Abstract
Bevacizumab (Avastin™, Genentech) is a monoclonal antibody that deactivates the vascular endothelial growth factor leading to disruption of vital cancer signaling pathways and inhibition of angiogenesis which results in its anti-tumor activity. The use of bevacizumab in treating cancers has steadily increased since it was initially approved by the Food and Drug Administration for metastatic colorectal cancer. Clinical trials have revealed that bevacizumab has serious side effects, including spontaneous bowel perforation, which can occur in patients who have no involvement of the gastrointestinal tract by cancer. Although risk factors for bevacizumab-associated bowel perforation have been identified, it is still unclear which patients are specifically at risk for this complication. The management of bevacizumab-induced bowel perforation depends on the clinical presentation and the goals of care set by the treating physicians and the patient.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
One of the more significant complications from bevacizumab is spontaneous bowel perforation, which may lead to peritonitis requiring emergency operative intervention, fistula formation, or intra-abdominal abscess. These consequences associated with bowel perforation can prohibit further chemotherapy and result in significant morbidity and mortality in cancer patients. It appears that all patients receiving bevacizumab are at risk for this complication, irrespective of tumor type [1–6••].
Herein, we review the literature that pertains to bevacizumab-induced bowel perforation. This subject will be explored with a focus on the incidence and risks associated with administering bevacizumab in patients with metastatic disease. Additionally, the various aspects of this complication management are addressed. The incidence of bowel perforation in selected clinical trials where bevacizumab was utilized is summarized in Table 1.
Metastatic Colorectal Cancers
Bevacizumab combined with 5-FU based chemotherapy regimens is FDA approved and widely used in the treatment of metastatic colorectal cancer (mCRC). The use of bevacizumab in this setting stems from randomized clinical trials that have shown survival benefit from adding bevacizumab to cytotoxic chemotherapies [7–10]. Promising results were also reported when adding bevacizumab to neoadjuvant chemotherapy regimens for locally advanced rectal cancer [11, 12]. Despite these benefits in patients with mCRC, it is now well established that bevacizumab increases the risk of serious complications, such as bowel perforation. It is noteworthy to mention that bevacizumab-induced bowel perforation was described to occur indiscriminately along the GI tract and not only in the primary tumor site [13].
The incidence of bowel perforation in patients with mCRC attributed to the use of bevacizumab ranges from 1 to 4 % [7, 13–15]. Hurwitz et al., in a phase III trial of mCRC where patients were randomized to irinotecan, bolus 5-FU and leucovorin with or without bevacizumab, reported a bowel perforation incidence of 1.5 % in the bevacizumab group vs. 0 % in the control group [7]. Hochster et al., in the TREE-2 trial reported an incidence rate of bowel perforation in the range of 2 % [14]. A meta-analysis by Hapani et al., which included six randomized clinical trials in mCRC, showed that the incidence of bowel perforation from bevacizumab was 0.9 % (95 % CI 0.6–1.3) [16••].
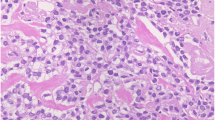
Several clinical risk factors were postulated to increase the risk of spontaneous bowel perforation from bevacizumab in the setting of treating mCRC. These include a history of peptic ulcer disease, diverticulitis, colitis, intestinal obstruction, tumor necrosis, recent sigmoidoscopy or colonoscopy, intact primary tumor, radiotherapy, higher cumulative dose of bevacizumab, or emergent surgery while receiving bevacizumab [16••, 17–19]. Various mechanisms are thought to mediate bevacizumab induced bowel perforation including disruption of vascular regeneration and resultant bowel ischemia, enhanced chemotherapy delivery to the tumor leading to necrosis, or impaired wound healing [16••, 20–22]. In spite of the accumulating knowledge of predisposing factors and proposed mechanisms of bevacizumab-induced bowel perforation, there is still no reliable method to accurately predict the occurrence of this complication in mCRC patients. Such a prediction model will be further complicated by the heterogeneity of mCRC patients in terms of the predisposing condition for colorectal cancer, the various chemotherapy regimens combined with bevacizumab, various bevacizumab doses and schedules, location and extent of the tumor, administration of bevacizumab with the primary tumor in situ or removed and patients’ comorbidities.
Ovarian Cancer
Bevacizumab has shown significant anti-tumor activity in epithelial ovarian cancer [1, 23–27]. As a single agent, Monk et al. reported in a case report on a heavily pretreated, recurrent and refractory serous ovarian carcinoma patient who experienced a durable response to bevacizumab [24]. Subsequently, phase II trials have shown a response rate of around 20 % prompting phase III trials to test bevacizumab in combination with platinum-based chemotherapy regimens as first line therapy in patients with advanced stage epithelial ovarian cancer [1, 25, 26]. Two recently reported large phase III trials met their primary end points of improving progression free survival with the addition of bevacizumab to carboplatin and paclitaxel in the adjuvant treatment of advanced stage epithelial ovarian cancer. In these trials, the addition of bevacizumab improved progression free survival by 2–4 months, but also appeared to be associated with a higher GI complication rate when compared to conventional therapy [23, 27].
In addition to extending progression free survival, the use of bevacizumab in treating patients with ovarian cancer leads to better control of cancer associated symptoms. This includes reducing ascites and pain, along with improving gastrointestinal and respiratory symptoms precipitated by advanced ovarian cancer which are often debilitating [1, 25, 26]. In preclinical studies, the level of VEGF expression by ovarian cancer cells was directly associated with ascites formation, which was averted by applying a VGEF inhibitor [28, 29]. Various clinical reports suggested that bevacizumab, whether administered IV or IP, might be effective in managing malignant ascites for palliative reasons [30].
As noticed in mCRC, bowel perforation is associated with the use of bevacizumab in epithelial ovarian cancers, however the incidence seems to be higher (3–11 %) [1, 31]. In October 2005, the National Cancer Institute (NCI) issued an action letter warning clinicians of the risk of GI perforation from bevacizumab in response to a phase II trial which reported 5 (11.4 %) GI perforations, one of them fatal, in 44 ovarian cancer patients [1]. Another phase II study of bevacizumab and erlotinib reported two cases of fatal GI perforations [32]. A recent larger phase III trial reported 10 (1 %) GI perforations in patients receiving bevacizumab compared with 3 (<1 %) in the standard chemotherapy arm [23]. Another similar phase III trial comparing cytotoxic chemotherapy with or without bevacizumab showed that the incidence of GI perforation was higher in patients treated with bevacizumab (3 vs 1.2 %), but the difference was not statistically different [27]. As noted, the more recent phase III trials appear to demonstrate a lower incidence of bowel perforation than what was observed in the earlier phase II trials, which may be due to more stringent patient selection.
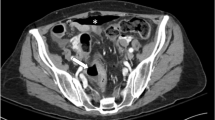
Certain ovarian cancer characteristics and management features may increase the risk of bevacizumab-associated bowel perforation. Diffuse peritoneal disease, a common finding in ovarian cancer, potentially increases the risk of bowel perforation [31]. Extensive peritoneal involvement may necessitate more aggressive surgical cytoreduction which in turn may increase the risk of bowel perforation. Bowel obstruction also seems to increase the risk of perforation, and was actually associated with two deaths from bowel perforation reported by Nimeiri et al. [32]. In the phase II ORBIT trial of bevacizumab monotherapy for platinum-resistant ovarian cancer, all five patients who had bowel perforation had signs of radiographic bowel involvement such as tumor involving the bowel, small bowel obstruction, bowel distension or bowel wall thickening [1]. It is unclear if administering IV bevacizumab in chemotherapy combinations that include intraperitoneal (IP) administration of other drugs increases the risk of bowel perforation. A phase II trial where IV bevacizumab was added to IP cisplatin and paclitaxel resulted in one fatal bowel perforation following rectosigmoid anastomotic dehiscence [33]. Interestingly, the bowel dehiscence occurred during the fourth treatment cycle, was limited to the anastomotic site, was distant from the IP catheter and was not associated with gross tumor involvement of the bowel [33].
In the authors opinion, in order to decrease the morbidity associated with bevacizumab administered to patients with ovarian cancer, implants along the GI tract noticed during surgical intervention or by imaging should warrant close monitoring and a heightened clinical suspicion for GI perforation in patients with previous bowel resection and anastomosis. Although GI involvement by cancer is not an absolute contraindication to use bevacizumab, Simpkins et al. showed that excluding patients with clinical or radiographic evidence of bowel obstruction, rectosigmoid involvement by cancer or refractory heavily pretreated disease resulted in no bevacizumab-associated bowel perforations in 25 ovarian cancer patients treated with bevacizumab [34].
Breast Cancer
Bevacizumab was first approved for the treatment of metastatic breast cancer in 2008 following the results of the E2100 open label phase III trial that showed progression-free survival benefit when bevacizumab was combined with paclitaxel, compared to paclitaxel alone (11.3 vs 5.8 months, respectively) [3]. Subsequently, the AVADO, RIBBON-1 and RIBBON-2 phase III clinical trials showed similar results in regards to significant progression-free survival in favor of bevacizumab. However, no overall survival benefit was demonstrated which incited the FDA to withdraw bevacizumab approval for the treatment of metastatic breast cancer [35–38].
The incidence of bevacizumab induced bowel perforation in breast cancer is thought to be less than 1 %. In fact, in a meta-analysis by Ranpura et al., the rate of serious adverse events from bevacizumab in breast cancer patients was the lowest among the other cancers included in that study (RR, 0.69; 95 % CI 0.30–1.62; incidence, 0.9 % vs 1.3 %) [6••]. Although this low rate of bowel perforation is not very surprising given that involvement of the GI tract by breast cancer is less common than in mCRC and ovarian cancer, it is noteworthy to mention that most of the metastatic breast cancer trials excluded patients with intra-abdominal abscesses, history of bowel perforation or recent abdominal fistulas. The four major phase III metastatic breast cancer trials discussed above showed that the incidence rate of bevacizumab associated bowel perforation is <1 %. In the AVADO and ATHENA trials where bevacizumab was discontinued 6 weeks before minor or major elective surgeries, or started 28–60 days (or following complete healing) after surgery, there was no increased risk of bowel perforation [36, 39, 40].
Non-Small Cell Lung Cancer
Bevacizumab is approved as a first line treatment in a combination regimen with carboplatin and paclitaxel for advanced stage non-squamous non-small cell lung cancer (NSCLC) [22]. This approval followed the results of the phase III trial (ECOG 4599) which showed an overall survival improvement of 2 months for the patients on the bevacizumab arm compared to carboplatin and paclitaxel alone (12.3 vs 10.3 months, HR for death, 0.79; P = 0.003) [2]. In the subsequent AVAiL trial in which advanced stage NSCLC patients were randomized to cisplatin and gemcitabine with or without bevacizumab, there was an improvement in progression-free survival that did not translate into overall survival benefit [41, 42].
Bevacizumab use in NSCLC led to bowel perforation, but also resulted in other unique toxicities that were rare in other cancers [2, 43–45]. The incidence rate of bevacizumab-associated bowel perforation in clinical trials is <1 % [41, 46]. Outside of clinical trials, two case reports described bowel perforation in NSCLC patients treated with bevacizumab. In one case there was full thickness involvement of the bowel by NSCLC whereas in the other case the patient experienced a colon perforation that was not involved by tumor [44, 45]. Spigel et al. reported on cases of tracheoesophageal fistulas in small cell and NSCLC patients treated with bevacizumab in clinical trials [47]. This complication seems to be unique to the use of bevacizumab in NSCLC patients. Aside from bowel perforation, bevacizumab has also been shown to be associated with severe pulmonary hemorrhage in NSCLC. In the randomized phase II trial of carboplatin and paclitaxel with or without bevacizumab, 6 of 67 patients experienced grade III/IV hemoptysis/pulmonary hemorrhage which resulted in three deaths attributed to this complication. In a subgroup analysis, some of the characteristics that were associated in pulmonary hemorrhage included squamous cell histology, proximity of the tumor to major blood vessels, tumor necrosis, or cavitary lesions [43]. This effectively led to excluding patients with squamous cell histology from subsequent NSCLC clinical trials, and a black box warning of pulmonary hemorrhage/hemoptysis in the bevacizumab prescribing information [48].
Malignant Glioma
Bevacizumab was associated with encouraging response rates in high grade gliomas [49]. So far, the available data from phase II trials support the use of bevacizumab as a single agent or in combination with irinotecan for recurrent/progressive glioblastoma multiforme (GBM). Phase III trials assessing survival benefit from integrating bevacizumab in the treatment of GBM are ongoing [49–54].
The use of bevacizumab in the treatment of GBM has been described to result in bowel perforation in addition to other complications that are more specific to the CNS [49, 53]. In a trial comparing bevacizumab with an irinotecan combination in patients with malignant gliomas, there were two treatment-related deaths, one of which was attributed to bowel perforation [50]. In another single arm phase II trial testing bevacizumab combined with irinotecan and carboplatin in 40 bevacizumab-naïve recurrent GBM patients, there were three cases of bowel perforation, one of which was fatal [55]. Friedman et al., in a phase II trial assigning patients to bevacizumab alone or bevacizumab and irinotecan, found 2 of 79 (3 %) patients in the combined arm had bowel perforations. No bowel perforation ensued in the single agent bevacizumab arm [53]. In a study combining bevacizumab with brain radiation for recurrent GBM, 1 of 25 (4 %) patients developed bowel perforation. Interestingly, this patient had the perforation while on chronic dexamethasone, which probably identifies another potential risk factor for bowel perforation in this patient population where high dose steroids are commonly used [56]. Notably, the GI perforations that occurred when bevacizumab was administered in GBM patients ensued when the drug was given in combination regimens.
Renal Cell Carcinoma
Bevacizumab is approved for the treatment of metastatic renal cell carcinoma (RCC) in conjunction with interferon alpha [48]. Randomized phase III trials in stage IV RCC have shown a significant prolongation of progression-free survival, but not overall survival, when bevacizumab was added to interferon [57–59]. The inability to demonstrate significant overall survival benefit could be due to the subsequent treatment of the bevacizumab trial patients with tyrosine kinase and mammalian target of rapamycin (mTOR) inhibitors which are now known to be effective in metastatic RCC [60–62].
Two key randomized phase III trials in metastatic RCC showed an incidence rate of 0.02–1 % of bevacizumab-associated bowel perforation [58, 59]. In the AVOREN phase III trial, 5 of 337 (1 %) patients treated with bevacizumab and interferon alpha experienced bowel perforation [58]. One of the patients had a gastric perforation leading to a grade V toxic event. There is an additional case report of a stage IV RCC patient who died after experiencing a gastric perforation and resultant gastropleural fistula which was attributed to the use of bevacizumab [63]. CALGB 90206 is a phase III randomized trial of bevacizumab with or without interferon alpha for patients with stage IV RCC. In this study, there were two bowel perforations (n = 366, 1 %) reported [59].
No definite risk factors have been associated with bevacizumab-induced bowel perforation in metastatic RCC. Notably, all patients in the AVOREN trial and more than 85 % of the patients in CALGB 90206 underwent nephrectomy before enrollment and all patients were treated with interferon alpha [58, 59]. Although it is unclear if cytokine administration increases the risk of perforation from bevacizumab, IL-2 in previous studies was associated with an increased risk of bowel perforation [64, 65].
Management of Bowel Perforation from Bevacizumab
As mentioned above, patients undergoing treatment with bevacizumab and other cytotoxic chemotherapies represent a group of patients at high risk for severe sequelae from bowel perforation. Not only are patients being treated with bevacizumab, which increases their risk for wound healing and hemostasis complications, but they are also potentially immunocompromised from chemotherapy. Therefore the management of bowel perforation in these patients is complex and should involve a multidisciplinary approach that involves medical oncologists, surgeons, and interventional radiologists.
Perforation may be asymptomatic in immunocompromised patients and difficult to diagnose. Patients can present with an acute abdomen due to peritoneal contamination, free air in the abdomen, hemoperitoneum, or intra-abdominal abscess. Postoperative patients or those being treated for rectal cancer can also present with fistula formation or anastomotic leak [17, 66].
The management of bowel perforation depends on the timing of presentation, the overall condition of the patient and the patients’ goals and wishes. Medical management will often fail in patients with bowel perforation, unless they have a contained perforation leading to abscess which can be potentially managed with percutaneous drainage. More likely, patients will require operative intervention and may require bowel resection and potentially diversion. Special circumstances in this population clearly exist, including patients with incurable cancer or poor performance status.
In a retrospective study, Badgwell et al. reported a series of 24 patients who experienced a bowel perforation within 7 weeks of receiving bevacizumab. The patients had tumors in multiple sites including pancreas (n = 7, 29 %), colorectal (n = 6, 25 %), renal cell (n = 4, 17 %), and ovarian cancer (n = 3, 13 %). This was a highly heterogeneous group of patients presenting with different types of complications including two patients with perforated diverticulitis and two with perforated appendicitis. Thirty-day mortality was 12.5 % (3/24 patients). Four patients (19 %) went immediately for operative intervention. Of the 20 patients initially selected for non-operative management, only one patient eventually required an operation. The 19 remaining patients were successfully managed non-operatively with treatments such as antibiotics, bowel rest, placement of a nasogastric tube, total parenteral nutrition, and in 7 patients interventional radiology placed percutaneous catheters [19]. Clearly these patients are well-selected and each patient presenting with this potentially lethal complication should be individually assessed as a candidates for conservative management.
The long half-life of bevacizumab, which ranges from 11 to 50 days [48], increases the risk of unplanned, urgent surgical procedures. There are strict recommendations regarding the timing of surgery for patients being treated with bevacizumab. Per the bevacizumab prescribing information insert, patients should not undergo surgery for at least 28 days following their last treatment due to the risk for poor wound healing and hemostasis [48]. Operations should ideally be delayed at least 4–6 weeks to assure complete metabolism of the drug. Earlier interventions, if necessary, may increase the risk of bevacizumab-associated complications. The addition of bevacizumab to chemotherapy 28–60 days after surgery did not seem to increase the risk of perforation in one study [22]. These recommendations are generally followed for elective surgery and are believed to decrease the risk of bevacizumab induced perforation, delayed wound healing, anastomotic dehiscence and other complications.
The risk of bevacizumab-related postoperative complications is higher when urgent surgical interventions are needed. In patients with near-obstructed bowel but minimally symptomatic tumors, the benefit of adding bevacizumab should be weighed against the potential need for surgical intervention during the early course of therapy. Scappaticci et al. showed that cancer patients who undergo emergency surgery while on bevacizumab are at higher risk for wound healing complications such as fascial dehiscence, cellulitis, intra-abdominal and cutaneous fistulae, anastomotic leak, intra-abdominal bleeding, hemothorax and bowel perforation [22].
Although the literature to date on how to manage bevacizumab-induced bowel perforation is largely dependent on case series, it should be noted that it will be hard to generate a common approach for this patient population because of the large heterogeneity of the underlying malignancy, treatment goals, and clinical presentation.
Conclusion
Bowel perforation is a serious complication of bevacizumab therapy that is seen across various cancers. The risk of this complication is higher in cancers that involve the GI tract, especially mCRC and epithelial ovarian cancer. However, perforation can also occur without GI involvement by tumor as demonstrated in malignant glioma. As outlined above, there are several pre-existing medical conditions and cancer-related treatments that may increase the risk of bevacizumab-induced bowel perforation. There is no well-established scoring system to predict which patients are at risk for bowel perforation in the setting of bevacizumab use; however, careful patient selection may help reduce the incidence of complications from this drug. For instance, if possible, bevacizumab use should be avoided in patients who may require early surgical intervention. Early recognition of bowel perforation is also of paramount importance.
Since multiple clinical trials have shown that the addition of bevacizumab to standard chemotherapy improves survival in metastatic cancer, the risk to benefit ratio of bevacizumab use should be communicated clearly with the patient. The patient should be also made aware of the risk of bowel perforation and be educated about the presenting symptoms of such a complication. The management of this complication should be individualized for each patient as well as the clinical presentation and the patient’s wishes and goals. Bevacizumab should be discontinued permanently if bowel perforation occurs. Future studies should focus on producing better predictive tools to identify the patients at higher risk for bevacizumab-induced bowel perforation.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Cannistra SA, Matulonis UA, Penson RT, et al. Phase II study of bevacizumab in patients with platinum-resistant ovarian cancer or peritoneal serous cancer. J Clin Oncol. 2007;25(33):5180–6.
Sandler A, Gray R, Perry MC, et al. Paclitaxel–carboplatin alone or with bevacizumab for non–small-cell lung cancer. N Engl J Med. 2006;355(24):2542–50.
Miller K, Wang M, Gralow J, et al. Paclitaxel plus bevacizumab versus paclitaxel alone for metastatic breast cancer. N Engl J Med. 2007;357(26):2666–76.
Rini BI, Halabi S, Rosenberg JE, et al. Bevacizumab plus interferon alfa compared with interferon alfa monotherapy in patients with metastatic renal cell carcinoma: CALGB 90206. J Clin Oncol. 2008;26(33):5422–8.
Van Cutsem E, Vervenne WL, Bennouna J, et al. Phase III trial of bevacizumab in combination with gemcitabine and erlotinib in patients with metastatic pancreatic cancer. J Clin Oncol. 2009;27(13):2231–7.
•• Ranpura V, Hapani S, Wu S. Treatment-related mortality with bevacizumab in cancer patients. JAMA. 2011;305(5):487–494. Ranpura and colleagues completed an excellent systematic review and meta-analysis and concluded that adding bevacizumab to chemotherapy increases the risk of treatment related mortality. This paper gives an insight into the type and incidence of bevacizumab induced serious adverse events in various cancers.
Hurwitz H, Fehrenbacher L, Novotny W, et al. Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med. 2004;350(23):2335–42.
Giantonio BJ, Catalano PJ, Meropol NJ, et al. Bevacizumab in combination with oxaliplatin, fluorouracil, and leucovorin (FOLFOX4) for previously treated metastatic colorectal cancer: results from the Eastern Cooperative Oncology Group Study E3200. J Clin Oncol. 2007;25(12):1539–44.
Kabbinavar F, Hurwitz HI, Fehrenbacher L, et al. Phase II, randomized trial comparing bevacizumab plus fluorouracil (FU)/leucovorin (LV) with FU/LV alone in patients with metastatic colorectal cancer. J Clin Oncol. 2003;21(1):60–5.
Saltz LB, Clarke S, Diaz-Rubio E, et al. Bevacizumab in combination with oxaliplatin-based chemotherapy as first-line therapy in metastatic colorectal cancer: a randomized phase III study. J Clin Oncol. 2008;26(12):2013–9.
Nogué M, Salud A, Vicente P, et al. Addition of bevacizumab to XELOX induction therapy plus concomitant capecitabine-based chemoradiotherapy in magnetic resonance imaging–defined poor-prognosis locally advanced rectal cancer: the AVACROSS study. Oncologist. 2011;16(5):614–20.
Velenik V, Ocvirk J, Music M, et al. Neoadjuvant capecitabine, radiotherapy, and bevacizumab (CRAB) in locally advanced rectal cancer: results of an open-label phase II study. Radiat Oncol. 2011;6(1):105.
Van Cutsem E, Rivera F, Berry S, et al. Safety and efficacy of first-line bevacizumab with FOLFOX, XELOX, FOLFIRI and fluoropyrimidines in metastatic colorectal cancer: the BEAT study. Ann Oncol. 2009;20(11):1842–7.
Hochster HS, Hart LL, Ramanathan RK, et al. Safety and efficacy of oxaliplatin and fluoropyrimidine regimens with or without bevacizumab as first-line treatment of metastatic colorectal cancer: results of the TREE Study. J Clin Oncol. 2008;26(21):3523–9.
Kabbinavar FF, Schulz J, McCleod M, et al. Addition of bevacizumab to bolus fluorouracil and leucovorin in first-line metastatic colorectal cancer: results of a randomized phase II trial. J Clin Oncol. 2005;23(16):3697–705.
•• Hapani S, Chu D, Wu S. Risk of gastrointestinal perforation in patients with cancer treated with bevacizumab: a meta-analysis. Lancet oncol. 2009;10(6):559–568. The meta-analysis by Hapani and colleagues studies in depth the gastrointestinal perforation as a complication from bevacizumab treatment. This meta-analysis provides very useful information when counseling patients about gastrointestinal perforation as an adverse effect of bevacizumab. It also gives a perspective to the treating physicians on the incidence of bowel perforation from bevacizumab use in various cancers.
Saif MW, Elfiky A, Salem RR. Gastrointestinal perforation due to bevacizumab in colorectal cancer. Ann Surg Oncol. 2007;14(6):1860–9.
Lordick F, Geinitz H, Theisen J, Sendler A, Sarbia M. Increased risk of ischemic bowel complications during treatment with bevacizumab after pelvic irradiation: report of three cases. Int J Radiat Oncol Biol Phys. 2006;64(5):1295–8.
Badgwell B, Camp E, Feig B, et al. Management of bevacizumab-associated bowel perforation: a case series and review of the literature. Ann Oncol. 2008;19(3):577–82.
Sugrue M, Kozloff M, Hainsworth J, et al. Risk factors for gastrointestinal perforations in patients with metastatic colorectal cancer receiving bevacizumab plus chemotherapy. J Clin Oncol. 2006;24(18 suppl):3535.
Abbrederis K, Kremer M, Schuhmacher C. Ischemic anastomotic bowel perforation during treatment with bevacizumab 10 months after surgery. Chirurg. 2008;79(4):351–5.
Scappaticci FA, Fehrenbacher L, Cartwright T, et al. Surgical wound healing complications in metastatic colorectal cancer patients treated with bevacizumab. J Surg Oncol. 2005;91(3):173–80.
Perren TJ, Swart AM, Pfisterer J, et al. A phase 3 trial of bevacizumab in ovarian cancer. N Engl J Med. 2011;365(26):2484–96.
Monk BJ, Choi DC, Pugmire G, Burger RA. Activity of bevacizumab (rhuMAB VEGF) in advanced refractory epithelial ovarian cancer. Gynecol Oncol. 2005;96(3):902–5.
Garcia AA, Hirte H, Fleming G, et al. Phase II clinical trial of bevacizumab and low-dose metronomic oral cyclophosphamide in recurrent ovarian cancer: a trial of the California, Chicago, and Princess Margaret Hospital phase II consortia. J Clin Oncol. 2008;26(1):76–82.
Burger RA, Sill MW, Monk BJ, Greer BE, Sorosky JI. Phase II trial of bevacizumab in persistent or recurrent epithelial ovarian cancer or primary peritoneal cancer: a Gynecologic Oncology Group Study. J Clin Oncol. 2007;25(33):5165–71.
Burger RA, Brady MF, Bookman MA, et al. Incorporation of bevacizumab in the primary treatment of ovarian cancer. N Engl J Med. 2011;365(26):2473–83.
Byrne AT, Ross L, Holash J, et al. Vascular endothelial growth factor-trap decreases tumor burden, inhibits ascites, and causes dramatic vascular remodeling in an ovarian cancer model. Clin Cancer Res. 2003;9(15):5721–8.
Yoneda J, Kuniyasu H, Price JE, Bucana CD, Fidler IJ, Crispens MA. Expression of angiogenesis-related genes and progression of human ovarian carcinomas in nude mice. J Natl Cancer Inst. 1998;90(6):447–54.
Kobold S, Hegewisch-Becker S, Oechsle K, Jordan K, Bokemeyer C, Atanackovic D. Intraperitoneal VEGF inhibition using bevacizumab: a potential approach for the symptomatic treatment of malignant ascites? Oncologist. 2009;14(12):1242–51.
Han ES, Monk BJ. What is the risk of bowel perforation associated with bevacizumab therapy in ovarian cancer? Gynecol Oncol. 2007;105(1):3–6.
Nimeiri HS, Oza AM, Morgan RJ, et al. Efficacy and safety of bevacizumab plus erlotinib for patients with recurrent ovarian, primary peritoneal, and fallopian tube cancer: a trial of the Chicago, PMH, and California Phase II Consortia. Gynecol Oncol. 2008;110(1):49–55.
Konner JA, Grabon DM, Gerst SR, et al. Phase II study of intraperitoneal paclitaxel plus cisplatin and intravenous paclitaxel plus bevacizumab as adjuvant treatment of optimal stage II/III epithelial ovarian cancer. J Clin Oncol. 2011;29(35):4662–8.
Simpkins F, Belinson JL, Rose PG. Avoiding bevacizumab related gastrointestinal toxicity for recurrent ovarian cancer by careful patient screening. Gynecol Oncol. 2007;107(1):118–23.
Brufsky AM, Hurvitz S, Perez E, et al. RIBBON-2: a randomized, double-blind, placebo-controlled, phase III trial evaluating the efficacy and safety of bevacizumab in combination with chemotherapy for second-line treatment of human epidermal growth factor receptor 2-negative metastatic breast cancer. J Clin Oncol. 2011;29(32):4286–93.
Miles DW, Chan A, Dirix LY, et al. Phase III study of bevacizumab plus docetaxel compared with placebo plus docetaxel for the first-line treatment of human epidermal growth factor receptor 2–negative metastatic breast cancer. J Clin Oncol. 2010;28(20):3239–47.
Robert NJ, Diéras V, Glaspy J, et al. RIBBON-1: Randomized, double-blind, placebo-controlled, phase III trial of chemotherapy with or without bevacizumab for first-line treatment of human epidermal growth factor receptor 2–negative, locally recurrent or metastatic breast cancer. J Clin Oncol. 2011;29(10):1252–60.
U.S. Food and Drug Administration. FDA Commissioner Removes Breast Cancer Indication from Avastin Label. 2011.http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm279485.htm. Accessed 16 April 2012.
Smith I, Pierga JY, Biganzoli L, et al. First-line bevacizumab plus taxane-based chemotherapy for locally recurrent or metastatic breast cancer: safety and efficacy in an open-label study in 2251 patients. Ann Oncol. 2011;22(3):595–602.
Cortés J, Caralt M, Delaloge S, et al. Safety of bevacizumab in metastatic breast cancer patients undergoing surgery. Eur J Cancer. 2012;48(4):475–81.
Reck M, von Pawel J, Zatloukal P, et al. Phase III trial of cisplatin plus gemcitabine with either placebo or bevacizumab as first-line therapy for nonsquamous non–small-cell lung cancer: AVAil. J Clin Oncol. 2009;27(8):1227–34.
Reck M, Von Pawel J, Zatloukal P, et al. Overall survival with cisplatin–gemcitabine and bevacizumab or placebo as first-line therapy for nonsquamous non-small-cell lung cancer: results from a randomised phase III trial (AVAiL). Ann Oncol. 2010;21(9):1804–9.
Johnson DH, Fehrenbacher L, Novotny WF, et al. Randomized phase II trial comparing bevacizumab plus carboplatin and paclitaxel with carboplatin and paclitaxel alone in previously untreated locally advanced or metastatic non-small-cell lung cancer. J Clin Oncol. 2004;22(11):2184–91.
Gray J, Murren J, Sharma A, Kelley S, Detterbeck F, Bepler G. Perforated viscus in a patient with non-small cell lung cancer receiving bevacizumab. J Thorac Oncol. 2007;2(6):571–3.
Schellhaas E, Loddenkemper C, Schmittel A, Buhr HJ, Pohlen U. Bowel perforation in non-small cell lung cancer after bevacizumab therapy. Invest New Drugs. 2009;27(2):184–7.
Herbst RS, O'Neill VJ, Fehrenbacher L, et al. Phase II study of efficacy and safety of bevacizumab in combination with chemotherapy or erlotinib compared with chemotherapy alone for treatment of recurrent or refractory non–small-cell lung cancer. J Clin Oncol. 2007;25(30):4743–50.
Spigel DR, Hainsworth JD, Yardley DA, et al. Tracheoesophageal fistula formation in patients with lung cancer treated with chemoradiation and bevacizumab. J Clin Oncol. 2010;28(1):43–8.
Genentech Inc. Avastin prescribing information. December 2011. Genentech, San Francisco, CA, USA.
Vredenburgh JJ, Desjardins A, Herndon JE, et al. Bevacizumab plus irinotecan in recurrent glioblastoma multiforme. J Clin Oncol. 2007;25(30):4722–9.
Stark-Vance V. Bevacizumab and CPT-11 in the treatment of relapsed malignant glioma. World Federation of Neuro-Oncology Meeting 2005:91.
Bokstein F, Shpigel S, Blumenthal DT. Treatment with bevacizumab and irinotecan for recurrent high–grade glial tumors. Cancer. 2008;112(10):2267–73.
Kreisl TN, Kim L, Moore K, et al. Phase II trial of single-agent bevacizumab followed by bevacizumab plus irinotecan at tumor progression in recurrent glioblastoma. J Clin Oncol. 2009;27(5):740–5.
Friedman HS, Prados MD, Wen PY, et al. Bevacizumab alone and in combination with irinotecan in recurrent glioblastoma. J Clin Oncol. 2009;27(28):4733–40.
Desjardins A, Reardon DA, Herndon II JE, et al. Bevacizumab plus irinotecan in recurrent WHO grade 3 malignant gliomas. Clin Cancer Res. 2008;14(21):7068–73.
Reardon DA, Desjardins A, Peters K, et al. Phase II study of metronomic chemotherapy with bevacizumab for recurrent glioblastoma after progression on bevacizumab therapy. J Neurooncol. 2011;103(2):1–9.
Gutin PH, Iwamoto FM, Beal K, et al. Safety and efficacy of bevacizumab with hypofractionated stereotactic irradiation for recurrent malignant gliomas. Int J Radiat Oncol Biol Phys. 2009;75(1):156–63.
Escudier B, Bellmunt J, Négrier S, et al. Phase III trial of bevacizumab plus interferon alfa-2a in patients with metastatic renal cell carcinoma (AVOREN): final analysis of overall survival. J Clin Oncol. 2010;28(13):2144–50.
Escudier B, Pluzanska A, Koralewski P, et al. Bevacizumab plus interferon alfa-2a for treatment of metastatic renal cell carcinoma: a randomised, double-blind phase III trial. Lancet. 2008;370(9605):2103–11.
Rini BI, Halabi S, Rosenberg JE, et al. Phase III trial of bevacizumab plus interferon alfa versus interferon alfa monotherapy in patients with metastatic renal cell carcinoma: final results of CALGB 90206. J Clin Oncol. 2010;28(13):2137–43.
Motzer RJ, Hutson TE, Tomczak P, et al. Sunitinib versus interferon alfa in metastatic renal-cell carcinoma. N Engl J Med. 2007;356(2):115–24.
Hudes G, Carducci M, Tomczak P, et al. Temsirolimus, interferon alfa, or both for advanced renal-cell carcinoma. N Engl J Med. 2007;356(22):2271–81.
Motzer RJ, Escudier B, Oudard S, et al. Efficacy of everolimus in advanced renal cell carcinoma: a double-blind, randomised, placebo-controlled phase III trial. Lancet. 2008;372(9637):449–56.
Dias OM, Barbosa CCL, Teixeira LR, Vargas FS. Gastropleural fistula from gastric perforation due to renal cell carcinoma after bevacizumab chemotherapy: a case report. Clinics. 2011;66(8):1495–8.
Smith FO, Goff SL, Klapper JA, et al. Risk of bowel perforation in patients receiving interleukin-2 after therapy with anti-CTLA 4 monoclonal antibody. J Immunother. 2007;30(1):130.
Heimann DM, Schwartzentruber DJ. Gastrointestinal perforations associated with interleukin-2 administration. J Immunother. 2004;27(3):254–8.
Ganapathi AM, Westmoreland T, Tyler D, Mantyh CR. Bevacizumab-associated fistula formation in postoperative colorectal cancer patients. J Am Coll Surg. 2012;214(4):582–8.
Yang JC, Haworth L, Sherry RM, et al. A randomized trial of bevacizumab, an anti–vascular endothelial growth factor antibody, for metastatic renal cancer. N Engl J Med. 2003;349(5):427–34.
Disclosure
No potential conflicts of interest relevant to this article were reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Abu-Hejleh, T., Mezhir, J.J., Goodheart, M.J. et al. Incidence and Management of Gastrointestinal Perforation from Bevacizumab in Advanced Cancers. Curr Oncol Rep 14, 277–284 (2012). https://doi.org/10.1007/s11912-012-0238-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11912-012-0238-8