Abstract
Purpose of Review
Preterm birth is the leading cause of death worldwide in children < 5 years of age; however, technology and advances in medical knowledge are increasing the survival of children born even at the fringes of viability. With increased survival comes increased risk of long-term neurologic impairments. This paper aims to review recent findings related to changes in brain development associated with prematurity and its impact on neurodevelopmental disabilities.
Recent Findings
Advanced imaging techniques, longitudinal follow-up of individuals born extremely preterm into adulthood and improved understanding of risk factors associated with neurologic impairment contribute to recent discoveries. Sensory impairments are often associated with later cognitive and social impairments and therefore represent targets for therapy.
Summary
All aspects of neurologic development can be affected by preterm delivery. Future research is needed to further elucidate targets for prenatal and postnatal interventions for neuroprotection and to improve outcomes of prematurity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The healthy in utero environment is the optimal location for brain development prior to 37–40 weeks gestation. The World Health Organization defines preterm birth based on gestational age (GA) with extremely preterm < 28 weeks gestation, very preterm 28–32 weeks, and moderate to late preterm 32–37 weeks gestation. Prematurity is a major global health problem as, worldwide, it is the leading cause of death in children less than 5 years old [1]. In the USA, according to Center for Disease Control statistics, birth prior to 37 weeks GA occurred in nearly 10% of completed pregnancies in 2016 with 2.76% of births < 34 weeks GA [2••]. Mortality in infants born at 22 to 24 weeks GA is 64% and survivors have a 43% chance of neurodevelopment impairment [3]. While technology and medical advances are allowing more children to survive, survivors of prematurity often face a lifetime of neurologic impairment—sometimes subtle and sometimes debilitating [2••]. Below, we review recent investigations into the long-term consequences of prematurity as it relates to neurologic, sensory, cognitive, and behavioral development.
Alterations in Brain Structure Resulting from Prematurity
Establishing in utero norms for the series of events resulting in normal cerebral development is technically challenging as imaging studies are complicated by fetal movement and resolution limitations due to intervening maternal tissues. Because sensory and experiential enrichment and deprivation have permanent effects on pathway maturation, synapse formation, and cellular differentiation [4,5,6], it is reasonable to consider that early extra-uterine experience may interfere with the normal progression of brain maturation.
Gross Differences in Brain Size
Gross measurements of brain development are altered by preterm birth. Neuroanatomically, infants born at < 32 weeks GA have overall reduced brain volume, particularly in the frontotemporal regions and hippocampi [7]. Postnatal factors that are associated with smaller volumes include sepsis, bronchopulmonary dysplasia, intraventricular hemorrhage (IVH), steroid exposure, oxygen therapy, and sedation.
Moderate and late preterm infants also have reduction in overall brain size, corpus callosum, deep gray structures, and cerebellum at term equivalent compared to term born babies. Additionally, moderate to late preterm birth is associated with reduced myelination in the posterior limb of the internal capsule and immature gyral pattern at term equivalent, even in the absence of obvious neurologic injury on magnetic resonance imaging (MRI) [8]. Differences in total brain volume and size of various brain regions persist into adolescence and adulthood and intelligence quotient (IQ) correlates with size of select regions in those born prematurely [9•].
Advanced Imaging—Comparing In Utero and Ex Utero Preterms
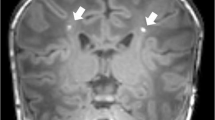
Advanced MRI techniques allow direct comparison of markers of brain maturation and network connectivity between premature infants and fetuses of equivalent GA. Diffusivity of water, as measured by the apparent diffusion coefficient (ADC), decreases as networks form. When imaged at 37 weeks GA, babies born preterm (mean 29 weeks) demonstrate accelerated sensory-motor pathway maturation, as evidenced by decreased ADC values in pons and increased MR spectroscopy (MRS) markers N-acetyl acetate, glutamate/glutamine, and creatinine in the centrum semiovale. Despite more rapid maturation in some areas, areas of injury and/or disturbed development were evident in preterm infants as increased ADC values in parietal white matter and increased markers of cell turnover on MRS [10].
Diffusion tensor imaging (DTI) tractography can also be applied to measure pathway maturation reflected by increasing fractional anisotropy. Preterm infants were found to be slower to mature compared to term babies in the body of the corpus callosum, the left inferior longitudinal fasciculus, and left dorsal visual stream (connecting occipital and temporal visual cortices) [11]. It was suggested that these areas eventually “catch up” in otherwise normal preterm children but not in children with persistent deficits such as cerebral palsy (CP) or visual impairment. Determining the cause of such region specific injury is a topic for future research.
While we are limited by technology to provide direct measurements of subtle differences in brain maturation and injury related to early extra-uterine exposure, the effects can be measured by sensory and neuropsychological delays and impairments that can last throughout life.
Neurosensory Impairment Resulting from Prematurity
Vision
Retinopathy of prematurity (ROP) is a traditionally identified risk factor for visual impairment in preterm infants and is monitored closely in neonatal intensive care units (NICU). Additionally, prematurity affects macular development and function [12]. However, cerebral visual system development is vulnerable through the third trimester, past the time of greatest risk for ROP. Biologic maturation of these systems may be influenced by the atypical visual experience that preterm birth affords. Visual function involves the ventral stream (the “what” of visual experience involving recognition which connects primary visual cortex with inferior temporal cortex) and the dorsal stream (the “how” of visual experience involving visual motor control, spatial attention, motion perception which connects primary visual cortex to posterior parietal cortex). The dorsal stream appears to be more vulnerable to prematurity potentially due to the combination of sensitivity to periventricular and white matter injury and premature visual experience [13, 14].
The “how” of visual perception—mediated by the dorsal stream—can be measured by visual motor tasks such as copying and motor coordination. Adults born at < 1500 g demonstrate lower scores in these tasks than adults who were born at term. Scores in the preterm, but not term, individuals correlated with cortical thickness (lateral occipital-temporal-parietal junction, superior temporal gyrus, insula, superior parietal regions), cortical surface area (superior temporal gyrus, insula, medial occipital lobe, posterior ventral temporal lobe), and fractional anisotropy (corpus callosum, inferior frontal-occipital fasciculus, anterior thalamic radiation) in brain regions involved in these tasks; these findings imply that prematurity can result in permanent deficits in these areas and their associated skills [15].
The “what” of visual perception—mediated by the ventral stream—may also be affected by prematurity. Infants born prematurely have abnormal habituation to visual stimuli [16]. The neuroanatomical correlates of this behavior have not been fully investigated. Such visual behavior at term equivalence is a predictor of later cognitive ability, suggesting that visual behavior has a complex relationship to a variety of brain functions [17].
Implication of the above-described brain regions in visual functioning and the previously discussed areas of reduced brain volume in people born prematurely help explain why prematurity alters visual development independent of the presence of ROP.
Auditory Development
Admission to the NICU for > 5 days is a risk factor for hearing loss, regardless of other medical diagnoses [18]. Additional risk factors for hearing loss in the NICU include prolonged oxygen use, gastrointestinal surgery, patent ductus arteriosus ligation, and low socioeconomic index [19]. Up to nearly 7% of infants born at 24 weeks GA eventually require amplification [20]. Essentially, all preterm infants are at risk and in need of follow-up screening even if the initial hearing screen was normal.
Auditory development is closely linked to later language skills and speech acquisition, making it a pillar of cognitive development throughout childhood. Fetal auditory development occurs in a low frequency, dampened acoustic environment with major ear structures in place by 25 weeks gestation. The auditory cortex undergoes a surprisingly early functional organization. By 32 weeks, infants can perceive differences in male vs. female voice and phenomes [21]. Human and animal studies have revealed that altered acoustic experience changes cortical maturation, neurotransmitter expression, and the development of language perception [22]. Premature infants have different patterns of cerebral activation in response to language compared to term infants; more abnormal patterns at term equivalent correlate with poorer neurodevelopmental performance at 6 months of age [23].
The noisy environment of the NICU with high-frequency, loud, and arrhythmic sounds may alter auditory pathway development and undoubtedly has broader physiologic effects. Loud noises result in increases in heart rate and blood pressure as well as decreases in respiratory rate and oxygen saturation. Startle from loud noises can interfere with sleep and results in crying which can increase intracranial pressure [24]. There are conflicting results when noise is correlated with later neurodevelopmental performance. Environmental noise interferes with an infant’s tactile learning as evidenced by reduced habituation to tactile stimuli in a noisy environment [25]. Excessive noise seems to be detrimental but exposure to human voice and speech is essential for language development so that efforts to reduce noise exposure should not filter out language exposure [24].
The quality of acoustic experience is important for development. Postnatal exposure to mother’s voice in premature infants may promote cortical plasticity [26]. Exposure to maternal voice prior to term equivalent increases auditory cortex volume compared to exposure to ambient NICU noise.
Somatic Sensation
Preterm somatosensory and pain circuitry is functional but immature. Peripheral receptive fields are large, descending networks that modulate the pain response are not functional until close to term, and pathways for noxious and benign stimuli overlap, making discrimination between the two types of input less sensitive. These factors can result in long-term changes in somatosensory processing after premature birth.
Unnatural somatosensory experience during preterm life can cause wide-spread alterations in physiologic development related to activation of the sympathetic system. Repeated painful procedures increase cortisol at a critical period of development. Repeated spikes in cortisol are hypothesized to cause long-term changes in network formation and hypothalamus-pituitary-adrenal axis set point as demonstrated in children and rat pups; there is initially a drop in circulating cortisol in early infancy followed by long-term elevations at 18 months [27, 28]. Painful stimuli increases cerebral metabolism and results in oxidative stress and inflammation, both of which may damage sensitive pre-oligodendrocytes. Maternal interactions can dampen the chronic cortisol increase seen in preterm infants [29].
Cortical thickness, functional cortical activity, and visual-perceptual abilities are reduced in children who were exposed to a higher number of painful procedures as preterm neonates [30, 31]. Such children also demonstrate more internalizing behaviors at school age [30]. Preterm infants are more likely to demonstrate sensory processing disorder and atypical “sensation seeking.” Risk factors for these symptoms include earlier prematurity, white matter lesions, and male gender [32]. Sensory abnormalities are associated with executive and cognitive dysfunction and can be improved with therapies [33].
Taste/Smell
Gustatory and olfactory systems are functional in the 2nd trimester. These two systems work together to establish feeding behavior and neural pathways that regulate hormonal control of appetite [34]. There is evidence that altered experience with taste and oral-motor functioning, as can be seen with extended tube feeding, may slow the achievement of oral feeds, alter the immune response, and affect long-term feeding habits [35].
In utero olfactory experience seems to create memory—babies may be able to identify the scent of amniotic fluid [36]. Postnatal olfactory memory of both pleasant and unpleasant odorants (such as NICU disinfectant) has been documented at 21 months of age [37, 38].
Preterm gustatory and olfactory experience is often disconnected from feeding. However, there is evidence that preterm exposure to mother’s colostrum and milk may decrease the time it takes to achieve full oral feeds, and ultimately reduce time to discharge home [39, 40]. Even before a baby is ready to feed orally, exposure to mother’s scent and milk may help prepare the infant for eventual oral feeds.
Given that there is a small but increased risk of diet-associated disease such as diabetes and hypertension in adults born preterm [41, 42], more research is needed on the association of integrating feeding and sensory experience with longer-term nutrition and health.
Motor Development and Cerebral Palsy
Premature exposure to the extra-uterine environment, including gravity and sensory experiences, alters musculoskeletal and nervous system development thereby altering the trajectory of motor development for otherwise healthy children [43,44,45,46]. Perinatal complications in very preterm and very low birth weight children such as IVH further increases the risk of motor impairment. During the first 2 years, milestone attainment rates are highly dependent on gestational age at birth [44]. Severe disability at 30 months is highly predictive of outcome at 6 years, but less affected children are still at risk for impairments. Of the children noted to have “other” or “no” disabilities at 30 months, 38% were found upon reassessment at 6 years to have moderate or severe disability. While preterm children may demonstrate normal milestone achievement in their toddler years, subtle motor problems often become apparent when greater demands are placed on them during their school years [47]. Importantly, motor impairments, whether mild or severe, are associated with poorer academic outcomes and less participation in social leisure activities when compared to children without motor impairment [48].
CP is a disorder of motor development and posture, which causes activity limitations that are due to a non-progressive disturbance occurring in the developing brain [49]. CP occurs more frequently in children born prematurely, with the risk increasing with decreasing gestation age. The prevalence of CP among extremely preterm children ranges from 16 to 21% [47]. The EPIPAGE Cohort (étude épidémiologique sur les petits âges gestationnels) study which is a large population-based cohort evaluated infants born between 22 and 32 weeks gestation in nine regions of France in 1997. This study found that at 2 years of age, prevalence of CP was 20% in those born at 24–26 weeks gestation compared with 4% in those born at 32 weeks [50]. Preterm children are more likely to present with bilateral cerebral palsy in which spastic diplegia is the most frequent subtype.
Risk factors for the development of CP include lower gestational age, low birthweight, multiple gestation, intrauterine infection, placental abruption, preterm labor or prolonged rupture of membranes, respiratory distress, postnatal corticosteroids, and neonatal sepsis [51]. As survival rates for extreme prematurity increase, the rate of cerebral palsy may also increase [52], although some studies also find increases in survival with normal neurodevelopment. For example, of infants born at 22–24 weeks GA from 200 to 2011 when assessed at 18–22 months, overall survival increased from 30 to 36% and normal neurologic outcome increased from 16 to 20% [3]. Cerebral lesions identified by cranial ultrasound in infants born 24–32 weeks gestation were the most important predictor found by the EPIPAGE study. Of particular note, the odds of developing CP were increased 30-fold in infants with white matter abnormalities consistent with cystic periventricular leukomalacia or intraparenchymal hemorrhage. This study and others also found male sex to be an independent risk factor for CP [53].
Identifying patients at risk of CP is important for initiating early therapy which is more likely to be effective than therapy after infancy [54•]. Cranial ultrasound abnormalities are able to predict motor disability in most preterm infants; however, one third of infants with CP had no ultrasound abnormalities identified. In addition to neuroimaging techniques, functional general movements assessment at 1 month corrected age have high sensitivity for predicting motor impairment in preterm infants born at < 30 weeks GA. It is recommended that general movements at both 1 and 3 months corrected age be evaluated [55].
Preterm infants also have a high prevalence of minor motor dysfunction and poor coordination that may not meet the diagnosis of cerebral palsy. Such children may be diagnosed with developmental coordination disorder (DCD) which is a motor deficit in coordination, balance, gross and fine motor control, and visual motor integration but not consistent with cerebral palsy. The Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (DSM-V) criteria for DCD includes deficiency in motor function but also in activities of daily living and intelligence. Motor impairments milder than CP also have long-term effects on academic achievement, participation in extracurricular activities, self-esteem, and mental health [56]. These impairments continue into adolescence and adulthood illustrating that these motor differences are not merely a delay in acquisition of skills.
Cognitive Development and Impairments Resulting from Prematurity
Cognitive Development
Cognitive development occurs through the interplay of many complex developmental processes. School performance, IQ, and executive functioning are difficult to separate when studying outcomes. At 6 years of age, children born < 26 weeks GA showed impairment of motor, visuospatial, and sensorimotor function which includes planning, self-regulation, inhibition, and motor persistence all of which contribute to cognitive impairments and poor classroom performance [57]. Impairments can be difficult to detect as some children without signs of neurodevelopmental impairment in early childhood will have impairments that only manifest at school age and may persist into adulthood [58].
The EPIPAGE study cohort found cognitive deficits in 31% of surviving children at 8 years old [59]. People born prematurely have lower IQ (approx. 0.82 SD), lower executive functioning (0.51 SD), and lower processing speed (0.49 SD) than term born controls [60•]. Decreasing gestational age, decreasing birth weight, neonatal complications, the presence of cerebral lesions, male gender, lack of breast feeding, and low socioeconomic status contribute to cognitive deficits that persist into early childhood and may not be ameliorated by intervention programs outside of infancy [54•, 57, 61,62,63]. Another study found that birth at < 32 weeks GA was associated with poor kindergarten readiness for reading and math [64].
Learning difficulties have been identified in preterm children even after correcting for IQ. The Extremely Low Gestational Age Newborn (ELGAN) cohort found at the 10-year follow-up in children without intellectual disability (verbal and nonverbal IQ > 70) low achievement in math was 27% which was 1.5 times higher than the risk of low reading which was 17%. This high rate of learning disability particularly in mathematics was present even after socioeconomic status was considered [65]. The highest level of education completed is also affected; with decreasing GA at birth, there is an increasing risk of having less than a high school education.
Attention Deficit Hyperactivity Disorder
Behavioral problems such as attention deficit hyperactivity disorder (ADHD) are increased in very premature infants in early childhood. These can substantially affect academic achievement and social integration. As with other neurological complications of prematurity, the lower the gestational age, the higher the rate of ADHD [66]. Expression of symptoms in this population may have a higher risk for the inattentive subtype of ADHD. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-V) categorizes ADHD as a neurodevelopmental disorder and allows the diagnosis to be made in patients with comorbid autism.
The ELGAN cohort evaluated at 10 years was able to identify antenatal and postnatal risk factors for ADHD. Three maternal factors were identified: young age at time of delivery, pre-pregnancy obesity, and pregnancy smoking. Additional antecedents to ADHD found include antenatal magnesium exposure which is thought to be a surrogate for pre-eclampsia, male sex, singleton birth, receipt of sedative or antibiotic medications, necrotizing enterocolitis, ventriculomegaly, pre-threshold retinopathy of prematurity, and mechanical ventilation on postnatal day 7 [67]. Children with ADHD with or without intellectual disability are at high risk of academic underachievement [68].
Language
Speech development and communication require a complex interaction of auditory, social, motor, and cognitive skills, and is dependent on the social environment in which the infant is cared for. These factors are affected by premature birth and result in language impairment that has early detectable signs as well as long lasting effects. For infants born at < 26 weeks GA, 25% have language impairment in preschool years, while 1/3 are affected if born at < 36 weeks GA [69]. Expressive language is more impaired than receptive [70]. By 36 months, gestational age at birth has less impact on cognition and receptive language compared to chronological age; however, expressive language is still a function of degree of prematurity, indicating that prematurity differentially affects various aspects of language development [71].
Development of communication starts with exposure to voice, which as discussed above, can be limited in the NICU, and confounded by exposure to other loud auditory inputs. Interventions aimed at increasing voice exposure may be beneficial. Exposure to maternal voice was observed to increase the size of auditory cortex in premature infants [26]. Language exposure between 32 and 36 weeks GA is associated with improved developmental measures of IQ and language skills at 18 months [72•].
The cerebral network correlates of abnormal language development have been studied by neuroimaging. Functional connectivity in language pathways is altered by preterm birth. This pathway alteration persists into adulthood and correlates with later language scores [73].
Mean diffusivity and fractional anisotropy at term equivalent along the left superior temporal gyrus can predict language skills at 2 years of age [74]. Deficits in simple language skills tend to catch up in otherwise neurologically intact children born prematurely, but deficits in complex language skills lag further behind peers even as children reach high school age [75]. There are persistent differences in cortical activation pathways while listening to language in preterm adolescents [76], specifically compared to full-term individuals, those born preterm recruited more areas of frontal cortex in order to comprehend difficult language tasks.
The risk of language delays is detectable in altered preverbal skills of joint attention and gaze following in preterm infants who have later language delay [77]. Intervention early with maternal voice may be important to maximize development. Music therapy can facilitate infant-parent communication, relieve infant and caregiver stress, and improve feeding behavior [78,79,80]. Direct intervention aimed at preparing caregivers can help as well because caregiver education and cognitive ability are major factors in a child’s language development after NICU discharge [81].
Social and Psychiatric Impairments
Several authors have described a “preterm behavioral phenotype” which includes a tendency toward internalizing traits (anxiety, depression), inattention, and social difficulties [82]. Externalizing behaviors including aggression are also more common in preterm born children [83]. Critical illness and NICU care also alter parental interaction and may affect longer-term parenting habits, which may contribute to altered social development. Survivors of prematurity have a 3–4-fold increased risk of psychiatric disorders, which emphasizes the importance of screening in this population [84]. The traits of this “preterm behavioral phenotype” are measurable from preschool age through adulthood [85•, 86, 87]. The “preterm personality” carries an increased risk of autism and psychiatric disorders [88]. Psychiatric risk is also impacted by cognitive impairment which is more common after preterm birth [89].
The neurologic basis for behavioral morbidity is an area of active study and structural correlates have been identified. Emotions of others are processed through a network involving the amygdala and fusiform gyrus in the temporal lobe. Preterm adolescents with difficulty with emotion-processing have alterations in the fusiform gyrus and orbitofrontal cortex [86]. Adults born preterm have difficulty recognizing anger and this difficulty corresponds to altered connectivity between the amygdala, temporal lobe, and parietal regions [90]. Gray and white matter volume also correspond to IQ, memory, and executive function, all of which impact social cognition [7].
Early clues to impaired social and emotional development can be seen in infants [91]. Impaired joint attention corresponds to lower IQ and social skills [92]. While the early visual experience of prematurity may result in accelerated maturation of gaze control, preterm infants demonstrate less visual fixation on social images than term infants and at times avoid social gaze [93], which may be a function of impaired attention [94]. “Theory of mind,” a concept that describes one’s ability to assign goals and beliefs to one’s self and to others, seems to be impaired by prematurity. Premature children demonstrate less empathy [95] and more difficulty with interpreting facial expression and body language [87].
The risk of autism spectrum disorder (ASD) in preterm individuals is associated with decreasing gestational age, growth restriction, and exposure to inflammatory states such as maternal infection, with the greatest risk in infants born < 1500 g and < 28 weeks GA [96, 97]. IVH and requiring high-frequency ventilation further increase the risk of ASD [98]. The prevalence of autism in the US population is 1.5% while the prevalence of autism in infants born 23–27 weeks GA is 7.1%, based on Autism Diagnostic Observation Scale criteria [99•]. The ASD phenotype in preterms may be different than in the general population—preterms demonstrate a less striking male predominance of ASD, there is increased symptom severity related to social skills [100], and preterms with autism are also more likely to have lower IQ than full-term individuals with autism (69.5 vs 74.6) [101].
While autism involves altered social interactions and may be contributed to by perinatal inflammation, schizophrenia shares many characteristics with ASD [102]. Several obstetric conditions contribute to the risk of schizophrenia including prematurity, infection, and pre-eclampsia—the latter two of which are major causes of prematurity [103]. Mood disorders (anxiety, depression, bipolar) are also more common in preterm individuals [82], although a recent study did not find this risk persistent through adulthood [104].
Other Neurologic Complications
Other neurologic complications can occur more often after preterm birth. Seizures are common in the neonatal period with 5% of unselected preterm infants experiencing seizures in the first 3 days of life [105•]. Seizures during this time are associated with IVH, death, and language delay at 2 years of age [106]. The risk of epilepsy increases with increasing prematurity. While the prevalence of epilepsy worldwide is 0.4–1% [107], 7% of children born < 28 weeks GA develop epilepsy [60•]. Preterm infants often receive steroids, which is associated with a higher risk of febrile seizure [108].
IVH occurs in 25–30% of preterm infants and is a risk factor for CP and hydrocephalus often requiring surgical intervention [109•]. IVH in turn is associated with in utero factors including placental abruption and inflammation, both of which lead to preterm birth [110••]. IVH may be reduced by cesarean section delivery in very preterm babies [111].
Sleep may also be impacted by prematurity. In early preterm children, sleep habits were associated with earlier bedtime, longer sleep onset latency, and longer sleep duration [112]. Altered sleep was noted even in preterm children without neurodevelopmental disability; however, sleep difficulties increased with increasing neurodevelopmental disabilities.
Conclusion
While survival of our youngest infants is increasing, neurodevelopmental impairments present a lifelong challenge for a significant proportion of survivors. Studies are underway to examine the mechanisms of altered neural development which will aid in eventually developing better ways to prevent and ameliorate long-term disability.
Abbreviations
- GA:
-
Gestational age
- IVH:
-
Intraventricular hemorrhage
- MRI:
-
Magnetic resonance imaging
- IQ:
-
Intelligence quotient
- ADC:
-
Apparent diffusion coefficient
- MRS:
-
Magnetic resonance spectroscopy
- DTI:
-
Diffusion tensor imaging
- CP:
-
Cerebral palsy
- ROP:
-
Retinopathy of prematurity
- NICU:
-
Neonatal intensive care unit
- ÉPIPAGE Cohort:
-
Epidemiological study of premature infants (étude épidémiologique sur les petits âges gestationnels)
- DCD:
-
Developmental coordination disorder
- DSM:
-
Diagnostic and Statistical Manual of Mental Disorders
- ADHD:
-
Attention deficit hyperactivity disorder
- ELGAN:
-
Extremely low gestational age newborns
- ASD:
-
Autism spectrum disorder
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major Importance
Liu L, Oza S, Hogan D, Chu Y, Perin J, Zhu J, et al. Global, regional, and national causes of under-5 mortality in 2000-15: an updated systematic analysis with implications for the Sustainable Development Goals. Lancet. 2016;388(10063):3027–35.
•• Younge N, Goldstein RF, Bann CM, Hintz SR, Patel RM, Smith PB, et al. Survival and neurodevelopmental outcomes among periviable infants. N Engl J Med. 2017;376(7):617–28. Neonatal Research Network study of outcomes of infants born at 22-24 weeks gestational age over an 11-year period followed up at 18-22 months. This large cohort over a decade was able to reveal trends over the period of the study.
Younge N, Goldstein RF, Cotten CM, Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Survival and neurodevelopment of periviable infants. N Engl J Med. 2017;376(19):1890–1.
Hubel DH, Wiesel TN. Ferrier lecture. Functional architecture of macaque monkey visual cortex. Proc R Soc Lond B Biol Sci. 1977;198(1130):1–59.
Greenough WT, West RW, DeVoogd TJ. Subsynaptic plate perforations: changes with age and experience in the rat. Science. 1978;202(4372):1096–8.
Markham JA, Greenough WT. Experience-driven brain plasticity: beyond the synapse. Neuron Glia Biol. 2004;1(4):351–63.
Nosarti C, Nam KW, Walshe M, Murray RM, Cuddy M, Rifkin L, et al. Preterm birth and structural brain alterations in early adulthood. Neuroimage Clin. 2014;6:180–91.
Walsh JM, Doyle LW, Anderson PJ, Lee KJ, Cheong JLY. Moderate and late preterm birth: effect on brain size and maturation at term-equivalent age. Radiology. 2014;273(1):232–40.
• Bjuland KJ, Rimol LM, Løhaugen GCC, Skranes J. Brain volumes and cognitive function in very-low-birth-weight (VLBW) young adults. Eur J Paediatr Neurol. 2014;18(5):578–90. This study is one of the few that performed neuroimaging in adults born prematurely..
Viola A, Confort-Gouny S, Schneider JF, le Fur Y, Viout P, Chapon F, et al. Is brain maturation comparable in fetuses and premature neonates at term equivalent age? AJNR Am J Neuroradiol. 2011;32(8):1451–8.
Akazawa K, Chang L, Yamakawa R, Hayama S, Buchthal S, Alicata D, et al. Probabilistic maps of the white matter tracts with known associated functions on the neonatal brain atlas: application to evaluate longitudinal developmental trajectories in term-born and preterm-born infants. Neuroimage. 2016;128:167–79.
Åkerblom H, Andreasson S, Holmström G. Macular function in preterm children at school age. Doc Ophthalmol. 2016;133(3):151–7.
Braddick O, Atkinson J, Wattam-Bell J. VERP and brain imaging for identifying levels of visual dorsal and ventral stream function in typical and preterm infants. Prog Brain Res. 2011;189:95–111.
Taylor NM, Jakobson LS, Maurer D, Lewis TL. Differential vulnerability of global motion, global form, and biological motion processing in full-term and preterm children. Neuropsychologia. 2009;47(13):2766–78.
Sripada K, Løhaugen GC, Eikenes L, Bjørlykke KM, Håberg AK, Skranes J, et al. Visual-motor deficits relate to altered gray and white matter in young adults born preterm with very low birth weight. Neuroimage. 2015;109:493–504.
Kavsek M, Bornstein MH. Visual habituation and dishabituation in preterm infants: a review and meta-analysis. Res Dev Disabil. 2010;31(5):951–75.
Weber P, Depoorter A, Hetzel P, Lemola S. Habituation as parameter for prediction of mental development in healthy preterm infants: an electrophysiological pilot study. J Child Neurol. 2016;31(14):1591–7.
American Academy of Pediatrics, J.i.C.o.I.H. Position statement: principles and guidelines for early hearing detection and intervention programs. Pediatrics. 2007;120(4):898–921.
Robertson CM, et al. Permanent bilateral sensory and neural hearing loss of children after neonatal intensive care because of extreme prematurity: a thirty-year study. Pediatrics. 2009;123(5):e797–807.
van Dommelen P, Verkerk PH, van Straaten HLM, Baerts W, von Weissenbruch M, Duijsters C, et al. Hearing loss by week of gestation and birth weight in very preterm neonates. J Pediatr. 2015;166(4):840–843.e1.
Mahmoudzadeh M, Dehaene-Lambertz G, Fournier M, Kongolo G, Goudjil S, Dubois J, et al. Syllabic discrimination in premature human infants prior to complete formation of cortical layers. Proc Natl Acad Sci U S A. 2013;110(12):4846–51.
McMahon E, Wintermark P, Lahav A. Auditory brain development in premature infants: the importance of early experience. Ann N Y Acad Sci. 2012;1252:17–24.
Baldoli C, Scola E, Della Rosa PA, Pontesilli S, Longaretti R, Poloniato A, et al. Maturation of preterm newborn brains: a fMRI-DTI study of auditory processing of linguistic stimuli and white matter development. Brain Struct Funct. 2015;220(6):3733–51.
Wachman EM, Lahav A. The effects of noise on preterm infants in the NICU. Arch Dis Child Fetal Neonatal Ed. 2011;96(4):F305–9.
Lejeune F, Parra J, Berne-Audéoud F, Marcus L, Barisnikov K, Gentaz E, et al. Sound interferes with the early tactile manual abilities of preterm infants. Sci Rep. 2016;6:23329.
Webb AR, Heller HT, Benson CB, Lahav A. Mother’s voice and heartbeat sounds elicit auditory plasticity in the human brain before full gestation. Proc Natl Acad Sci U S A. 2015;112(10):3152–7.
Grunau RE, Weinberg J, Whitfield MF. Neonatal procedural pain and preterm infant cortisol response to novelty at 8 months. Pediatrics. 2004;114(1):e77–84.
Vinall J, Miller SP, Bjornson BH, Fitzpatrick KPV, Poskitt KJ, Brant R, et al. Invasive procedures in preterm children: brain and cognitive development at school age. Pediatrics. 2014;133(3):412–21.
Brummelte S, Grunau RE, Zaidman-Zait A, Weinberg J, Nordstokke D, Cepeda IL. Cortisol levels in relation to maternal interaction and child internalizing behavior in preterm and full-term children at 18 months corrected age. Dev Psychobiol. 2011;53(2):184–95.
Ranger M, Chau CMY, Garg A, Woodward TS, Beg MF, Bjornson B, et al. Neonatal pain-related stress predicts cortical thickness at age 7 years in children born very preterm. PLoS One. 2013;8(10):e76702.
Doesburg SM, Chau CM, Cheung TPL, Moiseev A, Ribary U, Herdman AT, et al. Neonatal pain-related stress, functional cortical activity and visual-perceptual abilities in school-age children born at extremely low gestational age. Pain. 2013;154(10):1946–52.
Machado ACCP, et al. Sensory processing during childhood in preterm infants: a systematic review. Rev Paul Pediatr. 2017;35(1):92–101.
Barton EE, Reichow B, Schnitz A, Smith IC, Sherlock D. A systematic review of sensory-based treatments for children with disabilities. Res Dev Disabil. 2015;37:64–80.
Bloomfield FH, Alexander T, Muelbert M, Beker F. Smell and taste in the preterm infant. Early Hum Dev. 2017;114:31–4.
Lipchock SV, Reed DR, Mennella JA. The gustatory and olfactory systems during infancy: implications for development of feeding behaviors in the high-risk neonate. Clin Perinatol. 2011;38(4):627–41.
Varendi H, Porter RH, Winberg J. Attractiveness of amniotic fluid odor: evidence of prenatal olfactory learning? Acta Paediatr. 1996;85(10):1223–7.
Delaunay-El Allam M, et al. Long-lasting memory for an odor acquired at the mother’s breast. Dev Sci. 2010;13(6):849–63.
Bartocci M, Winberg J, Papendieck G, Mustica T, Serra G, Lagercrantz H. Cerebral hemodynamic response to unpleasant odors in the preterm newborn measured by near-infrared spectroscopy. Pediatr Res. 2001;50(3):324–30.
Beker F, Opie G, Noble E, Jiang Y, Bloomfield FH. Smell and taste to improve nutrition in very preterm infants: a randomized controlled pilot trial. Neonatology. 2017;111(3):260–6.
Yildiz A, Arikan D, Gözüm S, Taştekın A, Budancamanak I. The effect of the odor of breast milk on the time needed for transition from gavage to total oral feeding in preterm infants. J Nurs Scholarsh. 2011;43(3):265–73.
Crump C, Winkleby MA, Sundquist K, Sundquist J. Risk of diabetes among young adults born preterm in Sweden. Diabetes Care. 2011;34(5):1109–13.
Crump C, Winkleby MA, Sundquist K, Sundquist J. Risk of hypertension among young adults who were born preterm: a Swedish national study of 636,000 births. Am J Epidemiol. 2011;173(7):797–803.
van Haastert IC, de Vries LS, Helders PJM, Jongmans MJ. Early gross motor development of preterm infants according to the Alberta Infant Motor Scale. J Pediatr. 2006;149(5):617–22.
van Dokkum NH, de Kroon MLA, Bos AF, Reijneveld SA, Kerstjens JM. Attainment of gross motor milestones by preterm children with normal development upon school entry. Early Hum Dev. 2018;119:62–7.
Bracewell M, Marlow N. Patterns of motor disability in very preterm children. Ment Retard Dev Disabil Res Rev. 2002;8(4):241–8.
Fallang B, Hadders-Algra M. Postural behavior in children born preterm. Neural Plast. 2005;12(2–3):175–82. discussion 263-72
Marlow N, Wolke D, Bracewell MA, Samara M, EPICure Study Group. Neurologic and developmental disability at six years of age after extremely preterm birth. N Engl J Med. 2005;352(1):9–19.
Dahan-Oliel N, Mazer B, Riley P, Maltais DB, Nadeau L, Majnemer A. Participation and enjoyment of leisure activities in adolescents born at ≤ 29 week gestation. Early Hum Dev. 2014;90(6):307–14.
Himpens E, van den Broeck C, Oostra A, Calders P, Vanhaesebrouck P. Prevalence, type, distribution, and severity of cerebral palsy in relation to gestational age: a meta-analytic review. Dev Med Child Neurol. 2008;50(5):334–40.
Ancel PY, Livinec F, Larroque B, Marret S, Arnaud C, Pierrat V, et al. Cerebral palsy among very preterm children in relation to gestational age and neonatal ultrasound abnormalities: the EPIPAGE cohort study. Pediatrics. 2006;117(3):828–35.
McIntyre S, Morgan C, Walker K, Novak I. Cerebral palsy—don’t delay. Dev Disabil Res Rev. 2011;17(2):114–29.
Vincer MJ, Allen AC, Joseph KS, Stinson DA, Scott H, Wood E. Increasing prevalence of cerebral palsy among very preterm infants: a population-based study. Pediatrics. 2006;118(6):e1621–6.
Beaino G, et al. Predictors of cerebral palsy in very preterm infants: the EPIPAGE prospective population-based cohort study. Dev Med Child Neurol. 2010;52(6):e119–25.
• Spittle A, Orton J, Anderson PJ, Boyd R, Doyle LW. Early developmental intervention programmes provided post hospital discharge to prevent motor and cognitive impairment in preterm infants. Cochrane Database Syst Rev 2015;776(11): p. CD005495 Review of effectiveness of developmental interventions which highlights the importance of early therapy.
Spittle AJ, Boyd RN, Inder TE, Doyle LW. Predicting motor development in very preterm infants at 12 months’ corrected age: the role of qualitative magnetic resonance imaging and general movements assessments. Pediatrics. 2009;123(2):512–7.
Spittle AJ, Orton J. Cerebral palsy and developmental coordination disorder in children born preterm. Semin Fetal Neonatal Med. 2014;19(2):84–9.
Marlow N, Hennessy EM, Bracewell MA, Wolke D, for the EPICure Study Group. Motor and executive function at 6 years of age after extremely preterm birth. Pediatrics. 2007;120(4):793–804.
Serenius F, Ewald U, Farooqi A, Fellman V, Hafström M, Hellgren K, et al. Neurodevelopmental outcomes among extremely preterm infants 6.5 years after active perinatal care in Sweden. JAMA Pediatr. 2016;170(10):954–63.
Marret S, Marchand-Martin L, Picaud JC, Hascoët JM, Arnaud C, Rozé JC, et al. Brain injury in very preterm children and neurosensory and cognitive disabilities during childhood: the EPIPAGE cohort study. PLoS One. 2013;8(5):e62683.
• Hirschberger RG, et al. Co-occurrence and severity of neurodevelopmental burden (cognitive impairment, cerebral palsy, autism spectrum disorder, and epilepsy) at age ten years in children born extremely preterm. Pediatr Neurol. 2018;79:45–52. This study described long-term outcomes related to multiple neurodevelopmental impairments.
Saigal S, Ouden L, Wolke D, Hoult L, Paneth N, Streiner DL, et al. School-age outcomes in children who were extremely low birth weight from four international population-based cohorts. Pediatrics. 2003;112(4):943–50.
Young JM, Morgan BR, Powell TL, Moore AM, Whyte HEA, Smith ML, et al. Associations of perinatal clinical and magnetic resonance imaging measures with developmental outcomes in children born very preterm. J Pediatr. 2016;170:90–6.
Beaino G, Khoshnood B, Kaminski M, Marret S, Pierrat V, Vieux R, et al. Predictors of the risk of cognitive deficiency in very preterm infants: the EPIPAGE prospective cohort. Acta Paediatr. 2011;100(3):370–8.
Shah PE, Kaciroti N, Richards B, Lumeng JC. Gestational age and kindergarten school readiness in a national sample of preterm infants. J Pediatr. 2016;178:61–7.
Akshoomoff N, Joseph RM, Taylor HG, Allred EN, Heeren T, OʼShea TM, et al. Academic achievement deficits and their neuropsychological correlates in children born extremely preterm. J Dev Behav Pediatr. 2017;38(8):627–37.
Sucksdorff M, Lehtonen L, Chudal R, Suominen A, Joelsson P, Gissler M, et al. Preterm birth and poor fetal growth as risk factors of attention-deficit/hyperactivity disorder. Pediatrics. 2015;136(3):e599–608.
Leviton A, Hooper SR, Hunter SJ, Scott MN, Allred EN, Joseph RM, et al. Antecedents of screening positive for attention deficit hyperactivity disorder in ten-year-old children born extremely preterm. Pediatr Neurol. 2018;81:25–30.
Scott MN, Hunter SJ, Joseph RM, OʼShea TM, Hooper SR, Allred EN, et al. Neurocognitive correlates of attention-deficit hyperactivity disorder symptoms in children born at extremely low gestational age. J Dev Behav Pediatr. 2017;38(4):249–59.
Sansavini A, Guarini A, Justice LM, Savini S, Broccoli S, Alessandroni R, et al. Does preterm birth increase a child’s risk for language impairment? Early Hum Dev. 2010;86(12):765–72.
Zerbeto AB, Cortelo FM, Filho ÉC. Association between gestational age and birth weight on the language development of Brazilian children: a systematic review. J Pediatr. 2015;91(4):326–32.
Ionio C, Riboni E, Confalonieri E, Dallatomasina C, Mascheroni E, Bonanomi A, et al. Paths of cognitive and language development in healthy preterm infants. Infant Behav Dev. 2016;44:199–207.
• Caskey M, Stephens B, Tucker R, Vohr B. Adult talk in the NICU with preterm infants and developmental outcomes. Pediatrics. 2014;133(3):e578–84. This study highlights NICU practices and exposure of voice.
Kwon SH, Scheinost D, Vohr B, Lacadie C, Schneider K, Dai F, et al. Functional magnetic resonance connectivity studies in infants born preterm: suggestions of proximate and long-lasting changes in language organization. Dev Med Child Neurol. 2016;58 Suppl 4:28–34.
Aeby A, de Tiège X, Creuzil M, David P, Balériaux D, van Overmeire B, et al. Language development at 2 years is correlated to brain microstructure in the left superior temporal gyrus at term equivalent age: a diffusion tensor imaging study. Neuroimage. 2013;78:145–51.
van Noort-van der Spek IL, Franken MC, Weisglas-Kuperus N. Language functions in preterm-born children: a systematic review and meta-analysis. Pediatrics. 2012;129(4):745–54.
Barde LH, et al. Differences in neural activation between preterm and full term born adolescents on a sentence comprehension task: implications for educational accommodations. Dev Cogn Neurosci. 2012;2(Suppl 1):S114–28.
De Schuymer L, et al. Preverbal skills as mediators for language outcome in preterm and full term children. Early Hum Dev. 2011;87(4):265–72.
Shoemark H, Hanson-Abromeit D, Stewart L. Constructing optimal experience for the hospitalized newborn through neuro-based music therapy. Front Hum Neurosci. 2015;9:487.
Standley J. Music therapy research in the NICU: an updated meta-analysis. Neonatal Netw. 2012;31(5):311–6.
Allen KA. Music therapy in the NICU: is there evidence to support integration for procedural support? Adv Neonatal Care. 2013;13(5):349–52.
Asztalos EV, Church PT, Riley P, Fajardo C, Shah PS, Canadian Neonatal Network and Canadian Neonatal Follow-up Network Investigators. Association between primary caregiver education and cognitive and language development of preterm neonates. Am J Perinatol. 2017;34(4):364–71.
Johnson S, Marlow N. Preterm birth and childhood psychiatric disorders. Pediatr Res. 2011;69(5 Pt 2):11R–8R.
Arpi E, Ferrari F. Preterm birth and behaviour problems in infants and preschool-age children: a review of the recent literature. Dev Med Child Neurol. 2013;55(9):788–96.
Burnett AC, Anderson PJ, Cheong J, Doyle LW, Davey CG, Wood SJ. Prevalence of psychiatric diagnoses in preterm and full-term children, adolescents and young adults: a meta-analysis. Psychol Med. 2011;41(12):2463–74.
• Eryigit-Madzwamuse S, Strauss V, Baumann N, Bartmann P, Wolke D. Personality of adults who were born very preterm. Arch Dis Child Fetal Neonatal Ed. 2015;100(6):F524–9. The conclusion of this study attempts to generalize a preterm personality which can lead to inferences about psychological comorbidities of prematurity.
Healy E, Reichenberg A, Nam KW, Allin MPG, Walshe M, Rifkin L, et al. Preterm birth and adolescent social functioning-alterations in emotion-processing brain areas. J Pediatr. 2013;163(6):1596–604.
Williamson KE, Jakobson LS. Social perception in children born at very low birthweight and its relationship with social/behavioral outcomes. J Child Psychol Psychiatry. 2014;55(9):990–8.
Nosarti C, Reichenberg A, Murray RM, Cnattingius S, Lambe MP, Yin L, et al. Preterm birth and psychiatric disorders in young adult life. Arch Gen Psychiatry. 2012;69(6):E1–8.
Kroll J, Froudist-Walsh S, Brittain PJ, Tseng CEJ, Karolis V, Murray RM, et al. A dimensional approach to assessing psychiatric risk in adults born very preterm. Psychol Med. 2018:1–7.
Papini C, White TP, Montagna A, Brittain PJ, Froudist-Walsh S, Kroll J, et al. Altered resting-state functional connectivity in emotion-processing brain regions in adults who were born very preterm. Psychol Med. 2016;46(14):3025–39.
Zmyj N, Witt S, Weitkämper A, Neumann H, Lücke T. Social cognition in children born preterm: a perspective on future research directions. Front Psychol. 2017;8:455.
Smith L, Ulvund S. The role of joint attention in later development among preterm children: linkages between early and middle childhood. Soc Dev. 2003;12(2):222–34.
Telford EJ, Fletcher-Watson S, Gillespie-Smith K, Pataky R, Sparrow S, Murray IC, et al. Preterm birth is associated with atypical social orienting in infancy detected using eye tracking. J Child Psychol Psychiatry. 2016;57(7):861–8.
De Schuymer L, et al. Gaze aversion during social interaction in preterm infants: a function of attention skills? Infant Behav Dev. 2012;35(1):129–39.
Campbell C, Horlin C, Reid C, McMichael J, Forrest L, Brydges C, et al. How do you think she feels? Vulnerability in empathy and the role of attention in school-aged children born extremely preterm. Br J Dev Psychol. 2015;33(3):312–23.
Meldrum SJ, et al. Autism spectrum disorder in children born preterm-role of exposure to perinatal inflammation. Front Neurosci. 2013;7:123.
Joseph RM, Korzeniewski SJ, Allred EN, O’Shea TM, Heeren T, Frazier JA, et al. Extremely low gestational age and very low birthweight for gestational age are risk factors for autism spectrum disorder in a large cohort study of 10-year-old children born at 23-27 weeks’ gestation. Am J Obstet Gynecol. 2017;216(3):304.e1–304.e16.
Kuzniewicz MW, Wi S, Qian Y, Walsh EM, Armstrong MA, Croen LA. Prevalence and neonatal factors associated with autism spectrum disorders in preterm infants. J Pediatr. 2014;164(1):20–5.
• Joseph RM, O’Shea TM, Allred EN, Heeren T, Hirtz D, Paneth N, et al. Prevalence and associated features of autism spectrum disorder in extremely low gestational age newborns at age 10 years. Autism Res. 2017;10(2):224–32. This large cohort study of nearly 1000 preterm children used ADOS for autism diagnosis.
Movsas TZ, Paneth N. The effect of gestational age on symptom severity in children with autism spectrum disorder. J Autism Dev Disord. 2012;42(11):2431–9.
Schieve LA, Baio J, Rice CE, Durkin M, Kirby RS, Drews-Botsch C, et al. Risk for cognitive deficit in a population-based sample of U.S. children with autism spectrum disorders: variation by perinatal health factors. Disabil Health J. 2010;3(3):202–12.
Meyer U, Feldon J, Dammann O. Schizophrenia and autism: both shared and disorder-specific pathogenesis via perinatal inflammation? Pediatr Res. 2011;69(5 Pt 2):26R–33R.
Dalman C, Allebeck P, Cullberg J, Grunewald C, Köster M. Obstetric complications and the risk of schizophrenia: a longitudinal study of a national birth cohort. Arch Gen Psychiatry. 1999;56(3):234–40.
Jaekel J, Baumann N, Bartmann P, Wolke D. Mood and anxiety disorders in very preterm/very low-birth weight individuals from 6 to 26 years. J Child Psychol Psychiatry. 2018;59(1):88–95.
• Lloyd RO, et al. Electrographic seizures during the early postnatal period in preterm infants. J Pediatr. 2017;187:18–25.e2. Preterm infants were consequitively enrolled in this study for continuous EEG recording and seizure identification.
Vesoulis ZA, Inder TE, Woodward LJ, Buse B, Vavasseur C, Mathur AM. Early electrographic seizures, brain injury, and neurodevelopmental risk in the very preterm infant. Pediatr Res. 2014;75(4):564–9.
World Health Organization, Epilepsy Fact Sheet. 2018. http://www.who.int/news-room/factsheets/detail/epilepsy Accessed 2018 May 29.
Tu YF, Wang LW, Wang ST, Yeh TF, Huang CC. Postnatal steroids and febrile seizure susceptibility in preterm children. Pediatrics. 2016;137(4):e20153404.
• Radic JA, Vincer M, McNeely PD. Outcomes of intraventricular hemorrhage and posthemorrhagic hydrocephalus in a population-based cohort of very preterm infants born to residents of Nova Scotia from 1993 to 2010. J Neurosurg Pediatr. 2015;15(6):580–8. This is a large population-based study of approximately 400 preterm infants with IVH.
•• Chevallier M, et al. Leading causes of preterm delivery as risk factors for intraventricular hemorrhage in very preterm infants: results of the EPIPAGE 2 cohort study. Am J Obstet Gynecol. 2017;216(5):518.e1–518.e12. This large multicenter population-based study in France provided multiple important observations.
Gamaleldin I, Harding D, Siassakos D, Draycott T, Odd D. Significant intraventricular hemorrhage is more likely in very preterm infants born by vaginal delivery: a multi-centre retrospective cohort study. J Matern Fetal Neonatal Med. 2017:1–6.
Stangenes KM, Fevang SK, Grundt J, Donkor HM, Markestad T, Hysing M, et al. Children born extremely preterm had different sleeping habits at 11 years of age and more childhood sleep problems than term-born children. Acta Paediatr. 2017;106(12):1966–72.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Margie A. Ream and Lenora Lehwald declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Neurology of Systemic Diseases
Rights and permissions
About this article
Cite this article
Ream, M.A., Lehwald, L. Neurologic Consequences of Preterm Birth. Curr Neurol Neurosci Rep 18, 48 (2018). https://doi.org/10.1007/s11910-018-0862-2
Published:
DOI: https://doi.org/10.1007/s11910-018-0862-2