detected by PCR-based assays, known as chimerism studies. Recently, the presence of residual host-lineage-specific chimerism in CD34+ hematopoietic cells has been suggested to be a surrogate marker for persistence of the neoplastic clone. In patients with AML and MDS, 32 % of patients had residual host CD34+ chimerism, and most of these patients underwent tapering of immunosuppression or donor lymphocyte infusion [26]. Despite this intervention, the relapse-free survival rate remained significantly lower in patients with incomplete recipient chimerism (74 % vs 40 %). Thus, persistence of host CD34+ chimerism after HSCT is associated with inferior survival, but given the lack of randomized comparisons (i.e., between immune interventions and no intervention) the optimal intervention to prevent relapse is uncertain. Overexpression of the Wilms tumor 1 gene (WT1) is observed in most AMLs, and its presence can be detected by highly sensitive real-time PCR. The ability of WT1 to predict MRD was assessed in peripheral blood samples taken with standard morphologic and flow-cytometric assessments prior to HSCT [27]. Elevated levels of WT1 transcripts correlated with inferior survival, and in some cases predicted eventual hematologic relapse, suggesting its role in MRD monitoring warrants further study.
Donor Selection in AML
Is a Matched Unrelated Donor a Suitable Alternative to a Matched Related Donor?
Since much of the key literature supporting HSCT for patients in CR1 (particularly in patients with intermediate-risk cytogenetics) is based on data provided from matched related donors; extension of these findings to matched unrelated donors assumes equivalency of donor types. Recent data now suggest that matched unrelated donor HSCT outcomes are comparable with matched related donor HSCT outcomes. When unrelated donors are analyzed by the quality of HLA match, outcomes of matched related donor HRCT and matched unrelated donor HSCT are similar. In a large registry review from the CIBMTR database, Gupta et al. [28] analyzed outcomes for unfavorable-risk AML patients in CR1 receiving HSCT between 1996 and 2005. Similar LFS and overall survival were observed in patients receiving HLA-well-matched unrelated donor HSCT (no disparity at HLA-A, HLA-B, HLA-C, or HLA-DRB1) and HLA-matched related donor HSCT, but inferior outcomes were observed with HLA-partially matched unrelated donor HSCT. Despite this dataset being over a decade old, the donor type among well-matched donors did not influence the cumulative incidence of relapse or transplant-related mortality. A more recent comparative analysis has shown similar 4-year survival outcomes for AML patients with intermediate-risk AML in CR1 [29]. Additionally, Saber et al. [30•] performed an updated registry analysis in a very large cohort of 2,223 AML patients between 2002 and 2006, again comparing survival outcomes between matched related donor transplant, matched unrelated donor transplant, and partially matched unrelated donor transplant. The 3-year LFS and overall survival were similar between groups even after multivariate modeling adjusting for cytogenetic risk. Not surprisingly, partially matched unrelated donor transplant had higher early transplant-related mortality. These data provide strong evidence of equivalency in outcomes between matched related donor transplant and matched unrelated donor transplant in AML. However, a definitive modern donor versus no donor randomized analysis is unlikely to be performed considering the improvements and greater availability of matched unrelated donor HSCT.
Alternative Donor Transplantation
In patients for which HSCT is recommended, approximately 70 % lack a matched sibling donor. Of these, up to half of Caucasians may also lack a suitable unrelated donor, and this problem is even greater in racial and ethnic minorities. Emerging data now support the use of umbilical cord blood and possibly haploidentical transplant in situations where a matched related donor and a matched unrelated donor is lacking. A phase II Blood and Marrow Transplant Clinical Trials Network trial recently reported similar progression-free survival at 1 year after reduced-intensity double umbilical cord blood (dUCB) transplant and haploidentical transplants (46 % vs 48 %) [31]. Additionally, two single center retrospective analysis have reported similar survival between dUCB and matched unrelated donor HSCT [32, 33]. It is anticipated that ongoing studies may further improve outcomes with dUCB HSCT.
Haploidentical HSCT has seen resurgence in recent years. In a prospective study of AML in CR1 patients without a suitable matched related donor or matched unrelated donor, subjects were allowed to choose between chemotherapy and HSCT with a haploidentical transplant as postremission treatment [34•]. The incidence of relapse was significantly less in the HSCT group, with superior disease-free survival rate at 4 years (73.1 % vs 44.2 %; p < 0.0001). Whether haploidentical transplants will become a suitable replacement for dUCB transplants, matched unrelated donor transplants, or matched related donor transplants is unknown, but this study certainly supports considering this option over chemotherapy alone, particularly in AML patients at high risk of relapse.
Impact of Transplant Conditioning
Reduced-Intensity Conditioning
AML is predominantly a disease of the elderly, with a median age of onset of 66 years [35]. The advent of reduced-intensity conditioning (RIC) and nonmyeloablative conditioning regimens has expanded transplantation to older patients and those with medical comorbidities previously considered to be ineligible. The outcome for 372 patients aged 60–75 years receiving low-dose total body irradiation with or without fludarabine therapy was recently described [36]. The overall survival rate at 5 years was 35 %, without significant differences when patients were stratified by age group. However, a major premise of RIC is a greater reliance on donor immune cells to impart a graft-versus-leukemia (GVL) effect. In one study, AML patients older than 55 years receiving RIC with busulfan and fludarabine had a transplant-related mortality of approximately 20 %, but a cumulative incidence of relapse of 58 % [37]. Several nonrandomized comparisons of RIC with myeloablative conditioning have demonstrated a trade-off between toxicity and relapse resulting in similar survival [38–41]. There is are a paucity of randomized trials comparing conditioning intensities, and most retrospective analyses suffer from large heterogeneity in regimens. A recently reported phase III randomized comparison between RIC and myeloablative conditioning showed no significant difference in the incidence of relapse, nonrelapse mortality, or survival. However, this study was closed prematurely owing to slow accrual [41]. Comparative analyses among RIC regimens are scarce without randomized data. Chen et al. [42] reported outcomes for two reduced-intensity doses of intravenously administered busulfan (3.2 mg/kg vs 6.4 mg/kg) in AML and MDS patients. Despite differences in the GVHD prophylaxis regimens, the incidence of GVHD, nonrelapse mortality, and progression-free survival were similar between doses.
Since it is hypothesized that a greater reliance on a GVL effect is needed in RIC, the role of the stem cell source was reported by the European Group for Blood and Marrow Transplantation [43]. In multivariate analysis, recipients of peripheral blood stem cells had a higher incidence of grade II–IV acute GVHD [hazard ratio (HR) 2.33; p = 0.06] and higher nonrelapse mortality (HR 2.3, p = 0.015), but a decrease incidence of relapse (HR 0.61, p = 0.02) compared with recipients of bone marrow stem cells. Overall, this resulted in no significant difference in LFS between peripheral blood stem cells and bone marrow stem cells. In another large registry analysis of RIC in AML by the CIBMTR, the development of chronic GVHD or chronic plus acute GVHD was particularly important in limiting both early and late relapses (more than 1 year after HSCT) but came at the expense of increase transplant-related mortality and without benefit to survival [44].
Myeloablative Conditioning
Myeloablative conditioning combined with GVL effects provides the most effective antileukemic treatment for AML. Increasing intensity comes at the cost of greater transplant-related mortality; therefore, the ideal conditioning optimizes efficacy without adding toxicity. Bredeson et al. [45] suggest superiority of myeloablative intravenously administered busulfan over traditional total body irradiation based conditioning in myeloid malignancies. A prospective cohort of approximately 1,500 patients was analyzed from 2009 to 2011 for transplant outcomes. A survival advantage after multivariate analysis was observed for recipients of intravenously administered busulfan without increased risk of relapse or transplant-related mortality. However, as observed in earlier work using oral dosing, intravenously administered busulfan was associated with higher rates of hepatic sinusoidal obstruction syndrome [46]. Although not a primary end point of this analysis, outcomes in the intravenously administered busulfan group were similar between patients receiving cyclophosphamide and patients receiving fludarabine. A small prospective study from China randomized AML patients in first remission to receive either busulfan plus cyclophosphamide or busulfan plus fludarabine. Overall these regimens had similar outcomes in terms of relapse and survival, but the busulfan plus fludarabine regimen was associated with a trend towards reduced transplant-related mortality (18.8 % vs 9.9 %) [47].
Role of Conditioning in High-Risk AML
The cytogenetic profile and disease status are the primary determinants of relapse after HSCT; however, the role of conditioning intensity in modifying the risk is not established. The impact of cytogenetic risk on outcomes after RIC was reviewed by the European Group for Blood and Marrow Transplantation in 378 AML patients in CR1 undergoing transplant. Patients with poor-risk karyotype had twice the rate of relapse as patients with intermediate-risk karyotype (55 % vs. 28 %; p < 0.0001), which translated into inferior LFS at 2 years [48].
With the use of myeloablative conditioning, 10–30 % of patients who are not in remission at HSCT can achieve long-term remission of AML [49–51]. The use of RIC for patients with relapsed/refractory AML is generally not recommended outside a clinical trial owing to the very high relapse rate [52, 53]. Surprisingly, patients with active AML who have transplants have widely divergent outcomes according to five pretransplant factors—presence of circulating blasts, poor-risk cytogenetics, lack of MRD, Karnofsky performance score less than 90 %, and duration of CR1 of less than 6 months—which can be a helpful prognostic tool in advising such patients whether to pursue HSCT in such a high-risk setting. In an effort to improve HSCT outcomes in refractory hematologic malignancies, a phase I/II study of myeloablative clofarabine/busulfan conditioning was performed at our center. Most of the patients had AML and all were not in remission. The complete remission rate was 94 %, with a cumulative incidence of relapse, transplant-related mortality, and overall survival at 2 years of 42 %, 36 %, and 35 %, respectively [54]. We are now confirming these results in an ongoing multicenter phase II study of relapsed/refractory AML. A recent retrospective analysis of clofarabine-containing regimens was reported by the European Group for Blood and Marrow Transplantation in 69 AML patients, the majority with active leukemia at transplant [55]. LFS was 30 % at 2 years, suggesting clofarabine regimens warrant further study in protocols that address high-risk AML.
Relapse After HSCT
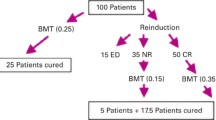
Although HSCT reduces the risk of relapse in intermediate-risk and high-risk AML, relapse remains the greatest cause of treatment failure. Survival after relapse in AML is very poor. Schmid et al. [56] recently described outcomes for AML patients relapsing after RIC HSCT performed while they were in complete remission. Overall, 32 % of patients experienced relapse, and the overall survival rate 2 years from the time of relapse was 14 %. Survival after post-HSCT relapse could be stratified according to the presence of three factors: remission after HSCT of more than 5 months, less than 27 % bone marrow blasts, and the absence of acute GVHD. Long-term survival was limited exclusively to patients able to recover complete remission status by cytoreductive therapy and subsequently receive either donor lymphocyte infusion (DLI) or a second HSCT.
Unlike the experience for DLI in chronic myelogenous leukemia, its use without preceding chemotherapy results in remissions in only 15 % of AML patients, likely due to the more rapid kinetics of this disease [57]. At the University of Minnesota, lymphocyte-depleting chemotherapy with fludarabine and cyclophosphamide followed by DLI at two different doses (1.0 × 108 or 0.5 × 108 CD3+ T cells per kilogram) was used to treat post-HSCT relapse in AML/MDS [58]. Approximately half of patients achieved complete remission, with the remission rates being similar between the two DLI dosing cohorts; however, the rates of grade II–IV acute GVHD were significantly greater with the higher dose (66 % vs 25 %).
Identifying effective and tolerable treatment options for post-HSCT relapse is a considerable challenge considering the effects on performance status from prolonged treatment and AML that has demonstrated resistance to chemotherapy and GVL. The hypomethylating agent azacitidine has been well tolerated as a prophylaxis and for treatment of relapse in combination with DLI [59, 60]. Responses can be observed in a third of patients, including some long-term remissions, typically after a median of three cycles. Patients with poor-risk cytogenetics and AML with MDS-related changes may be the most likely to respond.
Hypomethylating agents also possess salutary effects that may attenuate GVHD while preserving GVL responses. Choi et al. [61] demonstrated in vitro and in vivo that treatment with azacitidine causes inducible FOXP3 expression and other downstream epigenetic changes in CD4+CD25- T cells that impart a suppressive function. This conversion of peripheral effector T cells to regulatory T cells in the presence of azacitidine was posited to mitigate GVHD while preserving GVL in murine models [61]. Recently, RIC HSCT with azacitidine for treatment of AML was reported to result in increased numbers of regulatory T cells and elicit cytotoxic CD8+ T-cell responses to several tumor antigens (melanoma-associated antigen 1, B melanoma antigen 1, and Wilms tumor antigen 1) [62•].
The multikinase inhibitor sorafenib has been shown in some studies to induce remission states in FLT3-ITD mutation AML; however, these responses may not be durable [63, 64]. In 65 patients with relapsed/refractory FLT3-ITD-positive AML, sorafenib monotherapy was administered without significant toxicity, and 37 % had hematologic remissions [65•]. In patients who had undergone prior HSCT, development of sorafenib resistance occurred later than in those without prior HSCT (median 197 days vs 136 days), suggesting sorafinib does not impair GVL. Indeed, novel targeted agents may provide a niche treatment option for select patients, but treatments that prevent relapse remain the best approach.
Conclusion
HSCT now plays an integral role in the comprehensive treatment strategy for AML. Advances in HLA typing, alternative donor transplantation, conditioning therapy, and supportive care make HSCT a feasible treatment option for most AML patients. Our ability to identify high-risk cohorts, including use of genetic mutational analysis and matched related donors, is improving rapidly and should complement existing prognostic tools. The introduction of novel conditioning therapies, posttransplant maintenance, and immunomodulatory agents will likely play key roles in addressing the problem of relapse after HSCT.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Pasquini MC, Wang Z. Current uses and outcomes of hematopoietic stem cell transplantation 2012. Summary slides. CIBMTR. 2012. Available via http://www.cibmtr.org/referencecenter/slidesreports/summaryslides/pages/index.aspx.
• Stone RM. Acute myeloid leukemia in first remission: to choose transplantation or not? J Clin Oncol. 2013;31(10):1262–6. This is an excellent review of the evidence for and against HSCT in CR1 AML. Relapse risk is discussed in the context of cytogenetic and genetic mutation, with a suggested patient selection algorithm.
Gooley TA, Chien JW, Pergam SA, Hingorani S, Sorror ML, Boeckh M, et al. Reduced mortality after allogeneic hematopoietic-cell transplantation. N Engl J Med. 2010;363(22):2091–101.
Tallman MS, Dewald GW, Gandham S, Logan BR, Keating A, Lazarus HM, et al. Impact of cytogenetics on outcome of matched unrelated donor hematopoietic stem cell transplantation for acute myeloid leukemia in first or second complete remission. Blood. 2007;110(1):409–17.
Koreth J, Schlenk R, Kopecky KJ, Honda S, Sierra J, Djulbegovic BJ, et al. Allogeneic stem cell transplantation for acute myeloid leukemia in first complete remission: systematic review and meta-analysis of prospective clinical trials. JAMA. 2009;301(22):2349–61.
Burnett AK, Goldstone A, Hills RK, Milligan D, Prentice A, Yin J, et al. Curability of patients with acute myeloid leukemia who did not undergo transplantation in first remission. J Clin Oncol. 2013;31(10):1293–301.
• Cornelissen JJ, Breems D, van Putten WL, Gratwohl AA, Passweg JR, Pabst T, et al. Comparative analysis of the value of allogeneic hematopoietic stem-cell transplantation in acute myeloid leukemia with monosomal karyotype versus other cytogenetic risk categories. J Clin Oncol. 2012;30(17):2140–6. This is a large European registry analysis outlining the very poor prognosis of AML with monosomal karyotype. Data supporting a modest benefit for HSCT are given.
Kayser S, Zucknick M, Dohner K, Krauter J, Kohne CH, Horst HA, et al. Monosomal karyotype in adult acute myeloid leukemia: prognostic impact and outcome after different treatment strategies. Blood. 2012;119(2):551–8.
Mohr B, Schetelig J, Schafer-Eckart K, Schmitz N, Hanel M, Rosler W, et al. Impact of allogeneic haematopoietic stem cell transplantation in patients with abnl(17p) acute myeloid leukaemia. Br J Haematol. 2013;161(2):237–44.
• Middeke JM, Beelen D, Stadler M, Gohring G, Schlegelberger B, Baurmann H, et al. Outcome of high-risk acute myeloid leukemia after allogeneic hematopoietic cell transplantation: negative impact of abnl(17p) and −5/5q. Blood. 2012;120(12):2521–8. Similarly to other oncologic diagnoses, abnl(17p) confers one of the worst cytogenetic risks known. In light of these data, such patients are in need of novel therapeutic strategies.
• Armand P, Kim HT, Zhang MJ, Perez WS, Dal Cin PS, Klumpp TR, et al. Classifying cytogenetics in patients with acute myelogenous leukemia in complete remission undergoing allogeneic transplantation: a Center for International Blood and Marrow Transplant Research study. Biol Blood Marrow Transplant. 2012;18(2):280–8. This large registry review by the CIBMTR aims to validate existing cytogenetic risk classification and proposes a new HSCT-specific cytogenic risk model.
Paschka P, Marcucci G, Ruppert AS, Mrozek K, Chen H, Kittles RA, et al. Adverse prognostic significance of KIT mutations in adult acute myeloid leukemia with inv(16) and t(8;21): a Cancer and Leukemia Group B study. J Clin Oncol. 2006;24(24):3904–11.
Liu H, Stock W, Bishop MR. Expanded indications for allogeneic stem cell transplantation in patients with myeloid malignancies. Curr Opin Hematol. 2013;20(2):115–22.
• Ofran Y, Rowe JM. Genetic profiling in acute myeloid leukaemia ─ where are we and what is its role in patient management. Br J Haematol. 2013;160(3):303–20. This excellent review is recommended for the reader seeking a more in depth introduction to the prognostic and predictive roles of genetic profiling in AML.
Rollig C, Bornhauser M, Thiede C, Taube F, Kramer M, Mohr B, et al. Long-term prognosis of acute myeloid leukemia according to the new genetic risk classification of the European LeukemiaNet recommendations: evaluation of the proposed reporting system. J Clin Oncol. 2011;29(20):2758–65.
Brunet S, Labopin M, Esteve J, Cornelissen J, Socie G, Iori AP, et al. Impact of FLT3 internal tandem duplication on the outcome of related and unrelated hematopoietic transplantation for adult acute myeloid leukemia in first remission: a retrospective analysis. J Clin Oncol. 2012;30(7):735–41.
Sengsayadeth SM, Jagasia M, Engelhardt BG, Kassim A, Strickland SA, Goodman S, et al. Allo-SCT for high-risk AML-CR1 in the molecular era: impact of FLT3/ITD outweighs the conventional markers. Bone Marrow Transplant. 2012;47(12):1535–7.
Schlenk RF, Döhner K, Krauter J, Fröhling S, Corbacioglu A, Bullinger L, et al. Mutations and treatment outcome in cytogenetically normal acute myeloid leukemia. N Engl J Med. 2008;358(18):1909–18.
• Brunet S, Martino R, Sierra J. Hematopoietic transplantation for acute myeloid leukemia with internal tandem duplication of FLT3 gene (FLT3/ITD). Curr Opin Oncol. 2013;25(2):195–204. This is an in-depth focused review on the current role of HSCT in treating FLT3-ITD mutation AML.
Marcucci G, Maharry K, Radmacher MD, Mrozek K, Vukosavljevic T, Paschka P, et al. Prognostic significance of, and gene and microRNA expression signatures associated with, CEBPA mutations in cytogenetically normal acute myeloid leukemia with high-risk molecular features: a Cancer and Leukemia Group B study. J Clin Oncol. 2008;26(31):5078–87.
Pratcorona M, Brunet S, Nomdedeu J, Ribera JM, Tormo M, Duarte R, et al. Favorable outcome of patients with acute myeloid leukemia harboring a low-allelic burden FLT3-ITD mutation and concomitant NPM1 mutation: relevance to post-remission therapy. Blood. 2013;121(14):2734–8.
• Patel JP, Gonen M, Figueroa ME, Fernandez H, Sun Z, Racevskis J, et al. Prognostic relevance of integrated genetic profiling in acute myeloid leukemia. N Engl J Med. 2012;366(12):1079–89. Using a panel of 18 genes, the investigators identified somatic alterations in 97% of AML patients. This study demonstrates co-occurrence of mutations and their effect on outcomes in various cytogenetic risk groups. The role of IDH1/IDH2 mutations in the context of NPM1 is reported as are the response of patients with DNMT3A to high-dose daunorubicin.
Walter RB, Gooley TA, Wood BL, Milano F, Fang M, Sorror ML, et al. Impact of pretransplantation minimal residual disease, as detected by multiparametric flow cytometry, on outcome of myeloablative hematopoietic cell transplantation for acute myeloid leukemia. J Clin Oncol. 2011;29(9):1190–7.
Chen Y, Cortes J, Estrov Z, Faderl S, Qiao W, Abruzzo L, et al. Persistence of cytogenetic abnormalities at complete remission after induction in patients with acute myeloid leukemia: prognostic significance and the potential role of allogeneic stem-cell transplantation. J Clin Oncol. 2011;29(18):2507–13.
Oran B, Popat U, Rondon G, Ravandi F, Garcia-Manero G, Abruzzo L, et al. Significance of persistent cytogenetic abnormalities on myeloablative allogeneic stem cell transplantation in first complete remission. Biol Blood Marrow Transplant. 2013;19(2):214–20.
Rosenow F, Berkemeier A, Krug U, Muller-Tidow C, Gerss J, Silling G, et al. CD+ lineage specific donor cell chimerism for the diagnosis and treatment of impending relapse of AML or myelodysplastic syndrome after allo-SCT. Bone Marrow Transplant. 2013. doi:10.1038/bmt.2013.2.
Polak J, Hajkova H, Haskovec C, Cechova H, Marinov I, Mikulenkova D, et al. Quantitative monitoring of WT1 expression in peripheral blood before and after allogeneic stem cell transplantation for acute myeloid leukemia - a useful tool for early detection of minimal residual disease. Neoplasma. 2013;60(1):74–82.
Gupta V, Tallman MS, He W, Logan BR, Copelan E, Gale RP, et al. Comparable survival after HLA-well-matched unrelated or matched sibling donor transplantation for acute myeloid leukemia in first remission with unfavorable cytogenetics at diagnosis. Blood. 2010;116(11):1839–48.
Imahashi N, Suzuki R, Fukuda T, Kakihana K, Kanamori H, Eto T, et al. Allogeneic hematopoietic stem cell transplantation for intermediate cytogenetic risk AML in first CR. Bone Marrow Transplant. 2013;48(1):56–62.
• Saber W, Opie S, Rizzo JD, Zhang MJ, Horowitz MM, Schriber J. Outcomes after matched unrelated donor versus identical sibling hematopoietic cell transplantation in adults with acute myelogenous leukemia. Blood. 2012;119(17):3908–16. This is a very large registry analysis showing equivalent outcomes between matched unrelated donor HSCT and matched related donor HSCT in AML.
Brunstein CG, Fuchs EJ, Carter SL, Karanes C, Costa LJ, Wu J, et al. Alternative donor transplantation after reduced intensity conditioning: results of parallel phase 2 trials using partially HLA-mismatched related bone marrow or unrelated double umbilical cord blood grafts. Blood. 2011;118(2):282–8.
Brunstein CG, Eapen M, Ahn KW, Appelbaum FR, Ballen KK, Champlin RE, et al. Reduced-intensity conditioning transplantation in acute leukemia: the effect of source of unrelated donor stem cells on outcomes. Blood. 2012;119(23):5591–8.
Chen YB, Aldridge J, Kim HT, Ballen KK, Cutler C, Kao G, et al. Reduced-intensity conditioning stem cell transplantation: comparison of double umbilical cord blood and unrelated donor grafts. Biol Blood Marrow Transplant. 2012;18(5):805–12.
• Huang XJ, Zhu HH, Chang YJ, Xu LP, Liu DH, Zhang XH, et al. The superiority of haploidentical related stem cell transplantation over chemotherapy alone as postremission treatment for patients with intermediate- or high-risk acute myeloid leukemia in first complete remission. Blood. 2012;119(23):5584–90. For patients with AML without suitable donors, haploidentical donor HSCT provides a survival advantage compared with chemotherapy alone.
Szer J. The prevalent predicament of relapsed acute myeloid leukemia. Hematol Am Soc Hematol Educ Program. 2012;2012:43–8.
Sorror ML, Sandmaier BM, Storer BE, Franke GN, Laport GG, Chauncey TR, et al. Long-term outcomes among older patients following nonmyeloablative conditioning and allogeneic hematopoietic cell transplantation for advanced hematologic malignancies. JAMA. 2011;306(17):1874–83.
Alatrash G, de Lima M, Hamerschlak N, Pelosini M, Wang X, Xiao L, et al. Myeloablative reduced-toxicity i.v. busulfan-fludarabine and allogeneic hematopoietic stem cell transplant for patients with acute myeloid leukemia or myelodysplastic syndrome in the sixth through eighth decades of life. Biol Blood Marrow Transplant. 2011;17(10):1490–6.
Aoudjhane M, Labopin M, Gorin NC, Shimoni A, Ruutu T, Kolb HJ, et al. Comparative outcome of reduced intensity and myeloablative conditioning regimen in HLA identical sibling allogeneic haematopoietic stem cell transplantation for patients older than 50 years of age with acute myeloblastic leukaemia: a retrospective survey from the Acute Leukemia Working Party (ALWP) of the European group for Blood and Marrow Transplantation (EBMT). Leukemia. 2005;19(12):2304–12.
Ringden O, Labopin M, Ehninger G, Niederwieser D, Olsson R, Basara N, et al. Reduced intensity conditioning compared with myeloablative conditioning using unrelated donor transplants in patients with acute myeloid leukemia. J Clin Oncol. 2009;27(27):4570–7.
Luger SM, Ringden O, Zhang MJ, Perez WS, Bishop MR, Bornhauser M, et al. Similar outcomes using myeloablative vs reduced-intensity allogeneic transplant preparative regimens for AML or MDS. Bone Marrow Transplant. 2012;47(2):203–11.
Bornhauser M, Kienast J, Trenschel R, Burchert A, Hegenbart U, Stadler M, et al. Reduced-intensity conditioning versus standard conditioning before allogeneic haemopoietic cell transplantation in patients with acute myeloid leukaemia in first complete remission: a prospective, open-label randomised phase 3 trial. Lancet Oncol. 2012;13(10):1035–44.
Chen YB, Coughlin E, Kennedy KF, Alyea EP, Armand P, Attar EC, et al. Busulfan dose intensity and outcomes in reduced-intensity allogeneic peripheral blood stem cell transplantation for myelodysplastic syndrome or acute myeloid leukemia. Biol Blood Marrow Transplant. 2013;19(6):981–7.
Nagler A, Labopin M, Shimoni A, Niederwieser D, Mufti GJ, Zander AR, et al. Mobilized peripheral blood stem cells compared with bone marrow as the stem cell source for unrelated donor allogeneic transplantation with reduced-intensity conditioning in patients with acute myeloid leukemia in complete remission: an analysis from the Acute Leukemia Working Party of the European Group for Blood and Marrow Transplantation. Biol Blood Marrow Transplant. 2012;18(9):1422–9.
Weisdorf D, Zhang MJ, Arora M, Horowitz MM, Rizzo JD, Eapen M. Graft-versus-host disease induced graft-versus-leukemia effect: greater impact on relapse and disease-free survival after reduced intensity conditioning. Biol Blood Marrow Transplant. 2012;18(11):1727–33.
Bredeson C, Le-Rademacher J, Zhu X, Burkart J, Kato K, Armstrong E, et al. Improved survival with intravenous busulfan (IV BU) compared to total body irradiation (TBI)-based myeloablative conditioning regimens: a CIBMTR prospective study. Biol Blood Marrow Transplant. 2013;19(2 Suppl):S110–1.
Rozman C, Carreras E, Qian C, Gale RP, Bortin MM, Rowlings PA, et al. Risk factors for hepatic veno-occlusive disease following HLA-identical sibling bone marrow transplants for leukemia. Bone Marrow Transplant. 1996;17(1):75–80.
Liu H, Zhai X, Song Z, Sun J, Xiao Y, Nie D, et al. Busulfan plus fludarabine as a myeloablative conditioning regimen compared with busulfan plus cyclophosphamide for acute myeloid leukemia in first complete remission undergoing allogeneic hematopoietic stem cell transplantation: a prospective and multicenter study. J Hematol Oncol. 2013;6:15.
Chevallier P, Labopin M, Milpied N, Cornelissen JJ, Blaise D, Petersen E, et al. Impact of cytogenetics risk on outcome after reduced intensity conditioning allo-SCT from an HLA-identical sibling for patients with AML in first CR: a report from the acute leukemia working party of EBMT. Bone Marrow Transplant. 2012;47(11):1442–7.
Biggs JC, Horowitz MM, Gale RP, Ash RC, Atkinson K, Helbig W, et al. Bone marrow transplants may cure patients with acute leukemia never achieving remission with chemotherapy. Blood. 1992;80(4):1090–3.
Armistead PM, de Lima M, Pierce S, Qiao W, Wang X, Thall PF, et al. Quantifying the survival benefit for allogeneic hematopoietic stem cell transplantation in relapsed acute myelogenous leukemia. Biol Blood Marrow Transplant. 2009;15(11):1431–8.
Song KW, Lipton J. Is it appropriate to offer allogeneic hematopoietic stem cell transplantation to patients with primary refractory acute myeloid leukemia? Bone Marrow Transplant. 2005;36(3):183–91.
Blennow O, Remberger M, Klingspor L, Omazic B, Fransson K, Ljungman P, et al. Randomized PCR-based therapy and risk factors for invasive fungal infection following reduced-intensity conditioning and hematopoietic SCT. Bone Marrow Transplant. 2010;45(12):1710–8.
Shimoni A, Hardan I, Shem-Tov N, Yeshurun M, Yerushalmi R, Avigdor A, et al. Allogeneic hematopoietic stem-cell transplantation in AML and MDS using myeloablative versus reduced-intensity conditioning: the role of dose intensity. Leukemia. 2006;20(2):322–8.
Magenau J, Tobai H, Pawarode A, Braun T, Peres E, Reddy P, et al. Clofarabine and busulfan conditioning facilitates engraftment and provides significant antitumor activity in nonremission hematologic malignancies. Blood. 2011;118(15):4258–64.
Chevallier P, Labopin M, Buchholz S, Ganser A, Ciceri F, Lioure B, et al. Clofarabine-containing conditioning regimen for allo-SCT in AML/ALL patients: a survey from the Acute Leukemia Working Party of EBMT. Eur J Haematol. 2012;89(3):214–9.
Schmid C, Labopin M, Nagler A, Niederwieser D, Castagna L, Tabrizi R, et al. Treatment, risk factors, and outcome of adults with relapsed AML after reduced intensity conditioning for allogeneic stem cell transplantation. 2012;119(6):1599–606.
Collins Jr RH, Shpilberg O, Drobyski WR, Porter DL, Giralt S, Champlin R, et al. Donor leukocyte infusions in 140 patients with relapsed malignancy after allogeneic bone marrow transplantation. J Clin Oncol. 1997;15(2):433–44.
Warlick ED, DeFor T, Blazar BR, Burns L, Verneris MR, Ustun C, et al. Successful remission rates and survival after lymphodepleting chemotherapy and donor lymphocyte infusion for relapsed hematologic malignancies postallogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2012;18(3):480–6.
Schroeder T, Czibere A, Platzbecker U, Bug G, Uharek L, Luft T, et al. Azacitidine and donor lymphocyte infusions as first salvage therapy for relapse of AML or MDS after allogeneic stem cell transplantation. Leukemia. 2013;27(6):1229–35.
de Lima M, Giralt S, Thall PF, de Padua Silva L, Jones RB, Komanduri K, et al. Maintenance therapy with low-dose azacitidine after allogeneic hematopoietic stem cell transplantation for recurrent acute myelogenous leukemia or myelodysplastic syndrome: a dose and schedule finding study. Cancer. 2010;116(23):5420–31.
Choi J, Ritchey J, Prior JL, Holt M, Shannon WD, Deych E, et al. In vivo administration of hypomethylating agents mitigate graft-versus-host disease without sacrificing graft-versus-leukemia. Blood. 2010;116(1):129–39.
• Goodyear OC, Dennis M, Jilani NY, Loke J, Siddique S, Ryan G, et al. Azacitidine augments expansion of regulatory T cells after allogeneic stem cell transplantation in patients with acute myeloid leukemia (AML). Blood. 2012;119(14):3361–9. Azacitidine is shown here to potentially enhance GVL effects by eliciting cytotoxic T-cell responses and attenuating GVHD by increasing the number of regulatory T cells.
Metzelder S, Wang Y, Wollmer E, Wanzel M, Teichler S, Chaturvedi A, et al. Compassionate use of sorafenib in FLT3-ITD-positive acute myeloid leukemia: sustained regression before and after allogeneic stem cell transplantation. Blood. 2009;113(26):6567–71.
Sharma M, Ravandi F, Bayraktar UD, Chiattone A, Bashir Q, Giralt S, et al. Treatment of FLT3-ITD-positive acute myeloid leukemia relapsing after allogeneic stem cell transplantation with sorafenib. Biol Blood Marrow Transplant. 2011;17(12):1874–7.
• Metzelder SK, Schroeder T, Finck A, Scholl S, Fey M, Gotze K, et al. High activity of sorafenib in FLT3-ITD-positive acute myeloid leukemia synergizes with allo-immune effects to induce sustained responses. Leukemia. 2012;26(11):2353–9. This article describes the clinical activity of sorafenib in FLT3-ITD-positive AML, and this should be considered as a treatment of post-HSCT relapse in this cohort.
Compliance with ethics Guidelines
Conflict of Interest
John Magenau and Daniel Ricardo Couriel declare that they have no conflict of interest
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Magenau, J., Couriel, D.R. Hematopoietic Stem Cell Transplantation for Acute Myeloid Leukemia: To Whom, When, and How. Curr Oncol Rep 15, 436–444 (2013). https://doi.org/10.1007/s11912-013-0340-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11912-013-0340-6