Abstract
The long-standing debate of whether patients with acute myeloid leukemia (AML) should proceed to allogeneic hematopoietic cell transplantation (HCT) during first complete remission (CR1) remains unsettled. Although allogeneic HCT during CR1 used to be recommended for those with intermediate or poor cytogenetics if they had a matched sibling donor, the concept of indications for allogeneic HCT during CR1 has been evolving by virtue of advances in understanding of the molecular pathogenesis of AML and innovations in transplantation practice attained over the last few decades. The incorporation of molecular profiles of leukemia has been shown to contribute to further refinements of risk classification that had previously relied mostly on cytogenetics, while the progress in transplantation procedures has made it possible to perform transplantations more safely even for patients without a matched sibling donor. These significant changes have underpinned the need to reappraise indications for allogeneic HCT during CR1 of AML. Improvements in clinical applications of genetic and measurable residual disease information as well as in transplantation technology are expected to further refine indications for allogeneic HCT during CR1, and thus promote an individualized approach for the treatment of AML.
Similar content being viewed by others
Introduction
Allogeneic hematopoietic cell transplantation (HCT) is the most effective therapy for preventing relapse of acute myeloid leukemia (AML), which is the predominant cause of death for patients with the disease [1]. However, the efficacy of allogeneic HCT is compromised by high rates of morbidity and mortality related to the procedure. As a consequence, allogeneic HCT may be beneficial for some patients, but harmful for others, which makes it a matter of clinical concern whether allogeneic HCT should be recommended for AML patients who have attained first complete remission (CR1). This question has historically been examined in prospective studies that used biologic assignment according to donor availability, in which patients with a human leukocyte antigen (HLA)-identical sibling were assigned to undergo allogeneic HCT, while those without such a donor were assigned to chemotherapy with or without autologous HCT [2,3,4,5,6,7,8,9,10,11]. By integrating results obtained from such “donor vs no-donor” studies, a couple of meta-analysis studies published in the late 2000s showed that the beneficial effect of allogeneic HCT is greatest for patients with poor cytogenetics, also present for those with intermediate cytogenetics, but nonexistent for those with favorable cytogenetics [12, 13]. These results, however, do not seem to be directly applicable to current conditions for the following reasons. First, the practice of transplantation itself has evolved. With the advent of transplantation from alternative donors, donor versus no-donor studies have become less relevant today, because a considerable number of patients without a matched sibling donor may qualify for receiving allogeneic HCT from a matched unrelated donor, umbilical cord blood (UCB) or a haploidentical related donor [14, 15]. Second, our understanding of the molecular pathogenesis of AML has evolved. It is well recognized that the prognosis for patients in each cytogenetic risk group is still heterogeneous, and the incorporation of molecular profiles of leukemia has been shown to contribute to further refinements of risk classification that had previously relied mostly on cytogenetics [16, 17]. These significant changes attained over the last few decades have underpinned the need to reappraise indications for allogeneic HCT during CR1 of AML.
Basic principle
Because AML is a heterogenous disease consisting of subsets with distinct biological and prognostic features, a risk-adapted approach is a rational way for determining which patients should be selected for allogeneic HCT during CR1. The risk of relapse following chemotherapy and the risk of nonrelapse mortality (NRM) following allogeneic HCT represent the two most important factors to be taken into consideration. In 2012, experts provided, on behalf of the European LeukemiaNet (ELN), specific recommendations for indications for allogeneic HCT during CR1 of AML [18]. According to their recommendations, patients are classified into four relapse-risk groups primarily based on their genetic and cytogenetic profiles, and an acceptable post-transplant NRM rate is proposed for each of the groups (Table 1). This guide supports our clinical decision-making in daily practice.
Outcomes following chemotherapy according to genetic and cytogenetic status
It is widely accepted that cytogenetic findings at diagnosis are closely associated with the biology of AML and have important prognostic implications for patients treated with conventional chemotherapy [4, 19, 20]. Despite the usefulness of cytogenetic risk stratification, however, patients in each cytogenetic risk group remain prognostically heterogeneous. Subsequent studies have shown that mutations in the FLT3, NPM1, and CEBPA genes are useful for stratifying patients with cytogenetically normal AML (CN-AML) into different prognostic subgroups [21,22,23,24,25,26,27,28,29,30,31,32]. In 2010, the ELN first proposed a risk stratification system for AML, by integrating genetic and cytogenetic profiles of leukemia (Table 2) [33]. The ELN 2010 system took into account the presence or absence of mutations in the FLT3, NPM1, CEBPA genes to classify patients with normal karyotype. In 2017, the ELN 2010 risk classification was updated in light of the enhanced understanding of prognostic significance of genetic profiles (Table 3) [17]. The ELN 2017 system eliminated the distinction between the intermediate-I and the intermediate-II categories, resulting in the reduction of the number of risk categories from four to three. Furthermore, the use of gene mutations for risk classification is no longer restricted to patients with normal karyotype. Other major amendments include the consideration of only biallelic CEBPA mutations for the favorable-risk category, stratification of patients with internal tandem duplication (ITD) of the FLT3 gene based on the allelic ratio, and the inclusion of RUNX1, ASXL1, and TP53 mutations in the adverse-risk category. In addition, the ELN 2017 system has incorporated monosomal karyotype (MK) into the adverse-risk category. MK is defined as two or more autosomal monosomies or a single autosomal monosomy plus other structural abnormalities, and has recently been shown to be predictive of extremely poor prognosis [34,35,36,37].
The clinical utility of the ELN 2017 system has been validated in a large cohort of patients enrolled on two successive trials conducted by the German AML Cooperative Group (AMLCG), in which the ELN 2017 system proved to show a better discrimination of risk groups than the ELN 2010 system [38]. The incorporation of additional genetic information in the ELN 2017 system has contributed to the identification of more patients falling under the favorable- and adverse-risk categories. The usefulness of the ELN 2017 system has been confirmed by other studies, although some controversies remain, for example, regarding the prognostic significance of the allelic ratio of FLT3-ITD [39,40,41,42].
More detailed assessments of genetic profiles may further refine the ELN 2017 risk classification. Investigators in the Cancer and Leukemia Group B (CALGB) have shown that NPM1/ WT1 co-mutations, DNMT3A mutations, ZRSR2 mutations, and mutated NPM1 with FLT3-ITD high allelic ratio represent an adverse prognosis [43], which suggests that an inclusion of additional gene mutations may identify more patients with poor prognosis.
Outcomes following allogeneic HCT according to genetic and cytogenetic status
Cytogenetics can also predict outcomes after allogeneic HCT [44, 45]. Several studies have evaluated whether and to what extent post-transplant outcomes differ according to specific mutation status [46,47,48,49]. A study conducted by the Center for International Blood and Marrow Transplantation Research compared patients with or without FLT3 mutations who underwent allogeneic HCT during CR1 or second CR (CR2) [47]. For this study, data on the type of mutations, that is, ITD or tyrosine kinase domain mutations, were not available, and thus they were combined to form a FLT3-mutated group. Patients with FLT3-mutated AML showed a higher risk of post-transplant relapse, but there was no difference in NRM, relapse-free survival (RFS), or overall survival (OS) on the basis of the presence or absence of the FLT3 mutations.
The European Society for Blood and Marrow Transplantation (EBMT) study analyzed the effect of combinations of the NPM1 mutation and FLT3-ITD status on outcomes after allogeneic HCT for CN-AML [46]. In this study, molecularly defined subgroups were found to have different prognoses, with the best outcomes for the mutated NPM1 group without FLT3-ITD. Patients with wild-type NPM1 without FLT3-ITD had similarly favorable results, whereas outcomes were inferior for those with FLT3-ITD. More recently, the EBMT has proposed a prognostic model based on cytogenetics and FLT3-ITD for patients undergoing allogeneic HCT during CR1 [48]. This study showed that the presence of FLT3-ITD was significantly associated with worse outcomes only for the intermediate cytogenetic risk group.
Investigators at Leipzig University examined the prognostic impact of the ELN 2017 system in a cohort of patients treated with allogeneic HCT at their single center [49]. The study results showed that the ELN 2017 classification made it possible to differentiate patients into three groups with significantly distinct prognoses.
Risk of nonrelapse mortality following allogeneic HCT
Post-transplant NRM is another important factor when deciding indications for allogeneic HCT during CR1. Despite availability of several predicting systems for NRM after allogeneic HCT [50,51,52,53,54,55,56], the establishment of an accurate prediction model remains a challenge because the risk of NRM is multifactorial and can therefore vary according to disease and disease status. In response to this situation, we recently developed a comprehensive system to provide more accurate predictions of NRM during their CR1 for AML patients having undergone allogeneic HCT [57]. After assigning 2344 patients to a training set or a validation set, we first identified and scored five parameters—age, sex, performance status (PS), HCT-specific comorbidity index (HCT-CI), and donor type—on the basis of their effect on NRM in the training set. The new scoring system which was named the “NRM-J index”, used the sum of the assigned scores to stratify patients into four distinct risk groups, 0–3 points, 4 points, 5 points, and 6 or more points (Table 4). The application of the NRM-J index to patients in the validation set resulted in a clear differentiation of NRM, with expected 2-year rates of 11%, 16%, 27%, and 33%, respectively. The discriminative capability of the NRM-J index was found to be better than that of the EBMT score [50] or the HCT-CI [51]. The NRM-J index was developed based on data of patients with AML undergoing allogeneic HCT during first CR, which makes it more specific to this patient population. When combined with the ELN recommendations shown in Table 1 [18], the NRM-J index is expected to be able to provide practical guidance for indications for allogeneic HCT during CR1.
Studies comparing transplant versus non-transplant strategy for genetically distinct populations
Several studies have evaluated the efficacy of allogeneic HCT in comparison to that of chemotherapy with or without autologous HCT for patients with distinct genetic features [58,59,60,61,62,63,64]. However, the number of patients in any given genetic subgroup is generally small, which precludes a firm conclusion regarding the utility of allogeneic HCT, even from the results of an analysis of a large cohort. Therefore, most of such studies comparing allogeneic HCT with non-transplant therapy were post-hoc analyses based on pooled data of multiple prospective studies [58, 59, 62,63,64].
Schlenk et al. analyzed patients with CN-AML who entered one of four trials conducted by the German–Austrian Acute Myeloid Leukemia Study Group (AMLSG), in which only patients with a matched related donor were assigned to undergo allogeneic HCT [58]. Within the favorable subgroup of patients with mutant NPM1 without FLT3-ITD, donor availability did not make any difference in terms of RFS. For those with mutant CEBPA, a donor vs no-donor analysis could not be done because of limited sample size. For the remaining patients with non-favorable risk, the donor group showed better RFS than the no-donor group.
Röllig et al., on behalf of the Study Alliance Leukemia (SAL), evaluated outcomes for cytogenetically intermediate-risk patients with mutant NPM1 enrolled in their AML 2003 trial [60]. Patients in the donor group showed significantly better RFS than those in the no-donor group. However, OS of the donor and no-donor groups did not differ, primarily because of high rates of CR2 attainment after relapse and of proceeding to allogeneic HCT from an alternative donor for patients in the no-donor group. The SAL investigators also reported results of a donor versus no-donor analysis for patients with intermediate cytogenetics who had no FLT3-ITD, NPM1-, or biallelic CEBPA mutations who were enrolled on two prospective trials [63]. This study showed that RFS was significantly better for patients in the donor group than the no-donor group, but the difference in OS again did not reach statistical significance. Investigators from the Dutch–Belgian Hemato-Oncology Cooperative Group and Swiss Group for Clinical Cancer Research (HOVON/SAKK) evaluated the efficacy of allogeneic HCT for AML with MK, by using data of patients who participated in their three consecutive phase 3 trials [59]. For these studies, poor-risk patients were assigned to allogeneic HCT if a matched sibling or unrelated donor could be identified. They used allogeneic HCT as a time-dependent covariate, and showed a significant advantage of allogeneic HCT in terms of reduction of relapse and improvement of survival. The beneficial effect of allogeneic HCT for AML with MK was also reported by a joint study conducted by the European Organization for Research and Treatment of Cancer (EORTC) and the Gruppo Italiano Malattie Ematologiche dell’Adulto (GIMEMA), in which OS was shown to be better for patients with an HLA-identical related donor based on a donor versus no-donor analysis [64].
Measurable residual disease
Measurable residual disease (MRD) during and after treatment detected by flow cytometry, quantitative PCR, or next-generation sequencing (NGS) has emerged as a novel indicator for response to therapy. Achievement of MRD negativity has been shown in many studies of AML patients to be a powerful prognostic factor [65,66,67,68,69,70,71,72,73,74].
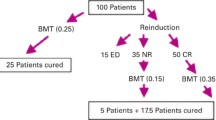
Freeman et al. attempted to determine the prognostic impact of MRD measured by multiparameter flow cytometry (MFC) after one course of induction therapy in a cohort of patients enrolled and treated in the National Cancer Research Institute (NCRI) AML17 trial [71]. The prognosis of patients who achieved CR could be clearly differentiated by the presence or absence of MRD, with OS for patients with MRD-positive CR resembling that for patients with partial remission rather than that for patients with MRD-negative CR.
Balsat et al. assessed post-induction NPM1-mutated MRD for patients enrolled in the Acute Leukemia French Association (ALFA) 0702 trial to determine whether NPM1 MRD can be used as a predictive factor for benefits from allogeneic HCT [70]. After induction therapy, patients who did not achieve a 4-log reduction in NPM1 MRD in the peripheral blood had a higher incidence of relapse and a shorter OS. Outcomes were significantly improved by the use of allogeneic HCT for patients with a less than 4-log reduction in NPM1 MRD, but this benefit was not observed for those with a more than 4-log reduction.
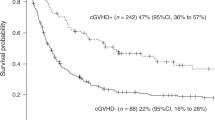
Jongen-Lavrencic et al. from the HOVON/SAKK group analyzed samples of bone marrow or peripheral blood before and after induction therapy by using NGS, and demonstrated that the detection of persistent mutations during CR, except for those associated with clonal hematopoiesis, are predictive of higher relapse and worse OS [72]. They also showed that NGS and MFC each had independent and additive prognostic value with respect to relapse and survival.
The GIMEMA investigators conducted a prospective study to test a treatment approach risk-adapted according to genetic and cytogenetic profiles at diagnosis and post-consolidation MRD status as defined by MFC [74]. Patients with favorable and poor risk were assigned to autologous and allogeneic HCT, respectively, regardless of MRD status, and those with intermediate risk were assigned to autologous if MRD was negative, and to allogeneic HCT if MRD was positive. This study showed similar RFS for patients with intermediate risk with or without MRD, and their RFS was almost identical to that for patients with favorable risk. These results suggest that, for patients with intermediate risk, allogeneic HCT may be able to override poor prognosis associated with positive MRD, and also that it may be possible to avoid allogeneic HCT if MRD is negative.
Although MRD response has been shown to be predictive of better outcomes [65,66,67,68,69,70,71,72,73,74], there is a significant heterogeneity across studies depending on the patient population, regimen used, MRD method and target, timing of MRD assessment, and threshold to define adequate response [75]. To focus the knowledge incorporating the findings of various studies on the clinical utility of MRD and generalize this knowledge for use in clinical practice, the priority needs be placed on attainment of standardization of the measuring procedure.
Future considerations
The last few decades have witnessed significant improvements in risk estimation for relapse by taking profiles of selected genes into account. However, some uncertainties remain regarding genetic risk in AML. First, elucidation of the genetic landscape of AML is still a work in progress, and novel genetic mutations of clinical significance are sure to be identified hereafter. Second, specific combinations of mutations may have an impact [76]. Third, a risk classification may be subject to the effect of treatments given to the patients analyzed. Accordingly, genetic mutations considered as adverse or favorable for patients treated with standard chemotherapy may lose their prognostic capability for patients treated with hypomethylating agents [77, 78] or venetoclax-based regimens [79, 80], and the addition of targeted agents, such as FLT3, IDH1, and IDH2 inhibitors to standard chemotherapy may cause changes in genetic risk classification [81, 82]. Because of the limited number of patients with a given type of genetic mutation, intergroup collaborations are required to develop and upgrade an accurate genetic risk classification system.
Another aspect to be taken into account is that indications for allogeneic HCT cannot be determined by genetic risk alone. The prognosis for patients in a genetically adverse-risk category is worse not only when they are treated with chemotherapy but also when they are treated with allogeneic HCT. What matters is whether there is a net benefit for the patients when they do or do not proceed to allogeneic HCT during CR1. This highlights the importance of comprehensive assessments by considering not only genetic and cytogenetic profiles but also age, comorbidities, PS and other factors. One major challenge would be the development of algorithms that combine pre-treatment risk factors and longitudinal MRD data to guide individualized treatments. In recent years, a knowledge bank that integrates clinical, genetic, cytogenetic, and therapeutic variables has been developed to estimate individualized survival. The French group evaluated use of the knowledge bank approach to act as a guide for decisions as to whether to proceed to allogeneic HCT during first CR by using data for patients enrolled in their ALFA 0702 trial [83]. The knowledge bank approach proved to not only result in more accurate survival prediction than the ELN 2017 system, but also better identified patients who might benefit from allogeneic HCT or chemotherapy alone.
Conclusions
The long-standing debate of whether AML patients in CR1 should proceed to allogeneic HCT remains unsettled. Although allogeneic HCT during CR1 used to be recommended only for those with intermediate or poor cytogenetics if they had a matched sibling donor [12, 13], the concept of indications for allogeneic HCT during CR1 has been evolving by virtue of advances in understanding of the molecular pathogenesis of AML and innovations in transplantation practice attained over the last few decades. Improvements in clinical applications of genetic and MRD information as well as in transplantation technology can be expected to further refine indications for allogeneic HCT during CR1 and promote an individualized approach for the treatment of AML.
References
Yanada M, Takami A, Yamasaki S, Arai Y, Konuma T, Uchida N, et al. Allogeneic hematopoietic cell transplantation for adults with acute myeloid leukemia conducted in Japan during the past quarter century. Ann Hematol. 2020;99:1351–60.
Zittoun RA, Mandelli F, Willemze R, de Witte T, Labar B, Resegotti L, et al. Autologous or allogeneic bone marrow transplantation compared with intensive chemotherapy in acute myelogenous leukemia. European Organization for Research and Treatment of Cancer (EORTC) and the Gruppo Italiano Malattie Ematologiche Maligne dell’Adulto (GIMEMA) Leukemia Cooperative Groups. N Engl J Med. 1995;332:217–23.
Keating S, de Witte T, Suciu S, Willemze R, Hayat M, Labar B, et al. The influence of HLA-matched sibling donor availability on treatment outcome for patients with AML: an analysis of the AML 8A study of the EORTC Leukaemia Cooperative Group and GIMEMA. European Organization for Research and Treatment of Cancer. Gruppo Italiano Malattie Ematologiche Maligne dell’Adulto. Br J Haematol. 1998;102:1344–53.
Slovak ML, Kopecky KJ, Cassileth PA, Harrington DH, Theil KS, Mohamed A, et al. Karyotypic analysis predicts outcome of preremission and postremission therapy in adult acute myeloid leukemia: a Southwest Oncology Group/Eastern Cooperative Oncology Group Study. Blood. 2000;96:4075–83.
Burnett AK, Wheatley K, Goldstone AH, Stevens RF, Hann IM, Rees JH, et al. The value of allogeneic bone marrow transplant in patients with acute myeloid leukaemia at differing risk of relapse: results of the UK MRC AML 10 trial. Br J Haematol. 2002;118:385–400.
Suciu S, Mandelli F, de Witte T, Zittoun R, Gallo E, Labar B, et al. Allogeneic compared with autologous stem cell transplantation in the treatment of patients younger than 46 years with acute myeloid leukemia (AML) in first complete remission (CR1): an intention-to-treat analysis of the EORTC/GIMEMAAML-10 trial. Blood. 2003;102:1232–40.
Schlenk RF, Benner A, Hartmann F, del Valle F, Weber C, Pralle H, et al. Risk-adapted postremission therapy in acute myeloid leukemia: results of the German multicenter AML HD93 treatment trial. Leukemia 2003;17:1521–8.
Jourdan E, Boiron JM, Dastugue N, Vey N, Marit G, Rigal-Huguet F, et al. Early allogeneic stem-cell transplantation for young adults with acute myeloblastic leukemia in first complete remission: an intent-to-treat long-term analysis of the BGMT experience. J Clin Oncol. 2005;23:7676–84.
Cornelissen JJ, van Putten WL, Verdonck LF, Theobald M, Jacky E, Daenen SM, et al. Results of a HOVON/SAKK donor versus no-donor analysis of myeloablative HLA-identical sibling stem cell transplantation in first remission acute myeloid leukemia in young and middle-aged adults: benefits for whom? Blood. 2007;109:3658–66.
Basara N, Schulze A, Wedding U, Mohren M, Gerhardt A, Junghanss C, et al. Early related or unrelated haematopoietic cell transplantation results in higher overall survival and leukaemia-free survival compared with conventional chemotherapy in high-risk acute myeloid leukaemia patients in first complete remission. Leukemia. 2009;23:635–40.
Sakamaki H, Miyawaki S, Ohtake S, Emi N, Yagasaki F, Mitani K, et al. Allogeneic stem cell transplantation versus chemotherapy as post-remission therapy for intermediate or poor risk adult acute myeloid leukemia: results of the JALSG AML97 study. Int J Hematol. 2010;91:284–92.
Yanada M, Matsuo K, Emi N, Naoe T. Efficacy of allogeneic hematopoietic stem cell transplantation depends on cytogenetic risk for acute myeloid leukemia in first disease remission: a metaanalysis. Cancer 2005;103:1652–8.
Koreth J, Schlenk R, Kopecky KJ, Honda S, Sierra J, Djulbegovic BJ, et al. Allogeneic stem cell transplantation for acute myeloid leukemia in first complete remission: systematic review and meta-analysis of prospective clinical trials. JAMA. 2009;301:2349–61.
Kekre N, Antin JH. Hematopoietic stem cell transplantation donor sources in the 21st century: choosing the ideal donor when a perfect match does not exist. Blood. 2014;124:334–43.
Yanada M. Allogeneic hematopoietic cell transplantation for acute myeloid leukemia during first complete remission: a clinical perspective. Int J Hematol. 2015;101:243–54.
Grimwade D, Ivey A, Huntly BJ. Molecular landscape of acute myeloid leukemia in younger adults and its clinical relevance. Blood. 2016;127:29–41.
Dohner H, Estey E, Grimwade D, Amadori S, Appelbaum FR, Buchner T, et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood. 2017;129:424–47.
Cornelissen JJ, Gratwohl A, Schlenk RF, Sierra J, Bornhauser M, Juliusson G, et al. The European LeukemiaNet AML Working Party consensus statement on allogeneic HSCT for patients with AML in remission: an integrated-risk adapted approach. Nat Rev Clin Oncol. 2012;9:579–90.
Byrd JC, Mrozek K, Dodge RK, Carroll AJ, Edwards CG, Arthur DC, et al. Pretreatment cytogenetic abnormalities are predictive of induction success, cumulative incidence of relapse, and overall survival in adult patients with de novo acute myeloid leukemia: results from Cancer and Leukemia Group B (CALGB 8461). Blood. 2002;100:4325–36.
Grimwade D, Hills RK, Moorman AV, Walker H, Chatters S, Goldstone AH, et al. Refinement of cytogenetic classification in acute myeloid leukemia: determination of prognostic significance of rare recurring chromosomal abnormalities among 5876 younger adult patients treated in the United Kingdom Medical Research Council trials. Blood. 2010;116:354–65.
Kiyoi H, Naoe T, Nakano Y, Yokota S, Minami S, Miyawaki S, et al. Prognostic implication of FLT3 and N-RAS gene mutations in acute myeloid leukemia. Blood. 1999;93:3074–80.
Kottaridis PD, Gale RE, Frew ME, Harrison G, Langabeer SE, Belton AA, et al. The presence of a FLT3 internal tandem duplication in patients with acute myeloid leukemia (AML) adds important prognostic information to cytogenetic risk group and response to the first cycle of chemotherapy: analysis of 854 patients from the United Kingdom Medical Research Council AML 10 and 12 trials. Blood. 2001;98:1752–9.
Yamamoto Y, Kiyoi H, Nakano Y, Suzuki R, Kodera Y, Miyawaki S, et al. Activating mutation of D835 within the activation loop of FLT3 in human hematologic malignancies. Blood. 2001;97:2434–9.
Thiede C, Steudel C, Mohr B, Schaich M, Schakel U, Platzbecker U, et al. Analysis of FLT3-activating mutations in 979 patients with acute myelogenous leukemia: association with FAB subtypes and identification of subgroups with poor prognosis. Blood. 2002;99:4326–35.
Schnittger S, Schoch C, Dugas M, Kern W, Staib P, Wuchter C, et al. Analysis of FLT3 length mutations in 1003 patients with acute myeloid leukemia: correlation to cytogenetics, FAB subtype, and prognosis in the AMLCG study and usefulness as a marker for the detection of minimal residual disease. Blood. 2002;100:59–66.
Boissel N, Cayuela JM, Preudhomme C, Thomas X, Grardel N, Fund X, et al. Prognostic significance of FLT3 internal tandem repeat in patients with de novo acute myeloid leukemia treated with reinforced courses of chemotherapy. Leukemia. 2002;16:1699–704.
Falini B, Mecucci C, Tiacci E, Alcalay M, Rosati R, Pasqualucci L, et al. Cytoplasmic nucleophosmin in acute myelogenous leukemia with a normal karyotype. N Engl J Med. 2005;352:254–66.
Schnittger S, Schoch C, Kern W, Mecucci C, Tschulik C, Martelli MF, et al. Nucleophosmin gene mutations are predictors of favorable prognosis in acute myelogenous leukemia with a normal karyotype. Blood. 2005;106:3733–9.
Dohner K, Schlenk RF, Habdank M, Scholl C, Rucker FG, Corbacioglu A, et al. Mutant nucleophosmin (NPM1) predicts favorable prognosis in younger adults with acute myeloid leukemia and normal cytogenetics: interaction with other gene mutations. Blood. 2005;106:3740–6.
Thiede C, Koch S, Creutzig E, Steudel C, Illmer T, Schaich M, et al. Prevalence and prognostic impact of NPM1 mutations in 1485 adult patients with acute myeloid leukemia (AML). Blood. 2006;107:4011–20.
Marcucci G, Maharry K, Radmacher MD, Mrozek K, Vukosavljevic T, Paschka P, et al. Prognostic significance of, and gene and microRNA expression signatures associated with, CEBPA mutations in cytogenetically normal acute myeloid leukemia with high-risk molecular features: a Cancer and Leukemia Group B Study. J Clin Oncol. 2008;26:5078–87.
Wouters BJ, Lowenberg B, Erpelinck-Verschueren CA, van Putten WL, Valk PJ, Delwel R. Double CEBPA mutations, but not single CEBPA mutations, define a subgroup of acute myeloid leukemia with a distinctive gene expression profile that is uniquely associated with a favorable outcome. Blood. 2009;113:3088–91.
Dohner H, Estey EH, Amadori S, Appelbaum FR, Buchner T, Burnett AK, et al. Diagnosis and management of acute myeloid leukemia in adults: recommendations from an international expert panel, on behalf of the European LeukemiaNet. Blood. 2010;115:453–74.
Breems DA, Van Putten WL, De Greef GE, Van Zelderen-Bhola SL, Gerssen-Schoorl KB, Mellink CH, et al. Monosomal karyotype in acute myeloid leukemia: a better indicator of poor prognosis than a complex karyotype. J Clin Oncol. 2008;26:4791–7.
Medeiros BC, Othus M, Fang M, Roulston D, Appelbaum FR. Prognostic impact of monosomal karyotype in young adult and elderly acute myeloid leukemia: the Southwest Oncology Group (SWOG) experience. Blood. 2010;116:2224–8.
Yanada M, Kurosawa S, Yamaguchi T, Yamashita T, Moriuchi Y, Ago H, et al. Prognosis of acute myeloid leukemia harboring monosomal karyotype in patients treated with or without allogeneic hematopoietic cell transplantation after achieving complete remission. Haematologica. 2012;97:915–8.
Kayser S, Zucknick M, Dohner K, Krauter J, Kohne CH, Horst HA, et al. Monosomal karyotype in adult acute myeloid leukemia: prognostic impact and outcome after different treatment strategies. Blood 2012;119:551–8.
Herold T, Rothenberg-Thurley M, Grunwald VV, Janke H, Goerlich D, Sauerland MC, et al. Validation and refinement of the revised 2017 European LeukemiaNet genetic risk stratification of acute myeloid leukemia. Leukemia. 2020;34:3161–72.
Harada Y, Nagata Y, Kihara R, Ishikawa Y, Asou N, Ohtake S, et al. Prognostic analysis according to the 2017 ELN risk stratification by genetics in adult acute myeloid leukemia patients treated in the Japan Adult Leukemia Study Group (JALSG) AML201 study. Leuk Res. 2018;66:20–27.
Sakaguchi M, Yamaguchi H, Najima Y, Usuki K, Ueki T, Oh I, et al. Prognostic impact of low allelic ratio FLT3-ITD and NPM1 mutation in acute myeloid leukemia. Blood Adv. 2018;2:2744–54.
Boddu PC, Kadia TM, Garcia-Manero G, Cortes J, Alfayez M, Borthakur G, et al. Validation of the 2017 European LeukemiaNet classification for acute myeloid leukemia with NPM1 and FLT3-internal tandem duplication genotypes. Cancer. 2019;125:1091–100.
Döhner K, Thiede C, Jahn N, Panina E, Gambietz A, Larson RA, et al. Impact of NPM1/FLT3-ITD genotypes defined by the 2017 European LeukemiaNet in patients with acute myeloid leukemia. Blood 2020;135:371–80.
Eisfeld AK, Kohlschmidt J, Mims A, Nicolet D, Walker CJ, Blachly JS, et al. Additional gene mutations may refine the 2017 European LeukemiaNet classification in adult patients with de novo acute myeloid leukemia aged <60 years. Leukemia. 2020;34:3215–27.
Armand P, Kim HT, Zhang MJ, Perez WS, Dal Cin PS, Klumpp TR, et al. Classifying cytogenetics in patients with acute myelogenous leukemia in complete remission undergoing allogeneic transplantation: a Center for International Blood and Marrow Transplant Research study. Biol Blood Marrow Transplant. 2012;18:280–8.
Yanada M, Mori J, Aoki J, Harada K, Mizuno S, Uchida N, et al. Effect of cytogenetic risk status on outcomes for patients with acute myeloid leukemia undergoing various types of allogeneic hematopoietic cell transplantation: an analysis of 7812 patients. Leuk Lymphoma. 2018;59:601–09.
Schmid C, Labopin M, Socie G, Daguindau E, Volin L, Huynh A, et al. Outcome of patients with distinct molecular genotypes and cytogenetically normal AML after allogeneic transplantation. Blood. 2015;126:2062–9.
Deol A, Sengsayadeth S, Ahn KW, Wang HL, Aljurf M, Antin JH, et al. Does FLT3 mutation impact survival after hematopoietic stem cell transplantation for acute myeloid leukemia? A Center for International Blood and Marrow Transplant Research (CIBMTR) analysis. Cancer. 2016;122:3005–14.
Canaani J, Labopin M, Itala-Remes M, Blaise D, Socie G, Forcade E, et al. Prognostic significance of recurring chromosomal abnormalities in transplanted patients with acute myeloid leukemia. Leukemia. 2019;33:1944–52.
Grimm J, Jentzsch M, Bill M, Goldmann K, Schulz J, Niederwieser D, et al. Prognostic impact of the ELN2017 risk classification in patients with AML receiving allogeneic transplantation. Blood Adv. 2020;4:3864–74.
Gratwohl A, Hermans J, Goldman JM, Arcese W, Carreras E, Devergie A, et al. Risk assessment for patients with chronic myeloid leukaemia before allogeneic blood or marrow transplantation. Chronic Leukemia Working Party of the European Group for Blood and Marrow Transplantation. Lancet. 1998;352:1087–92.
Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG, et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood. 2005;106:2912–9.
Barba P, Martino R, Perez-Simon JA, Fernandez-Aviles F, Castillo N, Pinana JL, et al. Combination of the Hematopoietic Cell Transplantation Comorbidity Index and the European Group for Blood and Marrow Transplantation score allows a better stratification of high-risk patients undergoing reduced-toxicity allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2014;20:66–72.
Sorror ML, Storb RF, Sandmaier BM, Maziarz RT, Pulsipher MA, Maris MB, et al. Comorbidity-age index: a clinical measure of biologic age before allogeneic hematopoietic cell transplantation. J Clin Oncol. 2014;32:3249–56.
Versluis J, Labopin M, Niederwieser D, Socie G, Schlenk RF, Milpied N, et al. Prediction of non-relapse mortality in recipients of reduced intensity conditioning allogeneic stem cell transplantation with AML in first complete remission. Leukemia. 2015;29:51–7.
Kongtim P, Parmar S, Milton DR, Perez JMR, Rondon G, Chen J, et al. Impact of a novel prognostic model, hematopoietic cell transplant-composite risk (HCT-CR), on allogeneic transplant outcomes in patients with acute myeloid leukemia and myelodysplastic syndrome. Bone Marrow Transplant. 2019;54:839–48.
Shouval R, Fein JA, Shouval A, Danylesko I, Shem-Tov N, Zlotnik M, et al. External validation and comparison of multiple prognostic scores in allogeneic hematopoietic stem cell transplantation. Blood Adv. 2019;3:1881–90.
Yanada M, Konuma T, Mizuno S, Saburi M, Shinohara A, Tanaka M, et al. Predicting non-relapse mortality following allogeneic hematopoietic cell transplantation during first remission of acute myeloid leukemia. Bone Marrow Transplant. 2021;56:387–94.
Schlenk RF, Dohner K, Krauter J, Frohling S, Corbacioglu A, Bullinger L, et al. Mutations and treatment outcome in cytogenetically normal acute myeloid leukemia. N Engl J Med. 2008;358:1909–18.
Cornelissen JJ, Breems D, van Putten WL, Gratwohl AA, Passweg JR, Pabst T, et al. Comparative analysis of the value of allogeneic hematopoietic stem-cell transplantation in acute myeloid leukemia with monosomal karyotype versus other cytogenetic risk categories. J Clin Oncol. 2012;30:2140–6.
Rollig C, Bornhauser M, Kramer M, Thiede C, Ho AD, Kramer A, et al. Allogeneic stem-cell transplantation in patients with NPM1-mutated acute myeloid leukemia: results from a prospective donor versus no-donor analysis of patients after upfront HLA typing within the SAL-AML 2003 trial. J Clin Oncol. 2015;33:403–10.
Kurosawa S, Yamaguchi H, Yamaguchi T, Fukunaga K, Yui S, Wakita S, et al. Decision analysis of postremission therapy in cytogenetically intermediate-risk acute myeloid leukemia: the impact of FLT3 internal tandem duplication, nucleophosmin, and CCAAT/enhancer binding protein alpha. Biol Blood Marrow Transplant. 2016;22:1125–32.
Versluis J, In ‘t Hout FE, Devillier R, van Putten WL, Manz MG, Vekemans MC, et al. Comparative value of post-remission treatment in cytogenetically normal AML subclassified by NPM1 and FLT3-ITD allelic ratio. Leukemia. 2017;31:26–33.
Heidrich K, Thiede C, Schäfer-Eckart K, Schmitz N, Aulitzky WE, Krämer A, et al. Allogeneic hematopoietic cell transplantation in intermediate risk acute myeloid leukemia negative for FLT3-ITD, NPM1- or biallelic CEBPA mutations. Ann Oncol. 2017;28:2793–98.
Baron F, Stevens-Kroef M, Kicinski M, Meloni G, Muus P, Marie JP, et al. Impact of induction regimen and allogeneic hematopoietic cell transplantation on outcome in younger adults with acute myeloid leukemia with a monosomal karyotype. Haematologica. 2019;104:1168–75.
Terwijn M, van Putten WL, Kelder A, van der Velden VH, Brooimans RA, Pabst T, et al. High prognostic impact of flow cytometric minimal residual disease detection in acute myeloid leukemia: data from the HOVON/SAKK AML 42A study. J Clin Oncol. 2013;31:3889–97.
Freeman SD, Virgo P, Couzens S, Grimwade D, Russell N, Hills RK, et al. Prognostic relevance of treatment response measured by flow cytometric residual disease detection in older patients with acute myeloid leukemia. J Clin Oncol. 2013;31:4123–31.
Hubmann M, Köhnke T, Hoster E, Schneider S, Dufour A, Zellmeier E, et al. Molecular response assessment by quantitative real-time polymerase chain reaction after induction therapy in NPM1-mutated patients identifies those at high risk of relapse. Haematologica. 2014;99:1317–25.
Klco JM, Miller CA, Griffith M, Petti A, Spencer DH, Ketkar-Kulkarni S, et al. Association between mutation clearance after induction therapy and outcomes in acute myeloid leukemia. JAMA 2015;314:811–22.
Ivey A, Hills RK, Simpson MA, Jovanovic JV, Gilkes A, Grech A, et al. Assessment of minimal residual disease in standard-risk AML. N Engl J Med. 2016;374:422–33.
Balsat M, Renneville A, Thomas X, de Botton S, Caillot D, Marceau A, et al. Postinduction minimal residual disease predicts outcome and benefit from allogeneic stem cell transplantation in acute myeloid leukemia with NPM1 mutation: a study by the Acute Leukemia French Association Group. J Clin Oncol. 2017;35:185–93.
Freeman SD, Hills RK, Virgo P, Khan N, Couzens S, Dillon R, et al. Measurable residual disease at induction redefines partial response in acute myeloid leukemia and stratifies outcomes in patients at standard risk without NPM1 mutations. J Clin Oncol. 2018;36:1486–97.
Jongen-Lavrencic M, Grob T, Hanekamp D, Kavelaars FG, Al Hinai A, Zeilemaker A, et al. Molecular minimal residual disease in acute myeloid leukemia. N Engl J Med. 2018;378:1189–99.
Morita K, Kantarjian HM, Wang F, Yan Y, Bueso-Ramos C, Sasaki K, et al. Clearance of somatic mutations at remission and the risk of relapse in acute myeloid leukemia. J Clin Oncol. 2018;36:1788–97.
Venditti A, Piciocchi A, Candoni A, Melillo L, Calafiore V, Cairoli R, et al. GIMEMA AML1310 trial of risk-adapted, MRD-directed therapy for young adults with newly diagnosed acute myeloid leukemia. Blood. 2019;134:935–45.
Short NJ, Ravandi F. How close are we to incorporating measurable residual disease into clinical practice for acute myeloid leukemia? Haematologica. 2019;104:1532–41.
Bezerra MF, Lima AS, Piqué-Borràs MR, Silveira DR, Coelho-Silva JL, Pereira-Martins DA, et al. Co-occurrence of DNMT3A, NPM1, FLT3 mutations identifies a subset of acute myeloid leukemia with adverse prognosis. Blood. 2020;135:870–75.
Kantarjian HM, Thomas XG, Dmoszynska A, Wierzbowska A, Mazur G, Mayer J, et al. Multicenter, randomized, open-label, phase III trial of decitabine versus patient choice, with physician advice, of either supportive care or low-dose cytarabine for the treatment of older patients with newly diagnosed acute myeloid leukemia. J Clin Oncol. 2012;30:2670–7.
Dombret H, Seymour JF, Butrym A, Wierzbowska A, Selleslag D, Jang JH, et al. International phase 3 study of azacitidine vs conventional care regimens in older patients with newly diagnosed AML with >30% blasts. Blood. 2015;126:291–9.
DiNardo CD, Jonas BA, Pullarkat V, Thirman MJ, Garcia JS, Wei AH, et al. Azacitidine and venetoclax in previously untreated acute myeloid leukemia. N Engl J Med. 2020;383:617–29.
Wei AH, Montesinos P, Ivanov V, DiNardo CD, Novak J, Laribi K, et al. Venetoclax plus LDAC for newly diagnosed AML ineligible for intensive chemotherapy: a phase 3 randomized placebo-controlled trial. Blood 2020;135:2137–45.
Stone RM, Mandrekar SJ, Sanford BL, Laumann K, Geyer S, Bloomfield CD, et al. Midostaurin plus chemotherapy for acute myeloid leukemia with a FLT3 mutation. N Engl J Med. 2017.
Stein EM, DiNardo CD, Fathi AT, Mims AS, Pratz KW, Savona MR, et al. Ivosidenib or enasidenib combined with intensive chemotherapy in patients with newly diagnosed AML: a phase 1 study. Blood. 2020.
Fenwarth L, Thomas X, de Botton S, Duployez N, Bourhis JH, Lesieur A, et al. A personalized approach to guide allogeneic stem cell transplantation in younger adults with acute myeloid leukemia. Blood. 2020.
Acknowledgements
This work was supported in part by a grant from the Aichi Cancer Research Foundation, grant number: 2020-1-11.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yanada, M. The evolving concept of indications for allogeneic hematopoietic cell transplantation during first complete remission of acute myeloid leukemia. Bone Marrow Transplant 56, 1257–1265 (2021). https://doi.org/10.1038/s41409-021-01247-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-021-01247-4
- Springer Nature Limited
This article is cited by
-
The effect of center experience on allogeneic hematopoietic cell transplantation outcomes in acute myeloid leukemia
Bone Marrow Transplantation (2024)
-
Allogeneic hematopoietic cell transplantation from alternative donors in acute myeloid leukemia
Annals of Hematology (2024)
-
External validation and extended application of the transplant conditioning intensity score in acute myeloid leukemia
Bone Marrow Transplantation (2023)
-
Efficacy and safety of allogeneic hematopoietic cell transplantation in acute myeloid leukemia patients aged > 65 years with unfavorable cytogenetics
Annals of Hematology (2023)
-
Age and allogeneic hematopoietic cell transplantation outcomes in acute myeloid leukemia
International Journal of Hematology (2023)